Abstract
Objective
To determine the efficacy of antibacterial prophylaxis in preventing infectious complications after percutaneous endoscopic gastrostomy.
Design
Prospective, randomised, placebo controlled, double blind, multicentre study.
Setting
Departments of internal medicine at six German hospitals.
Subjects
Of 106 randomised adult patients with dysphagia, 97 received study medication, and 84 completed the study. The median age of the patients was 65 years. Most had dysphagia due to malignant disease (65%), and many (76%) had serious comorbidity.
Interventions
A single intravenous 2.2 g dose of co-amoxiclav or identical appearing saline was given 30 min before percutaneous endoscopic gastrostomy performed by the thread pull method.
Main outcome measures
Occurrence of peristomal wound infections and other infections within one week after percutaneous endoscopic gastrostomy.
Results
The incidence of peristomal and other infections within one week after percutaneous endoscopic gastrostomy was significantly reduced in the antibiotic group (8/41 (20%) v 28/43 (65%), P<0.001). Similar results were obtained in an intention to treat analysis. Several peristomal wound infections were of minor clinical significance. After wound infections that required no or only local treatment were excluded from the analysis, antibiotic prophylaxis remained highly effective in reducing clinically important wound infections (1/41 (2%) v 11/43 (26%), P<0.01) and non-wound infections (2 (5%) v 9 (21%), P<0.05).
Conclusions
Antibiotic prophylaxis with a single dose of co-amoxiclav significantly reduces the risk of infectious complications after percutaneous endoscopic gastrostomy and should be recommended.
Key messages
Percutaneous endoscopic gastrostomy for enteral feeding can be associated with substantial rates of infectious complications, notably peristomal wound infection
Small, single centre studies on prevention of wound infection by antibiotic prophylaxis have given conflicting results
This prospective, randomised, placebo controlled, double blind, multicentre study showed that a single dose of 2.2 g co-amoxiclav significantly reduced the rate of infection
The favourable effect of antibiotic prophylaxis included a reduction in the rate of clinically important peristomal wound infection
Intention to treat analysis indicated a significant reduction in the need for therapeutic antibiotics
Introduction
Percutaneous endoscopic gastrostomy is commonly used for long term enteral feeding of patients with severe dysphagia.1–5 The most common complication is peristomal wound infection.5–11 Several investigators have reported low rates of wound infection in patients who were already receiving antibiotics at the time of percutaneous endoscopic gastrostomy,6,9,11 and some centres routinely use antibiotic prophylaxis.2,12 Conflicting results, however, have been obtained in prospective clinical trials of antibiotic prophylaxis in percutaneous endoscopic gastrostomy, and its value in reducing wound infection rates is controversial.8–11 To resolve the issue, we planned a large, prospective, randomised, double blind, multicentre study of antibiotic prophylaxis in percutaneous endoscopic gastrostomy.
Participants and methods
Patients
Eligible patients were at least 18 years of age and were referred for percutaneous endoscopic gastrostomy because of dysphagia. Exclusion criteria were a contraindication to percutaneous endoscopic gastrostomy, known allergy to a penicillin, treatment with any antibiotic within the past 4 days, neutropenia (<500 cells/μl), or serum creatinine concentration>300 μmol/l. Patients could be entered into the study only once. Written informed consent was required, and the study was approved by the ethics boards of the participating centres.
Assignment
We conducted a double blind, placebo controlled, clinical trial at six German hospitals. We used a permuted block design, with separate sequences of random numbers for each centre, to assign patients in roughly equal numbers to antibiotics or placebo. A sample size of 180 patients was required for a two sided test to detect a reduction in the incidence of peristomal wound and other infections in the antibiotic group from 20% to 5% at a significance level of 0.05 and a power of 0.80 and at an evaluability rate of 85%.
Because of a high overall incidence of infection after blinded review of 65 patients, an adaptive interim analysis of efficacy was performed by a biostatistician who had no other part in the study.13 The analysis estimated the difference in the infection rate as significant at the 0.05 level if the P value was less than 0.0234, with a one sided Fisher’s exact test. A P value of 0.00068 was calculated for the difference in infection rates in both groups. We therefore decided to terminate the study, at which time 106 patients had been randomised. The blinding for investigators, study nurses, reviewers, and data managers was maintained until data review for all patients was complete.
Treatment
About 30 minutes before endoscopy patients received either 2.2 g co-amoxiclav or identical appearing saline by short intravenous infusion. The medication was prepared in the hospital pharmacy or in a separate room and administered to patients by staff not involved in the study or care of the patients.
Percutaneous endoscopic gastrostomy was performed by the thread pull method.1 Tubes with a 3.6 mm inner and 4.8 mm outer diameter were routinely used (15 Ch/Fr Universalgastral, Fresenius, Bad Homburg, Germany). In a few cases tubes of 1.9 mm inner and 2.9 mm outer diameter (9 Ch/Fr Standardgastral, Fresenius) were used. Twenty four hours after gastrostomy, tea was administered through the tube, and after 48 hours, enteral feeding was started.
