Abstract
The aims of this study were to compare the prevalence of the metabolic syndrome according to the WHO and NCEP ATP III criteria in Korean adults, and to compare the prevalence of the metabolic syndrome with the results in previous Korean studies. The study comprised 1,230 subjects (627 men, 603 women) aged 30-79 years (mean 52.4±10.3 years) who underwent medical check-up from April to June, 2001 in the Korea Association of Health (KAH). The prevalence of the metabolic syndrome according to the modified WHO criteria was 21.8% of men and 19.4% of women. However, the prevalence was increased 1.6 times (34.2%) in men and 2.0 times (38.7%) in women using the modified NCEP criteria. The prevalence of the metabolic syndrome has varied widely according to differences in the criteria. Thus, further studies are necessary to define the appropriate criteria of the metabolic syndrome for Korean adults.
Keywords: Metabolic syndrome, criteria, obesity, prevalence
INTRODUCTION
In 1988, Gerald Reaven reintroduced the concept of syndrome X for the clustering of cardiovascular risk factors like glucose intolerance, hypertension, high triglycerides, and low HDL cholesterol.1
In 1998, the World Health Organization (WHO) proposed a working definition for this syndrome.2 Then the National Cholesterol Education Program (NCEP) proposed new criteria for this syndrome in 2001, which is considered easier for clinical application.3
While the prevalence of obesity is lower in Asian populations than in Western countries, the health risks associated with obesity occur at a lower body mass index (BMI) in Asian populations.4-7 Thus new criteria to define overweight and obesity for Asians in the Asia-Pacific Region were proposed in 2000 by WHO.8
The prevalence of the metabolic syndrome has shown marked variation from different studies, most likely because the criteria for the definition of the metabolic syndrome have not been determined and because of ethnic differences.9-13 In Korea, limited studies are available about the prevalence of the metabolic syndrome,14-18 and there are no appropriate diagnostic criteria which consider the Korean ethnic character. Thus, the aims of this study were, 1) to compare the prevalence of the metabolic syndrome according to the WHO and NCEP ATP III criteria in Korean adults, and 2) to compare the prevalence of the metabolic syndrome with the results in previous Korean studies.
MATERIALS AND METHODS
The Korean Metabolic Syndrome Study was designed in 2001 as a prospective study, primarily to investigate the metabolic syndrome as a risk factor for cardiovascular disease in the Korean general population. From individuals participating in medical check-ups for the Korea Association of Health (KAH) from April to June, 2001, 1,230 subjects (627 men, 603 women) aged 30-79 years (mean 52.4±10.3 years) were included in the present study.
Methods
After an overnight fast, fasting blood samples were drawn from subjects to measure plasma glucose, serum insulin, total cholesterol, HDL cholesterol, and triglyceride concentrations.
Plasma glucose was measured with a glucose oxidase method (Hitachi 747 automatic analyzer, Hitachi, Tokyo). Glucose tolerance was assessed according to the new American Diabetes Association criteria. Thus, subjects with a fasting plasma glucose ≥ 7.0 mmol/L (126 mg/dL) and/or use of medications for diabetes were considered to have diabetes, 6.1-6.9 mmol/L (110-125 mg/dL) to have impaired fasting glucose (IFG), and < 6.1 mmol/L (110 mg/dL) to have normal fasting glucose (NFG).
Serum insulin concentrations were measured with radioimmunoassay (Linco Research, Inc., Missouri, USA) with an interassay coefficient of variation (CV) of 4%. This assay does not crossreact with human pro-insulin (< 0.2%).
To obtain an estimate of insulin resistance, we applied the homeostasis model assessment of insulin resistance (HOMA-IR) using the following formula: HOMA-IR=fasting insulin (µU/ml) × fasting plasma glucose (mmol/l)/22.5.19 HOMA-IR was not estimated in patients treated with insulin.
Serum total cholesterol, HDL cholesterol, and triglycerides were measured using an autoanalyzer with enzymatic colorimetric method (Hitachi 747, Hitachi, Tokyo). LDL cholesterol concentrations were calculated using the Friedewald formula.20
Blood pressure was measured by using a standard mercury sphygmomanometer after the subject had been seated for at least 5 minutes.
BMI was calculated as weight (kg) divided by the square of height (m2) after body weight and height were measured with subjects in light clothing without shoes. Waist circumference was measured with a soft tape on standing subjects midway between the lowest rib and the iliac crest.
A standardized health questionnaire was completed by specially-trained nurses, covering the subjects' past medical history, including current and previous medication and smoking habits.
