Abstract
Epidemiologic studies have suggested the association between environmental exposure to volatile organic compounds (VOCs) and polycyclic aromatic hydrocarbons (PAHs) and the increased risk of incurring asthma. Yet there is little data regarding the relationship between personal exposure to air pollution and the incidence of asthma in children. This study was designed to evaluate the effect of exposure to air pollution on children with asthma by using exposure biomarkers. We assessed the exposure level to VOCs by measuring urinary concentrations of hippuric acid and muconic acid, and PAHs by 1-OH pyrene and 2-naphthol in 30 children with asthma and 30 children without asthma (control). The mean level of hippuric acid was 0.158 ± 0.169 µmol/mol creatinine in the asthma group and 0.148 ± 0.249 µmol/mol creatinine in the control group, with no statistical significance noted (p=0.30). The mean concentration of muconic acid was higher in the asthma group than in the control group (7.630 ± 8.915 µmol/mol creatinine vs. 3.390 ± 4.526 µmol/mol creatinine p=0.01). The mean level of urinary 1-OHP was higher in the asthma group (0.430 ± 0.343 µmol/mol creatinine) than the control group (0.239 ± 0.175 µmol/mol creatinine), which was statistically significant (p=0.03). There was no difference in the mean concentration of 2-NAP between the two groups (9.864 ± 10.037 µmol/mol in the asthma group vs. 9.157 ± 9.640 µmol/mol in the control group, p=0.96). In conclusion, this study suggests that VOCs and PAHs have some role in asthma.
Keywords: VOCs, PAHs, asthma
INTRODUCTION
The prevalence of asthma has increased worldwide while the most striking increases have come in industrialized countries during the last decades. Epidemiologic studies have suggested that environmental factors, including air pollution, play an important role in the increased prevalence of asthma. In Korea, there has also been an increase in the prevalence of asthma. In Korean children, the prevalence of asthma was 5.7% and 11% in 1983 and 1995, respectively.1
Volatile organic compounds (VOCs) are a diverse group of organic chemicals that share the property of evaporating into the atmosphere at normal room temperature. VOCs have been implicated as causative agents in asthma.2 Additionally, a reduction of PEF25-75 from 50 mg/m3 in atopic individuals exposed to VOCs was noted.3
Polycyclic aromatic hydrocarbons (PAHs) are natural components of most fossil fuels. They are formed by pyrolysis, an incomplete combustion or the high-temperature processing of organic materials such as crude oil boiling, coke production, or the production of other industrial carbon compounds. Nonoccupational epidemiologic studies have frequently shown associations between allergic responses and/or asthma with the exposure to ambient air pollutant mixtures having PAH components, including high traffic density emissions and environmental tobacco smoke (ETS).4
Urinary concentrations of hippuric and muconic acid have been considered to be biological indicators of exposure to VOCs.5-7 The levels of urinary 1-OH pyrene (1-OHP) and 2-naphthol (2-NAP) have been suggested as useful indicators of PAH exposure.8,9
There have been some epidemiologic studies concerning the association between air toxics and asthma, but there is little data regarding the relationship between asthma and personal exposure to air pollutants such as VOCs and PAHs. Therefore, this study was designed to evaluate the effect of exposure to air pollution on children with asthma by measuring exposure biomarkers.
MATERIALS AND METHODS
Subjects
The study subjects were recruited from the Pediatric Allergy Clinic at Inha University Hospital from March to August 2002. Current asthma was defined as a combination of at least one of the asthma-related symptoms (wheezing and dyspnea) and bronchial hyperresponsiveness (BHR). For those patients who could not undergo pulmonary function testing, current asthma was defined as at least one of the asthma-related symptoms and the following three criteria: 1) more than three episodes of wheezing attacks, 2) good response to bronchodilators, 3) no infiltration present on chest X-rays. Among the thirty children with asthma, there were 14 cases of mild intermittent asthma and 16 cases of mild persistent asthma. For comparison, 30 children who had no wheezing episodes or allergic disease were investigated.
We estimated the chemical exposure to VOCs and PAHs in the study subjects by urinary biomarkers and collected living environment information from their parents.
A written informed consent was obtained from each subject's family. The study was approved by the medical ethics committees of Inha University Hospital.
Methods
Measurement of VOC and PAH exposure markers
We took 40 ml of urine samples from the children with and without asthma. Urine samples were immediately frozen at -20℃ until analysis.