Monitoring and evaluation
The patients were followed for at least 7 days. Blood cell counts were done on days 1, 4, and 7 after gastrostomy, and serum creatinine and aminotransferase concentrations were measured on day 4. Monitoring included the measurement of body temperature three times daily, recording of peritoneal irritation and abdominal pain, and assessment of potential adverse events and clinical complications.
The peristomal region was examined daily, cleaned, and bandaged dry without antiseptic ointments. Peristomal erythema, induration, and wound secretions were noted and scored as proposed by Jain et al.9 The score was calculated by summing up the individual scores for erythema (0=none, 1=<5 mm, 2=6-10 mm, 3=11-15 mm, 4=>15 mm), induration (0=none, 1=<10 mm, 2=11-20 mm, 3 = >20 mm), and exudate (0=none, 1=serous, 2=serosanguinous, 3=sanguinous). When purulent secretion was suspected we collected material for microscopy and culture. Peristomal wound infection was defined either as a score >8 points or as microscopic evidence of suppurating secretion. The infection was considered clinically important if surgery or systemic antibiotics were required.
For patients with fever or other signs of infection, clinical and laboratory examinations were done and appropriate cultures taken to define the infection. Bacterial pathogens were identified and differentiated by standard methods. The susceptibility testing for co-amoxiclav was done by disc diffusion tests.
We recorded the occurrence of peristomal wound infection as defined above and of any other infection that required surgery or systemic antibiotics within 7 days after gastrostomy as a primary efficacy variable. The occurrence of serious adverse events and survival within 30 days after the procedure were also recorded.
Statistical analysis
We performed the analysis of efficacy as per protocol, including eligible patients with adequate data during follow up, and on an intention to treat basis, including all patients who received placebo or antibiotics and who had gastrostomy. The analysis of safety included all patients who received study medication. Fisher’s exact test was used to compare proportions. Wilcoxon’s test was used to assess quantitative variables. The time to onset of infection was analysed by Kaplan-Meier estimates and a log rank test. These tests were two sided.
Results
Participant flow
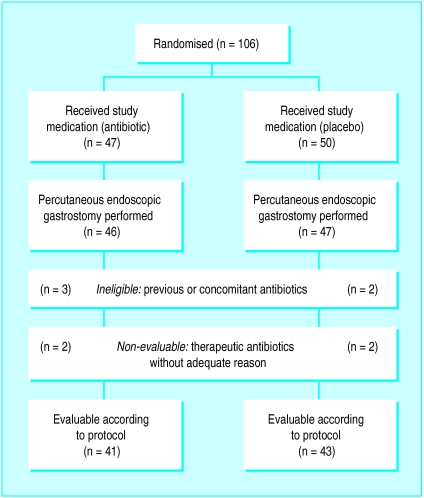
Of the 106 patients enrolled, eight did not receive study medication and one had inadequate documentation of drug administration. The remaining 97 patients were included in the analysis of safety. Thirteen patients (six in the antibiotic arm and seven in the placebo arm) were excluded from the per protocol analysis for various reasons (fig 1). Three patients developed non-infectious complications including bleeding, hypotension, and peritoneal irritation with abdominal pain. None of these complications was fatal.
Figure 1.
Participant flow and reasons for exclusion from per protocol analysis of efficacy
Per protocol analysis
Table 1 shows the demographic and clinical characteristics of the evaluable patients at baseline. Most of the patients had dysphagia due to malignant disease (65%), and many patients had serious comorbidity (76%). Patients in both arms had comparable baseline characteristics.
Table 1.
Demographic and baseline clinical characteristics of evaluable patients. Values are numbers (percentages) of patients unless stated otherwise*
| Characteristic | Co-amoxiclav (n=41) | Placebo (n=43) |
|---|---|---|
| Sex (M/F) | 30/11 | 31/12 |
| Median (range) age (years) | 69 (45B88) | 60 (36B93) |
| Median (range) body weight (kg) | 60 (40B113) | 60 (39B85) |
| Underlying disease: | ||
| Epipharyngeal/hypopharyngeal tumour | 15 (37) | 17 (40) |
| Oesophageal tumour | 8 (20) | 7 (16) |
| Other malignancy | 5 (12) | 3 (7) |
| Neurological disease | 13 (32) | 16 (37) |
| Previous method of feeding: | ||
| Oral | 31 (76) | 28 (65) |
| Nasogastric tube | 5 (12) | 6 (14) |
| Parenteral | 5 (12) | 9 (21) |
| Comorbidity: | ||
| Any | 30 (73) | 34 (79) |
| Multiple | 24 (59) | 25 (58) |
| Diabetes mellitus | 5 (12) | 3 (7) |
| Cardiovascular disease | 22 (54) | 21 (49) |
| Pulmonary disease | 6 (15) | 5 (12) |
| Cancer | 4 (10) | 3 (7) |
| Neurological disease | 7 (17) | 5 (12) |
| Performance status†: | ||
| 1B2 | 9 (22) | 14 (33) |
| 3B4 | 15 (36) | 11 (26) |
| 5B6 | 6 (15) | 5(12) |
| >6 | 11 (27) | 13 (30) |
Both groups were comparable in demographic and baseline clinical characteristics.