Definition of the metabolic syndrome according to modified WHO definition
We used modified criteria of the 1999 WHO definition for the metabolic syndrome.2 We excluded IGT because of the inconvenience and cost of the oral glucose tolerance test. We used HOMA-IR instead of the glucose disposal rate by insulin clamp for insulin resistance. Microalbuminuria was excluded as a component of the metabolic syndrome because of its low prevalence (3-7%) in nondiabetic subjects.11 We also used the new criteria of BMI in the Asia-Pacific Region.8
From these considerations, the modified WHO definition required fasting glucose ≥ 6.1 mmol/L (IFG or DM) or insulin resistance (HOMA-IR in the top quartile of the non diabetic population) plus at least two of the following: 1) obesity, defined as a high BMI (≥ 25 kg/m2) and/or a high WHR (≥ 0.9 in men and ≥ 0.85 in women), 2) dyslipidemia, defined as elevated triglyceride (≥ 1.7 mmol/L (150 mg/dL)) and/or low HDL cholesterol (< 0.9 mmol/L (35 mg/dL) in men and < 1.0 mmol/L (39 mg/dL) in women), and 3) hypertension, defined as antihypertensive medication and/or elevated blood pressure (≥ 140 mm Hg systolic and/or ≥ 90 mmHg diastolic).
Definition of the metabolic syndrome according to modified NCEP ATP III definition
We used the new criteria of waist circumference in the Asia-Pacific Region instead of the original criteria.8 Thus, the modified NCEP definition required at least three of the following: 1) increased waist circumference (> 90 cm in men and > 80 cm in women), 2) high triglycerides (≥ 1.7 mmol/L (150 mg/dL)), 3) low HDL cholesterol (< 1.04 mmol/L (40 mg/dL) in men and < 1.29 mmol/L (50 mg/dL) in women), 4) high blood pressure (≥ 130/85 mmHg or current antihypertensive medication), and 5) high fasting glucose (≥ 6.1 mmol/L (110 mg/dL) or current antidiabetic medication).3
Statistical analysis
The values are given as means±SD. The clinical and metabolic characteristics of the study subjects were compared by independent t-test, chi-square test or Fisher's exact test between men and women. The prevalence of the metabolic syndrome and its components between sex and age groups was compared by chi-square test or Fisher's exact test. The statistical analyses were performed with SPSS program for Windows (SPSS Inc., Chicago, IL, USA). A p value < 0.05 was considered statistically significant.
RESULTS
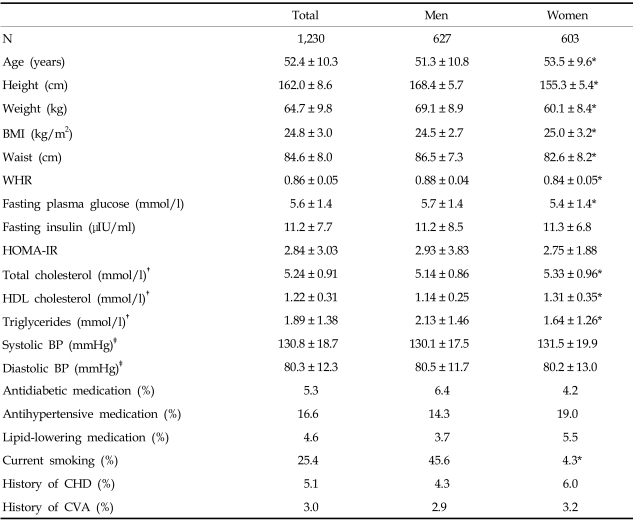
The clinical and metabolic characteristics of the subjects are given in Table 1. Women were older than men. The average levels of height, weight, WC, and WHR were higher in men than in women, but BMI was higher in women. FPG and TG levels were higher in men, but TC and HDL cholesterol levels were higher in women. However, SBP, DBP, fasting insulin level and HOMA-IR showed no significant difference between genders. Eight percent of women and 13.2% of men had diabetes, and 9.3% of men and 4.3% of women had IFG (data not shown).
Table 1.
Clinical and Metabolic Characteristics of the Subjects
CHD, coronary heart disease; CVA, cerebrovascular accident.
Data are means±SD and %.
*p < 0.05.
†, ‡only untreated patients.
