Abstract
Background
To evaluate the clinical results and operation technique of arthroscopic repair of combined Bankart and superior labrum anterior to posterior (SLAP) lesions, all of which had an anterior-inferior Bankart lesion that continued superiorly to include separation of the biceps anchor in the patients presenting recurrent shoulder dislocations.
Methods
From May 2003 to January 2006, we reviewed 15 cases with combined Bankart and SLAP lesions among 62 patients with recurrent shoulder dislocations who underwent arthroscopic repair. The average age at surgery was 24.2 years (range, 16 to 38 years), with an average follow-up period of 15 months (range, 13 to 28 months). During the operation, we repaired the unstable SLAP lesion first with absorbable suture anchors and then also repaired Bankart lesion from the inferior to superior fashion. We analyzed the preoperative and postoperative results by visual analogue scale (VAS) for pain, the range of motion, American Shoulder and Elbow Surgeon (ASES) and Rowe shoulder scoring systems. We compared the results with the isolated Bankart lesion.
Results
VAS for pain was decreased from preoperative 4.9 to postoperative 1.9. Mean ASES and Rowe shoulder scores were improved from preoperative 56.4 and 33.7 to postoperative 91.8 and 94.1, respectively. There were no specific complication and no significant limitation of motion more than 10 degree at final follow-up. We found the range of motions after the arthroscopic repair in combined lesions were gained more slowly than in patients with isolated Bankart lesions.
Conclusions
In recurrent dislocation of the shoulder with combined Bankart and SLAP lesion, arthroscopic repair using absorbable suture anchors produced favorable clinical results. Although it has technical difficulty, the concomitant unstable SLAP lesion should be repaired in a manner that stabilizes the glenohumeral joint, as the Bankart lesion can be repaired if the unstable SLAP lesion is repaired first.
Keywords: Shoulder, Arthroscopy, Repair, Combined Bankart and SLAP lesion
Superior labrum anterior to posterior (SLAP) lesions are labral tears extending anteriorly from the posterior superior labrum, involving the long head of the biceps tendon originating from the glenoid labrum, and stopping before the anterior glenoid notch. Common symptoms of SLAP lesions include pain, locking, and catching sensations. These lesions are frequently observed in athletes who use their upper limbs in their sport, such as baseball players. Snyder et al.1) have categorized SLAP lesions into 4 types, Type II and type IV SLAP lesions cause instability at the origin of the biceps long head, requiring watertight suture closure. Although SLAP lesions can occur as isolated injuries, they can also be accompanied by Bankart lesions (tears of the anteroinferior labrum) in cases of recurrent dislocation, which are categorized by Maffet et al.2) as type V SLAP lesions. The purpose of this study was to evaluate the clinical outcomes of arthroscopic repair using absorbable suture anchors for type V SLAP lesions (combined Bankart and SLAP lesions) in patients with recurrent shoulder dislocations. In addition, the surgical outcomes were compared with those of arthroscopic repairs for isolated Bankart lesions.
METHODS
Materials
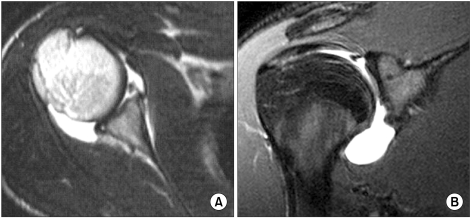
From May 2003 to January 2006, 62 patients underwent arthroscopic repair for recurrent shoulder dislocation at our institution and were followed for more than 12 months. There were 15 patients with arthroscopically confirmed combined Bankart and type II SLAP lesions; the patient cases were reviewed retrospectively. All of the subjects were males with a mean age of 24.2 years (range, 16 to 38 years) and the mean postoperative follow-up period was 15 months (range, 13 to 28 months). There were in 9 cases of the shoulder affected being on the dominant and 6 cases with the affected shoulder on the non-dominant side. All of the patients had greater than 10 experiences of shoulder dislocation. The mean interval from initial dislocation to the index operation was 34 months (range, 21 to 56 months). The clinical outcomes in terms of postoperative pain and range of motion recovery were compared to 15 of the 62 patients, who were selected as the control group. The patients in the control group had isolated Bankart lesions without type II SLAP lesions and were male. The affected shoulder was on the dominant side in 11 cases. The mean age was 24.6 years (range, 18 to 35 years) and the mean postoperative follow-up period was 22 months (range, 21 to 34 months). The preoperative physical tests included the anterior apprehension test, relocation test, O'Brien test, and biceps load test (Table 1). For the identification of osseous lesions, we took anteroposterior, axillary, Stryker notch, and West Point radiographs. There were no osseous Bankart lesions, while there were noted Hill-Sach lesions. In all cases, a Bankart lesion and a SLAP lesion was observed on the horizontal MRI and the coronal MRI, respectively (Fig. 1).
