Abstract
Rural women have among the highest rates of obesity and sedentary lifestyle, yet few studies have examined strategies for delivering state-of-the-art obesity treatment to hard-to-reach rural areas. The purpose of this pilot trial was to examine the impact and cost-effectiveness of a 6-month behavioral weight loss program delivered to rural women by phone either one-on-one with a counselor or to a group via conference call. Thirty-four rural women (mean BMI=34.4, SD=4.6) were randomized to group phone-based treatment or individual phone-based treatment. Completers analysis showed that weight loss was greater in the group condition (mean=14.9 kg=, SD=4.4) compared to the individual condition (mean=9.5 kg, SD=5.2; p=.03). Among the total sample, 62% of participants in the group condition achieved the 10% weight loss goal compared to 50% in the individual condition, and group treatment was found to be more cost-effective. Future research is warranted to examine the benefits of group phone-based treatment for long-term management of obesity among rural populations.
Keywords: obesity treatment, rural, phone counseling, group treatment
1. Introduction
Rural populations suffer from health disparities as evidenced by higher premature mortality rates, poorer access to healthcare, and poorer lifestyle behaviors, including higher rates of obesity and physical inactivity compared with their non-rural counterparts (Eberhardt & Pamuk, 2004; National Center for Health Statistics, 2001). In addition, rural women in particular suffer from higher rates of stress and depressive symptoms (Hauenstein & Boyd, 1994) which are established risk factors for weight regain (Byrne, 2002; Elfhag & Rossner, 2005). As a result, women of the most rural counties have the highest prevalence of obesity, with rates 1.6 times greater than suburban women (Sobal, Troiano, & Frongillo, 1996).
State-of-the-art behavioral obesity interventions are limited in rural areas. On-site obesity programs have been delivered in rural primary care clinics (Ely et al., 2008) schools (Davis, James, Curtis, Felts, & Daley, 2008), and Cooperative Extension Offices (regional offices affiliated with land-grant universities with the mission to “extend” their resources through non-credit programs; Janicke et al., 2008; Perri et al., 2008). However, these in-person treatment delivery approaches present a barrier for many rural residents who may have long transportation distances to clinic sites, especially in frontier areas, and where availability of trained health counselors may be limited. In response to a need for alternatives to face-to-face meetings, web- and telephone-based weight control interventions have been examined. Of these, phone-based treatment appears to have the greatest reach for rural populations of whom only 53% have home internet access, the majority of which is dial-up connection with variable download time (Pew Internet and American Life Project, 2006).
Phone-based interventions are typically delivered one-on-one between a patient and provider. Group phone-based treatment is an alternative approach that holds great promise because it capitalizes on the same mechanisms of face-to-face group treatment by allowing participants to interact with each other in real time while still providing the reduced participant and provider burden with the phone treatment modality. The benefits of group treatment have been written about extensively in the psychotherapy literature and include factors such as interpersonal learning, imparting information to others, and developing optimism and hope for change (Yalom, 1995). In behavioral obesity treatment, aspects of group counseling such as support, accountability to one another, and group problem-solving are believed to be important for sustaining difficult lifestyle changes (Donnelly et al., 2007; Perri et al., 2001). Renjilian et al. found that obese women randomized to face-to-face group treatment lost significantly greater weight than those randomized to face-to-face individual treatment, regardless of their expressed preference for individual or group counseling (Renjilian et al., 2001). However, it is unknown whether or not group treatment is more effective than individual treatment when delivered by phone. Treatment processes such as the counseling relationship and effective problem-solving may differ when interaction is limited to phone contact.
The purpose of this pilot study was to examine the effects of a behavioral weight loss program delivered to rural women in two formats: individual phone counseling and group phone counseling. It was hypothesized that group treatment would result in greater weight loss and improvements in diet and physical activity behaviors compared to individual treatment. We also explored psychosocial treatment process variables that may influence the effectiveness of group and individual phone-based treatment (i.e., development of problem-solving skills, working relationship between counselor and participant, and match or mismatch with participants’ stated baseline preference for individual or group treatment) as well as the cost-effectiveness of the two approaches.
