Abstract
Objective
To describe an adapted version of dialectical behavior therapy for adolescents with bipolar disorder.
Method
The dialectical behavior therapy intervention is delivered over 1 year and consists of two modalities: family skills training (conducted with individual family units) and individual therapy. The acute treatment period (6 months) includes 24 weekly sessions; sessions alternate between the two treatment modalities. Continuation treatment consists of 12 additional sessions tapering in frequency through 1 year. We conducted an open pilot trial of the treatment, designed as an adjunct to pharmacological management, to establish feasibility and acceptability of the treatment for this population. Participants included 10 patients (mean age 15.8 ± 1.5 years, range 14–18) receiving treatment in an outpatient pediatric bipolar specialty clinic. Symptom severity and functioning were assessed quarterly by an independent evaluator. Consumer satisfaction was also assessed posttreatment.
Results
Feasibility and acceptability of the intervention were high, with 9 of 10 patients completing treatment, 90% of scheduled sessions attended, and high treatment satisfaction ratings. Patients exhibited significant improvement from pre- to posttreatment in suicidality, nonsuicidal self-injurious behavior, emotional dysregulation, and depressive symptoms.
Conclusions
Dialectical behavior therapy may offer promise as an approach to the psychosocial treatment of adolescent bipolar disorder.
Keywords: bipolar disorder, therapy, psychosocial treatment
Over the past decade, bipolar disorder (BP) in children and adolescents has gained increasing attention. Research suggests that BP affects approximately 1% of community adolescents (Lewinsohn et al., 1995), with estimates as high as 6% to 15% in clinical samples (Biederman et al., 1995; Pavuluri et al., 2006). Adolescents with BP exhibit a difficult illness course characterized by prolonged episodes, substantial inter-episodic symptoms, and marked functional impairment (Birmaher et al., 2006). High rates of psychosis, comorbidity, and hospitalizations have also been reported in this population (Axelson et al., 2006). BP onset in adolescence is particularly pernicious due to its associations with drug and alcohol abuse, unprotected sex, and suicide (Brent and Lerner, 1994; Goldstein et al., 2005; McClellan et al., 1993). Evidence suggests the majority of adolescent-onset BP patients experience a deteriorating course into adulthood, with poor outcomes including chronic functional impairment and treatment resistance (Strober et al., 1995). Given the projected continuity and morbidity associated with adolescent BP, effective early intervention may minimize the long-term debilitating effects of the illness.
Although there has been progress in the area of pharmacotherapy for pediatric BP (Kowatch and DelBello, 2005), medications often leave patients with residual symptoms and side effects. Guidelines for the treatment of pediatric BP therefore identify psychosocial intervention that augments pharmacotherapy as a critical component of optimal treatment (Kowatch et al., 2005).
To date, there are no empirically validated psychosocial treatments for BP adolescents. However, several promising approaches are at various stages of treatment development. Miklowitz et al. (2004) demonstrated the feasibility of delivering a developmentally modified version of family-focused therapy (FFT-A) for BP adolescents in an open treatment development study. This 9-month psychoeducational/skills program was associated with decreases in manic, depressive, and problem behavior rating scores from intake to 1-year follow-up. Danielson et al. (2004) are testing a 12-session cognitive-behavioral therapy (CBT) for BP adolescents. For preadolescent BP, Fristad et al. (2003) tested the efficacy of a multifamily psychoeducational group. As compared with a waitlist control condition, parents receiving multifamily psychoeducational group therapy were more knowledgeable about their child’s mood disorder and more successful obtaining health services for their child over 6-month follow-up. Pavuluri et al. (2004) treated school-age BP children by combining +components of FFT and CBT. In this open trial, treatment was associated with improvement in psychosocial functioning, mood symptoms, and medication adherence.
DBT (Linehan, 1993a) is an evidence-based psychotherapy developed for adults with borderline personality disorder. The main DBT target is emotional dysregulation, characterized by high sensitivity to emotional stimuli, extreme emotional intensity, and a slow return to baseline emotional state. Not surprising, research indicates that teens with BP exhibit a range of extreme positive and negative emotions (Birmaher et al., 2006). In fact, recent literature posits that the core clinical feature underlying pediatric BP is emotional dysregulation (Leibenluft et al., 2003). Studies indicate that emotion regulatory processes are developmentally acquired, determined by both biological and psychosocial processes, and under consolidation during adolescence (Dahl and Spear, 2004). Yet, none of the interventions for adolescent BP examined to date expressly target this core illness feature. BP in adolescence is also associated with suicidal behaviors (Goldstein et al., 2005; Lewinsohn et al., 1995), interpersonal deficits (Goldstein et al., 2006), and treatment nonadherence (Coletti et al., 2005)—all DBT targets.
As compared with treatment as usual (TAU), DBT has been shown to reduce suicidal behaviors, hospitalizations, and anger, while improving social adjustment and treatment adherence among adults with borderline personality disorder (Linehan et al., 1994). Miller et al. (1997) adapted DBT for suicidal adolescents by incorporating age-appropriate language, decreasing treatment length, and involving family members in skills training groups. In a quasiexperimental design adolescents receiving DBT had fewer psychiatric hospitalizations and greater treatment adherence than TAU patients. DBT was also associated with decreases in depressive symptoms and suicidal ideation from pre-to posttreatment (Rathus and Miller, 2002). Katz et al. (2004) used DBT on an inpatient unit for suicidal adolescents, reporting decreased behavioral incidents, but not suicidality, as compared with a TAU unit.
In light of the successful adaptation of DBT for adolescents and the role of emotional dysregulation in BP, we applied DBT to the treatment of BP adolescents. First, we describe clinical methods and treatment adaptations for this population. We then present data from an open trial of DBT and pharmacotherapy in 10 adolescents with BP.
METHOD
Treatment Development
The DBT intervention for adolescents with BP is based on the manual of Miller et al. (2006) incorporating age-appropriate modifications for suicidal adolescents. We further incorporated illness-specific modifications designed to meet the unique needs of a BP population. In this section, we describe basic principles for applying DBT to adolescent BP.