Table 1.
Demographic and Clinical Findings
Fig. 1.
MRI findings showing the Bankart lesion (A) and the superior labrum anterior to posterior lesion (B).
Operative Technique
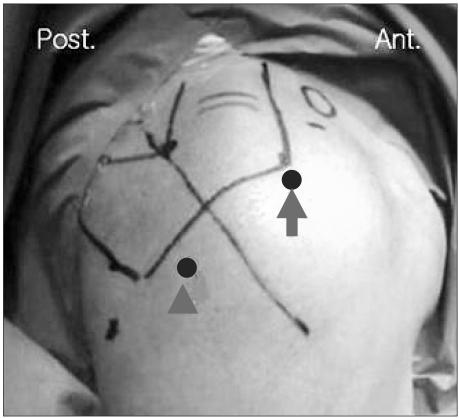
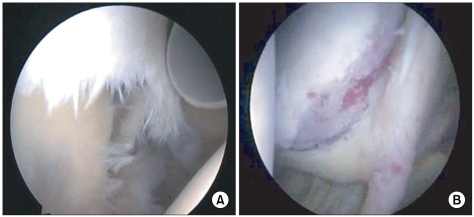
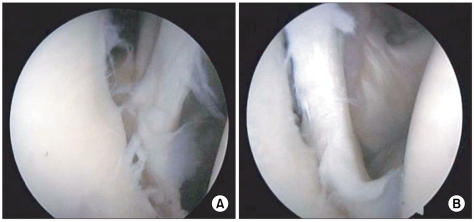
Surgery was performed with each patient placed in a beach-chair position at an angle of 70° to the floor under general anesthesia. A posterior portal was first established to identify intraarticular lesions. An anterior portal was created lateral to the coracoid process. Next, an anterosuperior portal was made at the anterolateral corner of the acromion for the repair of the anterior SLAP lesion and a port of Wilmington portal was created at a site 1 cm anterior and 1 cm lateral to the posterolateral corner of the acromion for the repair of the posterior SLAP lesion (Fig. 2). A 5.5 mm cannula (Linvatec, Largo, FL, USA) was inserted through the anterior portal and an instrument was passed through this cannula to observe the extent of a Bankart lesion and the presence of a SLAP lesion (Fig. 3). Before the repair of the SLAP lesion, we observed that anatomical reduction of the anteroinferiorly and medially displaced anteroinferior labrum could be obtained with tension when trial reduction of the superior labrum was performed with a probe (Fig. 4). With labral tissues of the SLAP lesion completely separated, the labrum was abraded with a burr until bleeding of the subchondral bone was evident. Then, the anteroinferior labral tissues were released from the articular surface and the labrum was abraded, until bleeding of the subchondral bone was noted. An anchor insertion area was marked with arthroscopic forceps on superior glenoid and SLAP lesion repair using absorbable anchors was started. A bone drill was inserted through the anterior portal and a hole was created at an angle of 45° from the edge of the glenoid with 1 to 2 mm of interval. The lowest anchor portal in the right shoulder was made below the 5 o'clock position and the suture ran superiorly. The suture was passed using a suture hook through the capsulolabral complex from a point 5 mm inferior to the lowest anchor. Finally, knot tying was performed with the inferior glenohumeral ligament pulled superiorly by arthroscopic forceps to make the anteroinferior labral complex displaced superiorly and then firm fixation was examined with probe (Fig. 5). In all cases, we used an average of 5.2 absorbable Panaloc® (Mitek, Norwood, MA, USA) anchors. Suture loop shuttle technique using a No. 2 Nylon suture was performed to prevent the suture strand from being twisted and the Samsung Medical Center knot was made (Fig. 6).