2. Method
2.1. Participants and randomization
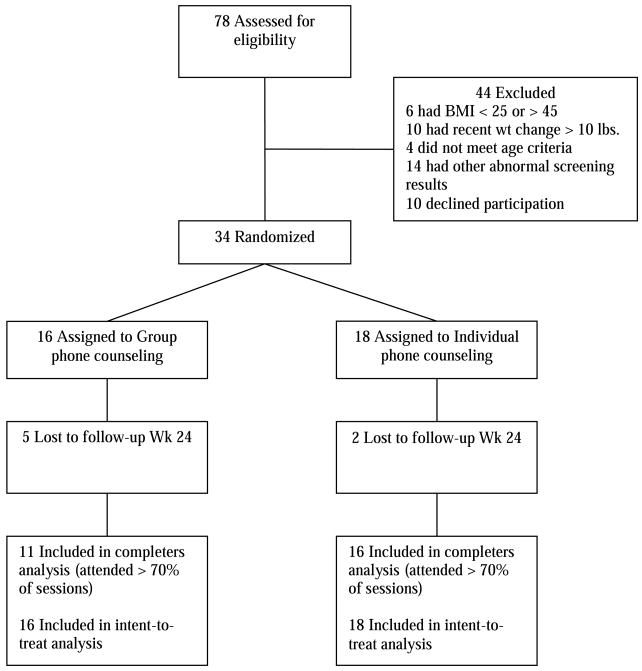
Women were recruited from seven non-metropolitan counties in Kansas using flyers, a staffed table at a local women’s health fair, and by word of mouth. A participant flow diagram is shown in Fig. 1. Eligibility criteria were 1) age 22–65 years, 2) female, 3) residence in a rural area defined Census Bureau as outside urban areas with 10,000 or more people (US Department of Agriculture, 2009), 4) BMI between 25 and 44.9 kg/m2, 5) English-speaking, 6) weight stable (no more than 10 lb weight fluctuation within previous 6 months), 7) not pregnant during previous six months, lactating, currently pregnant, or planning to become pregnant, 8) free from serious medical risk such as unstable cardiac condition, congestive heart failure, recent cancer treatment, or severe pulmonary disease, 9) able to walk briskly unassisted for at least 10 min, 10) free from substance abuse (2-item Conjoint Screener score=2; Brown, Leonard, Saunders, & Papasouliotis, 2001), depression (CES-D score >20; Hann, Winter, & Jacobsen, 1999), or binge eating disorder (Binge Eating Scale score ≥27; Gormally, Black, Daston, & Rardin, 1982), 11) working cell or home phone number, 12) no special dietary restrictions (e.g. vegetarian), and 13) able to obtain clearance to participate from a primary care provider who verified medical risk exclusion criteria. Participants were randomized sequentially using a closed envelope procedure that was created by a study statistician and concealed from the investigators and data collection staff until after baseline data collection. The study was approved by the Human Subjects Committee at the University of Kansas Medical Center.
Fig. 1.
Flow of participants.
2.2. Behavioral weight control intervention
The intervention targeted 10% weight loss over a 6-month period in accordance with NHLBI guidelines (1998). Both treatment arms received weekly treatment sessions for 16 weeks followed by 4 biweekly sessions. The intervention was guided by Social Cognitive Theory (Bandura, 1986) and focused on self-efficacy and self-regulation skills, including goal-setting, self-monitoring, problem-solving, stimulus control, and relapse prevention for diet and physical activity (PA) behaviors. Participants were instructed to turn in diet and PA self-monitoring logs twice per week, by phone or email. Weekly sessions began with a review of the participants self-monitoring logs, followed by questions and problem-solving, and ended with a weekly educational topic on nutrition, PA, or cognitive and behavioral strategies for sustaining lifestyle change.
Participants were instructed to follow a 1200 to 1500 kcal diet with <25%kcal from fat. To facilitate adherence to the diet and promote experiential learning of appropriate portion sizes, participants were provided with prepackaged entrees (two per day at <300 kcal each) and shakes (three per day at 100–110 kcal each; Health Management Resources, Inc.), shipped directly to their home bi-weekly for the first 16 weeks of the intervention. Participants were instructed to add ≥5 FV servings per day and calorie-free beverages. Prepackaged meals have consistently shown greater weight loss and weight loss maintenance compared to traditional diets that rely on individuals assembling their own meals (Ashley, St. Jeor, Perumean-Chaney, Schrage, & Bovee, 2001; Heymsfield, van Mierlo, van der Knaap, Heo, & Frier, 2003; LeCheminant, Jacobsen, Hall, & Donnelly, 2005; Wing et al., 1996) as well as greater increases in FVs and fiber, greater decrease in fat intake,(Ashley et al., 2001; Jeffery et al., 1993; McCarron et al., 1997; Metz et al., 2000; Noakes, Foster, Keogh, & Clifton, 2004; Pi-Sunyer et al., 1999) and greater adherence to weight management programs (Jeffery et al., 1993; Wing et al., 1996). For weeks 16 to 24, participants received a weight loss calorie goal based on the Harris-Benedict calculation of their current energy needs. They were encouraged to purchase and consume two commercially available prepackaged meals per day, along with ≥5 FV servings, and one home-prepared meal. Participants were also instructed to gradually increase their PA over the first 12 weeks to 300 min per week (60 min/day, 5 days/week) of moderate intensity activity, consistent with national PA guidelines for weight loss maintenance (Donnelly et al., 2009; Haskell et al., 2007).
2.1.1. Group and individual phone counseling
The format and content of sessions were the same for both conditions, and all participants were instructed to treat weekly calls as a standing appointment time when they needed to be in a private location free from distractions. The group condition consisted of one treatment group of 16 women. Women in the group condition called into a toll-free conference call number, whereas women in the individual condition received calls from their counselor. Participants in the individual condition were allowed to reschedule sessions if they contacted their counselor prior to their scheduled appointment time. Calls were approximately 60 min for group sessions and 25–45 min for individual sessions.
Group sessions were structured to allow all participants opportunity to contribute and to help ensure that they were actively listening. Ground rules included no multi-tasking while on the call and being in a location free from distractions and background noise. Each session began with an open-ended check-in question relevant to the previous session’s topic to which each participant responded in order of their choosing. The counselor called on participants by name throughout the sessions to ensure active participation. Norms were also encouraged for participants to speak directly to one another.