Treatment Structure
As in standard DBT, we employed two treatment modalities: skills training (adapted for individual family units) in which the primary focus was to teach new skills, and individual therapy, which aims to aid the adolescent in applying skills in their daily lives. The same therapist (the first author) delivered both modalities. Therapist training before conduct of the pilot study included attendance at a 2-day DBT training and completion of a 3-month clinical rotation at a DBT-based intensive outpatient program for suicidal and parasuicidal women. During conduct of the study the therapist received additional DBT training and supervision via a 6-month DBT training program conducted by a certified BehavioralTech trainer consisting of a 2-day workshop, weekly DBT seminar, and weekly individual clinical supervision in DBT.
During the acute treatment period (months 1–6) participants received 24 weekly 60-minute sessions, alternating between the two modalities: 12 family skills training and 12 individual therapy sessions. The continuation phase of treatment (months 7–12) consisted of 12 total sessions (six family skills training, six individual therapy; each modality monthly) during which the aim was to consolidate gains and review skills application.
Standard DBT for adults includes 1 year of weekly skills group (2 hours) and individual therapy (1 hour). The DBT therapy schedule employed by Miller et al. with adolescents is less intensive: 16 weeks of skills group (2 hours) and individual therapy (1 hour). Although our treatment is longer than that of Miller et al. (1 year vs. 16 weeks), the treatment is less intensive because skills training sessions are conducted biweekly for 1 hour (vs. weekly for 2 hours), and individual therapy sessions are conducted biweekly (vs. weekly). In sum, our year-long protocol includes 18 hours of skills training and 18 hours of individual therapy (36 total treatment hours) as compared with the 16-week program of Miller et al. that includes 32 hours of skills training and 16 hours of individual therapy (48 total treatment hours). This therapy schedule emerged from considerations specific to this population. Given the cyclical nature of BP, extending treatment over a prolonged period increases the opportunity for skills to be applied across mood states, thereby maximizing clinical benefit. Furthermore, given that many adolescents with BP exhibit attention deficits, abbreviating skills training sessions to 1 hour may optimize learning.
Family Skills Training
Family skills training was conducted with the family unit and began with psychoeducation (sessions 1–2, see below), then proceeded through the four standard DBT modules: mindfulness (sessions 3–4), distress tolerance (sessions 5–7), emotion regulation (sessions 8–10), and interpersonal effectiveness (sessions 11–12; see Linehan, 1993b and Miller et al., 2006 for detailed description of skills modules). Content from “walking the middle path,” an additional module developed for parents of adolescents (Rathus and Miller, 2000) was woven throughout treatment and into the continuation phase.
We used handouts to introduce new skills. Participants were guided through exercises and activities for each skill imparted. Homework was assigned for participants to gain practice applying new skills. Family members were encouraged to coach one another in the effective use of skills in their environment.
Individual Therapy Sessions
Individual therapy sessions were structured in standard format (Miller et al., 2006), and target behaviors were prioritized in accordance with the DBT hierarchy of treatment targets. Problem-solving strategies were applied, including the conduct of behavioral chain analyses for targeted problems (e.g., medication nonadherence) to understanding the function of the behavior, identify constructive alternative solutions, and develop techniques for avoiding future problem behaviors.
Skills Coaching by Telephone
The therapist was available to participants by pager for in vivo skills coaching, a crucial, albeit challenging, aspect of DBT that appears particularly important with adolescent clients (Miller et al., 2006). Participants were educated about appropriate coaching situations. DBT therapists must identify and observe their own reasonable personal limits for telephone calls. Calling the therapist too frequently (as well as too infrequently) is considered therapy-interfering behavior and is targeted in individual sessions. The frequency of skills coaching calls was not documented in the pilot study.
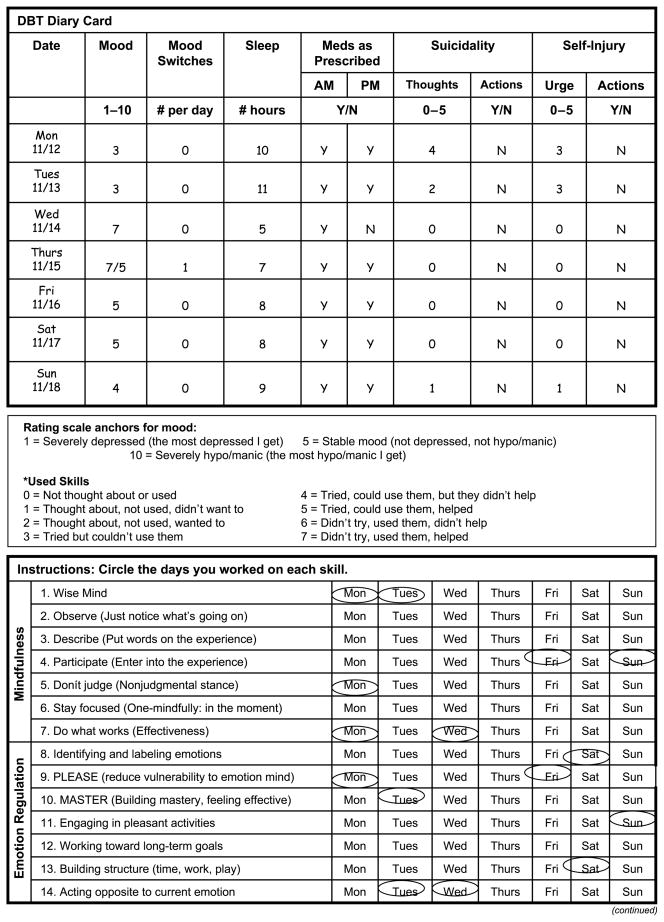
Diary Cards
Patients completed diary cards tailored for this population assessing mood, sleep, suicidality, and medication adherence daily during the study (Fig. 1). Patients reported use of specified DBT skills on the diary card; individualized treatment goals were also incorporated.
Fig. 1.
Sample diary card. Adapted from Miller et al. (2006).