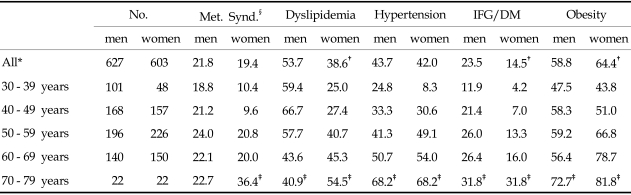
Prevalence of the metabolic syndrome and its components according to the modified WHO criteria (Table 2)
Table 2.
Prevalence of the Metabolic Syndrome and its Components According to the Modified WHO Criteria
IFG, impaired fasting glucose; DM, diabetes millitus.
Data are number or %.
*age-adjusted.
†p < 0.05 between men and women.
‡p < 0.05 between age group.
§metabotic syndrome.
The prevalence of the metabolic syndrome in women was increased significantly according to increasing age, but in men it did not differ with age group. The prevalence in the 30-39 and 40-49 years groups was higher in men than in women, but in the 50-59, 60-69 and 70-79 years groups was similar between men and women.
The prevalences of dyslipidemia, hypertension, IFG/DM and obesity were increased significantly according to increasing age in both men and women. However, the prevalence of dyslipidemia in men was decreased significantly according to increasing age. The prevalences of dyslipidemia and IFG/DM were higher in men than in women, but the prevalence of obesity was higher in women. The prevalence of hypertension was not different between men and women.
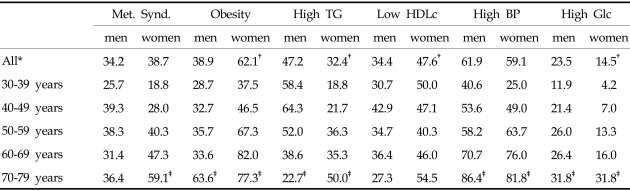
Prevalence of the metabolic syndrome and its components according to the modified NCEP criteria (Table 3)
Table 3.
Prevalence of the Metabolic Syndrome and Its Components According to the Modified NCEP ATP III Criteria
Data are number or %.
*age-adjusted.
†p < 0.05 between men and women.
‡p < 0.05 between age group.
The prevalence of the metabolic syndrome was not different between men and women. It was increased significantly according to increasing age in women, but was not different by age group in men. The prevalence in the 30-39 and 40-49 years groups was higher in men, but in the 50-59, 60-69 and 70-79 years groups was higher in women.
The prevalences of abdominal obesity, high TG, high BP and high glucose were increased significantly according to increasing age in both men and women. The prevalence of high TG in men was decreased significantly according to increasing age. The prevalence of low HDL cholesterol was not different according to increasing age. The prevalences of abdominal obesity and low HDL cholesterol were higher in women than in men, but the prevalences of high TG and high glucose were higher in men. The prevalence of hypertension was not different between men and women.
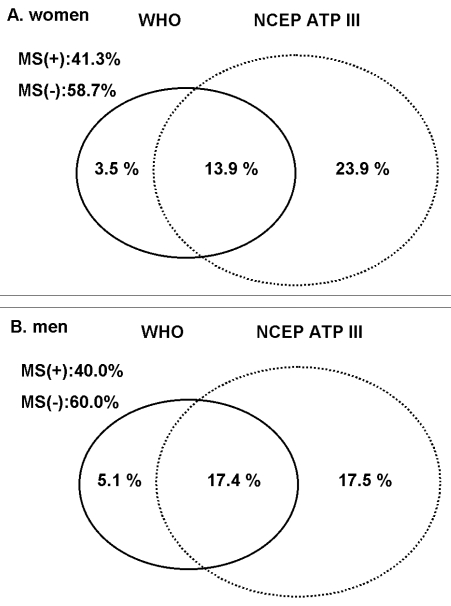
Discrepancy of the metabolic syndrome between the modified WHO and NCEP criteria
The prevalence of the metabolic syndrome according to the modified NCEP criteria was significantly higher than according to the WHO criteria. The prevalence of obesity was slightly higher in the WHO criteria, but the prevalence of high BP was significantly higher in the NCEP criteria.
The prevalence of the metabolic syndrome consistent in both criteria was 13.9% in women and 17.4% in men (Fig. 1). However, 23.9% of women and 17.5% of men had the metabolic syndrome according to the NCEP criteria, but did not according to the WHO criteria. 3.5% in women and 5.1% in men with metabolic syndrome according to the WHO criteria did not have it according to the NCEP criteria.
Fig. 1.
Discrepancy of the metabolic syndrome between the modified WHO and NCEP criteria.