A trained masters-level dietitian and two advanced doctoral students in clinical psychology with experience in weight control intervention provided the counseling using the same standardized treatment manual for both treatment conditions. The counselor for the group condition also provided treatment for participants in the individual condition. To maximize treatment fidelity, all counseling sessions were audio-taped, and 25% of tapes were randomly selected and reviewed during weekly supervision. A standardized checklist for each session guided supervision and was used to rate the extent to which counselors adhered to the treatment manual.
2.3. Measures
Data collection occurred at baseline, week 16, and week 24 during in-person visits at a Cooperative Extension Office facility in the county where the majority of participants resided. All data collection appointments were scheduled in the morning, and participants were instructed to refrain from breakfast until after their official weigh-in.
2.3.1. Weight and height
Participants were weighed without shoes in light clothing (shorts and t-shirt) to the nearest 0.1lb using a digital scale (Befour, Inc). Height was measured without shoes and rounded to the nearest 0.1 cm. Height and weight measurements were used to calculate BMI.
2.3.2. Dietary intake
Two 24-hour dietary recalls were conducted at each time period using the USDA multiple-pass approach (Conway, Ingwersen, Vinyard, & Moshfegh, 2003). Trained data collectors recorded specific and quantitative detail of every food and drink consumed during the previous day and entered them into the Nutrition Data System for Research (NDS-R) software. The first recall occurred in-person and incorporated food models, containers, and charts to assist participants with estimating portion size. Participants received a copy of the food charts to take home, and the second recall occurred by phone within a seven day period. The two recalls included one week day and one weekend day, and participants were not informed of when they would be called. Outcome variables included daily kcals, percent kcals from fat, and daily FV servings (excluding fried potatoes and fruit juice).
2.3.3. Physical activity
The Minnesota Physical Activity Questionnaire assesses weekly frequency and duration of 41 physical activities, including sports and lifestyle activities (Richardson, Leon, Jacobs, Ainsworth, & Serfass, 1994). Scoring yields estimates of energy expenditure (kcal/week) (Montoye, Kemper, Saras, & Washburn, 1996). Because the intervention targeted planned physical activity, lifestyle activities involving housework and gardening were not included in the scoring.
2.3.4. Psychosocial measures
Exploratory psychosocial treatment process measures included self-efficacy, problem-solving ability, and working relationship with their counselor. The Weight Efficacy Lifestyle Questionnaire (WEL) assessed self-efficacy for restricting eating in 20 high-risk situations (e.g., “when I am watching T.V.,” and “even when I am at a party;” Clark, Abrams, Niaura, Eaton, & Rossi, 1991). The WEL has adequate internal consistency (alpha=.70 to .90) and has shown significant increases over time in behavioral obesity treatment studies (Clark et al., 1991). A 5-item measure was used to assess self-efficacy for participating in regular exercise when faced with common barriers (e.g., “when I feel I don’t have the time;” Marcus, Selby, Niaura, & Rossi, 1992). Internal consistency for this measure has been .76 to .80 (Marcus et al., 1992; Purath & Miller, 2005). Problem-solving orientation and problem-solving skills were assessed with the 25-item Social Problem Solving Inventory (SPSI; D’Zurilla, Nezu, & Maydeu-Olivares, 2002). The SPSI instructions were adapted to direct participants to answer the questions regarding how they typically deal with problems specific to their weight management. Sample items for problem-solving orientation and problem-solving skills, respectively, include “Whenever I have a problem, I believe that it can be solved,” and “When I have a decision to make, I try to predict the positive and negative consequences of each option.” The sub-scales and overall score for the SPSI have good internal consistency (alpha=.79 to .93) and 3-week test–retest reliability (r=.72 to .84), and the measure has been shown to be sensitive to the effects of training in problem-solving interventions (D’Zurilla et al., 2002). The 12-item Working Alliance Inventory (Horvath & Greenberg, 1989) was used to assess participants’ working relationship with their counselor. Three subscale scores assess agreement on goals (“We have established a good understanding of the kind of changes that would be good for me”), agreement on how to achieve those goals (“We agree on what is important for me to work on”), and personal bond (“I am confident in my counselor’s ability to help me”). The subscales and composite scale of the WAI have good internal consistency (Cronbach alpha=.83 to .98; Tracey & Kokotovic, 1989), and client’s ratings on the WAI have correlated significantly with client-reported outcome in short-term psychotherapy (Horvath & Greenberg, 1989). Finally, we also assessed participants’ preference for individual or group treatment at baseline to explore whether match or mismatch to treatment preference influenced outcome.
2.3.5. Costs
Exploratory analyses of costs included the perspective of both the participants and the program. We assessed only variable costs that we expected to differ across treatment arms. Participant costs included value of time spent in session. Time data was derived from electronic recordings of all sessions and was valued as the average wage reported by participants ($12.50/h). We assumed each participant completed the average time in session. Program costs included provider time in preparation and record keeping, provider time in session, and phone charges. Provider time was valued as the average national wage from the Bureau of Labor Statistics for dietitians and all masters-level counselors ($21.81/h). Phone charges included long-distance fees for individual calls ($.03/min) and conference call charges for group calls ($.07/min/participant). Cost-effectiveness for each treatment arm was calculated as costs divided by the percentage of participants who achieved the recommended 10% weight loss (NHLBI, 1998). Cost-effectiveness was calculated from both a program perspective and a program plus participant perspective.