Fig. 2.
Arthroscopic portals were designed at the right shoulder. Arrow is the anterosuperior portal and arrow head is the port of Wilmington.
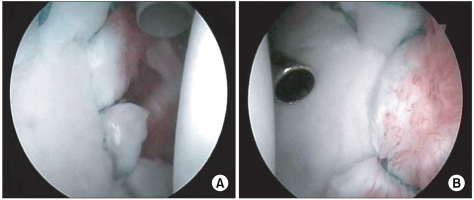
Fig. 3.
Arthroscopic image of the combined Bankart and superior labrum anterior to posterior lesion showing (A) inferiorly displaced superior labrum with significant fraying (right shoulder, from posterior viewing portal) and (B) medially displaced superior and anteroinferior labral complex (right shoulder, from anterior working portal).
Fig. 4.
The effect of the superior labrum anterior to posterior (SLAP) repair revealing (A) medially an inferiorly displaced anteroinferior labrum before the repair of the SLAP lesion (right shoulder, from posterior viewing portal) and (B) relatively anatomically reduced Bankart lesion after the repair of the SLAP lesion (right shoulder, from posterior viewing portal).
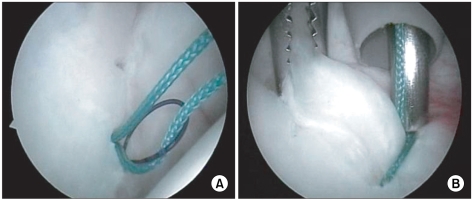
Fig. 5.
Final arthroscopic findings after the completion of the repair of combined Bankart and superior labrum anterior to posterior lesion in right shoulder viewing from (A) posterior viewing portal and (B) anterior working portal.
Fig. 6.
Suture relay and knot tying representing (A) intra-articular suture relay using 2-0 Nylon loop which shuttles capsular side of suture limbs and (B) sliding knot tying of the most inferior suture anchor around 5 o'clock while exerting upward tension of the anteroinferior labrum using tissue grasper (right shoulder, from posterior viewing portal).
Postoperative Treatment
Postoperatively, an Ultrasling shoulder immobilizer was used in all cases. At the 3rd postoperative week, the immobilizer was removed and passive exercise and active-assisted exercise (using the unaffected arm) were started. From the 6th postoperative week, full-range active exercise and strength training were started. From the 8th postoperative week, patients began strength training of their biceps. Beginning with the 6th postoperative month, all movements including sports activities were allowed when muscle strength and range of motion became almost normal.
Assessment
The visual analogue scale (VAS) score for pain, American Shoulder and Elbow Surgeons (ASES) scoring system,3) and Rowe shoulder scoring system4) were used to assess the outcomes. These assessment results, range of motion, and the time needed to recover the normal range of motion were used for comparisons with patients with an isolated Bankart lesion. SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) was used for data analysis. The paired samples t-test was used for comparisons of preoperative and postoperative conditions. To make comparisons to patients with an isolated Bankart lesion, the Mann-Whitney U test was used. A p-value ≤ 0.05 was considered statistically significant.
