Abstract
In September 2006, members of the Sex, Gender and Pain Special Interest Group of the International Association for the Study of Pain met to discuss the following: (1) what is known about sex and gender differences in pain and analgesia; (2) what are the “best practice” guidelines for pain research with respect to sex and gender; and (3) what are the crucial questions to address in the near future? The resulting consensus presented herein includes input from basic science, clinical and psychosocial pain researchers, as well as from recognized experts in sexual differentiation and reproductive endocrinology. We intend this document to serve as a utilitarian and thought-provoking guide for future research on sex and gender differences in pain and analgesia, both for those currently working in this field as well as those still wondering, “Do I really need to study females?”
Keywords: Sex differences, Gonadal hormones, Estrogens
1. The case for studying sex and gender differences in pain and analgesia
The pain field has moved from debating whether sex differences in pain exist to recognizing the importance of these differences. Attention is now directed toward understanding (1) what conditions lead to the expression of sex and gender differences in pain experience and reactivity, (2) what mechanisms underlie these differences, and (3) how these differences can inform clinical management of pain.
As noted in a recent review, at least 79% of animal studies published in Pain over the preceding 10 years included male subjects only, with a mere 8% of studies on females only, and another 4% explicitly designed to test for sex differences (the rest did not specify) [142]. Given the substantially greater prevalence of many clinical pain conditions in women vs. men [20,199], and growing evidence for sex differences in sensitivity to experimental pain and to analgesics [21,41,213], we recommend that all pain researchers consider testing their hypotheses in both sexes, or if restricted by practical considerations, only in females. It is invalid to assume that data obtained in male subjects will generalize to females, and the best non-human model of the modal human pain sufferer – a woman – is a female animal. If only males are examined in a given study, it is important that a rationale for exclusion of females be provided and that the potential limitation in generalizability of the findings be addressed in the discussion, particularly when examining a pain phenomenon that occurs with greater prevalence or severity in females. In both preclinical and clinical studies, a comparison of both sexes will further our understanding of individual differences in sensitivity to pain and analgesia, thus improving our ability to treat and prevent pain in all people.
2. General considerations
Two issues of terminology are important. First, the term “sex” refers to biologically based differences, while the term “gender” refers to socially based phenomena. Although biological sex exerts a major influence on one’s gender identity, sex and gender are not equivalent, and the terms are not interchangeable. If subjects are categorized by anatomical features (chromosomes, reproductive organs), it is appropriate to describe the study as one of “sex differences”. In contrast, if additional measures of masculinity/femininity or gender identity are used to describe subjects, then the term “gender differences” is appropriate [88,216]. Gender is often conceptualized as a dichotomous variable, yet individuals differ in the degree to which they conform to the norms for masculinity and femininity in their particular culture. Thus, gender is most accurately regarded as a continuous variable (ranging from exclusively feminine to exclusively masculine), with most individuals falling somewhere along the continuum of maleness to femaleness on a range of characteristics. Even within the same society, gender role expectations may differ for generations born at different times, and within an age-cohort, gender role expectations may change as a function of age. Finally, in any statistical analysis of human subjects, the dichotomous variable sex (male vs. female) is confounded with the social construct of gender. That is, in human studies in which the dependent measure is pain report, group differences are likely to be attributable to both sex and gender. Therefore, both constructs should be examined when possible in order to understand their relative contribution to differences in pain between men and women. For the sake of efficiency – and because most studies to date have classified subjects by sex rather than gender – the terms “sex” and “sex difference” will be used in this paper, except when gender is specifically discussed.
The second issue of terminology regards the use of the term “estrogen” to refer to any of a number of steroid hormones akin to estradiol. In fact, “estrogen” and “progestin” refer to classes of hormones, each specific hormone being “an estrogen” or “a progestin.” We encourage pain researchers to refer to the specific hormone used in their studies, whether it is estradiol, estrone, estriol, or others in the case of estrogens, or the naturally occurring progesterone or specific synthetic progestin in the case of progestins.
3. Experimental study of sex differences in pain and analgesia
Researchers studying sex differences in pain are strongly advised to consult a recent, comprehensive set of guidelines entitled “Strategies and Methods for Research on Sex Differences in Brain and Behavior” [17]. In addition, methodological issues that are specific to pain research are discussed below.
It is generally agreed that the first stage of any sex difference study should be a comparison of gonadally intact adult females and males. In the absence of previous evidence for large menstrual/estrous cycle-related variations in the measure of interest, it is not absolutely necessary to test females in specific stages. However, a failure to observe sex differences in pain can be interpreted in multiple ways: (1) no sex difference exists; (2) the observed sex difference occurs only when females are in a particular stage of the menstrual or estrous cycle (e.g., [193]), and the sex difference could not be discerned due to “averaging” across the cycle; (3) a sex difference in mechanism exists even though the magnitude of the phenomenon under study is similar in males and females (e.g., [126,127]); or (4) two sex-specific mechanisms exist that cancel each other out, resulting in no phenotypic sex difference [50,153]. Thus, in the case of a negative finding when comparing gonadally intact females vs. males, interpretations 2, 3, and 4 should be acknowledged.
When designing and interpreting studies on sex differences in pain or nociception, it is important to recognize that there are sex differences in a number of physiological systems that may directly or indirectly affect measures of pain/analgesia. For example, adult male rodents have greater percentage of body fat than females [124], while the opposite is true for humans [78]. This sexual dimorphism can affect the distribution of highly lipophilic drugs, and therefore influence analgesic drug potency, efficacy, and duration of action. Other aspects of pharmacokinetics, including liver metabolism and membrane transport, may differ between the sexes [139,144], possibly affecting analgesic potency, efficacy, and duration of action. Immune responses also differ between the sexes [21], which may contribute to sex differences in response to chronic inflammatory and neuropathic pain. The activity level of female rodents varies dramatically across the estrous cycle [24,74], which may introduce a confound on pain tests that allow subjects to locomote freely, such as the hot-plate test. Lastly, adverse effects of analgesics such as respiratory depression and nausea may occur differentially in females vs. males [32,46,179], which is important to consider when comparing analgesic efficacy in females vs. males.
3.1. Are sex differences mediated by gonadal hormones?
As described by Becker et al. [17], if a sex difference is observed in gonadally intact adults, a logical next step is to determine whether the sex difference can be attributed to the actions of gonadal steroid hormones, either activationally (in adulthood) or organizationally (during development). Organizational effects can only be practically examined in animal studies. Several recent reviews have described the multiple ways in which estrogens, progestins, and androgens may modulate nervous system function related to pain and analgesia [5,6,41,43,111,193].
3.2. Testing across the estrous cycle: animal studies
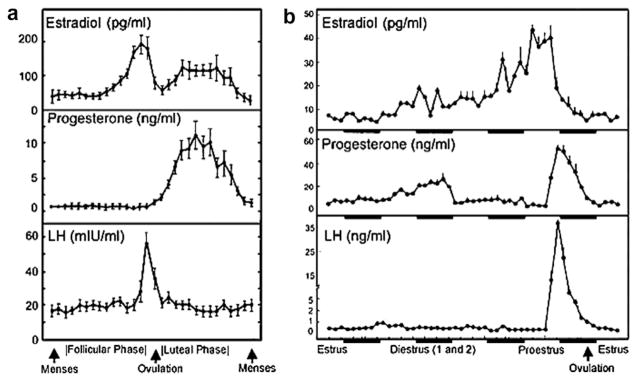
The value of testing female rodents at different stages of the estrous cycle is debatable. In rodents, an influence of estrous cycle stage is not necessarily indicated by larger observed variance [142]; therefore, large samples are typically required to adequately power studies examining females in specific stages of the estrous cycle. One of the most reliable and simple ways to determine stage of the estrous cycle in rodents, sampling vaginal cytology, requires that females be handled and probed daily for at least two cycles (approximately 8–10 days). Given that females and males often respond differently to acute stressors (e.g., [214]), it is not clear whether daily handling of males adequately controls for this potential confound. Obtaining repeated vaginal samples in rodents also may affect sensitivity to drugs [209]. An alternative to daily vaginal lavage is to measure motor activity (in the home cage), which peaks during proestrus [24]. Because rodent estrous cycles differ substantially from primate menstrual cycles (Fig. 1), one cannot readily extrapolate a cycle effect in a rodent to one in a human. Therefore, although estrous cycle fluctuations in a pain/analgesia measure suggest that reproductive hormones modulate the effect of interest, this hypothesis is more directly and efficiently tested using a hormone depletion/replacement approach (see Section 3.4), which is readily accomplished in rodents. If females in different stages of the estrous cycle are tested, it is imperative that the investigator explicitly state how the stages – particularly the stage of most dramatic hormone change, proestrus – are defined, as there is more than one way to designate stage of cycle. One study has shown significant differences in analgesic sensitivity between females in “early” vs. “late” proestrus [19].
Fig. 1.
Patterns of estradiol, progesterone, and leuteinizing hormone (LH) in humans (a) and rats (b) during the reproductive cycle. Time unit of the x-axis in (a) is days; in (b), it is hours. Dark bars in (b) indicate dark period of the day/night cycle. Note that during the follicular phase in humans and its analog in rats (diestrus 2), 17β-estradiol rises but progesterone secretion remains low. After the LH surge, progesterone is elevated in both rats and women. In humans, the corpus luteum also secretes some 17β-estradiol, whereas in rats, during the brief luteal phase, 17β-estradiol concentrations decline. Reproduced from [17], with permission.
3.3. Testing across the menstrual cycle and reproductive stages: human studies
In humans, while it may not always be important to test at different stages of the menstrual cycle, it is always important to consider whether such testing is appropriate. If menstrual cycle itself is not a factor to be evaluated, the investigator should plan to evaluate women in the same phase of their cycle. There is no one ideal phase of the cycle to choose. Both absolute and relative hormonal levels could influence pain. Times of rapid change in hormone levels (e.g., ovulation) or phases when subjective mood changes are thought to occur (e.g., pre-menstrual) may be of interest.
Start date of the last menstrual period can be reliably obtained from self-report, as can year and month of menarche [77]. A number of methods, including analysis of daily vaginal secretions, basal body temperature, and ovulation kits can provide information on the occurrence and approximate timing of ovulation, although some methods are more reliable than others [17] (p. 1663). Prediction of ovulation using urine-based home ovulation testing kits to assess leuteinizing hormone surge is a minimum standard in studies in which the menstrual cycle is of interest. These kits are relatively inexpensive, are easy for subjects to use, and have high sensitivity and specificity for detecting ovulation [138]. Additional measurement of blood or salivary levels of mid-luteal progesterone can confirm ovulation [183]. Although serum-based measurements are still the most widely used and considered the gold-standard for clinical research, saliva-based methods can be an alternative. Saliva-derived hormone measures reflect the fraction of the hormone that exerts biological effects [158]. Furthermore, collection of saliva is non-invasive and pain-free; with appropriate instruction, the subject can collect saliva at home and store it in a home freezer without deterioration of the sample [66]. A serious drawback is that salivary hormone levels may be below detection levels. Additionally, standardization across laboratories can be a problem. It should be noted that both serum and salivary measures of estradiol and progesterone exhibit great between-subject variability within the range of normal. However, because menstrual cycle length varies between and within women [198], and hormone levels also vary from one day to the next in some phases of the cycle, if hormonal status is a critical variable in the research, it is best measured directly rather than inferred from self-report and ovulation measures of menstrual cycle phase.
The standard designations for stages of the menstrual cycle (menstrual, follicular, ovulatory, and luteal) are gynecological terms based on reproductive function. However, a woman’s actual hormone levels within a phase vary radically. Thus, researchers must consider whether their interest is in reproductive function or in the relationship of hormone levels to pain. If the interest is in hormone levels, the gynecological nomenclature (and the lack of standardization with which it is applied) represents an obstacle to progress in the field [165,183]. We propose that use of the terms menstrual, follicular, ovulatory, and luteal be discouraged in human clinical pain studies, unless coupled with report of the actual days of the menstrual cycle, standardized to a 28-day cycle based on ovulation testing. One statistical standardization method is described by LeResche et al. [122]; however, other reasonable standardization methods are possible, and reaching consensus on the issue of how to standardize menstrual cycles of various lengths would facilitate comparison across studies. For these reasons, hormone levels should be reported when available.
If the research question is specifically cycle-related, as opposed to hormone-related, subjects with irregular cycles should be excluded. However, it is difficult to exclude irregularly cycling subjects based only on self-report; many subjects who describe their cycles as regular in fact have irregular cycles [198]. Even monitoring cycles before study enrollment may not solve this problem because there are no agreed criteria for distinguishing between a regular and irregular cycle. If the research question concerns the relationship between pain and hormone levels (or hormone variability) and hormones are measured directly, including irregularly cycling subjects may not be a problem, provided sufficient hormonal variability occurs. However, this approach assumes that the neurohormonal processes related to pain are comparable for women with regular and irregular cycles, which may not be the case. Finally, it is important to record dysmenorrheal status, as dysmenorrheic women may differ from those without dysmenorrhea in their responses to (non-menstrual) pain stimuli, especially during the perimenstrual period (e.g., [15,75]).
Circadian rhythms have been documented for steroid hormone levels [26,105], autonomic nervous system activity [27], and drug absorption [36]. These rhythms may be altered by menstrual cycle rhythms in women. For example, at the time of ovulation, decreased absorption of drugs such as aspirin and alcohol occurs and intestinal transit times are longer in the late luteal phase, during pregnancy and with hormone supplementation; these effects can influence drug onset time. With a few exceptions (e.g., [134]), the effect of circadian rhythms on pain and analgesia is largely unexplored.
Inclusion of non-cycling subjects may be of interest at specific life stages (pre-puberty, pregnancy, menopause). The conventional standard is to define puberty according to Tanner stages [196], based on clinical examination of development of secondary sex characteristics. Self-report measures with sufficient reliability and validity are available for use in studies where direct examination is not feasible [25]. A woman is conventionally defined as “post-menopausal” one year after the last menstrual period, provided the cause of amenorrhea is not pregnancy, nursing, disease, or medical intervention [217]. Date of menopause is the date of the last menstrual period. Standardized criteria for stages of the menopausal transition are also available [83]. If pregnant women are studied, stage of pregnancy should be clearly noted, as pain responses are known to change dramatically over the course of pregnancy (e.g., [16,121]). Reproductive history also may be important to document. For example, pain during breastfeeding in the first week postpartum is directly predicted by parity, with women who have given birth to more children experiencing more pain [87]. Conversely, in the laboratory (and not in close proximity to birth), multiparous women have higher pain thresholds than nulliparous women [82].