2.4. Statistical analyses
Baseline differences between treatment conditions and between completers and drop-outs were tested using two-sample t-tests and chi-square analyses. Effects of treatment on outcomes were analyzed using 2 (treatment conditions)×3 (time periods) repeated measures MANOVAs with follow-up univariate ANOVAs and pairwise comparisons. Analyses were conducted for both completers only and the total sample (intent-to-treat with missing data imputed as no change from baseline).
3. Results
Thirty-four women were enrolled and randomized to group counseling by phone (n=16) or individual counseling by phone (n=18). Retention was not significantly different for group and individual conditions; 85.3% of participants completed assessments at Week 16 and 79.4% at Week 24 (see Fig. 1). Completers were defined as women who attended at least 70% of treatment sessions and completed at least one follow-up assessment. Compared to drop-outs, completers were significantly older (M=51.0, SD=9.4 years vs. M=30.6, SD=4.8 years, p<.01). No other significant differences in baseline characteristics were found between completers and drop-outs.
Participants were on average 48.0±11.5 years old and had a mean BMI of 34.4 (SD=4.6. No significant differences in baseline characteristics were found across conditions (see Table 1).
Table 1.
Baseline participant characteristics.
| Characteristic | Group | Individual | Total |
|---|---|---|---|
| (n=16) | (n=18) | (n=34) | |
| Age, M (SD) | 47.6 (12.5) | 48.4 (10.9) | 48.0 (11.5) |
| Education, n (%) | |||
| H.S. degree | 4 (25.0) | 6 (33.3) | 10 (29.4) |
| Some college | 10 (62.5) | 6 (33.3) | 16 (47.1) |
| Bachelor’s degree | 2 (12.5) | 4 (22.2) | 6 (17.6) |
| Graduate degree | 0 (0) | 2 (11.2) | 2 (5.9) |
| Marital status, n (%) | |||
| Married | 13 (81.2) | 14 (77.8) | 27 (79.4) |
| Single | 0 (0) | 2 (11.1) | 2 (5.9) |
| Divorced/widowed | 3 (18.7) | 2 (11.1) | 5 (14.7) |
| Employment status, n (%) | |||
| Employed full-time | 12 (75.5) | 15 (83.3) | 27 (79.4) |
| Employed part-time | 2 (12.5) | 1 (5.6) | 3 (8.8) |
| Not employed | 0 (0) | 1 (5.6) | 1 (2.9) |
| Retired | 2 (12.5) | 1 (5.6) | 3 (8.8) |
| Weight, kg | 95.7 (13.7) | 90.5 (13.7) | 92.9 (13.7) |
| BMI | 35.8 (4.7) | 33.2 (4.2) | 34.4 (4.6) |
Attendance rates to treatment sessions were marginally greater for individual compared to group (including drop-outs, M=88% and 74% of sessions, respectively, p=.08; excluding drop-outs, M=94% and 88%, respectively, p=.08).
3.1. Weight changes
Table 2 presents weight changes for the completers. A 2 (treatment conditions)×3 (time periods) repeated measures multivariate analysis of variance (MANOVA) indicated a significant main effect for time, F(2,24)=124.8, p<.001, partial η2=.91, and a significant treatment × time interaction, F(2,24)=3.87, p=.035, partial η2=.24. Follow-up univariate ANOVAs indicated that compared to the individual condition, participants in the group condition showed greater weight loss from Baseline to week 16 (p=.01), from Baseline to Week 24 (p=.01), and marginally greater weight loss from week 16 to week 24 (p=.10). Pairwise comparisons across time showed that both conditions had significant weight loss from baseline to week 16 (both ps<.001), but only the group condition showed significant weight loss from week 16 to week 24 (p=.009).
Table 2.
Mean net weight changes (kg) by condition for completers.
| Condition |
||||
|---|---|---|---|---|
| Group (n=11) | Individual (n=16) | |||
| Time period | M | SD | M | SD |
| Baseline–Week 16 | −13.54a | 3.83 | −9.24b | 3.93 |
| Week 16–Week 24 | −1.37 | 1.62 | −0.29 | 1.58 |
| Baseline–Week 24 | −14.91a | 4.44 | −9.53b | 5.20 |
Means with different subscripts indicate significant between-group differences, p<.01.
For the total sample, assuming no weight change for missing data, repeated measures MANOVA indicated a significant main effect for time, F(2,31)=35.60, p<.001; the main effect for treatment and the interaction effect for treatment × time were not significant. For the group versus individual conditions, weight loss from baseline to Week 24 was 10.1 kg (SD=8.2) vs. 8.3 kg (SD=6.0), respectively. Among the total sample, 62% of group participants achieved the clinical recommendation of 10% weight loss, compared to 50% of individual participants.
3.2. Diet, physical activity, and psychosocial outcomes
We also explored potential dietary, physical activity, and psychosocial contributors to the differences in weight loss between completers in the group and individual conditions. For dietary and physical activity measures, repeated measures MANOVAs showed main effects for time, but no significant interaction effects for treatment × time. From Baseline to Week 24, participants in the group and individual conditions decreased their daily caloric intake by 427kcals (SD=321) and 542kcals (SD=623), decreased their fat consumption by 12.3 % (SD=9.9) and 11.9% (SD=11.4), increased their fruit and vegetable consumption by 3.1 servings (SD=2.1) and 2.9 servings (SD=4.7), and increased their physical activity by 747 METS (SD=1149) and 508 METS (SD=782), respectively (all ps for time <.001).