DISCUSSION
We first applied the WHO criteria to assess the prevalence of the metabolic syndrome and compared this assessment with that obtained with the NCEP criteria in Korean adults. The prevalence of the metabolic syndrome according to the modified WHO criteria was 21.8% of men and 19.4% of women. However, according to the modified NCEP criteria the prevalence was increased 1.6 times (34.2%) in men and 2.0 times (38.7%) in women.
In previous studies, the prevalence has varied widely, primarily due to different definitions of the syndrome or selection of various ethnic subgroups. In the ARIC study population, a combination of hypertension (blood pressure > 140/90 mm Hg and/or the use of antihypertensive treatment) and dyslipidemia (triglycerides > 2.26 mmol/l and/or HDL < 0.9 in men and < 1.2 mmol/l in women) was observed in 10% of the subjects.9 In the OPERA study, the prevalence of the metabolic syndrome varied depending on the definition from 0.8 to 35.3%, being lowest in the control men and women and highest in the hypertensive men.10
Applying the WHO definition to the population from the Botnia study in Finland and Sweden, about 10% of persons with NGT, 40% with IGT and 85% with type 2 diabetes had the metabolic syndrome, and the prevalence of the syndrome was also very age-dependent and higher in men than in women.11 In the West Bank population study, the age-adjusted prevalence of the metabolic syndrome defined by the WHO workgroup was 17%.12 In our study, about 10% of subjects with NFG, 50% with IFG and 70% with type 2 diabetes had the metabolic syndrome (data not shown). Thus, the prevalence of the metabolic syndrome in Korean adults according to the WHO criteria was similar to that in Western countries.
In the US, the unadjusted and age-adjusted prevalence of the metabolic syndrome as defined by the NCEP ATP III report was 21.8% and 23.7%, respectively.13 In the present study, the prevalence in Korean adults as defined by the modified NCEP criteria was significantly higher than in Western countries. Therefore, application of the Western NCEP criteria without modification to the Korean population may underestimate the adults at risk.
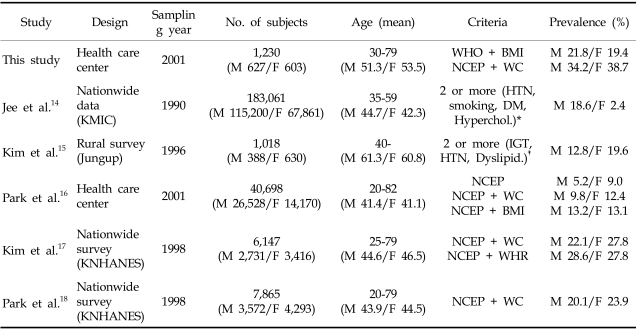
The prevalence of the metabolic syndrome in previous Korean studies has varied widely, from 5.2-28.6% in men and 2.4-27.8% in women (Table 4).14-18 This large variation partly results from different study design. In the Korea Medical Insurance Corporation (KMIC) study, dyslipidemia and obesity were not included in the criteria of the metabolic syndrome.14 In the Jungup study, the criteria of high triglycerides were higher than those of other studies and obesity was not included.15 Thus, the prevalence of the metabolic syndrome in these two studies may have been underestimated.
Table 4.
Prevalence of the Metabolic Syndrome in Korean Adults
KMIC, Korea Medical Insurance Corporation; KNHANES, Korea National Health and Nutrition Survey; WHO + BMI, BMI≥25.0 kg/m2; NCEP, original NCEP ATP III criteria; NCEP + WC, WC≥90(M), 80(F); NCEP + WHR/BMI, criteria for abdominal obesity was replaced with waist to hip ratio or body mass index.
*HTN, BP≥140/90 mmHg, DM, FBS≥126 mg/dL, Hyperchol, TC≥240 mg/dL.
†HTN, BP≥140/90 mmHg, dyslipidemia, TG≥200 mg/dL and HDLC<37(M) 45(F).
Park et al. reported that the prevalence of the metabolic syndrome as defined by the NCEP criteria with abdominal obesity criteria for Asians was 9.8% in men and 12.4% in women; prevalences that were lower than ours.16 The study subjects were recruited from among the clients of a health care center, as was the case in our study design. The different results of the two studies may have arisen from selection bias, which implied that our subjects were older and less healthy than those of Park et al.
In 1998, the first Korea National Health and Nutrition Survey (KNHANES) was conducted, and the nationwide prevalence of the metabolic syndrome was reported recently.17,18 The estimated prevalence according to the NCEP criteria of the present study was higher than that of KNHANES, as our subjects were older (51.3 vs. 44.6 years) and more obese (BMI 24.5 vs. 23.2 kg/m2, WC 86.5 vs. 83.2 cm in men) than those of KNHANES. Therefore, the prevalences of high BP, high TG, low HDL of our results seem to have been overestimated.