3.4. Hormone manipulations: animal studies
A useful approach for identifying effects of particular hormones on pain/analgesia in animals is gonadectomy with or without hormone replacement. However, it is important to keep in mind that hormone depletion via gonadectomy alters the physiological status of the animal in two significant ways. First, surgery can affect pain thresholds [93,173] and sensitivity to analgesics. Second, gonadectomy disrupts the normal feedback loop that sex steroids exert on the anterior pituitary and hypothalamus, leaving both males and females in a prolonged state of elevated (e.g., gonadotropin-releasing hormone (GnRH), leuteinizing hormone) or depressed (e.g., prolactin) circulating hormones [1,53,95,220]. The likelihood of unintended consequences due to altered hypothalamic/pituitary hormone secretion can be addressed by administering low (maintenance) doses of estradiol or testosterone rather than using gonadectomized animals with no hormone replacement. In the case of the female rat, daily s.c. injections of 1 μg estradiol benzoate are sufficient to reduce leuteinizing hormone and to elevate prolactin to diestrous levels without inducing receptive behavior [1,95].
Although there are “chemical castration” alternatives to gonadectomy, these have drawbacks and have not been fully characterized in terms of their possible effects on pain/analgesia. For example, continuous GnRH can be used to shut down the hypothalamo–pituitary–gonadal axis in both males and females. However, elevated GnRH may interfere with some aspects of opioid analgesia [160] and may cause long-term enhancement of glutamatergic post-synaptic activity [218]. Inhibitors of aromatase, the enzyme necessary for the synthesis of estrogens from androgens, can be used to substantially reduce synthesis of estrogens, and 5-α-reductase inhibitors can be used to reduce dihydrotestosterone synthesis; however, these inhibitors may also reduce synthesis of other steroid hormones within these metabolic pathways. The androgen antagonist flutamide can be used to block the effects of androgens, but it can also affect aromatase activity that is induced by androgens [23] and can act directly as an androgen agonist in some tissues [131]. The estrogen receptor antagonist tamoxifen, like other selective estrogen receptor modulators, has been shown to act as a partial agonist in some peripheral tissues [92]. ICI 182780 is a selective estrogen receptor antagonist, but it does not cross the blood–brain barrier [208]. Ultimately, convergent approaches to manipulate gonadal hormones will provide the most definitive testing of hypotheses that gonadal hormones modulate pain/analgesia.
When using a gonadectomy/hormone replacement approach, several issues must be considered. First, an effect of gonadectomy (relative to gonadally intact controls) implicates a role for gonadal secretions in pain/analgesia, but does not implicate any specific hormone. For example, one cannot conclude that testosterone mediates a given outcome based only on a castration effect in a male. Rather, studies in which testosterone is replaced in castrated males are also necessary. Second, to study the origins of sex differences, it is important to make the sex hormone levels as similar as possible in males and females at the time of testing. That is, both sexes rather than just males should be tested with androgens, and both sexes rather than just females should be tested with estrogens. This approach enables one to assess whether the mechanisms in question are sexually differentiated. If both sexes respond similarly to the same hormone treatment – even if one sex does not normally experience that hormone state – it can be concluded that the mechanism is likely to be similar in the two sexes (that is, not sexually differentiated).
A third point regarding gonadectomy/hormone replacement approaches is that failure to obtain an ovariectomy effect in females does not necessarily mean that ovarian hormones do not modulate pain/analgesia, particularly if the comparison group of intact females is in unknown or low hormone stages (i.e., an ovariectomy effect in females may only be apparent if the intact control group is in proestrus or estrus, when gonadal hormones are at or near peak levels). Fourth, the timing of hormone administration may be critical: if hormone replacement begins weeks rather than days (or immediately) after gonadectomy, responsiveness to exogenous hormone administration may diminish, requiring higher doses or longer duration treatment to obtain comparable effects [38,51]. Moreover, for estradiol, the interval between the last injection and behavioral testing as well as the duration of hormone exposure may dramatically influence the outcome [42,128,150,171].
Another aspect of hormonal manipulations concerns the age at which they are done. In rodents, the effects of ovariectomy and estradiol replacement depend upon the age at which the surgery is done [33,203]. Furthermore, there are important species differences in the pattern of hormonal changes during the progression through reproductive senescence (sometimes called “estropause” [33]). Unlike mice and women, in whom both estradiol and progesterone levels fall to very low levels following reproductive senescence, when rats progress through estropause, their estradiol levels remain elevated [203].
In the absence of relevant data to guide the design of a hormone replacement protocol, administration of a dose that has been shown to maintain or reinstate sexual behavior is a reasonable starting point. However, the dose ranges of hormone replacement relevant to the reproductive system may not be equivalent to ranges that modulate pain/analgesia. Even within the reproductive system, tissue sensitivities to estradiol vary widely [99]. Thus, reasonable starting doses for estradiol in ovariectomized rats would be in the range of 2 μg estradiol benzoate s.c., with testing beginning 24–48 h later; this dose/test interval has been shown to mimic proestrus–estrus, both behaviorally and in terms of plasma hormone levels [13]. Likewise, 500 μg of s.c. progesterone is a reasonable starting point for progestin replacement, with testing beginning 4–6 h later [58]. Of course, these testing intervals assume a nuclear steroid receptor-mediated (genomic) effect, whereas recent reports indicate that gonadal steroids may modulate pain thresholds at considerably shorter intervals [57]. Thus, it is important to consider shorter treatment-test intervals as well. For in vitro preparations, 100–1000 × Kd may be a reasonable starting dose to saturate a receptor [100], followed by decreasing the dose until the effect of interest disappears.
No obvious rationale exists for examining the influence of progesterone alone in a gonadectomized animal (other than as a control for progesterone + other hormone combinations), because gonadectomized humans are not exposed to progesterone alone under any known clinical treatment condition. However, it would be informative to test progestins and estrogens alone and in combination in gonadally intact animals, to model various clinical hormone treatments in humans (e.g., [48]).
3.5. Hormone manipulations: human studies
In human studies it is often impractical or unethical to manipulate hormones. However, women taking contraceptives for birth control or other reasons (and men taking androgens) can be studied. Additionally, short-term hormone administration is feasible (e.g., [187]). Hormone replacement and supplementation therapies differ markedly in the particular androgens, estrogens, and progestins they contain; these should always be clearly specified, as the various hormones likely exert different effects.
3.6. What types of pain tests are appropriate? Animal studies
The model system that is most appropriate is entirely hypothesis-driven. In animals, although acute pain tests such as the tail-flick test may not model clinical human pain per se, many advances have been made in understanding mechanisms of pain using such models. Face validity is less critical than using the model that is most appropriate to studying the specific mechanism of interest. In other words, mechanism “translates” better than phenomenology. A variety of approaches (e.g., visceral vs. cutaneous pain, acute vs. chronic [inflammatory or neuropathic] pain, behavioral vs. electrophysiological vs. molecular measures) are all worth pursuing, because they may reveal sex differences that have not yet been observed. Many existing pain models have not yet been applied to females, and animal models for female-specific pain syndromes are needed. In any model, the intensity of the noxious stimulus should be carefully considered. High-intensity stimuli are likely to result in a ceiling effect in which all subjects (or cells, etc.) respond at the limit of their capacity, thereby potentially obscuring individual differences (e.g., sex differences). Examination of more than one stimulus intensity is valuable in determining the generalizability of the sex difference.
As noted in reviews, sex differences in acute pain models have been observed, but are often protocol-, species-, and strain-dependent [140]. Very few studies have investigated sex differences in chronic pain models such as nerve injury and persistent inflammation. Notable exceptions include nerve ligation [40,113,195] and arthritis studies [4,39]. This dearth of information makes it premature to suggest which protocols or animal species are most relevant to any particular human pain condition. One valuable approach involves parallel testing in the animal and human laboratory (e.g., [29]).
3.7. What types of pain tests are appropriate? Human studies
In contrast to the robust sex difference found in the prevalence and severity of many chronic pain conditions, reported sex differences in experimental pain responsiveness, while generally consistent in direction, are often subtle in magnitude and sometimes absent. Sex differences may be more consistently observed when using particular stimulus modalities or psychophysical protocols. Specifically, a meta-analysis reported that sex differences in threshold and tolerance measures were largest and most consistently found for pressure pain and electrical stimulation, while smallest and least consistently found for thermal pain stimuli [164].
With respect to visceral pain, a lower pain threshold to esophageal distension was demonstrated in females [149], whereas rectal stimulation studies showed no gender differences in mechanical thresholds [11,186], or higher thresholds in healthy women [34]. Additionally, women have shown larger referred pain areas to the mechanical and thermal stimulation of the esophagus [161]. Characterizing sex differences in visceral pain, even with the limited number of studies published, is complicated. As with sex differences in somatic pain, detailed evaluations of visceral pain will be necessary to determine the mechanisms responsible.
Studies should include a range of stimulus intensities, as assessments of threshold or only mildly painful stimuli could fail to reveal differences that are manifest with more intensely noxious stimuli. Similarly, different physiological and psychological mechanisms operate in acute vs. sustained pain, such that sex/gender differences may be more prominent in tests of sustained pain.
Studies of experimentally induced hyperalgesia have demonstrated robust sex differences [29,70,71], but not all aspects of pain show significant sex differences in these models. Such observations provide the opportunity to selectively evaluate different mechanisms of hyperalgesia, and identify those in which sex is a significant factor.
When testing pain sensitivity of persons with clinical pain, it may be informative to use quantitative tests that are closely related to and replicate the clinical pain, as well as stimuli that differ from it in location and/or quality. The decision on these options should be based on the questions posed. For instance, evaluation of pain sensitivity at asymptomatic body sites can reveal information about general pain-processing alterations, as has been shown for fibromyalgia [118,189], various types of headaches [182], and temporomandibular disorders (TMD) [175]. Additionally, experimental provocation of a patient’s clinical pain allows separate assessment of that pathological condition, for instance evaluating pressure pain sensitivity of symptomatic muscles of fibromyalgia patients [188], or rectosigmoid distension of irritable bowel syndrome patients [34].
It is important to document as much of the experimental testing situation as possible. For example, experimenter (or clinician) sex should always be reported, as this variable may influence pain report in the laboratory (e.g., [14,76,94,125]) and in the clinic [133]. Other relevant factors to document include: (1) a detailed description of instructions to subjects and the training they received prior to data collection; (2) the history of subjects’ pain experiences; and (3) the history of subjects’ experience with similar experimental studies.
The goal of providing such information is to characterize the context of the experimental testing situation, and importantly, the subjects’ reaction to the context. While it is relatively simple to document the environmental features of the testing situation, it is more complicated – but likely more relevant – to document the subjects’ perception of and reaction to the testing environment. One example is the anxiety or stress that the subject feels in the testing environment. These states can vary substantially among subjects, and there is considerable evidence that stress or anxiety level influences pain perception, often in a sex-dependent manner [91]. Accordingly, it is valuable to document both the environmental conditions and the subjective state of the participants at the time of evaluation. Decidedly relevant factors are identified in Table 1 under “Context”.
Table 1.
Factors decidedly or likely relevant to sex differences in experimental studies of human pain
| Stimulus | Context | Individual | Response measures |
|---|---|---|---|
| Modality | Threat/safety | History | Threshold |
| Location | Stress | Age | Tolerance |
| Timing | Time of testing | Coping | Suprathreshold scaling |
| Tissue type | Experimenter gender | Genetic background | Stimulus discriminability |
| Phasic/tonic | Contingency | Race/ethnicity | Reflex |
| Sleep history | Hormonal status | Imaging | |
| Co-stimulation (odor, sounds, etc.) | Anxiety (trait and state) | Cardiovascular system | |
| Reproductive status (females) | |||
| Social environment | Communication (extent and style) | ||
| Attention | |||
| Expectation | |||
| Mood state |
Many variables other than a person’s sex or gender account for individual differences in pain sensitivity. Thus, sex differences may be more prominent in one sample than another due to differences in other sample characteristics. It is important to document the characteristics of the study population as thoroughly as possible; a list of relevant characteristics is presented in Table 1 under “Individual Factors.” Many of these factors are also relevant to clinical pain research.
4. Clinical and psychosocial study of sex and gender differences in pain and analgesia
Clinical pain research is defined as observational or experimental research with human subjects who have clinical pain conditions. Psychosocial pain research is the study of the cognitive and affective aspects of pain experiences, as well as social and psychological variables that influence risk for experiencing pain, manifestation of pain conditions, and treatment outcomes. Clinical and psychosocial research on sex and gender differences in pain is important for the following reasons:
Findings from clinical research are more directly relevant to clinical pain – and the relief of clinical pain – than are findings from studies involving laboratory study of animals or healthy, pain-free humans.
Sex and gender differences in pain are generally more pronounced in the clinic than in the laboratory. The higher prevalence of a wide range of clinical pain conditions in women than in men, coupled with the predominance of a few specific pain conditions in men (Table 2; [20]), suggests that (a) different clinical pain mechanisms may operate in men vs. women, (b) different or additional risk factors are relevant in one sex, or (c) differences compound such that small differences in mechanisms become large differences in morbidity and mortality through interactions with pharmacological and interventional therapies.
A review of studies conducted to date indicates that psychological and social variables powerfully influence pain, and can often explain more of the variance associated with pain than do biological variables – not only in clinical pain conditions, but also in the human laboratory [168,169,215].
Table 2.