Urinary hippuric acid concentrations were measured by high-performance liquid chromatography (HPLC) and UV analysis (Gilson, Middleton, WI, USA). Briefly, urine samples were diluted 10 fold with distilled water. Samples were then transferred to autosampler vials and analyzed by HPLC and UV at 225 nm. Hippuric acid was separated on a 150 mm long reverse-phase column (TSK gel ODS-80TM, Tosoh, Tokyo, Japan) with 20 mM potassium phosphate buffer (pH 3.3) containing 12.5% acetonitrile.
Urinary muconic acid concentrations were measured by the method described by Lee et al.10 and modified by Rauscher et al.11 The strongly acidified urine samples had to be adjusted for the ion-exchange chromatographic clean-up procedure to a pH value of about 4.5 with a sodium hydroxide solution. Because of the resulting high ionic strength of the urine samples, some analytical procedure modifications were necessary. Only 1 mL of each sample was subjected to the solid-phase extraction procedure, using two coupled cartridges, each containing 500 mg of a strongly basic anion exchange sorbent (500 mg SAX quaternary amine). The samples were then transferred to autosampler vials and analyzed by HPLC and UV at 264 nm. A 250×4.6 mm reverse-phase column (Shoko, Kyoto, Japan) was used. The mobile phase was 1% acetic acid, 10% methanol, and 5 mM sodium acetate buffer, flowing at 1 mL/min.
The concentration of urinary 1-OHP was analyzed according to the method developed by Jongeneelen et al.12 The level of 2-NAP was analyzed using the methods of Kim et al.13 Briefly, urine samples were buffered with sodium acetate buffer and hydrolyzed enzymatically using β-glucuronidase with sulfatase activity (Sigma, St. Louis, MO, USA) for 16 hours at 37℃ in a shaking water bath. After hydrolysis, acetonitrile was added and the samples were centrifuged at 10,000g for 10 min. A high-performance liquid chromatography (HPLC) system, consisting of a pump (Waters 600E, Millipore, Milford, MA, USA), variable fluorescence detector (RF-10AxL, Shimadzu, Kyoto, Japan), an automatic injector (L-7200, Hitachi, Tokyo, Japan), and an integrator (Chromatopac C-R3A, Shimadzu, Kyoto, Japan), was used. A 150 mm long reverse-phase column (TSK gel ODS-80TM, Tosoh, Tokyo, Japan) was used for 1-OHP analysis and a 250 mm long reverse-phase column (J'sphere ODS-H80, YMC, Wilmington, NC, USA) for 2-NAP analysis. The mobile phase was 58% (v/v) acetonitrile for 1-OHP, and 38% (v/v) acetonitrile for 2-NAP. Excitation/emission wavelengths used in the detection of 1-OHP and 2-NAP were 242/388 nm and 227/355 nm, respectively.
Statistical analysis
Data were statistically analyzed using SAS v 8.1. As urinary 1-OHP and 2-NAP concentrations were log-normally distributed, geometric means and geometric standard deviations were presented. Group differences in the concentration of hippuric acid, muconic acid, 1-OHP, and 2-NAP were tested via the Mann-Whitney test.
RESULTS
Environmental factors
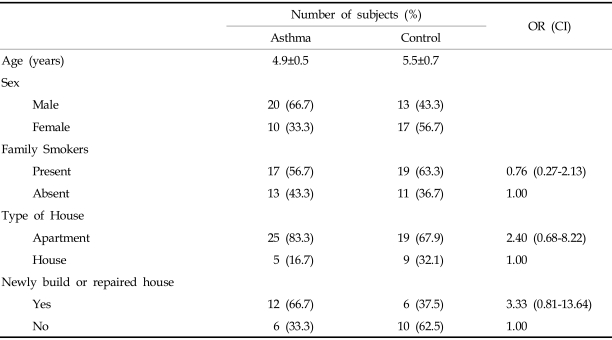
The mean age of the asthma subjects was 4.9 ± 0.5 years and that of controls was 5.5 ± 0.7 years (Table 1). There was no significant difference in the number of family members who smoked between the two groups (OR 0.76, 95% CI 0.27-2.13, Table 1). Children living in apartments had higher rates of asthma than children living in houses; however, this finding was not statistically significant (OR 2.4, 95% CI 0.68-8.22). Living in a newly built or repaired house within 1 year of completion was not a significant risk factor for having asthma (OR 3.33, 95% CI 0.81-13.64).
Table 1.
Characteristics and Environment of Study Subjects
OR, odds ratio; CI, 95% confidence interval.