Participants in group and individual conditions both showed improvements in self-efficacy for controlling diet and problem-solving skills (ps for time <.001 and .05, respectively); however, treatment× time interaction effects were non-significant. Between-subjects t-tests on participant ratings of their working relationship with their counselor (Working Alliance Inventory at Week 16) revealed that participants in the group condition evaluated their working relationship with their counselor more favorably than participants in the individual condition. Participants in the group condition reported greater agreement on goals, greater agreement on how to achieve those goals, and a stronger personal bond with their counselor (all ps<.05).
We also explored whether participants being matched to their preferred treatment modality (group versus individual) impacted weight loss. Prior to randomization, 76% of participants reported that they preferred individual treatment. Thus, 72% of participants who were randomized to individual treatment received their preferred treatment, compared to 20% of participants who were randomized to group treatment. A 2 (treatment condition)×2 (match to preference) univariate analysis of variance on weight change at Week 24 indicated a non-significant main effect for preference match and a non-significant interaction effect between treatment condition and preference match, indicating that match to treatment preference did not influence weight loss outcomes. These results were similar for both completers and intent-to-treat analyses.
3.3. Costs
Table 3 shows provider and participant costs for group and individual counseling. Individual counseling incurred higher costs for provider time in preparation/record keeping and in counseling sessions. Group counseling incurred higher costs for phone charges due to higher fees for conference call technology. Participant costs for time in session were higher for group counseling because group calls lasted on average 64 min per session compared to 34 min for individual sessions. Overall, provider and participant costs combined were lower for group counseling. Using the percentage of participants who achieved 10% weight loss in intent-to-treat analysis, cost-effectiveness from a program plus participant perspective (average cost per successful participant) was $714 for group counseling and $1029 for individual counseling. Thus, group treatment dominated individual treatment; it was less expensive and more effective.
Table 3.
Program and participant costs.
| Group (n=16) | Individual (n=18) | |
|---|---|---|
| Program costs | ||
| Preparation/record keeping, h | ||
| Total time, h | 57.4 | 98.8 |
| Per participant time, h | 3.6 | 5.5 |
| Cost per participant, $a | 78.27 | 119.73 |
| Time in counseling session | ||
| Total time, h | 23.2 | 190.5 |
| Per participant time, h | 1.4 | 10.6 |
| Cost per participant, $a | 31.67 | 230.79 |
| Phone costs | ||
| Cost per min per participant, $ | 0.07 | 0.03 |
| Total cost, $ | 1500.78 | 571.41 |
| Cost per participant, $ | 93.80 | 31.75 |
| Total program costs per participant, $ | 203.73 | 382.26 |
| Participant costs | ||
| Time in counseling session | ||
| Per participant time, h | 19.1 | 10.6 |
| Cost per participant, $b | 239.22 | 132.27 |
| Cost-effectiveness, program only, $c | 328.60 | 764.52 |
| Cost-effectiveness, program+participant, $c | 714.43 | 1029.06 |
Data are reported as mean per provider unless noted as per participant.
Cost calculated with average provider wage of $21.81/h.
Cost calculated with average participant wage of $12.50/h.
Cost-effectiveness calculated as per participant cost divided by intent-to-treat success rate of 10% weight loss (62% in group condition and 50% in individual condition).
4. Discussion
Among completers, group phone-based treatment resulted in greater weight loss than did individual treatment. The magnitude of the difference in weight loss between conditions was 5.4 kg, and the effect size was large. Among the total sample, weight loss did not statistically differ across conditions, however, the direction favored group treatment with 62% of group participants achieving the 10% weight loss goal compared to 50% in individual treatment. Given the small sample size of this pilot study, this difference is noteworthy as clinically meaningful.
This is the first examination of how group versus individual treatment compares when delivered entirely by phone, and the findings are consistent with previous findings showing superior weight loss with group compared to individual treatment when delivered in-person (Renjilian et al., 2001). Matching participants with their preferred treatment modality did not influence weight loss outcomes, consistent with previous findings showing greater weight loss with group treatment even for women who preferred individual treatment (Renjilian et al., 2001). Cost analyses further demonstrated that phone-based group treatment is a more cost-effective treatment modality than phone-based individual treatment.
Factors that contribute to better outcomes with group versus individual treatment deserve further exploration. In the current study, diet and physical activity changes did not differ across conditions in a consistent or meaningful manner. Problem-solving skills and self-efficacy likewise did not differ across conditions, however, group participants rated their relationship with their group counselor more favorably. Because the same counselor provided both individual and group treatment, this likely is not simply a counselor effect. Rather, this finding may reflect greater cohesion and perceived support in the group, both between participants and the counselor and among participants themselves. This finding was supported by follow-up process interviews during which participants in the group treatment arm indicated that group support, accountability, and information-sharing were the most helpful components of group treatment. Optimal group size for enhancing these factors in group-based obesity treatment has not been empirically demonstrated for in-person or phone-based treatment. However, based on our experience using the group phone-based approach, group sizes between 12 and 16 with a 75–80% average attendance rate provides ample opportunity for each member to participate in a meaningful manner.