Sex prevalence of various painful disorders
| Female prevalence | Male prevalence | No sex prevalence |
|---|---|---|
| Migraine headache with aura | Migraine without aura | Acute tension headache |
| Chronic tension headache | Cluster headache | Clustertic syndrome |
| Post-dural puncture headache | Post-traumatic headache | “Jabs” and “jolts” syndrome |
| Hemicrania continua | SUNCT syndrome | Secondary trigeminal neuralgia |
| Cervicogenic headache | Raeder’s paratrigeminal syndrome | Neuralgia of nervus intermedius |
| Tic douloureux | Pancoast tumor | Painful ophthalmoplegia |
| Temporomandibular joint disorder | Thromboangiitis obliterans | Maxillary sinusitis |
| Occipital neuralgia | Brachial plexus avulsion | Toothache due to dentinoenamel defects |
| Periapical periodontitis & abscess | Pancreatic disease | Toothache due to pulpitis |
| Atypical odontalgia | Duodenal ulcer | Cracked tooth syndrome |
| Burning tongue | Abdominal migraine | Dry socket |
| Carotidynia | Lateral femoral cutaneous neuropathy | Vagus nerve neuralgia |
| Chronic paroxysmal hemicrania | Post-herpetic neuralgia | Stylohyoid process syndrome |
| Temporal arteritis | Hemophilic arthropathy | Thoracic outlet syndrome |
| Carpal tunnel syndrome | Ankylosing spondylitis | Brachial plexus tumors |
| Raynaud’s disease | Esophageal motility disorders | |
| Chilblains | Chronic gastric ulcer | |
| Causalgia | Chron’s disease | |
| Reflex sympathetic dystrophy | Diverticular disease of colon | |
| Hemicrania continua | Carcinoma of the colon | |
| Chronic venous insufficiency | Familial Mediterranean fever | |
| Fibromyalgia syndrome | Hereditary coproporphyria | |
| Esophagitis | Acute herpes zoster | |
| Reflux esophagitis with peptic ulcer | Burns | |
| Slipping rib syndrome | ||
| Twelfth rib syndrome | ||
| Gallbladder disease | ||
| Post-cholecystectomy syndrome | ||
| Irritable bowel syndrome | ||
| Interstitial cystitis | ||
| Acute intermittent porphyria | ||
| Proctalgia fugax | ||
| Chronic constipation | ||
| Pyriformis syndrome | ||
| Peroneal muscular atrophy | ||
| Multiple sclerosis | ||
| Rheumatoid arthritis | ||
| Pain of psychological origin | ||
| Age dependent sex differences | ||
| Female prevalence | Male prevalence | |
| Gout (after age 60) | Gout (before age 60) | |
| Osteoarthritis (after age 45) | Osteoarthritis (before age 45) | |
| Livedo reticularis (after age 40) | Coronary artery disease (before age 65) | |
| Erythromelalgia (over age 50) | ||
Reproduced from [20], with permission from Cambridge University Press.
Basic science researchers often attempt to control a substantial number of individual differences (e.g., age, prior experience) in order to minimize “noise” when trying to identify and understand a specific mechanism underlying nociception or pain. In contrast, psychosocial research specifically examines these individual differences for their influence on pain. Research on sex and gender differences in clinical pain is necessarily complex because numerous factors that may influence the pain experience are themselves influenced by biological sex and by psychosocial factors. It is important to investigate how psychosocial variables differ in men and women, and how these variables interact with gender role and/or biological sex to influence the experience of pain in the two sexes. That is, to what extent are observed differences in clinical pain expression due to physiological differences, to differences in pathophysiology, and to psychosocial mediating factors? Factors to consider in planning clinical and psychosocial research on sex and gender differences in pain in human populations are described below.
4.1. Clinical and psychosocial factors of relevance to sex and gender influences on pain and analgesia
4.1.1. Age
The patterns of pain prevalence by age and sex differ for different pain conditions [120]. Many clinical pain conditions show no sex difference in prevalence before puberty, but show increased prevalence in one sex or the other (usually women) after puberty. Evidence suggests that the female prevalence in many common pain conditions increases across the pubertal period [123], and that the experience of multiple pain problems also becomes more common in girls as puberty progresses. Some of the differential in pain report among adolescents who seek care for chronic pain may be attributable to differences in coping strategies by gender, with females showing more catastrophizing, which is associated with higher pain levels [101]. Although it assumed that the pain behaviors of males and females are learnt through early experience, there is little research that explicitly examines the general development of sex differences in pain across the rapidly changing period of childhood and adolescence.
Some pain conditions, such as migraine headaches [180] and TMD [54], decline in prevalence after the fourth decade of life, whereas others, such as interstitial cystitis [45], joint pain and fibromyalgia [120], appear to persist until later ages. However, few studies have directly examined the relationship of specific pain problems to menopause. In addition, little information is available on the influence of sex/gender on the development and presentation of clinical pain in middle-aged and older adults, an age group frequently presenting with pain in clinical practice.
4.1.2. Race/ethnicity/culture
Few research studies have examined the influence of culture on gender-specific response to experimental pain or on presentation of clinical pain conditions. Cultural differences in gender-specific pain patterns would suggest sociocultural mechanisms, or possibly racial differences, whereas similarities across cultures would suggest biological or biopsychological mechanisms (e.g., [181]). There is evidence that culture/race interacts with gender on the experience of pain [59,147]. Future cross-cultural studies could be useful for illuminating mechanisms underlying sex differences in pain, although cultural and genetic factors may be difficult to differentiate.
4.1.3. History
In female-predominant pain disorders, physical abuse and sexual abuse appear to be related to pain and mood disorders [163]. For example, abuse history is associated with increased rates of pelvic pain in women [116]. However, these relationships are complex, with only certain aspects of pain or mood showing such relationships [35]. Few studies have examined sex or gender differences in the relationship between abuse and pain sensitivity [60]; clearly, more research is needed on this topic. Women are more likely to get post-infectious irritable bowel syndrome (IBS) than men [148], and chronic stress may be a risk factor. The number of existing pain conditions is a strong predictor of onset of new pain problems (e.g., [205]), and women are more likely to report multiple pains. Thus, pain history should be recorded in clinical studies.
4.1.4. Health vs. disease
A wide range of diseases have different prevalence rates and/or different presentations in males and females of the same age [63,157]. When possible, studies should compare not only women with pain to men with the same pain condition, but also healthy women to healthy men and patients of each sex to sex-matched healthy controls. For example, differences in symptoms and/or in pain sensitivity in the intestinal tract have been found between women with IBS and healthy women, between women with IBS and men with IBS, and between healthy women and healthy men [34]. Similarly, exaggerated temporal summation of pain has been documented for women with TMD, but not for men with TMD [174,175]. Moreover, researchers should be alert to the possibility that differences in presentation of disease between men and women may result in different diagnoses. In fact, it may be appropriate to develop sex/gender-specific diagnostic criteria for some pain conditions.
4.1.5. Comorbidities
Comorbidities are defined as: (1) pathological conditions, both physical and psychiatric, that exist in the patient with a pain condition; and (2) other symptoms that co-occur with pain that are not a direct result of the same condition. Investigations of comorbidities are important because: (1) they frequently occur; (2) they increase the burden of illness, which may affect treatment outcomes; (3) some comorbid conditions, notably depression, may share common mechanisms with pain; and (4) there are few relevant animal models. Women have more comorbid mood disorders [185], comorbid physical conditions [154], and numbers of somatic symptoms [204] than do men. Such comorbidities likely affect treatment outcomes [185]. Specifically, depression and anxiety are more common in women than in men, and genetic risk factors for mood disturbance may be more likely to result in these psychiatric disorders in women than in men [79,211]. Women have a larger number of comorbid pain conditions [120,123], and specific pain conditions with high female-to-male prevalence ratios may be etiologically related (e.g., [2]). Research is needed to determine whether comorbidities influence sex/gender differences in the effectiveness and side effects of specific treatments. For example, selective serotonin reuptake inhibitors (SSRIs) are more effective for women than for men for depression [106,197]; research is needed to determine whether this difference holds when SSRIs are used for pain.
4.1.6. Disability
Women are more likely than men to experience disability from the same pain condition [206]. In addition, patterns of disability may differ by sex [44,102,199]. Research is needed on why chronic pain is more likely to be disabling for women than for men.
4.1.7. Medications
Sex differences in the pharmacokinetic and pharmacodynamic properties of drugs [67], as well as in mechanisms of pain and analgesia, suggest that different medications may be more effective in one sex and that side-effect profiles and side-effect tolerance may differ between men and women. These variables can affect treatment adherence. Currently, some drugs are approved for use only in specific age groups, and recently a drug for the treatment of heart failure (BiDil®) was found to have differential effectiveness by race and was approved only for a specific racial group by the U.S. FDA [201]. Similarly, analgesic drug trials need to be powered to detect sex differences in effectiveness and side effects.
4.1.8. Physical variables
On average, blood pressure, height and weight differ by sex and these differences may affect response to a pain stimulus, as well as responses to pain treatment [3,61]. Physical variables should be measured and controlled for as much as possible.
4.1.9. Beliefs
Gender role expectations differ between sexes and are related to pain [137,169]. Studies of clinicians’ and patients’ perceptions/beliefs about pain and gender are needed.
4.1.10. Coping
Women with chronic pain seek more social support and use a wider range of coping strategies than men. They also report significantly more use of problem solving, positive self-statements, and palliative behaviors [200]. Female pain patients are more likely to catastrophize than male patients [96,101]. Studies are needed to assess the effectiveness of teaching male pain patients to use a range of additional coping strategies. Studies are also needed on the effectiveness of interventions to decrease catastrophizing in women with pain.
4.1.11. Mood
Women have higher levels of anxiety than men, and some studies suggest that anxiety and pain may be more closely related in men than in women [85,91]. However, there are exceptions. In clinic patients with pain, there are sex differences in level of mood disturbance (e.g., anxiety and depression symptom levels), but it is not clear whether they simply reflect the higher prevalence of mood disturbance among women in the general population. Possible mechanisms for the relationship of pain to mood and comorbidities include central sensitization and the balance of descending inhibition and descending facilitation [194].
4.1.12. Clinic vs. community
Sex and gender differences in pain may differ in clinical versus community populations. Although female-to-male ratios for pain may be substantial in the general population, these ratios are usually even larger among treatment seekers. However, treatment seeking is also related to pain level [207]. Women in the community report higher pain levels on average than men, which may explain the increased female-to-male ratio in clinical settings. In contrast, pain characteristics of men and women in treatment settings may not differ greatly [28,166]. Studies of community populations are needed to tease apart sex/gender-related risk factors for pain vs. treatment seeking.
4.1.13. Other psychosocial factors
A single cross-sectional study shows that the relationship of number of social roles and presence of pain differs by age and pain condition in women [119]. Studies are needed on gender differences in the effect of living arrangements, employment history, social support, marital status, and family composition on pain and pain outcomes (e.g., [68]).
5. Translational considerations for the study of sex differences in pain and analgesia
Translational research is an iterative process. While “translational” is generally regarded as applying knowledge from animal studies to human studies and eventually clinical practice, a more valuable model is presented in Fig. 2. Specifically, to complete the information flow, clinical experience and human experimental research findings should inform animal research. Such interactions exist for some recent studies of sex differences in pain, as demonstrated by the two examples that follow: temporal summation and opioid analgesia.
Fig. 2.
The full cycle of translational research.
5.1. Examples of translational research
5.1.1. Temporal summation of pain
The physiological phenomenon of “wind-up” was originally observed in the feline spinal cord in response to electrical stimulation of primary afferents [135]. Subsequent studies elaborated the conditions necessary for wind-up (e.g., C-fiber stimulation, interstimulus intervals of 5 s or less, NMDA-receptor activation) and extended observations to thermal and mechanical stimuli. Although wind-up is a transient upregulation of post-synaptic responsiveness to C-fiber input, it shares some properties with central sensitization, which is a long-term upregulation of post-synaptic response to a wider range of inputs. Thus, one could envision wind-up as a gateway to central sensitization, a potential factor in several chronic pain conditions [162].
As a first step in translation, a psychophysical correlate of wind-up was sought, and referred to as the temporal summation (TS) of pain [156]. Like wind-up, it required C-fiber stimulation, short interstimulus intervals, and NMDA-receptor activation [202]. As TS was explored further, studies reported that women showed greater temporal summation of pain than men [62,176,178]. The sex difference in TS could be attributed to factors other than wind-up, as suggested by studies pointing to gender role expectations as associated factors [167].
In another translational step, TS was found to be significantly more enhanced in women with chronic pain conditions such as fibromyalgia [188–190] and TMD [132,175]. This phenomenon was observed even in asymptomatic body sites. Because fibromyalgia and TMD are significantly more prevalent in women than men, it has been suggested that the naturally greater TS in women put them in a position to be more easily upregulated into a pathological state [177]. While this concept remains speculative, it should direct attention to altered CNS processing of nociceptive signals as at least one factor underlying the chronic pain of conditions with higher female prevalence.
5.1.2. Opioid analgesia
Another translational example involves the identification of a sex-dependent genetic association with opioid analgesia. Based on mouse strain surveys and subsequent genetic linkage mapping in mice, Mogil and colleagues determined that mutations of the murine melanocortin-1-receptor gene (Mc1r) influenced κ-opioid analgesia in a sex-dependent manner. Because most redheaded, fair-skinned humans show functional mutations of the human MC1R gene, a study of pentazocine analgesia was conducted in redheads. Consistent with the mouse data, women with two variant MC1R alleles displayed significantly greater analgesic responses to pentazocine on thermal and ischemic pain stimuli compared to women with either one or no variant MC1R alleles and men [143]. Thus, a novel sex-dependent genetic association with mixed action (κ/μ) opioid analgesia was successfully translated from mice to humans.
5.2. Future translational studies
Translational pain research could be aided by bringing tools and knowledge from other areas of neuroscience. Areas of particular value include affective, cognitive, and autonomic neuroscience, as well as the fields of stress and addition research. While these areas overlap with pain research to some extent, the sharing of translational models would be of value all around.
The discussion above hints at the significant gains that could be made from deliberate attempts at translational research. To assist in this effort, our field should promote increased communication among basic scientists, translational researchers, and clinicians dealing with pain patients. While pain research has developed such communication channels to some degree, as reflected in national and international scientific meetings, there is significant room for improvement. An important step would be organizing training programs (graduate, postgraduate, fellowships) to include substantive experience in all domains of the translational model [219].