Levels of VOC exposure marker
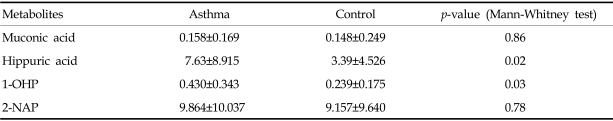
The mean level of hippuric acid was 0.158 ± 0.169 µmol/mol creatinine in children with asthma and 0.148 ± 0.249 µmol/mol creatinine in the control group, with no statistical significance noted (p=0.86). The mean concentration of muconic acid was 7.630 ± 8.915 µmol/mol creatinine and 3.390 ± 4.526 µmol/mol creatinine in children with and without asthma, respectively. There was a significant difference in the mean concentration of muconic acid between the two groups (p=0.02, Table 2)
Table 2.
Geometric Means (Geometric Standard Deviations) of Pollutant Metabolites (Unit: µmol/mol creatinine)
1-OHP, 1-OH-pyrene; 2-NAP, 2-naphthol.
Levels of PAH exposure marker
The mean level of urinary 1-OHP was significantly higher in the asthma group (0.430 ± 0.343 µmol/mol creatinine) than the control group (0.239 ± 0.175 µmol/mol creatinine, p=0.03, Table 2). The mean concentration of 2-NAP was 9.864 ± 10.037 µmol/mol creatinine and 9.157 ± 9.640 µmol/mol creatinine in the children with and without asthma, respectively. There was no significant difference for the mean level of 2-NAP between the two groups (p=0.78, Table 2).
DISCUSSION
The prevalence of asthma has been steadily increasing since the mid-1970s. Many studies have suggested that multiple factors including the westernized style of housing, increased exposure to house dust mites, immunization with vaccines, changing patterns of infection, dietary changes, and increasing levels of air pollution play important roles in the increasing prevalence of asthma.
In this study, the concentration of urinary muconic acid was higher in the asthma group than the control group. The urinary level of muconic acid represents exposure to VOCs like benzene.14 Sources of VOCs from indoor air include paints, cosmetics, adhesives, building materials, furnishings, dry-cleaned clothes, cleaning agents, carpets, and cigarettes.15 One common indoor air pollutant high in PAHs is environmental tobacco smoke (ETS). ETS also contains other toxic air pollutants that make it difficult to ascribe its effects to any one pollutant. Vehicle traffic and industrial emissions are also major sources of outdoor VOCs.14 Our results showed no difference in the presence of family members who smoked between asthma and control groups, although some studies do support the association between ETS and acute exacerbations of asthma in asthmatic children.16,17 A possible explanation to this finding is that family members who smoke might not smoke in the presence of their children or within their house. The mean age of our study subjects was 5 years. Children of preschool age usually spend much of their time indoors. Thus, the increased level of muconic acid in asthmatics in our data was probably due to increased VOC exposure in their residences. An association between indoor home VOCs and asthma has been shown in the European Community Respiratory Health Survey.18 This study reported that the prevalence of asthma was greater for newly painted homes (OR 1.5 95% CI 1.0-2.4), which is consistent with the considerable differences in VOCs.18 Our data showed that living in a newly built or repaired house within 1 year of completion was a risk factor for having asthma (OR 3.33, 95% CI 0.81-13.64), although this was not statistically significant. Unfortunately, our limited sample size reduced our ability to detect significant differences if they were present.
An epidemiologic study that was done via a survey of students 13-14 years of age showed the self-reported asthma prevalence was higher in schools with higher VOCs.19 Other risk factors, including aeroallergens, were not controlled for in this study. The researchers at Kanwha Valley, West Virginia surveyed 74 elementary school students in and outside of the valley and measured VOCs of elementary schools.2 Higher VOC concentrations were found in the valley than outside of the valley. The cross-sectional results showed that children in the valley had higher rates of physician-diagnosed asthma (OR 1.27 95% CI 1.09-1.48).