RESULTS
Postoperative Assessments
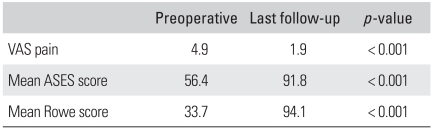
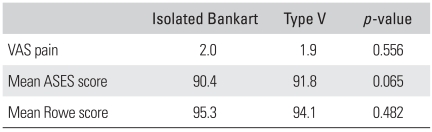
At the last follow-up, the mean VAS score for pain decreased from 4.9 preoperatively to 1.9 postoperatively. The mean ASES score and Rowe shoulder score increased from 56.4 and 33.7 preoperatively, to 91.8 and 94.1 postoperatively, respectively (p < 0.001) (Table 2). The shoulder joint function at the last follow-up was rated as excellent, good, fair, and poor according to the Rowe shoulder scoring system. All of the patients had better than good results (6 were excellent and 9 were good). Recurrent dislocation was not observed until the last follow-up and anterior instability was not noted during physical examination. In the comparison with the isolated Bankart lesion group, no statistical significance was found in the ASES score, Rowe shoulder score, or VAS score for pain (p > 0.05) (Table 3).
Table 2.
Comparison between Preoperative and Last Follow-up Score of Type V Superior Labrum Anterior to Posterior Lesion
VAS: Visual analogue scale, ASES: American Shoulder and Elbow Surgeons.
Table 3.
Last Follow-up Results between Isolated Bankart and Type V Superior Labrum Anterior to Posterior Lesion
VAS: Visual analogue scale, ASES: American Shoulder and Elbow Surgeons.
Range of Motion
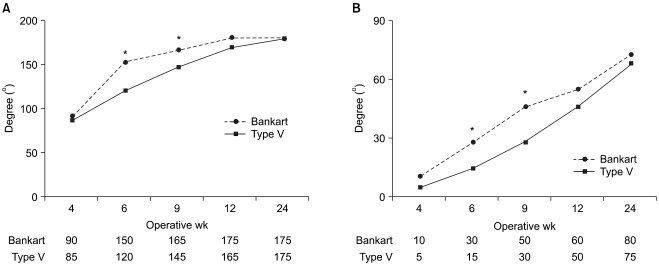
Anterior flexion, abduction, and internal rotation of the affected shoulder at the last follow-up were normal as they were before surgery. External rotation did not decrease ≥ 10° when the shoulder was placed in the neutral position and at 90° abduction in all cases. With regard to the time to recovery of the normal range of motion, forward elevation was 120° at the 6th postoperative week and was recovered to normal at the 12th postoperative week. External rotation with the shoulder positioned at 90° abduction improved from 30° at the 9th postoperative week to almost normal by the 6th postoperative month. Between the patients with isolated Bankart lesions and the patients with combined Bankart and SLAP lesions, no significant difference was found in terms of the range of motion measured at the last follow-up. However, the range of motion assessed between the 6th and 9th postoperative week was remarkably low the in the patients with combined Bankart and SLAP lesions. Therefore, the recovery of the normal range of motion was slower in the patients with combined Bankart and SLAP lesions (p < 0.05) (Fig. 7).
Fig. 7.
In type superior labrum anterior to posterior Lesion, the range of motions in (A) forward flexion and (B) external rotation at 90 degree abduction after the arthroscopic repair were gained more slowly than in patients with isolated Bankart lesion (*p < 0.05).
DISCUSSION
The glenoid labrum acts as shoulder joint stabilizer and a load distributor by deepening the glenoid cavity and increasing the surface of the shoulder joint. In 1985, Andrews et al.5) postulated that a SLAP lesion, an anteroposterior tear of the superior labrum, was caused by over loading and traction of the long head of the biceps tendon during the follow-through phase of throwing. Snyder et al.6) categorized SLAP lesions into 4 types and suggested that type II SLAP lesions were the most common injuries and were primarily responsible for pain and restricted mobility of the shoulder joint in overhead athletes. However, Maffet et al.2) added 3 more types to this classification, because 38% of the SLAP lesion patients did not fall into the classification by Snyder et al. in which instability of the shoulder joint and other combined intraarticular abnormalities were not taken into consideration. Among them, type V SLAP lesions are characterized by superior extension of an anteroinferior labral tear involving a Bankart lesion and are thought to be caused by traumatic instability. According to the domestic studies, 11% to 57% of the patients with recurrent dislocation had combined Bankart and SLAP lesions.7,8) In addition, we also found that 24% of the patients with Bankart lesions had SLAP lesions in our study.