The discrepancies of the prevalence of the metabolic syndrome in Korean adults were mainly caused by the criteria of high BP and dyslipidemia, especially the low HDL cholesterol level of the NCEP criteria. The prevalence of high BP as defined by the NCEP criteria in this study was about 1.5 times that of the WHO criteria. The mean level of HDL cholesterol in this study was 44 mg/dL in men and 51 mg/dL in women, which is the same as the results of a nationwide survey.17 In the US, the mean level of HDL cholesterol was 45 mg/dL in men and 55 mg/dL in women. So, the cut-off value to define low HDL cholesterol (40 mg/dL in men and 50 mg/dL in women) in the NCEP criteria is reasonable in the US, but is higher than the general population in Korea, especially in women. So, in the KNHANES study, the prevalence of the metabolic syndrome was higher than that of American whites.17
3.5% of women and 5.1% of men had metabolic syndrome according to the WHO criteria, but not according to the NCEP criteria. These subjects were more insulin resistant (HOMA-IR 4.4 ± 1.5 vs. 2.7 ± 5.5), had higher fasting glucose (6.0 ± 1.6 vs. 5.4 ± 1.1 mmol/L), were more obese (BMI 27.1 ± 2.7 vs. 25.8 ± 2.7 kg/m2), had lower triglycerides (1.9 ± 1.3 vs. 2.6 ± 1.6 mmol/L) and higher HDL cholesterol (1.4 ± 0.4 vs. 1.0 ± 0.2 mmol/L) than subjects of the metabolic syndrome with the NCEP criteria only.
We acknowledge some limitations of this study. We did not check urine albumin concentrations. By urine stick test, the prevalence of albuminuria above one positive was 2.4% of the total subjects. We excluded microalbuminuria from the criteria of the metabolic syndrome because of the low prevalence of microalbuminuria in other studies. Nevertheless, microalbuminuria has been a strong predictor of cardiovascular morbidity and mortality in several studies.11,21-23 We assessed glucose tolerance by only fasting plasma glucose, and did not perform an oral glucose tolerance test. Because of diagnostic discrepancy between fasting glucose and oral glucose tolerance test, IGT and type 2 diabetic patients may have been underestimated in this study.
We also acknowledge that these study subjects were older and more obese than the general population in Korea. The prevalence of the metabolic syndrome in this study population may therefore have been slightly overestimated.
In conclusion, the metabolic syndrome is seen in about 20 - 40% of Korean adults. Its prevalence has varied widely according to the criteria of its definition. Thus, further studies are necessary to define the criteria of the metabolic syndrome in Korean adults.
ACKNOWLEDGEMENTS
We are deeply grateful for the cooperation of the subjects who participated in this study. We thank the Korea Association of Health for their help and support in collecting the data for this manuscript.
References
- 1.Reaven GM. Role of insulin resistance in human disease. Diabetes. 1988;37:1595–1607. doi: 10.2337/diab.37.12.1595. [DOI] [PubMed] [Google Scholar]
- 2.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus, provisional report of a WHO consultation. Diabet Med. 1998;15:539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 3.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2496. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 4.Deurenberg-Yap M, Chew SK, Deureberg P. Elevated body fat percentage and cardiovascular risks at low body mass index levels among Singaporean Chinese, Malays and Indians. Obes Rev. 2002;3:209–215. doi: 10.1046/j.1467-789x.2002.00069.x. [DOI] [PubMed] [Google Scholar]
- 5.Deurenberg P, Deurenberg-Yap M, Guricci S. Asians are different from Caucasians and from each other in their body mass index/body fat percent relationship. Obes Rev. 2002;3:141–146. doi: 10.1046/j.1467-789x.2002.00065.x. [DOI] [PubMed] [Google Scholar]
- 6.Gurrici S, Hartriyanti Y, Hautvast JG, Deurenberg P. Relationship between body fat and body mass index: differences between Indonesians and Dutch Caucasians. Eur J Clin Nutr. 1998;52:779–783. doi: 10.1038/sj.ejcn.1600637. [DOI] [PubMed] [Google Scholar]