Treatment Modifications
Family Skills Training
The DBT model for adolescents incorporates family members in skills training in a multifamily group format. We similarly believed that including the family would yield the most potential for clinical benefit with adolescents with BP based on literature linking stressful family environments with BP relapse (Butzlaff and Hooley, 1998) and poor treatment adherence (Geller and Luby, 1997). Furthermore, relatives of patients with adolescent-onset BP have elevated rates of BP (Faraone et al., 2003; Geller et al., 2006). Thus, not only do patients gain in vivo coaches, but family members gain skills for managing their own emotional dysregulation. We elected to deliver family skills training to individual family units to maximize DBT therapists’ ability to address issues specific to each family and devote time to skills that addressed areas of greatest need.
Addition of a Psychoeducation Module
Given that psychoeducation is integral to successful BP treatment (Kowatch et al., 2005), we added a psychoeducational module (sessions 1–2) on adolescent BP informed by psychoeducational content used in family-focused therapy for adolescents (Miklowitz et al., 2004). Psychoeducational handouts are available on the Journal’s Web site at www.jaacap.com through the Article Plus feature. Topics included symptoms and illness course, medication, and vulnerability factors. The adolescent and family were asked to describe mood states, with prompts for associated cognitions, behaviors, and emotions. These individualized mood and symptom descriptions were then used as anchor points for diary card mood ratings.
Psychoeducation about DBT was also provided, with rationale for its application in BP. A particular emphasis was placed on the importance of balance in the management of BP. A biosocial model was presented in which BP is conceptualized as a transaction between biological and environmental influences. In standard DBT the specific environmental role of invalidation is stressed. Because little research has examined environmental factors specific to the onset and maintenance of adolescent BP to date, we presented an inclusive biosocial approach, with attention to invalidation as one of several potential environmental vulnerabilities.
The three main components of emotional vulnerability were presented (reactivity, intensity, and duration of affective responses) and applied to the adolescent’s own mood states. Triggers for mood states were then identified and revisited throughout treatment as they pertained to skills use.
Tailoring Skills for BP
Although DBT skills were expressly developed for individuals prone to emotional dysregulation, we further tailored skills for BP to maximize their utility. For example, when introducing the mindfulness concept “states of mind,” the differential experience of “emotional mind” associated with depressed, manic, mixed, and euthymic states were explicitly discussed. These distinctions helped participants identify early warning signs of pending mood episodes and distinguish “normal” emotions from illness symptoms in a nonjudgmental fashion.
A unique aspect of applying DBT principles to BP is that although the same skill set is appropriate for managing a range of mood states, skill selection and application vary by mood state. To illustrate skill selection by mood state, the emotion regulation skill aiming to build positive emotions by engaging in pleasant activities may prove effective when depressed, but may exacerbate difficulties when manic. An example of the differential application of skills by mood state includes the emotion regulation skill “please master” focused on reducing vulnerability to emotional mind. Several participants identified the importance of balancing sleep in reducing vulnerability to emotional mind; too much sleep increased vulnerability to depression, whereas too little sleep increased vulnerability to mania.
To aid the teen in determining which skills to apply when and how, the primary focus was on helping him or her articulate a situation-specific goal in the context of his or her mood state. One participant, when depressed, would isolate herself in her room and listen to sad music, which would often precede incidents of self-injury. She was able to identify that when in this state, her goal was to “feel less miserable.” Thus, applying the emotion regulation skill “acting opposite” to change the current emotion may be skillful in this circumstance. Her opposite action included getting active by taking her dog for a walk while listening to upbeat music. Once the patient’s goal was defined, the patient determined which skill(s) may help attain the stated goal. When teaching skills, the therapist posed the question, “when/how do you think this skill could help you?”
During the continuation phase, family skills training sessions were used to review and consolidate skills. Patients created “coping cards” listing helpful skills for frequently encountered situations. Patients were encouraged to divide their lists by mood state (e.g., “skills that work best when I am depressed”).
PILOT STUDY
Participants
Participants were recruited from the Child and Adolescent Bipolar Services (CABS) specialty clinic at Western Psychiatric Institute and Clinic, University of Pittsburgh. Twelve patients identified by their psychiatrist as study eligible were invited to participate. Two declined participation (one cited work demands and the other entered more intensive treatment). The University of Pittsburgh Institutional Review Board approved all of the study procedures.
Inclusionary Criteria
These criteria were age between 12 years, 0 months and 18 years, 11 months; a DSM-IV diagnosis of BP I, II, or not otherwise specified (operationalized criteria, see Diagnostic Evaluation) with an acute manic, mixed, or depressive episode in the 3 months preceding study entry; engaged in a pharmacotherapy regimen; at least one parent/guardian willing to participate in family sessions; no evidence of mental retardation or organic CNS disorder; and not receiving other outpatient psychotherapy.
Demographics
Sample demographics, illness characteristics, and treatment at intake are presented in Table 1. On average, participants were 16 years old (range 14–18); eight were female. Seven patients met criteria for BPI. Eight participants had at least one comorbid Axis I diagnosis (anxiety, behavioral, and substance use disorders). Eight patients had a history of at least one suicide attempt, and seven had at least one psychiatric hospitalization.
TABLE 1.
Demographics and Illness Characteristics of DBT Pilot Study Participants (n = 10)
| Age, y | 15.8 ± 1.5 |
| Sex | |
| Female | 8 |
| Male | 2 |
| Socioeconomic statusa | 3.6 ± 1.1 |
| Race | |
| White | 6 |
| African American | 1 |
| Multiracial | 3 |
| Participating family members | |
| 2 biological parents | 3 |
| 1 biological parent (mother) | 5 |
| 2 grandparents | 1 |
| 1 grandparent (grandmother) | 1 |
| BP type | |
| I | 7 |
| II | 2 |
| NOS | 1 |
| Most severe lifetime episode: symptom severity | |
| Depressionb | 36.1 ± 7.3 |
| Maniac | 32.1 ± 12.9 |
| Current comorbid diagnoses | |
| Anxiety disorder | 5 |
| Behavioral disorder | 4 |
| Substance abuse disorder | 1 |
| Medications at intake | 2.2 ± 1.3 |
| Mood stabilizer | 7 |
| Atypical antipsychotic | 8 |
| Stimulant | 2 |
| Antidepressant | 4 |
| Benzodiazepine | 1 |
| Age of BP illness onset | 13.2 ± 1.7 |
| Past hospitalizations | 2.2 ± 2.2 |
| Past suicide attempts | 1.4 ± 1.3 |
Note: DBT = dialectical behavior therapy; BP = bipolar disorder; NOS = not otherwise specified.