Snyder et al.6) described the most common mechanisms of SLAP lesions as compression injuries of the upper limb and traction injuries of the superior labrum-biceps tendon complex with the shoulder in hyperextension while others postulated recurrent subluxation and dislocation were attributable. Particularly, primary lesions of complex labral tears such as type V SLAP lesions should be examined thoroughly. According to Soslowsky et al.,9) inferior subluxation of the shoulder resulted in type II SLAP lesions. Lo and Burkhart10) concluded that anterior lesions led to the injuries of the superior and posterior labrum because history of trauma was observed in the shoulders when positioned in abduction and external rotation. Considering that a history of trauma was observed and led to anterior instability in all patients in our study and symptoms associated with the SLAP lesions were not noted before the traumatic event, we believe that recurrent anteroinferior instability was mainly responsible for the SLAP lesions.
Contrary to the anteroinferior labrum, the superior labrum is often attached to the glenoid rim and when a sublabral sulcus is formed due to loose attachment, it can be mistaken for a labral tear. Nam and Snyder11) differentiated type II SLAP lesions from normal variants of the superior labrum. According to these researchers, type II SLAP lesions can be diagnosed when formation of hematoma or ingrowth of granulation tissue are observed, or if articular cartilage is not present medial to the attachment site, the superior labrum is detached from the glenoid when the biceps brachii is under tension (Peel-back mechanism), and concomitant tension of middle glenohumeral ligament is seen under arthroscopy when the superior labrum is pulled with a probe. In this study, we applied these researchers' definitions and performed repair of unstable SLAP lesions.
There is controversy over proper repair techniques of SLAP lesions. Debridement alone resulted in satisfying results in some studies,12,13) while it was described as producing poor results and having high potential for instability in other studies.14,15) While Bankart lesions are known as essential lesions for anterior instability in patients with recurrent dislocation, Rodosky et al.16) and Itoi et al.17) reported that superior labrum-biceps tendon complex lesions could also affect shoulder joint stability. Therefore, we removed possibility of instability by performing arthroscopic repair of not only Bankart lesions but also SLAP lesions.
While successful reports have been introduced on arthroscopic Bankart lesion repairs using suture anchors in patients with recurrent dislocation, there is little in the literature on the repair of accompanied labral tears, such as the combination of Bankart and SLAP lesions. According to Warner et al.,18) arthroscopic repair of 7 cases of combined Bankart and SLAP lesions using absorbable anchors (Suretec; Acufex, Mansfield, MA, USA) resulted in 1 recurrent dislocation and 1 reoperation due to stiffness during the ≥ 1 year follow-up. However, Suretec anchors are not recommended these days because movement of the glenoidal labrum may be restricted due to the lack of suture strands and complications, such as tack fragmentation and synovitis have been reported.19,20) In this study, no complications associated with suture anchors were found and chances of recurrent dislocation were reduced by obtaining proper movement of the glenoidal labrum with the use of suture strands.
No agreement has been reached on whether Bankart lesion repair should precede SLAP lesion repair or vice versa. Warner et al.18) recommended to perform Bank art lesion repair prior to SLAP lesion repair, but provided no specific reasons. Lo and Burkhart10) passed a suture through the SLAP lesion, closed the Bankart lesion, and then finished the SLAP lesion repair in the cases of triple labral lesions (anterior, posterior, and superior labral tears). Based on our experience, we thought that performing Bankart lesion repair first in cases of complex labral lesions would lengthen the operative time causing swelling of the soft tissues, especially of those located superior to the SLAP lesion and accordingly disrupting clear visualization during SLAP lesion repair. In addition, inferior and medial displacement of the superior and anteroinferior labrum caused by chronic dislocation required us to involve an inferior area of the labrum in the repair in order to obtain enough movement of the labrum. However, when stabilization of the unstable SLAP lesions were performed first, the bowstring effect of the labrum contributed to the maintenance of tension on the labrum and anatomical reduction of the anteroinferior labrum. Accordingly, Bankart lesion repair could be performed more efficiently.
