Abstract
Background
Ankle arthrodesis and replacement are two common surgical treatment options for end-stage ankle osteoarthritis. However, the relative value of these alternative procedures is not well defined. This study compared the clinical and radiographic outcomes as well as the early perioperative complications of the two procedures.
Methods
Between January 2, 1998 and May 31, 2002, 138 patients were treated with ankle fusion or replacements. Seventy one patients had isolated posttraumatic or primary ankle arthritis. However, patients with inflammatory arthritis, neuropathic arthritis, concomitant hind foot fusion, revision procedures and two component system ankle replacement were excluded. Among them, one group of 42 patients had a total ankle replacement (TAR), whereas the other group of 29 patients underwent ankle fusion. A complete follow-up could be performed on 89% (37/42) and 73% (23/29) of the TAR and ankle fusion group, respectively. The mean follow-up period was 4.2 years (range, 2.2 to 5.9 years).
Results
The outcomes of both groups were compared using a student's t-test. Only the short form heath survery mental component summary score and Ankle Osteoarthritis Scale pain scale showed significantly better outcomes in the TAR group (p < 0.05). In the radiographic evaluation, there was no significant difference in preoperative and postoperative osteoarthritis between the TAR and fusion groups.
Conclusions
The clinical results of TAR are similar to those of fusion at an average follow-up of 4 years. However, the arthroplasty group showed better pain relief and more postoperative complications that required surgery.
Keywords: Ankle, Replacement, Arthroplasty, Arthrodesis
Although tremendous strides have been made in total joint arthroplasty for the knee and hip, this modality is still evolving in the ankle.1-3) Some of the problems that increase the difficulty in total ankle replacement (TAR) include a high prevalence of post-traumatic arthritis rather than chronic arthritis that causes poor anatomic access, a higher incidence of neuroarthropathy and vascular deficiency, particularly in diabetes-associated pathology and poor soft-tissue coverage. This is associated with an increased incidence of peri-operative complications, such as wound dehiscence and infection.
Mild to moderate ankle arthritis can often be managed with an ankle foot orthoses and a rocker-bottom shoe, provided that no significant varus/valgus deformity is present.2,4) Ankle arthrodesis and replacement are two common surgical treatment options for end-stage ankle osteoarthritis. The relative value of these alternative procedures is not well defined. The major drawbacks of arthrodesis are a 10-60% rate of arthrosis in the adjacent joints in the long-term,5) a nonunion rate of 10 to 20%, and a postoperative infection rate of 3-25%.6)
There are multiple TAR designs. However, most previous designs performed well only in the short-term and generally performed poorly in the long-term7) due mostly to rapid bone loss or implant wear. The current designs maintain better pressure distribution and wear characteristics.8,9) The Scandinavian Total Ankle Replacement (STAR; W. Link GmbH, Hamburg, Germany) is an uncemented, unconstrained, congruent, cylindrical replacement. Its advantages over previous designs include its bone-sparing design, which can allow an easier reconstruction after failure, as well as its mobile bearing that allows easy polyethylene component exchange.
There is limited data comparing the outcomes or perioperative complications and reoperations in ankle arthroplasty designs.8,10,11) Pyevich et al.12) reported a 93% satisfaction rate at 3 to 10 year follow-up of Agility arthroplasty. Knecht et al.13) reported > 90% survival at 5 years in the same cohort, which are encouraging results for patients with modern ankle arthroplasties.
This study compared the clinical and radiographic outcomes and the early perioperative complications between a series of ankle arthroplasty and arthrodesis patients. A group of STAR patients was matched with a similar group of arthrodesis patients from the same period. It was hypothesized that total ankle arthroplasty would have similar early outcomes to ankle fusion in terms of its ability to relieve the disabling symptoms of ankle osteoarthritis.
METHODS
This is a 2-6 year follow-up retrospective study of a cohort of ankle arthroplasty patients with noninflammatory arthritis. Patients with isolated ankle osteoarthritis were included but those patients with any confounding pathology were excluded. Only one type of prosthesis, the STAR device, was examined. However, many different techniques of ankle fusion were included. The ankle joint was fixed only with 6.5 or 7.3 mm cannulated screws in 14 cases, a plate and screws in 10 cases and external fixators in 3 cases.