Hollingshead Redlich criteria.
Schedule for Affective Disorders and Schizophrenia for School-Age Children–Depression Rating Scale; range 0–61.
Schedule for Affective Disorders and Schizophrenia for School-Age Children–Mania Rating Scale; range 0–63.
Procedures
Diagnostic Evaluation
Psychiatric diagnoses were established using the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime version (K-SADS-PL; Kaufman et al., 1997) and the K-SADS Mania Rating Scale (MRS; Axelson et al., 2003). Operationalized criteria for the diagnosis of BP not otherwise specified were adopted from the Course and Outcome of Bipolar Youth Study (see Birmaher et al., 2006). Diagnostic evaluation at CABS consisted of a 4-hour assessment process during which a CABS-trained interviewer (psychiatric nurse or social worker with a minimum of 5 years experience with youths with BP) administered the K-SADS, first to the parent/guardian and then to the adolescent (summary scores were based on a consensus between information provided by the adolescent and parent); the attending child and adolescent psychiatrist conducted a clinical interview with the adolescent and parent; and the evaluator and the attending used all available information to reach consensus on the patient’s diagnosis. No formal assessment of Axis II pathology was conducted.
Pharmacotherapy
CABS child and adolescent psychiatrists managed the pharmacological treatment of participants according to treatment guidelines established by an expert panel on pediatric BP (Kowatch et al., 2005). Standard pharmacological management in CABS consisted of follow-up visits weekly to biweekly for the first month of treatment. Assuming adequate treatment response, medication management visits were scheduled monthly thereafter. When patients were actively symptomatic, appointments were scheduled more frequently. The DBT therapist collaborated with subjects’ treating psychiatrists on a regular basis during weekly CABS clinic meetings, at which time each subject’s case was reviewed. CABS clinic meetings also offered the opportunity for consultation regarding treatment adaptations for adolescent BP in general.
At the baseline assessment the number of weeks on the prescribed medication regimen varied widely. The eligibility criterion requiring a syndromal mood episode within 3 months of study entry was intended to ensure that before treatment, mood symptoms were not fully stabilized by the current medication regimen alone.
Outcome Measures
Outcome measures were obtained at baseline and every 3 months during the 1-year protocol by a master’s degree–level independent evaluator trained to an acceptable level of reliability on all outcome measures (κ ≥ 0.80). Interrater reliability between the first author and the independent evaluator conducted on a random sample of five interviews yielded 80% exact item agreement on the K-SADS-P-DRS (Chambers et al., 1985a), 88% on MRS, and 100% on the Modified Scale for Suicidal Ideation (MSSI; Miller et al., 1986). Participants received $20 compensation after completion of each interview. Outcome variables were assessed in the domains of suicidality, emotional dysregulation, mood symptomatology, interpersonal functioning, and treatment satisfaction.
Suicidality
Suicidality was assessed via the MSSI (Miller et al., 1986); items are rated on a 0 to 3 scale indicating extent of suicidal ideation and intent. Research indicates the MSSI has good internal consistency and correlates highly with experienced clinicians’ ratings of patients’ suicidal ideation. Suicidality and nonsuicidal self-injurious behavior were also assessed using five K-SADS-DRS items (Chambers et al., 1985a).
Emotional Dysregulation
Parents completed the Children’s Affective Lability Scale (Gerson et al., 1996) designed to measure behavior reflective of emotional dysregulation. Items are rated on a 4-point scale indicating frequency of each behavior. Reliability has been demonstrated among controls, outpatient, and inpatient psychiatric samples.
Mood Symptomatology
Manic symptoms were assessed via the K-SADS-MRS (Axelson et al., 2003; Chambers et al., 1985b), a 13-item semistructured interview designed to elicit symptoms associated with mania in pediatric populations. The scale yields scores ranging from 0 to 63. The original MRS psychometric study demonstrated the scale to be a reliable measure of manic symptoms that is sensitive to changes in manic symptom severity with treatment.
Depressive symptoms were assessed using the DRS section of the K-SADS-P semistructured interview, on which depressive symptoms are rated on a 6-point scale from none to severe. The scale has good internal consistency and interrater reliability (Chambers et al., 1985a). The 12-item K-SADS-DRS was extracted from the K-SADS-P semistructured interview. The 12-item K-SADS-DRS has been shown to be a reliable measure of depressive symptom severity (Ambrosini et al., 1989) and yields scores ranging from 0 to 61.
The evaluator conducted separate interviews with the patient and parent. Final symptom ratings were based on summary scores incorporating information from both sources; in the event of conflicting information, clinical judgment guided summary ratings.
Interpersonal Functioning
Participants completed the self-rated Matson Evaluation of Social Skills with Youngsters (MESSY; Matson et al., 1983) on which subjects rate social behaviors on a 5-point scale according to behavioral frequency. The MESSY correlates highly with other measures of social competence and directly observed social behaviors (Matson et al., 1986). Parents completed the parent-rated version (T-MESSY).
Treatment Satisfaction
Posttreatment, patients and parents completed a treatment satisfaction questionnaire assessing acceptability and satisfaction with treatment, each rated on a 7-point scale.
Data Analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences Version 13 (SPSS). A series of paired comparison t tests were conducted to determine whether significant changes occurred in each of the domains of interest from pre- to posttreatment. Statistical significance was set at α = .05.
RESULTS
Feasibility
DBT was highly feasible to administer to adolescent BP patients and their families. Of the 10 patients who consented to participate, nine successfully completed the entire treatment study; one patient terminated prematurely because she moved out of state. Attendance at treatment was high, with more than 90% of scheduled sessions attended. Over the 1-year treatment period, patients received 33.2 ± 7.5 total sessions (the protocol calls for 36 sessions: family skills training session mean 15.3 ± 6.0, individual therapy session mean 17.9 ± 3.3).