6. Is there enough evidence to warrant sex-specific pain interventions?
The evidence does not appear strong enough to warrant sex-specific pain interventions in most situations. Initial studies [72,73] found that mixed action (κ/μ) opioid drugs produced greater analgesia after third molar extraction in women than in men. However, later human and animal research has produced equivocal results regarding sex differences in opioid analgesia [43]. Some evidence indicates that serotonergic agents (5HT4 agonists, 5HT3 antagonists) may be more efficacious in alleviating IBS symptoms in women than in men [30,97,145,151]. However, these clinical trials have been criticized because the higher frequency of IBS in females skewed the sex distribution. Studies with larger numbers of males should be conducted. Furthermore, research into the mechanisms by which these drugs produce their effects is needed in order to explain why a unique serotonin receptor pharmacology is specifically relevant to IBS, and also the significant influence of estrogens on this system [22]. There may be female-specific pain mechanisms that are yet to be elucidated, and these may lead to novel therapeutic approaches for pain in women. A prime example is the recent report that the antinociception resulting from the i.t. application of morphine requires the functional recruitment of spinal dynorphin in females, but not males [127].
Alongside studies of pharmacological interventions, a few non-pharmacological treatment studies have examined the potential for sex effects [90,103,109]. However, findings are mixed, and more studies are required that not only consider whether men and women respond differently to such interventions, but also compare effects for different pain conditions and treatment approaches. Including sex as a factor in clinical trials and reporting any differences in outcomes are paramount in addressing the lack of research in this area.
7. Future directions
The main goals of research on sex differences in pain/analgesia are to: (1) determine mechanisms that contribute to the generally greater prevalence of pain in females than males, (2) discover how sex-specific mechanisms of pain/analgesia can be exploited to improve pain management for both sexes, and (3) determine differences in outcome when similar treatments (pharmacological, interventional, behavioral) are applied. To attain this goal, a number of important issues remain to be addressed. These are listed below, in no particular order of importance:
What are the hormonal vs. genetic (sex chromosome) contributions to sex differences in pain/analgesia?
Mouse models now exist to test whether mice of the same gonadal sex (either males or females), which differ in sex chromosome complement (XX vs. XY), have different phenotypes reflective of pain or analgesia. If XX and XY males, for example, differ in their response to pain, then one can conclude that Y chromosome genes present only in the XY mice, or X chromosome genes (present in different genomic doses in XX vs. XY, and with different parental genomic imprints), cause the difference [12,49,69,153]. The sex chromosome effect does not tell where the X or Y chromosome genes act to cause the sex difference, although direct actions of Y chromosome genes have been demonstrated in the brain [52]. These new mouse models offer the opportunity to discover previously unknown direct effects of specific X or Y chromosome genes, which influence phenotypes via mechanisms that are not mediated by sex hormones. The models also allow testing, for the first time, the interaction of effects between sex chromosome complement and gonadal hormones.
What is the contribution of local hormone effects to sex differences in pain/analgesia?
Many hormone effects on pain/analgesia that were initially thought to be due to gonadal release of hormone may actually be due to de novo hormone synthesis in tissues such as the brain and spinal cord (e.g., progesterone [136,184], estradiol [9,86,108]). For example, changes in spinal aromatase activity dramatically and immediately affected pain thresholds in the Japanese quail, without changes in plasma levels of gonadal steroids [56,57]. Future studies in which various steroidogenic enzyme inhibitors (or hormone agonists or antagonists) are locally infused would contribute to our understanding of how local changes in hormone action result in behavioral changes in sensitivity to pain and analgesia.
How do psychological factors such as stress, mood, and conditioning (expectation) contribute to sex differences in pain/analgesia?
Psychosocial factors contribute substantially to pain perception in humans and may differentially influence pain in men and women [64,101,159,167,172]. There are well-documented sex differences in stress responses in both animals and humans [112], and sex differences in mechanisms of stress-induced analgesia have been reported in rodents [141]. Because pain is a stressful experience in itself, it is likely that sex differences in stress responses contribute to sex differences in pain. For instance, housing conditions (isolated vs. grouped) significantly affect the onset of inflammatory responses in rats. Furthermore, sex differences in acute stress effects on the inflammatory response are dependent on the housing conditions of the animals [84]. Social factors can be examined in rodents, as in a recent study demonstrating modulation of pain sensitivity in mice as a function of witnessing their cagemates (but not strangers) in pain [114]. Further animal and human research is necessary to reveal the extent to which psychological and social factors contribute to sex differences in pain/analgesia, and the mechanisms by which they do so. Additional research is also needed on how observers’ perceptions of pain are related to the sex/gender of the person experiencing pain.
How does pain chronicity contribute to sex differences in pain/analgesia?
For ethical and practical reasons, most animal studies to date have used acute painful stimuli, despite the facts that (a) the most robust and striking sex differences in pain in humans are the 2- to 6-fold greater prevalence and greater intensity of chronic pain syndromes in women compared to men [199], and (b) the most pressing need for research advances is for alleviation of chronic, severe pain. Because women are more likely than men to have a history of clinical pain experiences, and pain history influences current pain perception [170], chronicity of pain is most likely an important contributing factor to sex differences in pain/analgesia. Animal studies can be utilized to determine whether sex differences in pain/analgesia are amplified as the duration of persistent pain lengthens [39,89,210], or as subjects experience repeated episodes of pain over time. Repeated episodes of formalin testing engender adaptations in nociception that are gonadal hormone-dependent [7,31], suggesting that pain chronicity is indeed an important factor to consider in future preclinical studies of sex differences in pain/analgesia. The extent to which chronic pain or analgesic use alters an individual’s circulating gonadal hormones (e.g., [8,10,47,104]), which can in turn affect their pain/analgesic sensitivity, should also be considered.
To what extent are sex differences in pain or analgesia due to sexually dimorphic ascending (afferent) pathways vs. sexually dimorphic pain modulation?
Some pathological pain states might be attributable to inadequate tonic levels of endogenous analgesia rather than (or along with) sensitization of the nociceptive system. For example, a growing literature documents that human sufferers of complex pain disorders such as fibromyalgia are impaired in their ability to recruit endogenous pain inhibitory mechanisms [107,117]. Staud and colleagues [191] found that diffuse noxious inhibitory control (DNIC)-induced attenuation of experimental pain “wind-up” was absent in normal females and fibromyalgia patients, suggesting that women may be overrepresented among fibromyalgia patients precisely because of this deficiency. Moreover, hypertonic saline-induced muscle pain activates brain μ-opioid receptors less in women than in men [221], and brain μ-opioid receptor activation is estradiol-dependent in women [187]. The spinal cord endorphin/μ-opioid receptor analgesic system is more robust and ‘higher gain’ in male vs. female rodents, which, if also true for humans, could be one mechanism underlying the greater female prevalence and intensity of chronic pain syndromes [81]. Sex differences in the anatomy and physiology of endogenous descending pain modulatory pathways have been reported in the rat [129,130]. These pathways are also sexually dimorphic in terms of their activation by persistent pain as well as in their responsiveness to exogenous opioids. Given that most previous studies characterizing the anatomical and physiological organization of pain pathways were conducted in males, these results highlight the necessity of including female subjects in all experimental paradigms, and further suggest the need for a reevaluation of conclusions based on the previous anatomical studies.
What are the cellular and molecular bases of sex differences in and hormonal modulation of pain/analgesia?
Investigators should focus studies on qualitative rather than simply quantitative sex differences, the former referring to whether mechanisms underlying pain-related responses are fundamentally different in females versus males. We know little about the cellular mechanisms of steroid action in the brain, especially with regard to pain/analgesia. Many of the central regions implicated in pain and analgesia (i.e., periaqueductal gray, spinal cord, dorsal root ganglion) contain receptors for both estrogens and androgens and have the ability to synthesize steroids locally [18,56,146]. Binding of specific steroids to their receptors within these central and peripheral regions is likely involved in ligand-dependent transcriptional events, thereby influencing the expression of various neurotransmitters and receptors. Future studies are needed to further explore steroid-induced cellular consequences such as μ-opioid receptor internalization [55], uncoupling of the μ-opioid receptor from such downstream targets as ion channels [98] and regulators of gene expression, synthesis of endogenous neurosteroids that might modulate pain [155], and variables regulating the inflammatory response in chronic pain such as prostaglandins and cytokines [212]. Moving beyond steroids and steroid receptors may reveal new cellular pathways that mediate sex differences in sensitivity to pain and analgesia.
How do sex differences in pain/analgesia change over the lifespan?
The vast majority of animal and human studies have been conducted in relatively young, healthy adult subjects. A few studies suggest that sex differences in pain/analgesia develop by the early neonatal period in the rodent [37,110,192], although it is not clear whether sex differences are observed that early in humans [65,80,152]. In contrast, beginning around puberty, age-dependent sex differences occur for several types of pain in humans. Animal models can be readily employed to determine sex differences in pain/analgesia over the lifespan, although pursuing this question will require continued development of age-appropriate and more comprehensive pain tests in animals. Additionally, a body of research exists on pain-related gender roles in college-aged men and women (at least in the United States), but we know very little about generational differences and change in pain-related gender roles over the lifespan. The importance of this issue is escalating as life expectancy increases world-wide.
Should diagnostic criteria for certain pain-related conditions differ by sex?
It is recommended that researchers use the same core instruments for measurement in both sexes, but investigate whether additional questions or tests need to be added for one sex or the other. Research is also needed on whether the form of specific diagnostic questions should differ for male and female patients.
Are there factors that lead to chronic pain resilience or chronic pain susceptibility?
Research is needed on sex/gender differences in factors that protect against developing a pain problem, or, when pain is present, prevent debilitating pain. Further research is also necessary to determine the impact of pain and trauma during the perinatal period on pain sensitivity and responsiveness to reinjury in adulthood. For example, a recent study in rats reports that long-term negative consequences of neonatal inflammatory pain are significantly exacerbated in females in comparison to males [115].
Can existing data be better exploited?
Existing clinical databases should be used to assess sex differences in the effectiveness of clinical treatments, including psychological, physical medicine, and medication treatments. For example, female–male comparisons of the analgesic effects of pain medications (measured in opioid equivalents), as well as of the effectiveness of SSRIs for pain, should be conducted.
8. Recommendations to governments and professional and research bodies
Clinical trial methods, analysis, and reporting should be modified such that subject flow through the study and reports of treatment effects (both positive effects and adverse events) is broken out by sex, e.g., through updated CONSORT guidelines.
Both sexes should be included in medication trials in sufficient numbers to detect sex or gender effects. Report of outcomes in each sex should also be mandated in medication trials. Governmental regulatory bodies are in a position to implement these recommendations.
Acknowledgments
We thank the following sponsors for their support of the conference, which led to the development of this report: Merck Research Laboratories, University of Maryland Dental School, University of Maryland Research Center for Neuroendocrine Influences on Pain, UCLA Center for Neurovisceral Studies and Women’s Health, University of Maryland Women’s Health Research Group, University of Maryland Medical Center, American Pain Foundation, Fannie E. Ripple Foundation, PriCara, Johnson & Johnson Pharmaceutical Research and Development.