Between January 2, 1998 and May 31, 2002, 138 patients were treated with ankle fusion or replacement at our institution. Among them, 71 had isolated posttraumatic or primary ankle arthritis. The remaining 67 were excluded. Of these patients, 12 and 55 patients had a different ankle prosthesis (Agility) and ankle arthritis with confounding pathology, respectively. The reasons for their exclusion was inflammatory arthritis (n = 20), neuropathic arthritis (n = 4), concomitant hindfoot fusions (n = 25) and revision procedures (n = 6).
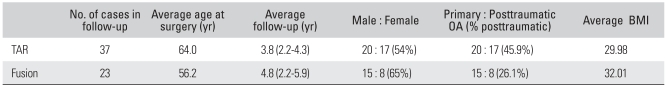
Among the 71 eligible subjects, one group of 42 patients underwent STAR total ankle arthroplasty while the other group comprised of 29 patients who underwent ankle fusion. A complete follow-up could be per formed on 88% (37/42) of the TAR group and 79% (23/29) of the ankle fusion group. Table 1 lists the subject characteristics. The fusion group has a younger age at surgery (p = 0.034), higher proportion of males and a higher percentage of those with posttraumatic osteoarthritis (OA). There were no significant differences in the mean BMI (p = 0.258) or follow up length (p = 0.874) between the two groups.
Table 1.
Subject Characteristics of the Total Ankle Replacement and Fusion Groups
TAR: Total ankle replacement, OA: Osteoarthritis, BMI: Body mass index.
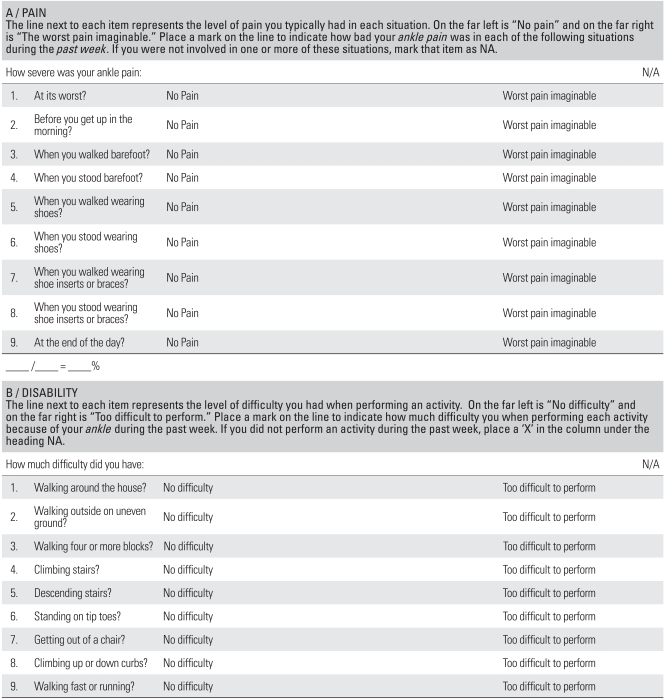
Detailed physical examination data, including information on perioperative and postoperative complications, was collected. The foot function was evaluated using the Ankle Osteoarthritis Scale (AOS) (Table 2). This is a reliable, validated, visual-analog based, disease-specific self-administered instrument, which is based on the foot function index (FFI). It is designed specifically to measure the disability and pain from ankle osteoarthritis.14) It has two subscales, pain and disability. The index study revealed an effect of gender, body mass index and arthritis on the other joints. Each item of the AOS was graded, and the subscales for pain and disability were generated independently. The foot function index is a validated reliable instrument that was developed in rheumatoid arthritis patients for measuring the level of foot pain, disability and activity restriction.15,16) In contrast, the ankle osteoarthritis scale was developed based on the FFI, but was validated in patients with osteoarthritis.
Table 2.