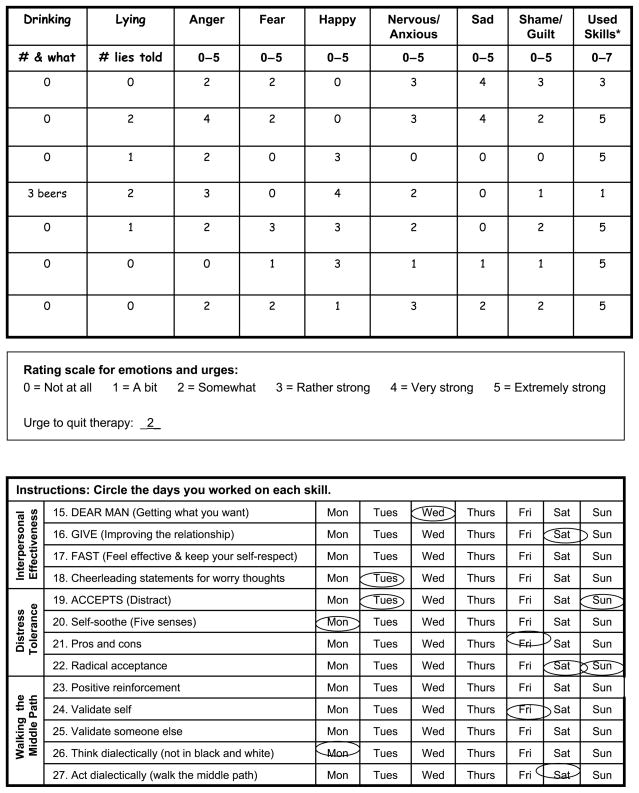
Patient Satisfaction
Posttreatment satisfaction questionnaires indicate the intervention was acceptable and appropriate to participants’ needs. Both patients and parents reported that the frequency of visits was acceptable (Likert scale rating 1–7 where 1 = too infrequent, 4 = acceptable, and 7 = too frequent; patient mean 4.7 ± 1.0, parent mean 3.7 ± 0.8), as was treatment length (Likert scale rating 1–7 where 1 = too short, 4 = acceptable, and 7 = too long; patient mean 3.8 ± 0.4, parent mean 3.4 ± 0.8). Satisfaction ratings show that patients and parents were highly satisfied with the DBT approach as well as with the gains that the adolescents made during treatment (Fig. 2).
Fig. 2.
Posttreatment satisfaction ratings for dialectical behavior therapy.
Treatment Response
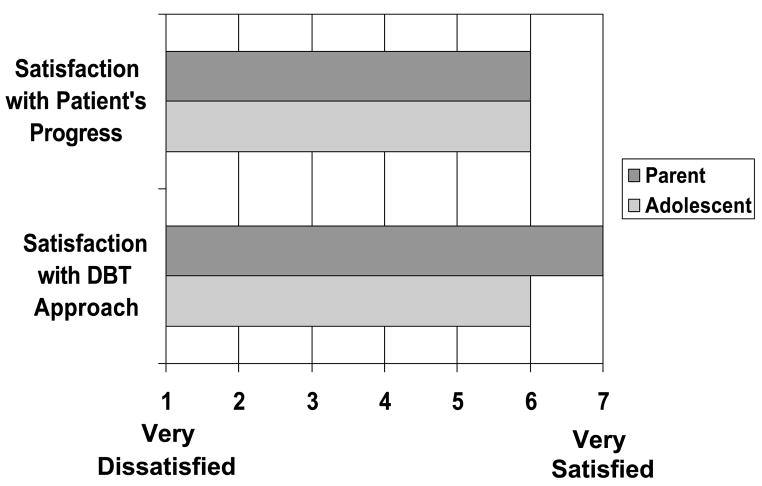
Suicidality
Although 80% of participants had a history of attempted suicide, and mean suicidal ideation ratings on both the MSSI and K-SADS-DRS (item 25) reflected the presence of suicidal ideation at intake, none of the participants reported attempting suicide (defined as a self-injurious act with minimal or greater intent to die via the MSSI and/or K-SADS-DRS) during the year-long study. Evaluator ratings of suicidality showed statistically significant improvement during the course of treatment (MSSI paired t = 2.5, p = .04, Cohen’s d = 1.2; DRS paired t = 2.4, p = .04, Cohen’s d = 0.9), and ratings reflect the absence of suicidality by the conclusion of treatment (Fig. 3). Similarly, at intake, four participants endorsed a history of nonsuicidal self-injurious behavior. Decreases in nonsuicidal self-injury on the K-SADS-DRS (item 30) were not statistically significant (paired t = 2.1, p = .06, d = 0.8), but it is noteworthy that no nonsuicidal self-injurious acts were reported during the final study assessment period.
Fig. 3.
Mean ratings of suicidality decrease with dialectical behavior therapy.
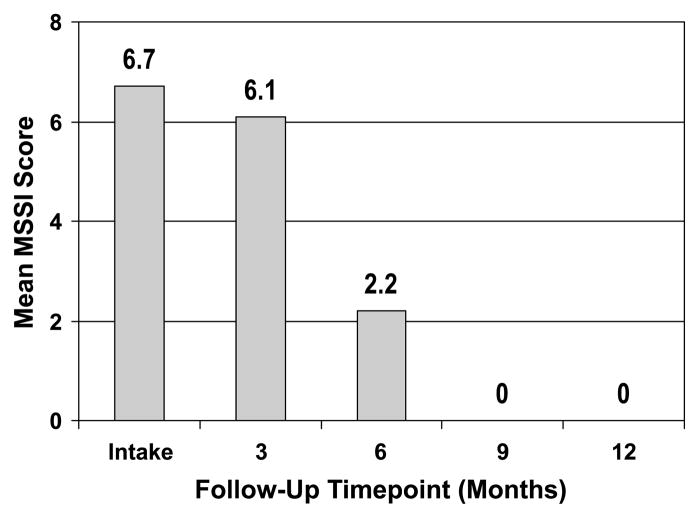
Emotional Dysregulation
As seen in Figure 4, total Children’s Affective Lability Scale scores decreased significantly (paired t = 3.0, p = .02, d = 0.3) from mean pretreatment values comparable to those reported among inpatient samples, to posttreatment values below those reported for outpatient samples (see Gerson et al., 1996).