The larger literature on group versus individual treatment modalities for behavioral or psychological conditions generally has shown no treatment differences. A meta-analysis of nine studies found no differences in treatment outcomes between group and individual treatment across presenting conditions and treatment approaches (Tillitski, 1990). More recent randomized studies have found no difference between group and individual cognitive behavioral treatments for insomnia (Bastien, Morin, Ouellet, Blais, & Bouchard, 2004), substance abuse (Graham, Annis, Brett, & Venesoen, 1996), chronic pain and headaches (Johnson & Thorn, 1989; Turner-Stokes et al., 2003), bulimia nervosa (Nevonen & Broberg, 2006), and other psychological conditions (Anderson & Rees, 2007; McCloskey, Noblett, Deffenbacher, Gollan, & Coccaro, 2008). Thus, the combined evidence indicates that group treatment produces at least equal outcomes as individual treatment and thus may be more cost-effective.
The results of the current study contribute to the growing body of research on how to effectively reach rural populations with weight control interventions. Both conditions in this study achieved clinically meaningful weight loss over the course of 6 months that are on par with large multisite behavioral weight control trials, and with Perri et al.’s (2008) recently completed rural weight management trial that used an in-person group approach at Cooperative Extension Offices for the initial 6-month weight loss phase. Perri et al. examined the impact of two approaches for weight loss maintenance: individual phone treatment versus in-person group treatment, both compared to an education control. They found no difference between individual phone and in-person group treatment over the course of a 12-month weight loss maintenance phase. Further research is needed to determine if the benefits of group over individual counseling diminish with longer treatment periods. Regardless, given that group phone-based treatment is more cost-effective, it is a viable alternative to individual phone-based treatment that combines the convenience of phone treatment with the benefits of group support and accountability.
Several limitations of the current study are worth noting. First, as a pilot study, the sample size did not provide desired power, however, weight outcomes showed meaningful differences across conditions with moderate to large effect sizes that were significant for completers and in the same direction for the total sample. A larger study is needed to adequately test behavioral and psychosocial factors that contribute to weight loss differences across treatment conditions. Second, the magnitude of weight loss may not generalize to programs that do not include prepackaged meals. Provision of prepackaged food is known to enhance weight loss outcomes, thus practitioners in rural settings may not achieve the same magnitude of weight loss without the resources for providing food. However, because both treatment arms were provided the same program components, this should not impact the observed effect showing better weight loss with a group phone-based approach. Third, results may not generalize to rural men. We chose to focus on rural women given their greater disparities in obesity rates. Finally, further research is needed to examine the benefits of group phone-based treatment for weight loss maintenance and long-term management of obesity.
Acknowledgments
We gratefully acknowledge the Cooperative Extension Office in Miami County, Kansas for their support of this project and the research staff who contributed to the study, with special appreciation for Heather Austin, MS, Angela Banitt, MA, and Susan Krigel, MA.
Role of funding source
Funding for this study was provided by NICHD Grant K12 HD052027. Food for the intervention was provided by Health Management Resources Corporation (HMR). NICHD and HMR had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Contributors
Dr. Befort wrote the protocol, oversaw the study procedures, and conducted the statistical analyses. Drs. Donnelly, Sullivan, Ellerbeck, and Perri contributed to the design of the study and the intervention procedures. Dr. Befort wrote the first draft of the manuscript and all authors contributed to and have approved the final manuscript.
Conflict of interest
Dr. Donnelly has received grants and products, and Dr. Befort received products for the current study, from Health Management Resources Corporation. All other authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anderson RA, Rees CS. Group versus individual cognitive–behavioural treatment for obsessive–compulsive disorder: A controlled trial. Behavior Research and Therapy. 2007;45(1):123–137. doi: 10.1016/j.brat.2006.01.016. [DOI] [PubMed] [Google Scholar]
- Ashley JM, St Jeor ST, Perumean-Chaney S, Schrage J, Bovee V. Meal replacements in weight intervention. Obesity Research. 2001;9(Suppl 4):312S–320S. doi: 10.1038/oby.2001.136. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social foundation of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- Bastien CH, Morin CM, Ouellet MC, Blais FC, Bouchard S. Cognitive–behavioral therapy for insomnia: Comparison of individual therapy, group therapy, and telephone consultations. Journal of Consulting and Clinical Psychology. 2004;72(4):653–659. doi: 10.1037/0022-006X.72.4.653. [DOI] [PubMed] [Google Scholar]