References
- 1.Ajika K, Krulich L, Fawcett CP, McCann SM. Effects of estrogen on plasma and pituitary gonadotropins and prolactin, and on hypothalamic releasing and inhibiting factors. Neuroendocrinology. 1972;9:304–15. doi: 10.1159/000122062. [DOI] [PubMed] [Google Scholar]
- 2.Akkus S, Senol A, Ayvacioglu N, Tunc E, Eren I, Isler M. Is female predominance in irritable bowel syndrome related to fibromyalgia? Rheumatol Int. 2004;24:106–9. doi: 10.1007/s00296-003-0328-x. [DOI] [PubMed] [Google Scholar]
- 3.al’Absi M, Buchanan TW, Marrero A, Lovallo WR. Sex differences in pain perception and cardiovascular responses in persons with parental history for hypertension. Pain. 1999;83:331–8. doi: 10.1016/s0304-3959(99)00122-0. [DOI] [PubMed] [Google Scholar]
- 4.Allen JB, Blatter D, Calandra GB, Wilder RL. Sex hormonal effects on the severity of streptococcal cell wall-induced polyarthritis in the rat. Arthritis Rheum. 1983;26:560–3. doi: 10.1002/art.1780260418. [DOI] [PubMed] [Google Scholar]
- 5.Aloisi AM. Gonadal hormones and sex differences in pain reactivity. Clin J Pain. 2003;19:168–74. doi: 10.1097/00002508-200305000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Aloisi AM, Bonifazi M. Sex hormones, central nervous system and pain. Horm Behav. 2006;50:1–7. doi: 10.1016/j.yhbeh.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 7.Aloisi AM, Ceccarelli I, Fiorenzani P. Gonadectomy affects hormonal and behavioral responses to repetitive nociceptive stimulation in male rats. Ann NY Acad Sci. 2003;1007:232–7. doi: 10.1196/annals.1286.022. [DOI] [PubMed] [Google Scholar]
- 8.Aloisi AM, Pari G, Ceccarelli I, Vecchi I, Ietta F, Lodi L, et al. Gender-related effects of chronic non-malignant pain and opioid therapy on plasma levels of macrophage migration inhibitory factor (MIF) Pain. 2005;115:142–51. doi: 10.1016/j.pain.2005.02.019. [DOI] [PubMed] [Google Scholar]
- 9.Amateau SK, Alt JJ, Stamps CL, McCarthy MM. Brain estradiol content in newborn rats: sex differences, regional heterogeneity, and possible de novo synthesis by the female telencephalon. Endocrinology. 2004;145:2906–17. doi: 10.1210/en.2003-1363. [DOI] [PubMed] [Google Scholar]
- 10.Amini H, Ahmadiani A. In vivo evidence for an increase in 5alpha-reductase activity in the rat central nervous system following morphine exposure. Int J Dev Neurosci. 2005;23:621–6. doi: 10.1016/j.ijdevneu.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 11.Arendt-Nielsen L, Bajaj P, Drewes AM. Visceral pain: gender differences in response to experimental and clinical pain. Eur J Pain. 2004;8:465–72. doi: 10.1016/j.ejpain.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 12.Arnold AP, Burgoyne PS. Are XX and XY brain cells intrinsically different? Trends Endocrinol Metab. 2004;15:6–11. doi: 10.1016/j.tem.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 13.Asarian L, Geary N. Cyclic estradiol treatment normalizes body weight and restores physiological patterns of spontaneous feeding and sexual receptivity in ovariectomized rats. Horm Behav. 2002;42:461–71. doi: 10.1006/hbeh.2002.1835. [DOI] [PubMed] [Google Scholar]
- 14.Aslaksen PM, Myrbakk IN, Hoifodt RS, Flaten MA. The effect of experimenter gender on autonomic and subjective responses to pain stimuli. Pain. 2007;129:260–8. doi: 10.1016/j.pain.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 15.Bajaj P, Bajaj P, Madsen H, Arendt-Nielsen L. A comparison of modality-specific somatosensory changes during menstruation in dysmenorrheic and nondysmenorrheic women. Clin J Pain. 2002;18:180–90. doi: 10.1097/00002508-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Bajaj P, Bajaj P, Madsen H, Moller M, Arendt-Nielsen L. Antenatal women with or without pelvic pain can be characterized by generalized or segmental hypoalgesia in late pregnancy. J Pain. 2002;3:451–60. doi: 10.1054/jpai.2002.128065. [DOI] [PubMed] [Google Scholar]
- 17.Becker JB, Arnold AP, Berkley KJ, Blaustein JD, Eckel LA, Hampson E, et al. Strategies and methods for research on sex differences in brain and behavior. Endocrinology. 2005;146:1650–73. doi: 10.1210/en.2004-1142. [DOI] [PubMed] [Google Scholar]
- 18.Bennett HL, Gustafsson JA, Keast JR. Estrogen receptor expression in lumbosacral dorsal root ganglion cells innervating the female rat urinary bladder. Autonom Neurosci. 2003;105:90–100. doi: 10.1016/S1566-0702(03)00044-4. [DOI] [PubMed] [Google Scholar]
- 19.Berglund LA, Simpkins JW. Alterations in brain opiate receptor mechanisms on proestrous afternoon. Neuroendocrinology. 1988;48:394–400. doi: 10.1159/000125040. [DOI] [PubMed] [Google Scholar]
- 20.Berkley KJ. Sex differences in pain. Behav Brain Sci. 1997;20:371–80. doi: 10.1017/s0140525x97221485. [DOI] [PubMed] [Google Scholar]
- 21.Berkley KJ, Zalcman SS, Simon VR. Sex and gender differences in pain and inflammation: a rapidly maturing field. Am J Physiol Regul Integr Comp Physiol. 2006;291:R241–4. doi: 10.1152/ajpregu.00287.2006. [DOI] [PubMed] [Google Scholar]
- 22.Bethea CL, Lu NZ, Gundlah C, Streicher JM. diverse actions of ovarian steroids in the serotonin neural system. Front Neuroendocrinol. 2002;23:41–100. doi: 10.1006/frne.2001.0225. [DOI] [PubMed] [Google Scholar]
- 23.Beyer C, Green SJ, Hutchison JB. Androgens influence sexual differentiation of embryonic mouse hypothalamic aromatase neurons in vitro. Endocrinology. 1994;135:1220–6. doi: 10.1210/endo.135.3.8070366. [DOI] [PubMed] [Google Scholar]
- 24.Brobeck J, Wheatland M, Stominger JL. Variations in regulation of energy exchange associated with estrus, diestrus and pseudo-pregnancy in rats. Endocrinology. 1947;40:65–72. doi: 10.1210/endo-40-2-65. [DOI] [PubMed] [Google Scholar]
- 25.Brooks-Gunn J, Warren MP, Rosso J, Gargiulo J. Validity of self-report measures of girls’ pubertal status. Child Dev. 1987;58:829–41. [PubMed] [Google Scholar]
- 26.Buijs RM, Kalsbeek A. Hypthalamic intergration of central and peripheral clocks. Nat Rev Neurosci. 2001;2:521–6. doi: 10.1038/35081582. [DOI] [PubMed] [Google Scholar]
- 27.Buijs RM, Scheer FA, Kreier F, Yi C, Bos N, Goncharuk VD, et al. Organization of circadian functions: interaction with the body. In: Kalsbeek A, editor. Hypothalamic integration of energy metabolism. Elsevier; 2006. pp. 341–60. [DOI] [PubMed] [Google Scholar]
- 28.Bush FM, Harkins SW, Harrington WG, Price DD. Analysis of gender effects on pain perception and symptom presentation in temporomandibular pain. Pain. 1993;53:73–80. doi: 10.1016/0304-3959(93)90058-W. [DOI] [PubMed] [Google Scholar]
- 29.Cairns BE, Hu JW, Arendt-Nielsen L, Sessle BJ, Svensson P. Sex-related differences in human pain and rat afferent discharge evoked by injection of glutamate into the masseter muscle. J Neurophysiol. 2001;86:782–91. doi: 10.1152/jn.2001.86.2.782. [DOI] [PubMed] [Google Scholar]
- 30.Camilleri M, Mayer EA, Drossman DA, Heath A, Dukes GE, McSorley D, Kong S, Mangel AW, Northcutt AR. Improvement in pain and bowel function in female irritable bowel patients with alosetron, a 5-HT3 receptor antagonist. Aliment Pharmacol Ther. 1999;13:1149–59. doi: 10.1046/j.1365-2036.1999.00610.x. [DOI] [PubMed] [Google Scholar]
- 31.Ceccarelli I, Fiorenzani P, Massafra C, Aloisi AM. Repeated nociceptive stimulation induces different behavioral and neuronal responses in intact and gonadectomized female rats. Brain Res. 2006;1106:142–9. doi: 10.1016/j.brainres.2006.05.089. [DOI] [PubMed] [Google Scholar]
- 32.Cepeda MS, Farrar JT, Baumgarten M, Boston R, Carr DB, Strom BL. Side effects of opioids during short-term administration: effect of age, gender, and race. Clin Pharmacol Ther. 2003;74:102–12. doi: 10.1016/S0009-9236(03)00152-8. [DOI] [PubMed] [Google Scholar]
- 33.Chakraborty TR, Gore AC. Aging-related changes in ovarian hormones, their receptors, and neuroendocrine function. Exp Biol Med. 2004;229:977–87. doi: 10.1177/153537020422901001. [DOI] [PubMed] [Google Scholar]
- 34.Chang L, Mayer EA, Labus JS, Schmulson M, Lee OY, Olivas TI, et al. Effect of sex on perception of rectosigmoid stimuli in irritable bowel syndrome. Am J Physiol Regul Integr Comp Physiol. 2006;291:R277–84. doi: 10.1152/ajpregu.00729.2005. [DOI] [PubMed] [Google Scholar]
- 35.Ciccone DSP, Elliott DKB, Chandler HKP, Nayak SP, Raphael KGP. Sexual and physical abuse in women with fibromyalgia syndrome: a test of the trauma hypothesis. Clin J Pain. 2005;21:378–86. doi: 10.1097/01.ajp.0000149796.08746.ea. [DOI] [PubMed] [Google Scholar]
- 36.Ciccone GK, Holdcroft A. Drugs and sex differences: a review of drugs relating to anaesthesia. Br J Anaesth. 1999;82:255–65. doi: 10.1093/bja/82.2.255. [DOI] [PubMed] [Google Scholar]
- 37.Cicero TJ, Nock B, O’Connor L, Meyer ER. Role of steroids in sex differences in morphine-induced analgesia: activational and organizational effects. J Pharmacol Exp Ther. 2002;300:695–701. doi: 10.1124/jpet.300.2.695. [DOI] [PubMed] [Google Scholar]
- 38.Clark CR, MacLusky NJ, Parsons B, Naftolin F. Effects of estrogen deprivation on brain estrogen and progestin receptor levels and the activation of female sexual behavior. Horm Behav. 1981;15:289–98. doi: 10.1016/0018-506x(81)90018-0. [DOI] [PubMed] [Google Scholar]
- 39.Cook CD, Nickerson MD. Nociceptive sensitivity and opioid antinociception and antihyperalgesia in Freund’s adjuvant-induced arthritic male and female rats. J Pharmacol Exp Ther. 2005;313:449–59. doi: 10.1124/jpet.104.077792. [DOI] [PubMed] [Google Scholar]
- 40.Coyle DE, Sehlhorst CS, Mascari C. Female rats are more susceptible to the development of neuropathic pain using the partial sciatic nerve ligation (PSNL) model. Neurosci Lett. 1995;186:135–8. doi: 10.1016/0304-3940(95)11304-f. [DOI] [PubMed] [Google Scholar]
- 41.Craft RM. Sex differences in opioid analgesia: from mouse to man. Clin J Pain. 2003;19:175–86. doi: 10.1097/00002508-200305000-00005. [DOI] [PubMed] [Google Scholar]
- 42.Craft RM, Ulibarri C, Leitl MD, Sumner JE. Dose- and time-dependent estradiol modulation of morphine antinociception in adult female rats. Eur J Pain. 2007 doi: 10.1016/j.ejpain.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 43.Craft RM, Mogil JS, Maria Aloisi A. Sex differences in pain and analgesia: the role of gonadal hormones. Eur J Pain. 2004;8:397–411. doi: 10.1016/j.ejpain.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 44.Crook J, Moldofsky H. The probability of recovery and return to work from work disability as a function of time. Qual Life Res. 1994;3:S97–S103. doi: 10.1007/BF00433383. [DOI] [PubMed] [Google Scholar]
- 45.Curhan GC, Speizer FE, Hunter DJ, Curhan SG, Stampfer MJ. Epidemiology of interstitial cystitis: a population based study. J Urol. 1999;161:549–52. [PubMed] [Google Scholar]
- 46.Dahan A, Sarton E, Teppema L, Olievier C. Sex-related differences in the influence of morphine on ventilatory control in humans. Anesthesiology. 1998;88:903–13. doi: 10.1097/00000542-199804000-00009. [DOI] [PubMed] [Google Scholar]
- 47.Daniell HW. Hypogonadism in men consuming sustained-action oral opioids. J Pain. 2002;3:377–84. doi: 10.1054/jpai.2002.126790. [DOI] [PubMed] [Google Scholar]
- 48.Dawson-Basoa MB, Gintzler AR. 17-Beta-estradiol and progesterone modulate an intrinsic opioid analgesic system. Brain Res. 1993;601:241–5. doi: 10.1016/0006-8993(93)91716-6. [DOI] [PubMed] [Google Scholar]
- 49.De Vries GJ, Rissman EF, Simerly RB, Yang L-Y, Scordalakes EM, Auger C, et al. Sex chromosome effects on the induction of sexually dimorphic neural and behavioral development. J Neurosci. 2002;22:9005–14. doi: 10.1523/JNEUROSCI.22-20-09005.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.De Vries GJ. Minireview: sex differences in adult and developing brains: compensation, compensation, compensation. Endocrinology. 2004;145:1063–8. doi: 10.1210/en.2003-1504. [DOI] [PubMed] [Google Scholar]
- 51.Delville Y, Blaustein JD. Long-term ovariectomy and hormone-induced sexual behavior, progestin receptors, and hypothalamic morphology in female rats. Horm Behav. 1989;23:269–78. doi: 10.1016/0018-506x(89)90066-4. [DOI] [PubMed] [Google Scholar]
- 52.Dewing P, Chiang CWK, Sinchak K, Sim H, Fernagut PO, Kelly S, et al. Direct regulation of adult brain function by the male-specific factor SRY. Curr Biol. 2006;16:415–20. doi: 10.1016/j.cub.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 53.Dierschke DJ, Bhattacharya AN, Atkinson LE, Knobil E. Circhoral oscillations of plasma LH levels in the ovariectomized rhesus monkey. Endocrinology. 1970;87:850–3. doi: 10.1210/endo-87-5-850. [DOI] [PubMed] [Google Scholar]
- 54.Drangsholt MT, LeResche L. Temporomandibular disorder pain. In: Crombie IK, Croft PR, Linton SJ, LeResche L, Von Korff M, editors. Epidemiology of pain. Seattle: IASP Press; 1999. pp. 203–33. [Google Scholar]