Fig. 4.
Ratings of emotional dysregulation normalize with dialectical behavior therapy. CALS = Children’s Affective Lability Scale.
Mood Symptoms
Adolescents showed significant improvement in depressive symptomatology. Total K-SADS-DRS summary scores dropped from the moderate range at intake (mean 23.1 ± 12.0) to the mild range at 12-month follow-up (mean 14.9 ± 10.6; paired t = 2.6, p = .03, d = .7). We did not find significant differences between pretreatment (mean 13.3 ± 12.1) and posttreatment (mean 12.2 ± 14.2; paired t = 0.3, p > .05, d = 0.1) K-SADS-MRS ratings. However, mean intake MRS scores reflected mild manic symptomatology.
Interpersonal Functioning
Improvements in interpersonal functioning with treatment were not statistically significant (teen-reported MESSY paired t = 1.2, p >.05, d = 0.4; parent-reported T-MESSY paired t = 0.9, p > .05, d = 0.2). Mean pretreatment teen report scores were elevated compared with norms for healthy controls (Matson, 1994), whereas posttreatment self-ratings fell within the normal range. In contrast, posttreatment parent ratings remained elevated when compared with norms for this age group; they were, however, below those reported for other outpatient samples of BP adolescents engaged in treatment (Goldstein et al., 2006).
Pharmacotherapy
There were no differences in the number of medications prescribed for participants from pre- to posttreatment (pretreatment mean 2.2 ± 1.3, posttreatment mean 2.6 ± 1.7, paired t = −0.8, p >.05, d = −0.2). At the conclusion of the protocol, 7 of the 10 patients were maintained on the same number of medications as at intake, 1 was prescribed fewer medications, and 2 were prescribed more medications. Adherence to medication regimen was not assessed.
DISCUSSION
Results from this open trial provide initial support for the feasibility and clinical efficacy of DBT for adolescents with BP in a highly symptomatic sample. Significant improvement from pre- to posttreatment was evident in suicidality, nonsuicidal self-injurious behavior, emotional dysregulation, and depressive symptoms.
Nine of the 10 enrolled families completed this year-long treatment. More than 90% of scheduled sessions were attended, which is consistent with high acceptability and satisfaction ratings from participants. Conduct of skills training with individual family units was well received by participants and may have further contributed to the high attendance rates. Furthermore, both patients and parents indicated that they were highly satisfied with the DBT approach and the gains made during treatment. In fact, following the 12-month program, many parents expressed a desire for continued DBT. These satisfaction ratings come from highly experienced consumers of mental health services: 8 of 10 participants had at least one previous course of psychotherapy, 7 of whom had multiple courses.
This patient sample exhibited a high degree of illness severity. Eighty percent of participants had a history of attempted suicide compared with 20% to 44% of other pediatric BP samples (Lewinsohn et al., 2003; Strober et al., 1995). Seventy percent of the sample had a history of psychiatric hospitalization compared with 41% to 52% in other well-characterized pediatric BP samples (Axelson et al., 2006; Findling et al., 2001). With respect to mood symptomatology at intake, DBT participants had more severe depressive, but not manic, symptom scores compared with Course and Outcome of Bipolar Youth Study participants; similarly, DBT participants endorsed more severe symptoms during their worst lifetime episode of depression, but not mania (Axelson et al., 2006). The illness profile of the study sample taken with their treatment response raises the possibility that BP severity, and particularly that of the depressive pole, moderates the effects of DBT for this population; this may occur via numerous pathways. One possibility is that families of more severely ill teens are more willing to commit to and attend treatment, thereby maximizing the efficacy of the intervention. Perhaps severely ill teens are more motivated to practice skills application and thus derive more benefit from a skills-based approach. Alternatively, given that BP and borderline personality disorder frequently co-occur (Magill, 2004), it is possible that illness severity in this sample is indicative of comorbid borderline features that served to moderate treatment response.
Clinical gains from pre- to posttreatment were evident in the domains of suicidality, nonsuicidal self-injurious behavior, emotional dysregulation, and depressive symptoms. It is noteworthy that the domains of improvement that we document are similar to those reported in randomized, controlled trials of DBT for adults, as well as those reported in the quasiexperimental DBT study with suicidal adolescents (Rathus and Miller, 2002). These findings may lend support to the emerging view of pediatric BP as a disorder of emotional dysregulation and DBT as a viable treatment approach targeting this core feature.
Limitations
These findings are from a small open trial, and therefore should be viewed as preliminary. Given that we do not have data from a comparison group, we cannot conclude that DBT was responsible for the observed improvement. That is, improvement could be attributable to other factors including natural course of illness, medications, or nonspecific therapeutic elements like attention. In addition, given that patients exhibited only mild manic symptomatology at pre-treatment, we have limited ability to assess manic symptom improvement with DBT in the present sample. Furthermore, elements of DBT overlap with other efficacious interventions for BP (e.g., CBT, social rhythm therapy, family-focused therapy), rendering it possible that the “active ingredient” in DBT for BP adolescents is common to other therapies. Nonetheless, there is a logical link between the treatment modules delivered and the areas of clinical improvement observed; namely, skills focused on improving emotion regulation and distress tolerance, and improvements were noted in related areas of mood lability and suicidality. Finally, because the first author was the only DBT-trained clinic staff member, the consultation team (a central DBT element to provide therapist support and improve adherence) was not employed. This omission may have caused higher levels of therapist burnout resulting in reduced effectiveness. Without data on treatment adherence, we are unable to determine whether absence of the consultation team compromised adherence to the DBT model.