Ankle Osteoarthritis Scale
The patient's general health was evaluated using the short form health survey (SF-36), which is a generic measure of mental and physical health and a well established quality of life out come measure. The SF-36 evaluates the impact of a disease on the patient, and is well supported by evidence of reliability and validity, and responsiveness in musculoskeletal disorders.17) Separate mental component summary (MCS) and physical component summary (PCS) scores were generated.
For the pre-operative films, an ankle anteroposterior (AP), mortise and lateral view were taken. On the day of the study, foot lateral views were taken in the maximum dorsi- and plantar-flexion, foot AP, hindfoot alignment, and Brodens views. The pre and post-operative arthritic changes were evaluated for 4 joints: subtalar, talonavicular, calcaneocuboid, and midfoot (Lisfranc + naviculocuneiform joint). The Kellgren/Lawrence (K/L) arthritis scale was used, which is a 5-point grading of the radiographic signs of arthritis.18) All X-rays were read and scored by one of the authors, limiting the interobserver variance in the results. The same procedure was carried out 2 weeks later to reduce the intraobserver variance. A second opinion was given by another physician in the rare case of different scores.
Statistical Analysis
All analyses were performed using SAS (SAS Ins., Cary, NC, USA). The AOS and SF-36 scores were analyzed using a student's t-test. The AOS and SF-36 scores were also examined using a 2-tailed t-test at the 0.05 significance level, which had 0.80 power to detect a difference in a mean score of at least 0.76 SD units between the two groups. Using a standard deviation of 10 and 26 for SF-36 and AOS scores, respectively, a difference in the mean SF-36 and AOS score between the two groups of at least 7.6 and 20, respectively, could be detected with 0.80 power.
The X-ray data was arranged in a table showing the frequency of each K/L grade for each joint. There was a separate table for the pre and postoperative score. A Wilcoxon signed-rank test was used to compare the K/L grade ranked data. Power analysis revealed that a difference in the median K/L grade of at least 1 between the groups could be detected with 0.90 power at the 0.05 significance level.
RESULTS
Clinical Outcomes
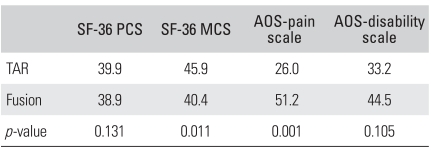
Table 3 shows the mean AOS pain and disability scores, as well as the mean SF-36 PCS and MCS scores. A perfect AOS score is zero, showing no disability and no pain. The population mean SF-36 score was 50 with higher scores representing better function. The outcomes between the TAR and fusion groups were compared using a student's t-test. For each of the four outcomes, a better outcome was observed in the TAR group. However, using a critical p-value of 0.05, significant differences were noted only in the SF-36 MCS and AOS pain scale.
Table 3.
The Average AOS Pain and Disability Scores and SF-36 PCS and MCS Function Score in the TAR and Fusion Groups
AOS: Ankle osteoarthritis scale, SF-36: Short form health survey, PCS: Physical component summary score, MCS: Mental component summary score, TAR: Total ankle replacement.
Radiographic Outcomes
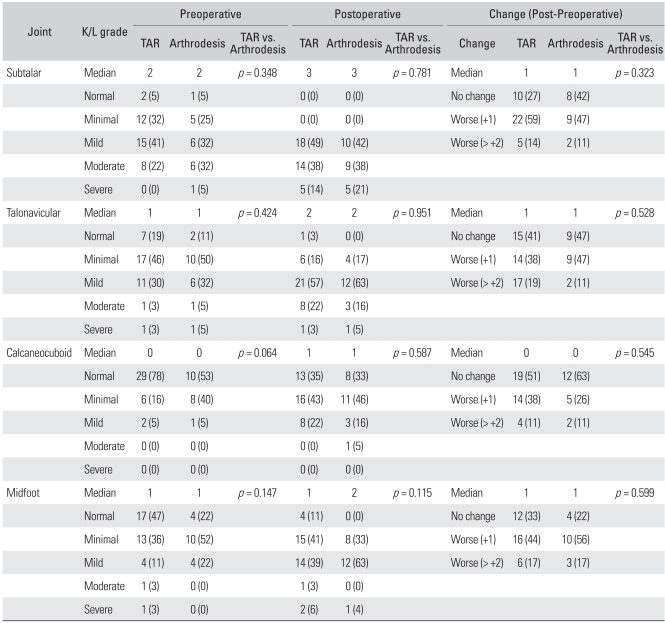
The K/L grade was recorded at the subtalar, talonavicular, calcaneocuboid and midfoot for both the pre and postoperative X-rays. The radiographic data were evaluated by asking three questions: Is there a significant difference in the pre-operative K/L grade, post operative K/L grade, or the change in the K/L grades between the TAR and fusion groups?