Human experimental and epidemiologic studies regarding the effects of VOCs on nonoccupational asthma are limited, and there are still few studies on the mechanism of VOC-induced asthma. According to some studies, there were no significant changes in bronchial hyperreactivity following exposures to VOCs.3,18,20 The suggested possible mechanisms are that VOCs effect asthma via neurogenic inflammation through irritant-induced induction of the inflammatory mediators.21,22
Our data showed that increased urinary levels of 1-OHP were noted in asthma subjects. Urinary 1-OHP and 2-NAP levels have been suggested to be useful indicators of PAH exposure.8 Vehicle traffic emissions, industrial emissions, and cigarette smoke are major sources of VOCs and PAHs.14 The epidemiologic results showing associations between ETS, traffic-related exposures, and childhood asthma may be partially explained by PAHs.4 Experimental evidence indicates that airborne PAH exposure linked to diesel exhaust particles (DEPs) enhance immunological responses to allergens and induce inflammatory reactions in the airways.23-25
There are several limitations of this study including small sample size, unmeasured indoor VOCs, PAHs, and aeroallergens, and lack of data for traffic density near the residence. Therefore, we could not make any conclusions as to whether the increased air pollution metabolites in children with asthma were due to high levels of indoor air pollutants, including building materials, or if this was due to traffic-related exposures due to living near a high volume of traffic. However, we did find a relation between asthma and exposure to VOCs and PAHs. To our knowledge, there are few studies on the relationship between asthma and air pollutants like VOCs and PAHs that have used exposure biomarkers. The results of our study cannot determine whether the effect of exposure to air pollutants aggravates asthma symptoms in asthma patients or whether they induce asthma in susceptible persons.
In conclusion, our study suggests that VOCs and PAHs have some role in asthma. Additional research is needed to investigate the mechanisms of association between VOCs, PAHs, and asthma.
Footnotes
This study was supported by the Ministry of Health and Welfare, South Korea (grant NO 02-PJ1-PG1-CH03-0001).
References
- 1.Pyun BY. New point of view in guidelines of pediatric asthma 2003. Pediatr Allergy Respir Dis (Korea) 2003;13(Suppl 1):S27. [Google Scholar]
- 2.Ware JH, Spengler JD, Neas LM, Samet JM, Wagner GR, Coultas D, et al. Respiratory and irritant health effects of ambient volatile organic compounds. The Kanawha County Health Study. Am J Epidemiol. 1993;137:1287–1301. doi: 10.1093/oxfordjournals.aje.a116639. [DOI] [PubMed] [Google Scholar]
- 3.Pappas GP, Herbert RJ, Henderson W, Koenig J, Stover B, Barnhart S. The respiratory effects of volatile organic compounds. Int J Occup Environ Health. 2000;6:1–8. doi: 10.1179/oeh.2000.6.1.1. [DOI] [PubMed] [Google Scholar]
- 4.Delfino RJ. Epidemiologic evidence for asthma and exposure to air toxics: Linkages between occupational, indoor, and community air pollution research. Environ Health Perspect. 2002;110(Suppl 4):573–589. doi: 10.1289/ehp.02110s4573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cok I, Dagdelen A, Gokce E. Determination of urinary hippuric acid and o-cresol levels as biological indicators of toluene exposure in shoe-workers and glue sniffers. Biomarkers. 2003;8:119–127. doi: 10.1080/1354750031000119398. [DOI] [PubMed] [Google Scholar]
- 6.Wiwanitkit V, Suwansaksri J, Srita S, Fongsoongnern A. High levels of hippuric acid in the urine of Thai press workers. Southeast Asian J Trop Med Public Health. 2002;33:624–627. [PubMed] [Google Scholar]
- 7.Cocco P, Tocco MG, Ibba A, Scano L, Ennas MG, Flore C, et al. trans,trans-Muconic acid excretion in relation to environmental exposure to benzene. Int Arch Occup Environ Health. 2003;76:456–460. doi: 10.1007/s00420-002-0413-6. [DOI] [PubMed] [Google Scholar]
- 8.Heminki K, Dickey C, Karlsson S, Bell D, Hsu Y, Tsai WY, et al. Aromatic DNA adducts in foundry workers in relation to exposure, life style and CYP1A1 and glutathione trasferase M1 genotype. Carcinogenesis. 1997;18:345–350. doi: 10.1093/carcin/18.2.345. [DOI] [PubMed] [Google Scholar]