Clinical Implications
Clinicians providing treatment to adolescent BP patients encounter a myriad of treatment challenges. DBT’s emphasis on skill building and improving emotion regulation provide a coherent framework well suited for addressing the cyclicity and chronicity associated with BP. This study demonstrates the feasibility of implementing DBT with adolescent BP patients and their families by incorporating adaptations for age and illness. Preliminary data from a highly ill sample of BP adolescents suggest the intervention was well accepted by patients and their families and was associated with improvement from pre- to posttreatment in multiple domains including suicidality, nonsuicidal self-injury, emotional dysregulation, and depressive symptomatology.
Future Directions
Conduct of a randomized, controlled trial incorporating a comparison condition will be an important future direction to demonstrate treatment efficacy. Furthermore, identification of factors (e.g., Axis I or II comorbidity) predicting treatment response within this highly heterogeneous group may prove beneficial, so that we may match patients with treatments from which they are most likely to derive benefit.
Future studies should also aim to understand the mechanisms of treatment-related improvement. For example, we plan to add posttreatment measures assessing participants’ knowledge of DBT skills to determine to what extent clinical improvement is related to skills acquisition.
Acknowledgments
This research was supported by an American Foundation for Suicide Prevention (AFSP) Pilot Grant, a seed grant from the University of Pittsburgh Advanced Center for Intervention and Services Research for Early-Onset Mood and Anxiety Disorders (MH66371, D.A.B.), and NIMH training grant MH18951 (D.A.B.). The authors acknowledge the contributions of Heather Schwickrath, Colleen Grimm, and Pamala Pyle.
Footnotes
Disclosure: The authors have no financial relationships to disclose.
References
- Ambrosini PJ, Metz C, Prabucki K, Lee J. Videotape reliability of the third edition of the K-SADS. J Am Acad Child Adolesc Psychiatry. 1989;28:723–728. doi: 10.1097/00004583-198909000-00013. [DOI] [PubMed] [Google Scholar]
- Axelson DA, Birmaher B, Brent D, et al. A preliminary study of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children Mania Rating Scale for Children and Adolescents. J Child Adolesc Psychopharmacol. 2003;13:463–470. doi: 10.1089/104454603322724850. [DOI] [PubMed] [Google Scholar]
- Axelson DA, Birmaher B, Strober M, et al. Phenomenology of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006;63:1139–1148. doi: 10.1001/archpsyc.63.10.1139. [DOI] [PubMed] [Google Scholar]
- Biederman J, Wozniak J, Kiely K, et al. CBCL clinical scales discriminate prepubertal children with structured interview-derived diagnosis of mania from those with ADHD. J Am Acad Child Adolesc Psychiatry. 1995;34:464–471. [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Strober M, et al. Clinical course of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry. 2006;63:175–183. doi: 10.1001/archpsyc.63.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Lerner MS. Cognitive therapy with affectively ill, suicidal adolescents. In: Wilkes TCR, Belsher G, Rush AJ, Frank E, editors. Cognitive Therapy for Depressed Adolescents. New York: Guilford; 1994. pp. 298–320. [Google Scholar]
- Butzlaff RL, Hooley J. Expressed emotion and psychiatric relapse: a meta-analysis. Arch Gen Psychiatry. 1998;55:547–552. doi: 10.1001/archpsyc.55.6.547. [DOI] [PubMed] [Google Scholar]
- Chambers WJ, Puig-Antich J, Hirsch M, et al. The assessment of affective disorders in children and adolescents by semistructured interview: test-retest reliability of the schedule for affective disorders and schizophrenia for school-age children, present episode version. Arch Gen Psychiatry. 1985a;42:696–702. doi: 10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Tabrizi MA, Johnson R. The schedule for affective disorders and schizophrenia for school age children. Arch Gen Psychiatry. 1985b;42:696–702. doi: 10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- Coletti DJ, Leigh E, Gallelli KA, Kantafaris V. Patterns of adherence to treatment in adolescents with bipolar disorder. J Child Adolesc Psychopharmacol. 2005;15:913–917. doi: 10.1089/cap.2005.15.913. [DOI] [PubMed] [Google Scholar]
- Dahl RE, Spear L. Adolescent Brain Development: Vulnerabilities and Opportunities. New York: New York Academy of Sciences; 2004. [DOI] [PubMed] [Google Scholar]
- Danielson CK, Feeny N, Findling RL, Youngstrom EA. Psychosocial treatment of bipolar disorders in adolescents: a proposed cognitive-behavioral intervention. Cogn Behav Pract. 2004;11:283–297. [Google Scholar]
- Faraone S, Glatt S, Tsuang MT. The genetics of pediatric-onset bipolar disorder. Biol Psychiatry. 2003;53:970–977. doi: 10.1016/s0006-3223(02)01893-0. [DOI] [PubMed] [Google Scholar]
- Findling R, Gracious BL, McNamara NK, et al. Rapid, continuous cycling and psychiatric co-morbidity in pediatric bipolar I disorder. Bipolar Disord. 2001;3:202–210. [PubMed] [Google Scholar]
- Fristad MA, Goldberg-Arnold JS, Gavazzi SM. Multi-family psychoeducation groups in the treatment of children with mood disorders. J Marital Fam Ther. 2003;29:491–504. doi: 10.1111/j.1752-0606.2003.tb01691.x. [DOI] [PubMed] [Google Scholar]
- Geller B, Luby J. Child and adolescent bipolar disorder: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 1997;36:1168–1176. doi: 10.1097/00004583-199709000-00008. [DOI] [PubMed] [Google Scholar]
- Geller B, Tillman R, Bolhofner K, Zimmerman B, Strauss N, Kaufmann P. Controlled, blindly rated, direct-interview family study of a prepubertal and early-adolescent bipolar I disorder phenotype. Arch Gen Psychiatry. 2006;63:1130–1138. doi: 10.1001/archpsyc.63.10.1130. [DOI] [PubMed] [Google Scholar]