Repairs of relatively extensive labral tears such as combined Bankart and SLAP lesions can result in restrictions on the range of motion. According to Warner et al.,18) no side-to-side difference was found with regard to external rotation when the shoulder was placed in the neutral position while it was restricted by 6° in the unaffected side when the shoulder was at 90° abduction. In this study, when the shoulder was either in the neutral position or at 90° abduction, ≥ 10° of restriction in external rotation was not observed. However, slower motion range recovery was noted in the combined Bankart and SLAP lesion patients compared to the isolated Bankart lesion patients. We attributed this to the difference in the extent of the lesions and intraarticular adhesion. Limited joint mobility is a relatively common complication in patients with isolated SLAP lesion repair. Oh et al.21) reduced the risk of postoperative stiffness by omitting closure of the anterosuperior labrum during SLAP lesion repair to reduce tension in the rotator interval. Therefore, we thought that the delay in the recovery of the range of motion was caused by closure of the anterosuperior labrum in patients at our institution. Although controversial, arthroscopic portals created for SLAP repair can affect postoperative functions of the shoulder. According to Cohen et al.,22) trans-rotator cuff portal resulted in 25% of reduction in function compared to the rotator interval portal. Therefore, we believed that the delay in joint motion observed in 10 in 15 of our patients with posterior labral tear might have been caused by the use of a transrotator cuff portal (port of Wilmington) which resulted in postoperative pain or impingement. The limitations of this study include the small study population and relatively short follow-up period. Therefore, we believe that studies involving more cases and a long-term follow-up period should be performed to clarify the reason for the delay in the recovery of the range of motions. In addition, we expect more studies will contribute to resolving the controversy over the precedence of Bankart lesion repair and SLAP lesion repair.
In recurrent dislocation of the shoulder with combined Bankart and SLAP lesion, arthroscopic repair using absorbable suture anchors produced favorable clinical results in terms of pain reduction and shoulder function improvement. This procedure may delay the postoperative recovery of the shoulder motions, but no statistically significant clinical limitations of motion were noted in anterior elevation and external rotation at the last follow-up examination. Therefore, repair of a concomitant unstable SLAP lesion, despite its technical difficulty, should be performed to stabilize the glenohumeral joint. In addition, we believe that Bankart lesion repair can be performed more easily when SLAP lesion repair precedes the Bankart lesion repair.
References
- 1.Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ. SLAP lesions of the shoulder. Arthroscopy. 1990;6(4):274–279. doi: 10.1016/0749-8063(90)90056-j. [DOI] [PubMed] [Google Scholar]
- 2.Maffet MW, Gartsman GM, Moseley B. Superior labrumbiceps tendon complex lesions of the shoulder. Am J Sports Med. 1995;23(1):93–98. doi: 10.1177/036354659502300116. [DOI] [PubMed] [Google Scholar]
- 3.Richards RR, An KN, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder and Elbow Surg. 1994;3(6):347–352. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 4.Rowe CR, Zarins B. Recurrent transient subluxation of the shoulder. J Bone Joint Surg Am. 1981;63(6):863–872. [PubMed] [Google Scholar]
- 5.Andrews JR, Carson WG, Jr, McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13(5):337–341. doi: 10.1177/036354658501300508. [DOI] [PubMed] [Google Scholar]