Table 4 summarizes the radiographic data. For each joint, the frequency distribution of each K/L grade (0 = Normal, 1 = Minimal, 2 = Mild, 3 = Moderate, 4 = Severe) on the preoperative and postoperative X-rays is shown.
Table 4.
Distribution of the Preoperative and Postoperative K/L Grade in the Subtalar, Talonavicular, Calcaneocuboid, Midfoot Joints in the TAR and Arthrodesis Groups
Values are presented as number (%).
K/L: Kellgren/Lawrence, TAR: Total ankle replacement.
Firstly, the hypothesis that there was a difference in the preoperative K/L grade between the fusion and TAR groups was tested. For each joint, the frequency distribution of each K/L grade was determined (Table 4). The distribution between the TAR and fusion groups was then compared. A Wilcoxon rank test was used, and all p-values are shown in Table 4. There was no significant difference in the preoperative OA between the TAR and fusion groups at any joint evaluated.
Secondly, the hypothesis that there was a difference in the postoperative K/L grade between the two groups was tested. Another frequency distribution was developed for each joint. The Wilcoxon rank-sum test was used. All p-values are shown in Table 4. There was no significant difference in postoperative OA between the TAR and fusion groups.
Thirdly, the hypothesis that there was a difference in the change in K/L grade between fusion and TAR groups was tested. Using a similar method, there was no difference in the change in OA between the two groups.
Perioperative Problems
In the 37 TAR patients, fifteen additional procedures were performed after the index operation during the follow-up period. These included the following: 7 cases of debridement plus bony resection for lateral or posterior impingement; 2 cases of bone debridement for exostosis; 3 cases of osteolysis requiring poly exchange and bone grafting including one revision of tibial component with calcaneal realignment; 2 cases of revision closure for wound dehiscence; and one case of medial malleolar osteotomy revision fixation for nonunion. There were 5 intraoperative medial or posterior malleolar fractures; all were fixed internally at the index operation. Two patients developed deep venous thromboses requiring anticoagulation and one superficial wound dehiscence that healed uneventfully.
In the 23 patients with ankle fusion, there were 5 postoperative events that required surgery: 2 cases of nonunion that required revision arthrodesis; 2 cases of hardware pain that required hardware removal; and one case of naviculocuneiform joint arthritis progression that required fusion. There was one case each of leg length discrepancy, delayed union, tibia stress fracture, hardware pain and wound dehiscence, and impingement. All were treated successfully without surgery.
DISCUSSION
This study demonstrated a tendency toward better clinical outcomes among the ankle arthroplasty group at the 2-6 year follow up. There was better ultimate pain relief from ankle arthroplasty than fusion. This finding is very important because the primary indication for both procedures is pain relief. The cause of continued pain for both groups is unclear because the rates of new-onset, radiographically apparent arthritis was similar in the two groups. The AOS disability scale, though not significant, also suggests a better outcome among the TAR group.
The SF-36 MCS scores for the arthroplasty patients are higher, suggesting a possible difference in life outlook with the fusion patients having marginally poorer mental health despite their younger age. This might be related to the finding that a higher percentage of the fusion group had posttraumatic rather than degenerative arthritis. The long-term effect of ankle trauma on the patient's function and outlook was discussed previously by Marsh et al.19) and Dirschl et al.20) The PCS scores also showed a trend toward a better outcome among TAR subjects but the significance was not definite.