- Gerson AC, Gerring JP, Freund L, Joshi PK. The children’s affective lability scale: a psychometric evaluation of reliability. Psychiatry Res. 1996;65:189–197. doi: 10.1016/s0165-1781(96)02851-x. [DOI] [PubMed] [Google Scholar]
- Goldstein TR, Birmaher B, Axelson D, et al. History of suicide attempts in pediatric bipolar disorder: factors associated with increased risk. Bipolar Disord. 2005;7:525–535. doi: 10.1111/j.1399-5618.2005.00263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein TR, Mullen K, Miklowitz DJ. Social skills knowledge and performance among adolescents with bipolar disorder. Bipolar Disord. 2006;8:350–361. doi: 10.1111/j.1399-5618.2006.00321.x. [DOI] [PubMed] [Google Scholar]
- Katz LY, Cox BJ, Gunasekara S, Miller AL. Feasibility of dialectical behavior therapy for suicidal adolescent inpatients. J Am Acad Child Adolesc Psychiatry. 2004;43:276–282. doi: 10.1097/00004583-200403000-00008. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children Present and Lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kowatch R, Fristad MA, Birmaher B, et al. Treatment guidelines for children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry. 2005;44:213–235. doi: 10.1097/00004583-200503000-00006. [DOI] [PubMed] [Google Scholar]
- Kowatch RA, DelBello MP. Pharmacotherapy of children and adolescents with bipolar disorder. Psychiatr Clin North Am. 2005;28:385–397. doi: 10.1016/j.psc.2005.02.001. [DOI] [PubMed] [Google Scholar]
- Leibenluft E, Charney DS, Pine D. Researching the pathophysiology of pediatric bipolar disorder. Soc Biol Psychiatry. 2003;53:1009–1020. doi: 10.1016/s0006-3223(03)00069-6. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Klein DN, Seeley JR. Bipolar disorders in a community sample of older adolescents: prevalence, phenomenology, comorbidity and course. J Am Acad Child Adolesc Psychiatry. 1995;34:454–463. [PubMed] [Google Scholar]
- Lewinsohn PM, Seeley JR, Klein DN. Bipolar disorder in adolescents: epidemiology and suicidal behavior. In: Geller B, DelBello MP, editors. Bipolar Disorder in Childhood and Early Adolescence. New York: Guilford; 2003. pp. 7–24. [Google Scholar]
- Linehan MM. Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York: Guilford; 1993a. [Google Scholar]
- Linehan MM. Skills Training Manual for Treating Borderline Personality Disorder. New York: Guilford; 1993b. [Google Scholar]
- Linehan MM, Tutek DA, Heard HL, Armstrong HE. Interpersonal outcome of cognitive behavioral treatment for chronically suicidal borderline patients. Am J Psychiatry. 1994;151:1771–1776. doi: 10.1176/ajp.151.12.1771. [DOI] [PubMed] [Google Scholar]
- Magill CA. The boundary between borderline personality disorder and bipolar disorder: current concepts and challenges. Can J Psychiatry. 2004;49:551–556. doi: 10.1177/070674370404900806. [DOI] [PubMed] [Google Scholar]
- Matson J. Matson Evaluation of Social Skills With Youngsters: Manual. Baton Rouge, LA: IDS Publishing; 1994. [Google Scholar]
- Matson JL, Heinze A, Helsel WJ, Kapperman G, Rotatori A. Assessing social behaviors in the visually handicapped: the Matson Evaluation of Social Skills With Youngsters. J Clin Child Psychol. 1986;15:78–87. [Google Scholar]
- Matson JL, Rotatori AF, Helsel WJ. Development of a rating scale to measure social skills in children: the Matson Evaluation of Social Skills With Youngsters (MESSY) Behav Res Ther. 1983;21:335–400. doi: 10.1016/0005-7967(83)90001-3. [DOI] [PubMed] [Google Scholar]
- McClellan J, Werry JS, Ham M. A follow-up study of early onset psychosis: comparison between outcome diagnoses of schizophrenia, mood disorders, and personality disorders. J Autism Dev Disord. 1993;23:243–262. doi: 10.1007/BF01046218. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, George EL, Axelson DA, et al. Family-focused treatment for adolescents with bipolar disorder. J Affect Disord. 2004;82:113–128. doi: 10.1016/j.jad.2004.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AL, Rathus JH, Linehan MM. Dialectical Behavior Therapy With Suicidal Adolescents. New York: Guilford; 2006. [Google Scholar]
- Miller AL, Rathus JH, Linehan MM, Wetzler S, Leigh E. Dialectical behavior therapy adapted for suicidal adolescents. J Pract Psychiatry Behav Health. 1997;3:78–86. [Google Scholar]
- Miller IW, Norman WH, Bishop SB, Dow MG. The modified scale for suicidal ideation: reliability and validity. J Consult Clin Psychol. 1986;54:724–725. doi: 10.1037//0022-006x.54.5.724. [DOI] [PubMed] [Google Scholar]
- Pavuluri MN, Birmaher B, Naylor MW. Pediatric bipolar disorder: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2006;44:846–871. doi: 10.1097/01.chi.0000170554.23422.c1. [DOI] [PubMed] [Google Scholar]
- Pavuluri MN, Graczyk P, Henry D, Carbray JA, Heidenreich J, Miklowitz D. Child- and family-focused cognitive behavioral therapy for pediatric bipolar disorder: development and preliminary results. J Am Acad Child Adolesc Psychiatry. 2004;43:528–537. doi: 10.1097/00004583-200405000-00006. [DOI] [PubMed] [Google Scholar]
- Rathus JH, Miller AL. DBT for adolescents: dialectical dilemmas and secondary treatment targets. Cogn Behav Pract. 2000;7:425–434. [Google Scholar]
- Rathus JH, Miller AL. Dialectical behavior therapy adapted for suicidal adolescents. Life Threat Behav. 2002;32:146–157. doi: 10.1521/suli.32.2.146.24399. [DOI] [PubMed] [Google Scholar]
- Strober M, Schmidt-Lackner S, Freeman R, Bower S, Lampert C, DeAntonio M. Recovery and relapse in adolescents with bipolar affective illness: a five-year naturalistic, prospective follow-up. J Am Acad Child Adolesc Psychiatry. 1995;34:724–731. doi: 10.1097/00004583-199506000-00012. [DOI] [PubMed] [Google Scholar]