- 55.Eckersell CB, Popper P, Micevych PE. Estrogen-induced alteration of mu-opioid receptor immunoreactivity in the medial preoptic nucleus and medial amygdala. J Neurosci. 1998;18:3967–76. doi: 10.1523/JNEUROSCI.18-10-03967.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Evrard HC. Estrogen synthesis in the spinal dorsal horn: a new central mechanism for the hormonal regulation of pain. Am J Physiol Regul Integr Comp Physiol. 2006;291:R291–9. doi: 10.1152/ajpregu.00930.2005. [DOI] [PubMed] [Google Scholar]
- 57.Evrard HC, Balthazart J. Rapid regulation of pain by estrogens synthesized in spinal dorsal horn neurons. J Neurosci. 2004;24:7225–9. doi: 10.1523/JNEUROSCI.1638-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fadem BH, Barfield RJ, Whalen RE. Dose–response and time-response relationships between progesterone and the display of patterns of receptive and proceptive behavior in the female rat. Horm Behav. 1979;13:40–8. doi: 10.1016/0018-506x(79)90033-3. [DOI] [PubMed] [Google Scholar]
- 59.Fillingim RB. Individual differences in pain responses. Curr Rheumatol Rep. 2005;7:342–7. doi: 10.1007/s11926-005-0018-7. [DOI] [PubMed] [Google Scholar]
- 60.Fillingim RB, Edwards RR. Is self-reported childhood abuse history associated with pain perception among healthy young women and men? Clin J Pain. 2005;21:387–97. doi: 10.1097/01.ajp.0000149801.46864.39. [DOI] [PubMed] [Google Scholar]
- 61.Fillingim RB, Maixner W. The influence of resting blood pressure and gender on pain responses. Psychosom Med. 1996;58:326–32. doi: 10.1097/00006842-199607000-00005. [DOI] [PubMed] [Google Scholar]
- 62.Fillingim RB, Maixner W, Kincaid S, Silva S. Sex differences in temporal summation but not sensory-discriminative processing of thermal pain. Pain. 1998;75:121–7. doi: 10.1016/S0304-3959(97)00214-5. [DOI] [PubMed] [Google Scholar]
- 63.Forrest JB, Vo Q. Observations on the presentation, diagnosis, and treatment of interstitial cystitis in men. Urology. 2001;57:26–9. doi: 10.1016/s0090-4295(01)01121-9. [DOI] [PubMed] [Google Scholar]
- 64.Frot M, Feine JS, Bushnell MC. Sex differences in pain perception and anxiety. A psychophysical study with topical capsaicin. Pain. 2004;108:230–6. doi: 10.1016/j.pain.2003.11.017. [DOI] [PubMed] [Google Scholar]
- 65.Fuller BF. Infant gender differences regarding acute established pain. Clin Nurs Res. 2002;11:190–203. doi: 10.1177/105477380201100207. [DOI] [PubMed] [Google Scholar]
- 66.Gandara BK, LeResche L, Mancl L. Patterns of salivary estradiol and progesterone across the menstrual cycle. Ann N Y Acad Sci. 2007;1098:446–50. doi: 10.1196/annals.1384.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gandhi M, Aweeka F, Greenblatt RM, Blaschke TF. Sex differences in pharmacokinetics and pharmacodynamics. Annu Rev Pharmacol Toxicol. 2004;44:499–523. doi: 10.1146/annurev.pharmtox.44.101802.121453. [DOI] [PubMed] [Google Scholar]
- 68.Gatchel RJ, Mayer TG, Kidner CL, McGeary DD. Are gender, marital status or parenthood risk factors for outcome of treatment for chronic disabling spinal disorders? J Occup Rehabil. 2005;15:191–201. doi: 10.1007/s10926-005-1218-8. [DOI] [PubMed] [Google Scholar]
- 69.Gatewood JD, Wills A, Shetty S, Xu J, Arnold AP, Burgoyne PS, et al. Sex chromosome complement and gonadal sex influence aggressive and parental behaviors in mice. J Neurosci. 2006;26:2335–42. doi: 10.1523/JNEUROSCI.3743-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gazerani P, Kaeseler Andersen O, Arendt-Nielsen L. A human experimental capsaicin model for trigeminal sensitization. Gender-specific differences. Pain. 2005;118:155–63. doi: 10.1016/j.pain.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 71.Gazerani P, Wang K, Cairns BE, Svensson P, Arendt-Nielsen L. Effects of subcutaneous administration of glutamate on pain, sensitization and vasomotor responses in healthy men and women. Pain. 2006;124:338–48. doi: 10.1016/j.pain.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 72.Gear RW, Gordon NC, Heller PH, Paul S, Miaskowski C, Levine JD. Gender difference in analgesic response to the kappa-opioid pentazocine. Neurosci Lett. 1996;205:207–9. doi: 10.1016/0304-3940(96)12402-2. [DOI] [PubMed] [Google Scholar]
- 73.Gear RW, Miaskowski C, Gordon NC, Paul SM, Heller PH, Levine JD. The kappa opioid nalbuphine produces gender- and dose-dependent analgesia and antianalgesia in patients with postoperative pain. Pain. 1999;83:339–45. doi: 10.1016/s0304-3959(99)00119-0. [DOI] [PubMed] [Google Scholar]
- 74.Gerall AA, Napoli AM, Cooper UC. Daily and hourly estrous running in intact, spayed, and estrone implanted rats. Physiol Behav. 1973;10:225–9. doi: 10.1016/0031-9384(73)90302-8. [DOI] [PubMed] [Google Scholar]
- 75.Giamberardino MA, Berkley KJ, Iezzi S, De Bigontina P, Vecchiet L. Pain threshold variations in somatic wall tissues as a function of menstrual cycle, segmental site and tissue depth in non-dysmenorrheic women, dysmenorrheic women and men. Pain. 1997;71:187–97. doi: 10.1016/s0304-3959(97)03362-9. [DOI] [PubMed] [Google Scholar]
- 76.Gijsbers K, Nicholson F. Experimental pain thresholds influenced by sex of experimenter. Percept Mot Skills. 2005;101:803–7. doi: 10.2466/pms.101.3.803-807. [DOI] [PubMed] [Google Scholar]
- 77.Gilger JW, Geary DC. Reliability and validity of retrospective self-reports of the age of pubertal onset using twin. Adolescence. 1991;26:41–54. [PubMed] [Google Scholar]
- 78.Greil H. Patterns of sexual dimorphism from birth to senescence. Coll Antropol. 2006;30:637–41. [PubMed] [Google Scholar]
- 79.Grillon C, Warner V, Hille J, Merikangas KR, Bruder GE, Tenke CE, et al. Families at high and low risk for depression: a three-generation startle study. Biol Psychiatry. 2005;57:953–60. doi: 10.1016/j.biopsych.2005.01.045. [DOI] [PubMed] [Google Scholar]
- 80.Guinsburg R, Peres CD, De Almeida MFB, Balda RDX, Berenguel RC, Tonelotto J, et al. Differences in pain expression between male and female newborn infants. Pain. 2000;85:127–33. doi: 10.1016/s0304-3959(99)00258-4. [DOI] [PubMed] [Google Scholar]
- 81.Gupta DS, von GH, Gintzler AR. Sex-/ovarian steroid-dependent release of endomorphin 2 from spinal cord. J Pharmacol Exp Ther. 2007;321:635–41. doi: 10.1124/jpet.106.118505. [DOI] [PubMed] [Google Scholar]
- 82.Hapidou EG, DeCatanzaro D. Responsiveness to laboratory pain in women as a function of age and childbirth pain experience. Pain. 1992;48:177–81. doi: 10.1016/0304-3959(92)90056-H. [DOI] [PubMed] [Google Scholar]
- 83.Harlow SD, Crawford S, Dennerstein L, Burger HG, Mitchell ES, Sowers MF. Recommendations from a multi-study evaluation of proposed criteria for staging reproductive aging. Climacteric. 2007;10:112–9. doi: 10.1080/13697130701258838. [DOI] [PubMed] [Google Scholar]
- 84.Hermes GL, Rosenthal L, Montag A, McClintock MK. Social isolation and the inflammatory response: sex differences in the enduring effects of a prior stressor. Am J Physiol Regul Integr Comp Physiol. 2006;290:R273–82. doi: 10.1152/ajpregu.00368.2005. [DOI] [PubMed] [Google Scholar]
- 85.Hirsh AT, Waxenberg LB, Atchison JW, Gremillion HA, Robinson ME. Evidence for sex differences in the relationships of pain, mood, and disability. J Pain. 2006;7:592–601. doi: 10.1016/j.jpain.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 86.Hojo Y, Hattori TA, Enami T, Furukawa A, Suzuki K, Ishii HT, et al. Adult male rat hippocampus synthesizes estradiol from pregnenolone by cytochromes P45017 alpha and P450 aromatase localized in neurons. Proc Natl Acad Sci USA. 2004;101:865–70. doi: 10.1073/pnas.2630225100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Holdcroft A, Snidvongs S, Cason A, Dore CJ, Berkley KJ. Pain and uterine contractions during breast feeding in the immediate post-partum period increase with parity. Pain. 2003;104:589–96. doi: 10.1016/S0304-3959(03)00116-7. [DOI] [PubMed] [Google Scholar]
- 88.Hughes RN. The categorisation of male and female laboratory animals in terms of gender. Brain Res Bull. 2003;60:189–90. doi: 10.1016/s0361-9230(03)00037-6. [DOI] [PubMed] [Google Scholar]
- 89.Hurley RW, Hammond DL. The analgesic effects of supraspinal mu- and delta-opioid receptor agonists are potentiated during persistent inflammation. J Neurosci. 2000;20:1249–59. doi: 10.1523/JNEUROSCI.20-03-01249.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jensen IB, Bergström G, Ljungquist T, Bodin L, Nygren ÅL. A randomized controlled component analysis of a behavioral medicine rehabilitation program for chronic spinal pain: are the effects dependent on gender? Pain. 2001;91:65–78. doi: 10.1016/s0304-3959(00)00420-6. [DOI] [PubMed] [Google Scholar]
- 91.Jones A, Zachariae R, Arendt-Nielsen L. Dispositional anxiety and the experience of pain: gender-specific effects. Eur J Pain. 2003:387–95. doi: 10.1016/S1090-3801(02)00139-8. [DOI] [PubMed] [Google Scholar]
- 92.Jordan VC. Antiestrogenic action of raloxifene and tamoxifen: today and tomorrow. J Natl Cancer Inst. 1998;90:967–71. doi: 10.1093/jnci/90.13.967. [DOI] [PubMed] [Google Scholar]
- 93.Juhl GI, Svensson P, Norholt SE, Jensen TS. Long-lasting mechanical sensitization following third molar surgery. J Orofac Pain. 2006;20:59–73. [PubMed] [Google Scholar]
- 94.Kallai I, Barke A, Voss U. The effects of experimenter characteristics on pain reports in women and men. Pain. 2004;112:142–7. doi: 10.1016/j.pain.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 95.Kalra PS, Fawcett CP, Krulich L, McCann SM. The effects of gonadal steroids on plasma gonadotropins and prolactin in the rat. Endocrinology. 1973;92:1256–68. doi: 10.1210/endo-92-4-1256. [DOI] [PubMed] [Google Scholar]
- 96.Keefe FJ, Lefebvre JC, Egert JR, Affleck G, Sullivan MJ, Caldwell DS. The relationship of gender to pain, pain behavior, and disability in osteoarthritis patients: the role of catastrophizing. Pain. 2000;87:325–34. doi: 10.1016/S0304-3959(00)00296-7. [DOI] [PubMed] [Google Scholar]
- 97.Kellow J, Lee OY, Chang FY, Thongsawat S, Mazlam MZ, Yuen H, et al. An Asia-Pacific, double blind, placebo controlled, randomised study to evaluate the efficacy, safety, and tolerability of tegaserod in patients with irritable bowel syndrome. Gut. 2003;52:671–6. doi: 10.1136/gut.52.5.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kelly MJ, Qiu J, Ronnekleiv OK. Estrogen modulation of G-protein-coupled receptor activation of potassium channels in the central nervous system. Ann N Y Acad Sci. 2003;1007:6–9. doi: 10.1196/annals.1286.001. [DOI] [PubMed] [Google Scholar]
- 99.Kelner MJ, Kirchick HJ, Peck EJ., Jr Differential sensitivity of estrogen target tissues: the role of the receptor. Endocrinology. 1982;111:1986–95. doi: 10.1210/endo-111-6-1986. [DOI] [PubMed] [Google Scholar]
- 100.Kenakin T. Pharmacologic analysis of drug-receptor interaction. 3. New York: Raven Press; 1997. [Google Scholar]
- 101.Keogh E, Eccleston C. Sex differences in adolescent chronic pain and pain-related coping. Pain. 2006;123:275–84. doi: 10.1016/j.pain.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 102.Keogh E, McCracken LM, Eccleston C. Gender moderates the association between depression and disability in chronic pain patients. Eur J Pain. 2006;10:413–22. doi: 10.1016/j.ejpain.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 103.Keogh E, McCracken LM, Eccleston C. Do men and women differ in their response to interdisciplinary chronic pain management? Pain. 2005;114:37–46. doi: 10.1016/j.pain.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 104.Khoromi S, Muniyappa R, Nackers L, Gray N, Baldwin H, Wong KA, et al. Effects of chronic osteoarthritis pain on neuroendocrine function in men. J Clin Endocrinol Metab. 2006;91:4313–8. doi: 10.1210/jc.2006-1122. [DOI] [PubMed] [Google Scholar]
- 105.Klerman EB, Goldenberg DL, Brown EN, Maliszewski AM, Adler GK. Circadian rhythms of women with fibromyalgia. J Clin Endocrinol Metab. 2001;86:1034–9. doi: 10.1210/jcem.86.3.7293. [DOI] [PubMed] [Google Scholar]
- 106.Kornstein SG, Schatzberg AF, Thase ME, Yonkers KA, McCullough JP, Keitner GI, et al. Gender differences in treatment response to sertraline versus imipramine in chronic depression. Am J Psychiatry. 2000;157:1445–52. doi: 10.1176/appi.ajp.157.9.1445. [DOI] [PubMed] [Google Scholar]
- 107.Kosek E, Hansson P. Modulatory influence on somatosensory perception from vibration and heterotopic noxious conditioning stimulation (HNCS) in fibromyalgia patients and healthy subjects. Pain. 1997;70:41–51. doi: 10.1016/s0304-3959(96)03295-2. [DOI] [PubMed] [Google Scholar]
- 108.Kretz O, Fester L, Wehrenberg U, Zhou L, Brauckmann S, Zhao S, et al. Hippocampal synapses depend on hippocampal estrogen synthesis. J Neurosci. 2004;24:5913–21. doi: 10.1523/JNEUROSCI.5186-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Krogstad BS, Jokstad A, Dahl BL, Vassend O. The reporting of pain, somatic complaints, and anxiety in a group of patients with TMD before and 2 years after treatment: sex differences. J Orofac Pain. 1996;10:263–9. [PubMed] [Google Scholar]