- Brown RL, Leonard T, Saunders LA, Papasouliotis O. A two-item conjoint screen for alcohol and other drug problems. Journal of the American Board of Family Practice. 2001;14(2):95–106. [PubMed] [Google Scholar]
- Byrne SM. Psychological aspects of weight maintenance and relapse in obesity. Journal of Psychosomatic Research. 2002;53:1029–1036. doi: 10.1016/s0022-3999(02)00487-7. [DOI] [PubMed] [Google Scholar]
- Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. Journal of Consulting and Clinical Psychology. 1991;59(5):739–744. doi: 10.1037//0022-006x.59.5.739. [DOI] [PubMed] [Google Scholar]
- Conway JM, Ingwersen LA, Vinyard BT, Moshfegh AJ. Effectiveness of the US Department of Agriculture 5-step multiple-pass method in assessing food intake in obese and nonobese women. American Journal of Clinical Nutrition. 2003;77(5):1171–1178. doi: 10.1093/ajcn/77.5.1171. [DOI] [PubMed] [Google Scholar]
- Davis AM, James RL, Curtis MR, Felts SM, Daley CM. Pediatric obesity attitudes, services, and information among rural parents: A qualitative study. Obesity (Silver Spring) 2008;16(9):2133–2140. doi: 10.1038/oby.2008.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Medicine and Science in Sports and Exercise. 2009;41(2):459–471. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- Donnelly JE, Smith BK, Dunn L, Mayo MM, Jacobsen DJ, Stewart EE, et al. Comparison of a phone vs clinic approach to achieve 10% weight loss. International Journal of Obesity. 2007;31(8):1270–1276. doi: 10.1038/sj.ijo.0803568. [DOI] [PubMed] [Google Scholar]
- D’Zurilla TJ, Nezu AM, Maydeu-Olivares A. Social problem-solving inventory-revised: Technical manual. North Tonawanda, NY: Multi-Health Systems; 2002. [Google Scholar]
- Eberhardt MS, Pamuk ER. The importance of place of residence: Examining health in rural and nonrural areas. American Journal of Public Health. 2004;94(10):1682–1686. doi: 10.2105/ajph.94.10.1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elfhag K, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obesity Reviews. 2005;6(1):67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- Ely AC, Banitt A, Befort C, Hou Q, Rhode PC, Grund C, et al. Kansas primary care weighs in: A pilot randomized trial of a chronic care model program for obesity in 3 rural Kansas primary care practices. Journal of Rural Health. 2008;24(2):125–132. doi: 10.1111/j.1748-0361.2008.00148.x. [DOI] [PubMed] [Google Scholar]
- Gormally J, Black S, Daston S, Rardin D. The assessment of binge eating severity among obese persons. Addictive Behavior. 1982;7(1):47–55. doi: 10.1016/0306-4603(82)90024-7. [DOI] [PubMed] [Google Scholar]
- Graham K, Annis HM, Brett PJ, Venesoen P. A controlled field trial of group versus individual cognitive–behavioural training for relapse prevention. Addiction. 1996;91(8):1127–1139. doi: 10.1046/j.1360-0443.1996.91811275.x. [DOI] [PubMed] [Google Scholar]
- Hann D, Winter K, Jacobsen P. Measurement of depressive symptoms in cancer patients: Evaluation of the Center for Epidemiological Studies Depression Scale (CES-D) Journal of Psychosomatic Research. 1999;46(5):437–443. doi: 10.1016/s0022-3999(99)00004-5. [DOI] [PubMed] [Google Scholar]
- Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Medicine and Science in Sports and Exercise. 2007;39(8):1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- Hauenstein EJ, Boyd MR. Depressive symptoms in young women of the Piedmont: Prevalence in rural women. Women’s Health. 1994;21(2–3):105–123. doi: 10.1300/j013v21n02_07. [DOI] [PubMed] [Google Scholar]
- Heymsfield SB, van Mierlo CA, van der Knaap HC, Heo M, Frier HI. Weight management using a meal replacement strategy: Meta and pooling analysis from six studies. International Journal of Obesity and Related Metabolic Disorders. 2003;27(5):537–549. doi: 10.1038/sj.ijo.0802258. [DOI] [PubMed] [Google Scholar]
- Horvath AO, Greenberg LS. Development and validation of the Working Alliance Inventory. Journal of Counseling Psychology. 1989;36(2):223–233. [Google Scholar]
- Janicke DM, Sallinen BJ, Perri MG, Lutes LD, Silverstein JH, Huerta MG, et al. Sensible treatment of obesity in rural youth (STORY): Design and methods. Contemporary Clinical Trials. 2008;29(2):270–280. doi: 10.1016/j.cct.2007.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffery RW, Wing RR, Thorson C, Burton LR, Raether C, Harvey J, et al. Strengthening behavioral interventions for weight loss: A randomized trial of food provision and monetary incentives. Journal of Consulting and Clinical Psychology. 1993;61(6):1038–1045. doi: 10.1037//0022-006x.61.6.1038. [DOI] [PubMed] [Google Scholar]
- Johnson PR, Thorn BE. Cognitive behavioral treatment of chronic headache: Group versus individual treatment format. Headache. 1989;29(6):358–365. doi: 10.1111/j.1526-4610.1989.hed2906358.x. [DOI] [PubMed] [Google Scholar]