- 7.Wang J, Thornton JC, Russell M, Burastero S, Heymsfield S, Pierson RN., Jr Asians have lower boy mass index (BMI) but higher percent body fat than do whites: comparisons of anthropometric measurements. Am J Clin Nutr. 1994;60:23–28. doi: 10.1093/ajcn/60.1.23. [DOI] [PubMed] [Google Scholar]
- 8.Western Pacific Regional Office of the World Health Organization, The International Obesity Task Force. Sydney: Health Communications Australia; 2000. The Asia-Pacific perspective: redefining obesity and its treatment. http://www.obesityasiapacific.com. [Google Scholar]
- 9.Liese AD, Mayer-Davis EJ, Tyroler HA, Davis CE, Keil U, Schmidt MI, et al. Familial components of the multiple metabolic syndrome: the ARIC Study. Diabetologia. 1997;40:963–970. doi: 10.1007/s001250050775. [DOI] [PubMed] [Google Scholar]
- 10.Rantala AO, Kauma H, Lilja M, Savolainen MJ, Reunanen A, Kesaniemi YA. Prevalence of the metabolic syndrome in drug-treated hypertensive patients and control subjects. J Intern Med. 1999;245:163–174. doi: 10.1046/j.1365-2796.1999.00429.x. [DOI] [PubMed] [Google Scholar]
- 11.Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24:683–689. doi: 10.2337/diacare.24.4.683. [DOI] [PubMed] [Google Scholar]
- 12.Abdul-Rahim HF, Husseini A, Bjertness E, Giacaman R, Gordon NH, Jervell J. The metabolic syndrome in the West Bank population: An urban-rural comparison. Diabetes Care. 2001;24:275–279. doi: 10.2337/diacare.24.2.275. [DOI] [PubMed] [Google Scholar]
- 13.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination survey. JAMA. 2002;287:356–359. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 14.Jee SH, Appel LJ, Suh I, Whelton PK, Kim IS. Prevalence of cardiovascular risk factors in South Korean adults: Results from the Korea Medical Insurance Corporation (KMIC) Study. Ann Epidemiol. 1998;8:14–21. doi: 10.1016/s1047-2797(97)00131-2. [DOI] [PubMed] [Google Scholar]
- 15.Kim SW, Kim JY, Kim ES, Kim YI, Lee MS, Kim HH, et al. Prevalence of insulin resistance syndrome in subjects living in Jungup district, Korea. J Korean Diabet Assoc. 1999;23:70–78. [Google Scholar]
- 16.Park JS, Park HD, Yun JW, Jung CH, Lee WY, Kim SW. Prevalence of the metabolic syndrome as defined by NCEP-ATP III among the urban Korean population. Korean J Med. 2002;63:290–298. [Google Scholar]
- 17.Kim MH, Kim MK, Choi BY, Shin YJ. Prevalence of the metabolic syndrome and its association with cardiovascular diseases in Korea. J Korean Med Sci. 2004;19:195–201. doi: 10.3346/jkms.2004.19.2.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park HS, Oh SW, Cho SI, Choi WH, Kim YS. The metabolic syndrome and associated lifestyle factors among South Korean adults. Int J Epidemiol. 2004;33:328–336. doi: 10.1093/ije/dyh032. [DOI] [PubMed] [Google Scholar]
- 19.Haffner SM, Miettinen H, Stern MP. The homeostasis model in the San Antonio Heart Study. Diabetes Care. 1997;20:1087–1092. doi: 10.2337/diacare.20.7.1087. [DOI] [PubMed] [Google Scholar]
- 20.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low density lipoprotein cholesterol in plasma without use of preparative ultracentrifugation. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 21.Borch-Johnsen K, Feldt-Rasmussen B, Strandgaard S, Schroll M, Jensen JS. Urinary albumin excretion: an independent predictor of ischemic heart disease. Arterioscler Thromb Vasc Biol. 1999;19:1992–1997. doi: 10.1161/01.atv.19.8.1992. [DOI] [PubMed] [Google Scholar]
- 22.Dinneen SF, Gerstein HC. The association of microalbuminuria and mortality in non-insulin-dependent diabetes mellitus: a systematic overview of the literature. Arch Intern Med. 1997;157:1413–1418. [PubMed] [Google Scholar]
- 23.Kim YI, Kim C-H, Choi CS, Chung YE, Lee MS, Lee SI, et al. Microalbuminuria is associated with the insulin resistance syndrome independent of hypertension and type 2 diabetes in the Korean population. Diabetes Res Clin Pract. 2001;52:145–152. doi: 10.1016/s0168-8227(01)00228-5. [DOI] [PubMed] [Google Scholar]