- 9.Kim H, Cho SH, Kang JW, Kim YD, Nam HM, Lee CH, et al. Urinary 1-hydroxypyrene and 2-naphthol concentrations in male Koreans. Int Arch Occup Environ Health. 2001;74:59–62. doi: 10.1007/s004200000193. [DOI] [PubMed] [Google Scholar]
- 10.Lee BL, New AL, Kok PW, Ong HY, Shi CY, Ong CN. Urinary trans,trans-muconic acid determined by liquid chromatography: application in biological monitoring of benzene exposure. Clin Chem. 1993;39:1788–1792. [PubMed] [Google Scholar]
- 11.Rauscher D, Popp W, Muller G, Angerer J, Norpoth K. Concentrations of benzene in blood and S-phenylmercapturic and t,t-muconic acid in urine in car mechanics. Int Arch Occup Environ Health. 1994;66:1–6. doi: 10.1007/BF00386572. [DOI] [PubMed] [Google Scholar]
- 12.Jongeneelen FJ, Anzion RBM, Henderson PT. Determination of hydroxylated metabolites of polycyclic aromatic hydrocarbons in urine. J Chromatogr. 1987;413:227–232. doi: 10.1016/0378-4347(87)80230-x. [DOI] [PubMed] [Google Scholar]
- 13.Kim H, Kim YD, Lee H, Kawamoto T, Yang M, Katoh T. Assay of 2-naphthol in human urine by high-performance liquid chromatography. J Chromatogr B Biomed Sci Appl. 1999;734:211–217. doi: 10.1016/s0378-4347(99)00350-3. [DOI] [PubMed] [Google Scholar]
- 14.Saieva C, Tumino R, Masala G, Frasca G, Salvini S, Giurdanella MC, et al. Urinary 1-hydroxypyrene and t, t-muconic acid as biomarkers of exposure to environmental pollutants in two areas in Italy (EPIC-Florence and Ragusa) Tumori. 2003;89:679–686. doi: 10.1177/030089160308900612. [DOI] [PubMed] [Google Scholar]
- 15.Samet JM, Marnury MC, Spengler JD. Health effects and sources of indoor air pollution. Part II. Am Rev Respir Dis. 1988;137:221–242. doi: 10.1164/ajrccm/137.1.221. [DOI] [PubMed] [Google Scholar]
- 16.Strachan DP, Cook DG. Health effects of passive smoking: Parental smoking and childhood asthma: longitudinal and case-control studies. Thorax. 1998;53:204–212. doi: 10.1136/thx.53.3.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwartz J, Timonen KL, Pekkanen J. Respiratory effects of environmental tobacco smoke in a panel study of asthmatic and symptomatic children. Am J Respir Crit Care Med. 2000;161:802–806. doi: 10.1164/ajrccm.161.3.9901002. [DOI] [PubMed] [Google Scholar]
- 18.Wieslander G, Norback D, Bjornsson E, Janson C, Boman G. Asthma and the indoor environment: the significance of emission of formaldehyde and volatile organic compounds from newly painted surfaces. Int Arch Occup Environ Health. 1997;69:115–124. doi: 10.1007/s004200050125. [DOI] [PubMed] [Google Scholar]
- 19.Smedje G, Norback D, Edling C. Asthma among secondary school children in relation to the school environment. Clin Exp Allergy. 1997;27:1270–1278. [PubMed] [Google Scholar]
- 20.Molhave L, Bach B, Peterson F. Human reaction to low concentrations of volatile organic compounds. Environ Int. 1986;12:167–175. [Google Scholar]
- 21.Meggs WJ. Neurogenic inflammation and sensitivity to environmental chemicals. Environ Health Perspect. 1993;101:234–238. doi: 10.1289/ehp.93101234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Thoracic Society Workshop. Immunobiology of asthma and rhinitis. Pathogenic factors and therapeutic options. Am J Respir Crit Care Med. 1999;160(5 part 1):1778–1787. doi: 10.1164/ajrccm.160.5.ats7-99. [DOI] [PubMed] [Google Scholar]
- 23.Diaz-Sanchez D. The role of diesel exhaust particles and their associated polyaromatic hydrocarbons in the induction of allergic airway disease. Allergy. 1997;52(Suppl):52–58. doi: 10.1111/j.1398-9995.1997.tb04871.x. [DOI] [PubMed] [Google Scholar]
- 24.Ma JY, Ma JK. The dual effect of the particulate and organic components of diesel exhaust particles on the alteration of pulmonary immune/inflammatory responses and metabolic enzymes. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 2002;20:117–147. doi: 10.1081/GNC-120016202. [DOI] [PubMed] [Google Scholar]
- 25.Nel AE, Diaz-Sanchez D, Ng D, Hiura T, Saxon A. Enhancement of allergic inflammation by the interaction between diesel exhaust particles and the immune system. J Allergy Clin Immunol. 1998;102:539–554. doi: 10.1016/s0091-6749(98)70269-6. [DOI] [PubMed] [Google Scholar]