- 110.Krzanowska EK, Ogawa S, Pfaff DW, Bodnar RJ. Reversal of sex differences in morphine analgesia elicited from the ventro-lateral periaqueductal gray in rats by neonatal hormone manipulations. Brain Res. 2002;929:1–9. doi: 10.1016/s0006-8993(01)03350-9. [DOI] [PubMed] [Google Scholar]
- 111.Kuba T, Quinones-Jenab V. The role of female gonadal hormones in behavioral sex differences in persistent and chronic pain: clinical versus preclinical studies. Brain Res Bull. 2005;66:179–88. doi: 10.1016/j.brainresbull.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 112.Kudielka BM, Kirschbaum C. Sex differences in HPA axis responses to stress: a review. Biol Psychol. 2005;69:113–32. doi: 10.1016/j.biopsycho.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 113.LaCroix-Fralish ML, Tawfik VL, Spratt KF, DeLeo JA. Sex differences in lumbar spinal cord gene expression following experimental lumbar radiculopathy. J Mol Neurosci. 2006;30:283–95. doi: 10.1385/JMN:30:3:283. [DOI] [PubMed] [Google Scholar]
- 114.Langford DJ, Crager SE, Shehzad Z, Smith SB, Sotocinal SG, Levenstadt JS, et al. Social modulation of pain as evidence for empathy in mice. Science. 2006;312:1967–70. doi: 10.1126/science.1128322. [DOI] [PubMed] [Google Scholar]
- 115.LaPrairie JL, Murphy AZ. Female rats are more vulnerable to the long-term consequences of neonatal inflammatory injury. Pain. 2007;132(Suppl 1):S120–9. doi: 10.1016/j.pain.2007.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Latthe P, Mignini L, Gray R, Hills R, Khan K. Factors predisposing women to chronic pelvic pain: systematic review. BMJ. 2006;332:749–55. doi: 10.1136/bmj.38748.697465.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lautenbacher S, Rollman GB. Possible deficiencies of pain modulation in fibromyalgia. Clin J Pain. 1997;13:189–96. doi: 10.1097/00002508-199709000-00003. [DOI] [PubMed] [Google Scholar]
- 118.Lautenbacher S, Rollman GB, McCain GA. Multi-method assessment of experimental and clinical pain in patients with fibromyalgia. Pain. 1994;59:45–53. doi: 10.1016/0304-3959(94)90046-9. [DOI] [PubMed] [Google Scholar]
- 119.Lee C, Powers JR. Number of social roles, health, and well-being in three generations of Australian women. Int J Behav Med. 2002;9:195–215. doi: 10.1207/s15327558ijbm0903_03. [DOI] [PubMed] [Google Scholar]
- 120.LeResche L. Epidemiologic perspectives on sex differences in pain. In: Fillingim RB, editor. Sex, gender, and pain, progress in pain research and management. Vol. 17. Seattle: IASP Press; 2000. pp. 233–49. [Google Scholar]
- 121.LeResche L, Sherman JJ, Huggins KH, Saunders K, Mancl LA, Lentz G, et al. Musculoskeletal orofacial pain and other signs and symptoms of temporomandibular disorders during pregnancy: a prospective study. J Orofac Pain. 2005;19:193–201. [PubMed] [Google Scholar]
- 122.LeResche L, Mancl L, Sherman JJ, Gandara B, Dworkin SF. Changes in temporomandibular pain and other symptoms across the menstrual cycle. Pain. 2003;106:253–61. doi: 10.1016/j.pain.2003.06.001. [DOI] [PubMed] [Google Scholar]
- 123.LeResche L, Mancl LA, Drangsholt MT, Saunders K, Korff MV. Relationship of pain and symptoms to pubertal development in adolescents. Pain. 2005;118:201–9. doi: 10.1016/j.pain.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 124.Leshner AI, Collier G. The effects of gonadectomy on the sex differences in dietary self-selection patterns and carcass compositions of rats. Physiol Behav. 1973;11:671–6. doi: 10.1016/0031-9384(73)90253-9. [DOI] [PubMed] [Google Scholar]
- 125.Levine FM, De Simone LL. The effects of experimenter gender on pain report in male and female subjects. Pain. 1991;44:69–72. doi: 10.1016/0304-3959(91)90149-R. [DOI] [PubMed] [Google Scholar]
- 126.Liu NJ, Gintzler AR. Prolonged ovarian sex steroid treatment of male rats produces antinociception: identification of sex-based divergent analgesic mechanisms. Pain. 2000;85:273–81. doi: 10.1016/s0304-3959(99)00278-x. [DOI] [PubMed] [Google Scholar]
- 127.Liu NJ, von GH, Gintzler AR. Sexually dimorphic recruitment of spinal opioid analgesic pathways by the spinal application of morphine. J Pharmacol Exp Ther. 2007;322:654–60. doi: 10.1124/jpet.107.123620. [DOI] [PubMed] [Google Scholar]
- 128.Liuzzi FJ, Scoville SA, Bufton SM. Effects of short-term estrogen replacement on trkA mRNA levels in axotomized dorsal root ganglion neurons. Exp Neurol. 1999;159:433–40. doi: 10.1006/exnr.1999.7169. [DOI] [PubMed] [Google Scholar]
- 129.Loyd DR, Morgan MM, Murphy AZ. Morphine preferentially activates the periaqueductal gray-rostral ventromedial medullary pathway in the male rat: a potential mechanism for sex differences in antinociception. Neuroscience. 2007;147:456–68. doi: 10.1016/j.neuroscience.2007.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Loyd DR, Murphy AZ. Sex differences in the anatomical and functional organization of the periaqueductal gray-rostral ventromedial medullary pathway in the rat: a potential circuit mediating the sexually dimorphic actions of morphine. J Comp Neurol. 2006;496:723–38. doi: 10.1002/cne.20962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.MacLusky NJ, Hajszan T, Leranth C. Effects of dehydroepiandrosterone and flutamide on hippocampal CA1 spine synapse density in male and female rats: implications for the role of androgens in maintenance of hippocampal structure. Endrocrinology. 2004;145:4154–61. doi: 10.1210/en.2004-0477. [DOI] [PubMed] [Google Scholar]
- 132.Maixner W, Fillingim R, Sigurdsson A, Kincaid S, Silva S. Sensitivity of patients with painful temporomandibular disorders to experimentally evoked pain: evidence for altered temporal summation of pain. Pain. 1998;76:71–81. doi: 10.1016/s0304-3959(98)00028-1. [DOI] [PubMed] [Google Scholar]
- 133.Marquie L, Raufaste E, Lauque D, Marine C, Ecoiffier M, Sorum P. Pain rating by patients and physicians: evidence of systematic pain miscalibration. Pain. 2003;102:289–96. doi: 10.1016/S0304-3959(02)00402-5. [DOI] [PubMed] [Google Scholar]
- 134.McLean SA, Williams DA, Harris RE, Kop WJ, Groner KH, Ambrose K, et al. Momentary relationship between cortisol secretion and symptoms in patients with fibromyalgia. Arthritis Rheum. 2005;52:3660–9. doi: 10.1002/art.21372. [DOI] [PubMed] [Google Scholar]
- 135.Mendell LM. Physiological properties of unmyelinated fiber projection to the spinal cord. Exp Neurol. 1966;16:316–32. doi: 10.1016/0014-4886(66)90068-9. [DOI] [PubMed] [Google Scholar]
- 136.Micevych P, Sinchak K, Mills RH, Tao L, LaPolt P, Lu JKH. The luteinizing hormone surge is preceded by an estrogen-induced increase of hypothalamic progesterone in ovariectomized and adrenalectomized rats. Neuroendocrinology. 2003;78:29–35. doi: 10.1159/000071703. [DOI] [PubMed] [Google Scholar]
- 137.Miller C, Newton SE. Pain perception and expression: the influence of gender, personal self-efficacy, and lifespan socialization. Pain Manage Nurs. 2006;7:148–52. doi: 10.1016/j.pmn.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 138.Miller PB, Soules MR. The usefulness of a urinary LH kit for ovulation prediction during menstrual cycles of normal women. Obstet Gynecol. 1996;87:13–7. doi: 10.1016/0029-7844(95)00352-5. [DOI] [PubMed] [Google Scholar]
- 139.Mode A, Gustafsson J. Sex and the liver: a journey through five decades. Drug Metab Rev. 2006;38:197–207. doi: 10.1080/03602530600570057. [DOI] [PubMed] [Google Scholar]
- 140.Mogil JS, Chesler EJ, Wilson SG, Juraska JM, Sternberg WF. Sex differences in thermal nociception and morphine antinociception in rodents depend on genotype. Neurosci Biobehav Rev. 2000;24:375–89. doi: 10.1016/s0149-7634(00)00015-4. [DOI] [PubMed] [Google Scholar]
- 141.Mogil JS, Sternberg WF, Kest B, Marek P, Liebeskind JC. Sex differences in the antagonism of swim stress-induced analgesia: effects of gonadectomy and estrogen replacement. Pain. 1993;53:17–25. doi: 10.1016/0304-3959(93)90050-Y. [DOI] [PubMed] [Google Scholar]
- 142.Mogil JS, Chanda ML. The case for the inclusion of female subjects in basic science studies of pain. Pain. 2005;117:1–5. doi: 10.1016/j.pain.2005.06.020. [DOI] [PubMed] [Google Scholar]
- 143.Mogil JS, Wilson SG, Chesler EJ, Rankin AL, Nemmani KVS, Lariviere WR, et al. The melanocortin-1 receptor gene mediates female-specific mechanisms of analgesia in mice and humans. Proc Natl Acad Sci USA. 2003;100:4867–72. doi: 10.1073/pnas.0730053100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Morris ME, Lee HJ, Predko LM. Gender differences in the membrane transport of endogenous and exogenous compounds. Pharmacol Rev. 2003;55:229–40. doi: 10.1124/pr.55.2.1. [DOI] [PubMed] [Google Scholar]
- 145.Muller-Lissner SA, Fumagalli I, Bardhan KD, Pace F, Pecher E, Nault B, et al. Tegaserod, a 5-HT4 receptor partial agonist, relieves symptoms in irritable bowel syndrome patients with abdominal pain, bloating and constipation. Aliment Pharmacol Ther. 2001;15:1655–66. doi: 10.1046/j.1365-2036.2001.01094.x. [DOI] [PubMed] [Google Scholar]
- 146.Murphy AZ, Hoffman GE. Distribution of gonadal steroid receptor-containing neurons in the preoptic-periaqueductal gray-brainstem pathway: a potentia circuit for the initiation of male sexual behavior. J Comp Neurol. 2001;438:191–212. doi: 10.1002/cne.1309. [DOI] [PubMed] [Google Scholar]
- 147.Myers CD, Riley JL, Robinson ME. Psychosocial contributions to sex-correlated differences in pain. Clin J Pain. 2003;19:225–32. doi: 10.1097/00002508-200307000-00005. [DOI] [PubMed] [Google Scholar]
- 148.Neale KR, Hebden J, Spiller R. Prevalence of gastrointestinal symptoms six months after bacterial gastroenteritis and risk factors for development of the irritable bowel syndrome: postal survey of patients. BMJ. 1997;314:779–82. doi: 10.1136/bmj.314.7083.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Nguyen P, Lee SD, Castell DO. Evidence of gender differences in esophageal pain threshold. Am J Gastroenterol. 1995;90:901–4. [PubMed] [Google Scholar]
- 150.Nomikos G, Spyraki C, Kazandjian A, Sfikakis A. Estrogen treatment to ovariectomized rats modifies morphine-induced behavior. Pharmacol Biochem Behav. 1987;27:611–7. doi: 10.1016/0091-3057(87)90182-1. [DOI] [PubMed] [Google Scholar]
- 151.Nyhlin H, Bang C, Elsborg L, Silvennoinen J, Holme I, egg P, et al. A double-blind, placebo-controlled, randomized study to evaluate the efficacy, safety and tolerability of tegaserod in patients with irritable bowel syndrome. Scand J Gastroenterol. 2004;39:119–26. doi: 10.1080/00365520310006748. [DOI] [PubMed] [Google Scholar]
- 152.Owens ME, Todt EH. Pain in infancy: neonatal reaction to a heel lance. Pain. 1984;20:77–86. doi: 10.1016/0304-3959(84)90813-3. [DOI] [PubMed] [Google Scholar]
- 153.Palaszynski KM, Smith DL, Burgoyne PS, Arnold AP, Voskuhl RR. A yin-yang effect between sex chromosomes and sex hormones on the immune response. Endocrinology. 2005;146:3280–5. doi: 10.1210/en.2005-0284. [DOI] [PubMed] [Google Scholar]
- 154.Paykel ES, Brugha T, Fryers T. Size and burden of depressive disorders in Europe. Eur Neuropsychopharmacol. 2005;15:411–23. doi: 10.1016/j.euroneuro.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 155.Poisbeau P, Patte-Mensah C, Keller AF, Barrot M, Breton JD, Luis-Delgado OE, et al. Inflammatory pain upregulates spinal inhibition via endogenous neurosteroid production. J Neurosci. 2005;25:11768–76. doi: 10.1523/JNEUROSCI.3841-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Price DD. Characteristics of second pain and flexion reflexes indicative of prolonged central summation. Exp Neurol. 1972;37:371–87. doi: 10.1016/0014-4886(72)90081-7. [DOI] [PubMed] [Google Scholar]
- 157.Purnell B, Roberts L, Smith O. Vive la différence. Science. 2005;308:1569. [Google Scholar]
- 158.Quissel DO. Steroid hormone analysis in human saliva. Ann N Y Acad Sci. 1993;694:143–5. doi: 10.1111/j.1749-6632.1993.tb18348.x. [DOI] [PubMed] [Google Scholar]
- 159.Quiton RL, Greenspan JD. Sex differences in endogenous pain modulation by distracting and painful conditioning stimulation. Pain. 2007;132:S134–49. doi: 10.1016/j.pain.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Ratka A, Simpkins JW. A modulatory role for luteinizing hormone-releasing hormone in nociceptive responses of female rats. Endocrinology. 1990;127:667–73. doi: 10.1210/endo-127-2-667. [DOI] [PubMed] [Google Scholar]
- 161.Reddy H, Arendt-Nielsen L, Staahl C, Pedersen J, Funch-Jensen P, Gregersen H, et al. Gender differences in pain and biomechanical responses after acid sensitization of the human esophagus. Dig Dis Sci. 2005;50:2050–8. doi: 10.1007/s10620-005-3006-x. [DOI] [PubMed] [Google Scholar]
- 162.Ren K, Dubner R. Central nervous system plasticity and persistent pain. J Orofac Pain. 1999;13:155–63. [PubMed] [Google Scholar]
- 163.Riley JL, Robinson ME, Kvaal SA, Gremillion HA. Effects of physical and sexual abuse in facial pain: direct or mediated? Cranio. 1998;16:1–8. doi: 10.1080/08869634.1998.11746066. [DOI] [PubMed] [Google Scholar]