- LeCheminant JD, Jacobsen DJ, Hall MA, Donnelly JE. A comparison of meal replacements and medication in weight maintenance after weight loss. Journal of the American College of Nutrition. 2005;24(5):347–353. doi: 10.1080/07315724.2005.10719484. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Research Quarterly for Exercise and Sport. 1992;63(1):60–66. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- McCarron DA, Oparil S, Chait A, Haynes RB, Kris-Etherton P, Stern JS, et al. Nutritional management of cardiovascular risk factors. A randomized clinical trial. Archives of Internal Medicine. 1997;157(2):169–177. [PubMed] [Google Scholar]
- McCloskey MS, Noblett KL, Deffenbacher JL, Gollan JK, Coccaro EF. Cognitive–behavioral therapy for intermittent explosive disorder: A pilot randomized clinical trial. Journal of Consulting and Clinical Psychology. 2008;76(5):876–886. doi: 10.1037/0022-006X.76.5.876. [DOI] [PubMed] [Google Scholar]
- Metz JA, Stern JS, Kris-Etherton P, Reusser ME, Morris CD, Hatton DC, et al. A randomized trial of improved weight loss with a prepared meal plan in overweight and obese patients: Impact on cardiovascular risk reduction. Archives of Internal Medicine. 2000;160(14):2150–2158. doi: 10.1001/archinte.160.14.2150. [DOI] [PubMed] [Google Scholar]
- Montoye HJ, Kemper H, Saras W, Washburn RA. Measuring physical activity and energy expenditure. Champaign, IL: Human Kinetics; 1996. [Google Scholar]
- National Center for Health Statistics. Health United States 2001: With Urban and Rural Health Chartbook (PHS) 2001. p. 1232. [Google Scholar]
- Nevonen L, Broberg AG. A comparison of sequenced individual and group psychotherapy for patients with bulimia nervosa. International Journal of Eating Disorders. 2006;39(2):117–127. doi: 10.1002/eat.20206. [DOI] [PubMed] [Google Scholar]
- NHLBI. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: Executive summary. Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. American Journal of Clinical Nutrition. 1998;68(4):899–917. doi: 10.1093/ajcn/68.4.899. [DOI] [PubMed] [Google Scholar]
- Noakes M, Foster PR, Keogh JB, Clifton PM. Meal replacements are as effective as structured weight-loss diets for treating obesity in adults with features of metabolic syndrome. Journal of Nutrition. 2004;134(8):1894–1899. doi: 10.1093/jn/134.8.1894. [DOI] [PubMed] [Google Scholar]
- Perri MG, Limacher MC, Durning PE, Janicke DM, Lutes LD, Bobroff LB, et al. Extended-care programs for weight management in rural communities: The treatment of obesity in underserved rural settings (TOURS) randomized trial. Archives of Internal Medicine. 2008;168(21):2347–2354. doi: 10.1001/archinte.168.21.2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perri MG, Nezu AM, McKelvey WF, Shermer RL, Renjilian DA, Viegener BJ. Relapse prevention training and problem-solving therapy in the long-term management of obesity. Journal of Consulting and Clinical Psychology. 2001;69(4):722–726. [PubMed] [Google Scholar]
- Pew Internet and American Life Project. Broadband Adoption 2006. From www.pewinternet.org/pdfs/PIP_Broadband_trends2006.pdf.
- Pi-Sunyer FX, Maggio CA, McCarron DA, Reusser ME, Stern JS, Haynes RB, et al. Multicenter randomized trial of a comprehensive prepared meal program in type 2 diabetes. Diabetes Care. 1999;22(2):191–197. doi: 10.2337/diacare.22.2.191. [DOI] [PubMed] [Google Scholar]
- Purath J, Miller AM. Predictors of improvement in women’s physical activity. Women’s Health. 2005;42(3):57–75. doi: 10.1300/j013v42n03_04. [DOI] [PubMed] [Google Scholar]
- Renjilian DA, Perri MG, Nezu AM, McKelvey WF, Shermer RL, Anton SD. Individual versus group therapy for obesity: Effects of matching participants to their treatment preferences. Journal of Consulting and Clinical Psychology. 2001;69(4):717–721. [PubMed] [Google Scholar]
- Richardson MT, Leon AS, Jacobs DR, Jr, Ainsworth BE, Serfass R. Comprehensive evaluation of the Minnesota Leisure Time Physical Activity Questionnaire. Journal of Clinical Epidemiology. 1994;47(3):271–281. doi: 10.1016/0895-4356(94)90008-6. [DOI] [PubMed] [Google Scholar]
- Sobal J, Troiano RP, Frongillo EA. Rural–urban differences in obesity. Rural Sociology. 1996;61(2):289–305. [Google Scholar]
- Tillitski CJ. A meta-analysis of estimated effect sizes for group versus individual control treatments. International Journal of Group Psychotherapy. 1990;40(2):215–224. doi: 10.1080/00207284.1990.11490601. [DOI] [PubMed] [Google Scholar]
- Tracey TJ, Kokotovic AM. Factor structure of the Working Alliance Inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1989;1(3):207–210. [Google Scholar]
- Turner-Stokes L, Erkeller-Yuksel F, Miles A, Pincus T, Shipley M, Pearce S. Outpatient cognitive behavioral pain management programs: A randomized comparison of a group-based multidisciplinary versus an individual therapy model. Archives of Physical Medicine and Rehabilitation. 2003;84(6):781–788. doi: 10.1016/s0003-9993(03)00015-7. [DOI] [PubMed] [Google Scholar]
- US Department of Agriculture and Economic Research Services. Rural definitions. Retrieved March 2, 2009, from http://www.ers.usda.gov/data/ruraldefinitions/
- Wing RR, Jeffery RW, Burton LR, Thorson C, Nissinoff KS, Baxter JE. Food provision vs structured meal plans in the behavioral treatment of obesity. International Journal of Obesity and Related Metabolic Disorders. 1996;20(1):56–62. [PubMed] [Google Scholar]
- Yalom ID. The theory and practice of group psychotherapy. New York: BasicBooks; 1995. [Google Scholar]