There was a higher incidence of surgical procedures performed postoperatively in the arthroplasty group. The significance of these findings is unclear. All the procedures were small, and none involved any revision of the hardware or a conversion to fusion. However, the risk from these procedures is an important factor when comparing arthroplasty with arthrodesis.
This is a retrospective study and must be interpreted in terms of patient selection bias. It is impossible to control all the known sources of bias in such a study. One of the main concerns is that the indications for ankle fusion are different from TAR. Generally, fusion patients tend to be younger and more active with a diagnosis of posttraumatic osteoarthritis. Since obesity or severe malalignment is a relative contraindication to arthroplasty, fusion patients may be heavier and more malaligned. However, there was no significant difference in BMI in this study. Therefore, the body habitus is not believed to have affected the results. Basically, a direct comparison of both group demographics and outcomes may not be appropriate. Despite these limitations, useful comparative data was obtained on the short term results of fusion and TAR.
Another major assumption is that the AOS is a real reflection of the patient's condition after either fusion or TAR. This is a reasonable assumption because Domsic and Saltzman14) reported it to be "a reliable and valid instrument that specifically measures the patient's symptoms and disability related to ankle arthritis." They validated the AOS scale in patients with ankle OA.
These results are encouraging and consistent with other data published regarding this device. Hintermann21) followed 48 patients who had undergone arthroplasty for 1 to 4 years. They noted 91% satisfaction using the American Orthopaedic Foot and Ankle Society-Hindfoot-Score, no migration and a good range of motion. Seven cases required revision surgery: fibula resection for lateral impingement (3 cases), posteromedial soft tissue revision for a painful restriction of dorsiflexion (2 cases), percutaneous lengthening of the Achilles tendon (1 case), and osteotomy and distraction for angular correction after a stress fracture of the distal tibia (1 case).
Implant survival was not evaluated in this early postoperative period but there are studies that showed good wear characteristics for this device. Wood et al.9,22) reported that at 5 years, the STAR prosthesis had superior clinical and radiographic outcomes compared to a cemented comparable implant. Andersen et al.23) reviewed 51 STAR implants for 36 to 97 months, and reported a 70% 5-year survival rate. This study focused on the early clinical and radiographic outcomes, and showed a higher incidence of postoperative events that required surgery than arthrodesis. However, there was no conversion to fusion during this time period.
The clinical results of ankle arthroplasty and arthrodesis after an average 4 year follow-up were almost equivalent. The arthroplasty group had more postoperative complications that required surgery than the fusion group. On the other hand, the arthroplasty group showed better pain relief and preservation of motion.
References
- 1.Culpan P, Le Strat V, Piriou P, Judet T. Arthrodesis after failed total ankle replacement. J Bone Joint Surg Br. 2007;89(9):1178–1183. doi: 10.1302/0301-620X.89B9.19108. [DOI] [PubMed] [Google Scholar]
- 2.Coughlin MJ, Mann RA. Surgery of the foot and ankle. 7th ed. St. Louis: Mosby; 1999. [Google Scholar]
- 3.Saltzman CL, Mclff TE, Buckwalter JA, Brown TD. Total ankle replacement revisited. J Orthop Sports Phys Ther. 2000;30(2):56–67. doi: 10.2519/jospt.2000.30.2.56. [DOI] [PubMed] [Google Scholar]
- 4.Martin RL, Stewart GW, Conti SF. Posttraumatic ankle arthritis: an update on conservative and surgical management. J Orthop Sports Phys Ther. 2007;37(5):253–259. doi: 10.2519/jospt.2007.2404. [DOI] [PubMed] [Google Scholar]