- 164.Riley JL, Robinson ME, Wise EA, Myers CD, Fillingim RB. Sex differences in the perception of noxious experimental stimuli: a meta-analysis. Pain. 1998;74:181–7. doi: 10.1016/s0304-3959(97)00199-1. [DOI] [PubMed] [Google Scholar]
- 165.Riley JL, Robinson E, Wise EA, Price D. A meta-analytic review of pain perception across the menstrual cycle. Pain. 1999;81:225–35. doi: 10.1016/S0304-3959(98)00258-9. [DOI] [PubMed] [Google Scholar]
- 166.Robinson ME, Wise EA, Riley JL, Atchison JW. Sex differences in clinical pain: a multi-sample study. J Clin Psychol Med Settings. 1998;5:413–24. [Google Scholar]
- 167.Robinson M, Wise E, Gagnon C, Fillingim R, Price D. Influences of gender role and anxiety on sex differences in temporal summation of pain. J Pain. 2004;5:77–82. doi: 10.1016/j.jpain.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 168.Robinson ME, Gagnon CM, Riley JL, Price DD. Altering gender role expectations: effects on pain tolerance, pain threshold, and pain ratings. J Pain. 2003;4:284–8. doi: 10.1016/s1526-5900(03)00559-5. [DOI] [PubMed] [Google Scholar]
- 169.Robinson ME, Riley JL, Myers CD, Papas RK, Wise EA, Waxenberg LB, et al. Gender role expectations of pain: relationship to sex differences in pain. J Pain. 2001;2:251–7. doi: 10.1054/jpai.2001.24551. [DOI] [PubMed] [Google Scholar]
- 170.Rollman GB, bdel-Shaheed J, Gillespie JM, Jones KS. Does past pain influence current pain: biological and psychosocial models of sex differences. Eur J Pain. 2004;8:427–33. doi: 10.1016/j.ejpain.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 171.Ryan SM, Maier SF. The estrous cycle and estrogen modulate stress-induced analgesia. Behav Neurosci. 1988;102:371–80. doi: 10.1037//0735-7044.102.3.371. [DOI] [PubMed] [Google Scholar]
- 172.Sanford SD, Kersh BC, Thorn BE, Rich MA, Ward LC. Psychosocial mediators of sex differences in pain responsivity. J Pain. 2002;3:58–64. doi: 10.1054/jpai.2002.xb30066. [DOI] [PubMed] [Google Scholar]
- 173.Sanoja R, Cervero F. Estrogen-dependent abdominal hyperalgesia induced by ovariectomy in adult mice: a model of functional abdominal pain. Pain. 2005;118:243–53. doi: 10.1016/j.pain.2005.08.021. [DOI] [PubMed] [Google Scholar]
- 174.Sarlani E, Garrett PH, Grace EG, Greenspan JD. Temporal summation of pain characterizes women but not men with TMD. J Orofac Pain. 2007 in press. [PMC free article] [PubMed] [Google Scholar]
- 175.Sarlani E, Grace EG, Reynolds MA, Greenspan JD. Evidence for up-regulated central nociceptive processing in patients with masticatory myofascial pain. J Orofac Pain. 2004;18:41–55. [PubMed] [Google Scholar]
- 176.Sarlani E, Greenspan JD. Gender differences in temporal summation of mechanically evoked pain. Pain. 2002;97:163–9. doi: 10.1016/s0304-3959(02)00015-5. [DOI] [PubMed] [Google Scholar]
- 177.Sarlani E, Greenspan JD. Why look in the brain for answers to temporomandibular disorder pain? Cells Tissues Organs. 2005;180:69–75. doi: 10.1159/000086200. [DOI] [PubMed] [Google Scholar]
- 178.Sarlani E, Grace EG, Reynolds MA, Greenspan JD. Sex differences in temporal summation of pain and after sensations following repetitive noxious mechanical stimulation. Pain. 2004;109:115–23. doi: 10.1016/j.pain.2004.01.019. [DOI] [PubMed] [Google Scholar]
- 179.Sarton E, Olofsen E, Romberg R, Den Hartigh J, Kest B, Nieuwenhuijs D, et al. Sex differences in morphine analgesia–an experimental study in healthy volunteers. Anesthesiology. 2000;93:1245–54. doi: 10.1097/00000542-200011000-00018. [DOI] [PubMed] [Google Scholar]
- 180.Scher AI, Stewart WF, Lipton RB. Migraine and headache: a meta-analytic approach. In: Crombie IK, Croft PR, Linton SJ, LeResche L, Von Korff M, editors. Epidemiology of pain. Seattle: IASP Press; 1999. pp. 159–70. [Google Scholar]
- 181.Scher AI, Stewart WF, Liberman J, Lipton RB. Prevalence of frequent headache in a population sample. Headache. 1998;38:497–506. doi: 10.1046/j.1526-4610.1998.3807497.x. [DOI] [PubMed] [Google Scholar]
- 182.Schmidt-Hansen PT, Svensson P, Bendtsen L, Graven-Nielsen T, Bach FW. Increased muscle pain sensitivity in patients with tension-type headache. Pain. 2007;129:113–21. doi: 10.1016/j.pain.2006.09.037. [DOI] [PubMed] [Google Scholar]
- 183.Sherman JJ, LeResche L. Does experimental pain response vary across the menstrual cycle? A methodological review. Am J Physiol Regul Integr Comp Physiol. 2006;291:R245–56. doi: 10.1152/ajpregu.00920.2005. [DOI] [PubMed] [Google Scholar]
- 184.Sinchak K, Mills RH, Tao L, LaPolt P, Lu JK, Micevych P. Estrogen induces de novo progesterone synthesis in astrocytes. Dev Neurosci. 2003;25:343–8. doi: 10.1159/000073511. [DOI] [PubMed] [Google Scholar]
- 185.Sloan DM, Kornstein SG. Gender differences in depression and response to antidepressant treatment. Psychiatr Clin North Am. 2003;26:581–94. doi: 10.1016/s0193-953x(03)00044-3. [DOI] [PubMed] [Google Scholar]
- 186.Sloots CE, Felt-Bersma RJ, Cuesta MA, Meuwissen SG. Rectal visceral sensitivity in healthy volunteers: influences of gender, age and methods. Neurogastroenterol Motil. 2000;12:361–8. doi: 10.1046/j.1365-2982.2000.00210.x. [DOI] [PubMed] [Google Scholar]
- 187.Smith YR, Stohler CS, Nichols TE, Bueller JA, Koeppe RA, Zubieta JK. Pronociceptive and antinociceptive effects of estradiol through endogenous opioid neurotransmission in women. J Neurosci. 2006;26:5777–85. doi: 10.1523/JNEUROSCI.5223-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Staud R, Cannon RC, Mauderli AP, Robinson ME, Price DD, Vierck CJ., Jr Temporal summation of pain from mechanical stimulation of muscle tissue in normal controls and subjects with fibromyalgia syndrome. Pain. 2003;102:87–95. doi: 10.1016/s0304-3959(02)00344-5. [DOI] [PubMed] [Google Scholar]
- 189.Staud R, Vierck CJ, Cannon RL, Mauderli AP, Price DD. Abnormal sensitization and temporal summation of second pain (wind-up) in patients with fibromyalgia syndrome. Pain. 2001;91:165–75. doi: 10.1016/s0304-3959(00)00432-2. [DOI] [PubMed] [Google Scholar]
- 190.Staud R, Price DD, Robinson ME, Mauderli AP, Vierck CJ. Maintenance of windup of second pain requires less frequent stimulation in fibromyalgia patients compared to normal controls. Pain. 2004;110:689–96. doi: 10.1016/j.pain.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 191.Staud R, Robinson ME, Vierck CJ, Price DD. Diffuse noxious inhibitory controls (DNIC) attenuate temporal summation of second pain in normal males but not in normal females or fibromyalgia patients. Pain. 2003;101:167–74. doi: 10.1016/s0304-3959(02)00325-1. [DOI] [PubMed] [Google Scholar]
- 192.Sternberg WF, Smith L, Scorr L. Nociception and antinociception during the first week of life in mice: sex differences and test dependence. J Pain. 2004;5:420–6. doi: 10.1016/j.jpain.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 193.Stoffel EC, Ulibarri CM, Craft RM. Gonadal steroid hormone modulation of nociception, morphine antinociception and reproductive indices in male and female rats. Pain. 2003;103:285–302. doi: 10.1016/s0304-3959(02)00457-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Suzuki R, Dickenson A. Spinal and supraspinal contributions to central sensitization in peripheral neuropathy. Neurosignals. 2005;14:175–81. doi: 10.1159/000087656. [DOI] [PubMed] [Google Scholar]
- 195.Tall JM, Stuesse SL, Cruce WLR, Crisp T. Gender and the behavioral manifestations of neuropathic pain. Pharmacol Biochem Behav. 2001;68:99–104. doi: 10.1016/s0091-3057(00)00461-5. [DOI] [PubMed] [Google Scholar]
- 196.Tanner J. Growth and adolescence. Oxford: Blackwell; 1962. [Google Scholar]
- 197.Thase ME, Entsuah R, Cantillon M, Kornstein SG. Relative antidepressant efficacy of venlafaxine and SSRIs: sex–age interactions. J Womens Health. 2005;14:609–16. doi: 10.1089/jwh.2005.14.609. [DOI] [PubMed] [Google Scholar]
- 198.Treloar AE, Boynton RE, Behn BG, Brown BW. Variation of the human menstrual cycle through reproductive life. Int J Fertil. 1967;12:77–126. [PubMed] [Google Scholar]
- 199.Unruh AM. Gender variations in clinical pain experience. Pain. 1996;65:123–67. doi: 10.1016/0304-3959(95)00214-6. [DOI] [PubMed] [Google Scholar]
- 200.Unruh AM, Ritchie J, Merskey H. Does gender affect appraisal of pain and pain coping strategies? Clin J Pain. 1999;15:31–40. doi: 10.1097/00002508-199903000-00006. [DOI] [PubMed] [Google Scholar]
- 201.US Food and Drug Administration. FDA approves BiDil heart failure drug for black patients. FDA News. 2005:P05–P32. [Google Scholar]
- 202.Vierck CJ, Cannon RL, Fry G, Maixner W, Whitsel BL. Characteristics of temporal summation of second pain sensations elicited by brief contact of glabrous skin by a preheated thermode. J Neurophysiol. 1997;78:992–1002. doi: 10.1152/jn.1997.78.2.992. [DOI] [PubMed] [Google Scholar]
- 203.vom Saal FS, Finch CE, Nelson JF. Natural history and mechanisms of reproductive aging in humans, laboratory rodents, and other selected vertebrates. In: Knobil E, Neill JD, editors. The physiology of reproduction. New York: Raven Press; 1994. pp. 1213–314. [Google Scholar]
- 204.Von Korff M, Dworkin SF, Le Resche L, Kruger A. An epidemiologic comparison of pain complaints. Pain. 1988;32:173–83. doi: 10.1016/0304-3959(88)90066-8. [DOI] [PubMed] [Google Scholar]
- 205.Von Korff M, Le Resche L, Dworkin SF. First onset of common pain symptoms: a prospective study of depression as a risk factor. Pain. 1993;55:251–8. doi: 10.1016/0304-3959(93)90154-H. [DOI] [PubMed] [Google Scholar]
- 206.Von Korff M, Ormel J, Keefe FJ, Dworkin SF. Grading the severity of chronic pain. Pain. 1992;50:133–49. doi: 10.1016/0304-3959(92)90154-4. [DOI] [PubMed] [Google Scholar]
- 207.Von Korff M, Wagner EH, Dworkin SF, Saunders KW. Chronic pain and use of ambulatory health care. Psychosom Med. 1991;53:61–79. doi: 10.1097/00006842-199101000-00006. [DOI] [PubMed] [Google Scholar]
- 208.Wade GN, Blaustein JD, Gray JM, Meredith JM. ICI-182,780 – a pure antiestrogen that affects behavior and energy balance in rats without acting in the brain. Am J Physiol. 1993;265:R1398. doi: 10.1152/ajpregu.1993.265.6.R1392. [DOI] [PubMed] [Google Scholar]
- 209.Walker QD, Nelson CJ, Smith D, Kuhn CM. Vaginal lavage attenuates cocaine-stimulated activity and establishes place preference in rats. Pharmacol Biochem Behav. 2002;73:743–52. doi: 10.1016/s0091-3057(02)00883-3. [DOI] [PubMed] [Google Scholar]
- 210.Wang X, Traub RJ, Murphy AZ. Persistent pain model reveals sex difference in morphine potency. Am J Physiol Regul Integr Comp Physiol. 2006;291:R300–6. doi: 10.1152/ajpregu.00022.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Weissman MM. Recent advances in depression across the generations. Epidemiol Psychiatr Soc. 2006;15:16–9. [PubMed] [Google Scholar]
- 212.Wieseler-Frank J, Maier SF, Watkins LR. Immune-to-brain communication dynamically modulates pain: physiological and pathological consequences. Brain Behav Immun. 2005;19:104–11. doi: 10.1016/j.bbi.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 213.Wiesenfeld-Hallin Z. Sex differences in pain perception. Gend Med. 2005;2:137–45. doi: 10.1016/s1550-8579(05)80042-7. [DOI] [PubMed] [Google Scholar]
- 214.Wilson MA, Biscardi R. Sex differences in GABA/benzodiazepine receptor changes and corticosterone release after acute stress in rats. Exp Brain Res. 1994;101:297–306. doi: 10.1007/BF00228750. [DOI] [PubMed] [Google Scholar]
- 215.Wise EA, Price DD, Myers CD, Heft MW, Robinson ME. Gender role expectations of pain: relationship to experimental pain perception. Pain. 2002;96:335–42. doi: 10.1016/s0304-3959(01)00473-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Wizemann TM, Pardue M-L. Exploring the biological contributions to human health: does sex matter? Inst Med. 2001 [PubMed] [Google Scholar]
- 217.World Health Organization. WHO Technical Report Series. 670. 1981. Report of a WHO scientific group: research on menopause; pp. 8–12. [Google Scholar]
- 218.Yang SN, Lu F, Wu JN, Liu DD, Hsieh WY. Activation of gonadotropin-releasing hormone receptors induces a long-term enhancement of excitatory postsynaptic currents mediated by ionotropic glutamate receptors in the rat hippocampus. Neurosci Lett. 1999;260:33–6. doi: 10.1016/s0304-3940(98)00939-2. [DOI] [PubMed] [Google Scholar]
- 219.Yezierski RP. The next generation of pain scientists: the need for integrative and translational training in pain research. APS Bull. 2007;17:3–5. [Google Scholar]
- 220.Zanisi M, Martini L. Differential effects of castration on LH and FSH secretion in male and female rats. Acta Endocrinol. 1975;78:683–8. doi: 10.1530/acta.0.0780683. [DOI] [PubMed] [Google Scholar]
- 221.Zubieta JK, Smith YR, Bueller JA, Xu Y, Kilbourn MR, Jewett DM, et al. μ-Opioid receptor-mediated antinociceptive responses differ in men and women. J Neurosci. 2002;22:5100–7. doi: 10.1523/JNEUROSCI.22-12-05100.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]