- 6.Snyder SJ, Banas MP, Karzel RP. An analysis of 140 injuries to the superior glenoid labrum. J Shoulder Elbow Surg. 1995;4(4):243–248. doi: 10.1016/s1058-2746(05)80015-1. [DOI] [PubMed] [Google Scholar]
- 7.Kim KT, Kim CH, Kim SH. Arthroscopic Bankart repair with suture anchor. J Korean Orthop Sports Med. 2002;1(2):149–153. [Google Scholar]
- 8.Rhee YG, Kim YK, Chun YS. Arthroscopic fixation for unstable SLAP lesion using biodegradable tack. J Korean Orthop Assoc. 1998;33(3):508–514. [Google Scholar]
- 9.Soslowsky LJ, Malicky DM, Blasier RB. Active and passive factors in inferior glenohumeral stabilization: a biomechanical model. J Shoulder Elbow Surg. 1997;6(4):371–379. doi: 10.1016/s1058-2746(97)90005-7. [DOI] [PubMed] [Google Scholar]
- 10.Lo IK, Burkhart SS. Triple labral lesions: pathology and surgical repair technique-report of seven cases. Arthroscopy. 2005;21(2):186–193. doi: 10.1016/j.arthro.2004.09.022. [DOI] [PubMed] [Google Scholar]
- 11.Nam EK, Snyder SJ. The diagnosis and treatment of superior labrum, anterior and posterior (SLAP) lesions. Am J Sports Med. 2003;31(5):798–810. doi: 10.1177/03635465030310052901. [DOI] [PubMed] [Google Scholar]
- 12.Depuy J, Steiner ME. Isolated shoulder labral tears: treatment and correlation with labral anatomy. Orthop Trans. 1990;14(2):244. [Google Scholar]
- 13.Resch H, Golser K, Thoeni H, Sperner G. Arthroscopic repair of superior glenoid labral detachment (the SLAP lesion) J Shoulder Elbow Surg. 1993;2(3):147–155. doi: 10.1016/S1058-2746(09)80051-7. [DOI] [PubMed] [Google Scholar]
- 14.Ogilvie-Harris DJ, Wiley AM. Arthroscopic surgery of the shoulder: a general appraisal. J Bone Joint Surg Br. 1986;68(2):201–207. doi: 10.1302/0301-620X.68B2.3958003. [DOI] [PubMed] [Google Scholar]
- 15.Pappas AM, Goss TP, Kleinman PK. Symptomatic shoulder instability due to lesions of the glenoid labrum. Am J Sports Med. 1983;11(5):279–288. doi: 10.1177/036354658301100501. [DOI] [PubMed] [Google Scholar]
- 16.Rodosky MW, Harner CD, Fu FH. The role of the long head of the biceps muscle and superior glenoid labrum in anterior stability of the shoulder. Am J Sports Med. 1994;22(1):121–130. doi: 10.1177/036354659402200119. [DOI] [PubMed] [Google Scholar]
- 17.Itoi E, Kuechle DK, Newman SR, Morrey BF, An KN. Stabilising function of the biceps in stable and unstable shoulders. J Bone Joint Surg Br. 1993;75(4):546–550. doi: 10.1302/0301-620X.75B4.8331107. [DOI] [PubMed] [Google Scholar]
- 18.Warner JJ, Kann S, Marks P. Arthroscopic repair of combined Bankart and superior labral detachment anterior and posterior lesions: technique and preliminary results. Arthroscopy. 1994;10(4):383–391. doi: 10.1016/s0749-8063(05)80188-4. [DOI] [PubMed] [Google Scholar]
- 19.Freehill MQ, Harms DJ, Huber SM, Atlihan D, Buss DD. Poly-L-lactic acid tack synovitis after arthroscopic stabilization of the shoulder. Am J Sports Med. 2003;31(5):643–647. doi: 10.1177/03635465030310050201. [DOI] [PubMed] [Google Scholar]
- 20.Wilkerson JP, Zvijac JE, Uribe JW, Schurhoff MR, Green JB. Failure of polymerized lactic acid tacks in shoulder surgery. J Shoulder Elbow Surg. 2003;12(2):117–121. doi: 10.1067/mse.2003.16. [DOI] [PubMed] [Google Scholar]
- 21.Oh JH, Kim SH, Lee HK, Jo KH, Bae KJ. Trans-rotator cuff portal is safe for arthroscopic superior labral anterior and posterior lesion repair: clinical and radiological analysis of 58 SLAP lesions. Am J Sports Med. 2008;36(10):1913–1921. doi: 10.1177/0363546508317414. [DOI] [PubMed] [Google Scholar]
- 22.Cohen DB, Coleman S, Drakos MC, et al. Outcomes of isolated type II SLAP lesions treated with arthroscopic fixation using a bioabsorbable tack. Arthroscopy. 2006;22(2):136–142. doi: 10.1016/j.arthro.2005.11.002. [DOI] [PubMed] [Google Scholar]