- 5.Coester LM, Saltzman CL, Leupold J, Pontarelli W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg Am. 2001;83(2):219–228. doi: 10.2106/00004623-200102000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Bauer G, Kinzl L. Arthrodesis of the ankle joint. Orthopade. 1996;25(2):158–165. [PubMed] [Google Scholar]
- 7.Kofoed H, Lundberg-Jensen A. Ankle arthroplasty in patients younger and older than 50 years: a prospective series with long-term follow-up. Foot Ankle Int. 1999;20(8):501–506. doi: 10.1177/107110079902000807. [DOI] [PubMed] [Google Scholar]
- 8.Haddad SL, Coetzee JC, Estok R, Fahrbach K, Banel D, Nalysnyk L. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis: a systematic review of the literature. J Bone Joint Surg Am. 2007;89(9):1899–1905. doi: 10.2106/JBJS.F.01149. [DOI] [PubMed] [Google Scholar]
- 9.Wood PL, Prem H, Sutton C. Total ankle replacement: medium-term results in 200 Scandinavian total ankle replacements. J Bone Joint Surg Br. 2008;90(5):605–609. doi: 10.1302/0301-620X.90B5.19677. [DOI] [PubMed] [Google Scholar]
- 10.Piriou P, Culpan P, Mullins M, Cardon JN, Pozzi D, Judet T. Ankle replacement versus arthrodesis: a comparative gait analysis study. Foot Ankle Int. 2008;29(1):3–9. doi: 10.3113/FAI.2008.0003. [DOI] [PubMed] [Google Scholar]
- 11.SooHoo NF, Zingmond DS, Ko CY. Comparison of reoperation rates following ankle arthrodesis and total ankle arthroplasty. J Bone Joint Surg Am. 2007;89(10):2143–2149. doi: 10.2106/JBJS.F.01611. [DOI] [PubMed] [Google Scholar]
- 12.Pyevich MT, Saltzman CL, Callaghan JJ, Alvine FG. Total ankle arthroplasty: a unique design. Two to twelve-year follow-up. J Bone Joint Surg Am. 1998;80(10):1410–1420. [PubMed] [Google Scholar]
- 13.Knecht SI, Estin M, Callaghan JJ, et al. The Agility total ankle arthroplasty: seven to sixteen-year follow-up. J Bone Joint Surg Am. 2004;86(6):1161–1171. [PubMed] [Google Scholar]
- 14.Domsic RT, Saltzman CL. Ankle osteoarthritis scale. Foot Ankle Int. 1998;19(7):466–471. doi: 10.1177/107110079801900708. [DOI] [PubMed] [Google Scholar]
- 15.Budiman-Mak E, Conrad KJ, Roach KE. The Foot Function index: a measure of foot pain and disability. J Clin Epidemiol. 1991;44(6):561–570. doi: 10.1016/0895-4356(91)90220-4. [DOI] [PubMed] [Google Scholar]
- 16.Saag KG, Saltzman CL, Brown CK, Budiman-Mak E. The Foot Function Index for measuring rheumatoid arthritis pain: evaluating side-to-side reliability. Foot Ankle Int. 1996;17(8):506–510. doi: 10.1177/107110079601700814. [DOI] [PubMed] [Google Scholar]
- 17.Beaton DE, Schemitsch E. Measures of health-related quality of life and physical function. Clin Orthop Relat Res. 2003;(413):90–105. doi: 10.1097/01.blo.0000079772.06654.c8. [DOI] [PubMed] [Google Scholar]
- 18.Kellgren JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marsh JL, Weigel DP, Dirschl DR. Tibial plafond fractures: How do these ankles function over time? J Bone Joint Surg Am. 2003;85(2):287–295. [PubMed] [Google Scholar]
- 20.Dirschl DR, Marsh JL, Buckwalter JA, et al. Articular fractures. J Am Acad Orthop Surg. 2004;12(6):416–423. doi: 10.5435/00124635-200411000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Hintermann B. Short- and mid-term results with the STAR total ankle prosthesis. Orthopade. 1999;28(9):792–803. doi: 10.1007/PL00003669. [DOI] [PubMed] [Google Scholar]
- 22.Wood PLR, Clough TM, Jari S. Clinical comparison of two total ankle replacements. Foot Ankle Int. 2000;21(7):546–550. doi: 10.1177/107110070002100703. [DOI] [PubMed] [Google Scholar]
- 23.Anderson T, Montgomery F, Carlsson A. Uncemented STAR total ankle prostheses: three to eight-year follow-up of fifty-one consecutive ankles. J Bone Joint Surg Am. 2003;85(7):1321–1329. [PubMed] [Google Scholar]