Karnofsky index.
The incidence of any infection within 7 days was significantly lower in the antibiotic arm than in the placebo arm (table 2). Eight of 41 (20%) patients in the antibiotic arm developed infection compared with 28 of 43 (65%) patients receiving placebo (P<0.001). The effect of prophylaxis on infection rates was similar in patients with cancer (21% v 63% in placebo group) and neurological disease (15% v 69%).
Table 2.
Rates of infection after percutaneous endoscopic gastrostomy
|
Co-amoxiclav (n=41)
|
Placebo (n=43)
|
% difference (95% CI) | P value | ||||
|---|---|---|---|---|---|---|---|
| No (%) of patients | 95% CI (%) | No (%) of patients | 95% CI (%) | ||||
| Total | 8 (20) | 6 to 29 | 28 (65) | 29 to 60 | 46 (25 to 66) | <0.001 | |
| Peristomal wound infection | 6 (15) | 6 to 29 | 19 (44) | 29 to 60 | 30 (9 to 51) | 0.004 | |
| Minor | 5 (13) | 4 to 26 | 8 (19) | 8 to 33 | 6 (−13 to 28) | >0.1 | |
| Clinically important | 1 (2) | 0 to 13 | 11 (26) | 14 to 41 | 23 (5 to 44) | 0.003 | |
| Other infection | 2 (5)* | 1 to 17 | 9 (21)† | 10 to 36 | 16 (0 to 30) | 0.049 | |
Urinary tract infections.
Urinary tract infection (four patients), pneumonia (three), bacteraemia (one), and unexplained fever (one).
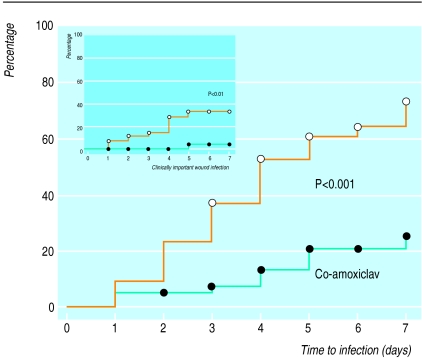
Peristomal wound infection was diagnosed in six (15%) patients who had received co-amoxiclav and 19 (44%) who had received placebo (P=0.004) (table 2). No wound without purulent secretion had a maximum combined daily wound score of 8 points. Since purulent secretion alone was diagnostic of wound infection in this study, the wound score did not add sensitivity in evaluating this end point. Only one patient who received co-amoxiclav developed clinically important wound infection compared with 11 who received placebo (P=0.003) (table 2). Figure 2 shows the time to infection in the two groups. Clinically important wound infections occurred within 5 days after gastrostomy. Non-wound infections were less common among the co-amoxiclav group than the placebo group (table 2).
Figure 2.
Kaplan-Meier plots showing time to infection (any site) and time to clinically important wound infection (requiring medical or surgical treatment) after percutaneous endoscopic gastrostomy. P values are from log rank tests
Table 3 shows the bacterial pathogens causing infection. No Staphylococcus aureus or streptococci infections occurred in the co-amoxiclav group. Three Gram negative isolates were resistant to co-amoxiclav in vitro. Clinically important infections were more common among patients with culture positive than culture negative wound infections (10/13 v 2/12).
Table 3.
Bacterial pathogens isolated from patients with infectious complications within 7 days after percutaneous endoscopic gastrostomy
| No given co-amoxiclav | No given placebo | |
|---|---|---|
| Wound isolates: | ||
| Staphylococcus aureus | 0 | 1 |
| Streptococci | 0 | 4 |
| Gram negative bacteria | 0 | 3 |
| Polymicrobial or mixed | 3 | 2 |
| No positive culture | 3 | 9 |
| Other isolates: | ||
| Staphylococcus aureus | 0 | 2 |
| Gram negative bacteria | 2† | 3* |
| Polymicrobial or mixed | 0 | 1† |
| No positive culture | 0 | 3 |
One isolate in each group was resistant in vitro to co-amoxiclav.
Pneumonia due to Proteus sp and co-amoxiclav resistant Pseudomonas aeruginosa.
Intention to treat analysis
An intention to treat analysis confirmed the differences in infection rates (table 4); 10/46 (22%) patients in the antibiotic arm and 31/47 (66%) in the placebo arm developed infection (P<0.001). The difference between the groups was large for clinically important wound infections but non-significant for minor wound infection. One patient who was excluded from the per protocol analysis required tube replacement in the week after gastrostomy because of leakage leading to peritonitis.
Table 4.
Intention to treat analysis for infection after percutaneous endoscopic gastrostomy with and without antibiotic use
| No (%) in co-amoxiclav group (n=46) | No (%) in placebo group (n=47) | % difference (95% CI) | P value | |
|---|---|---|---|---|
| Infection: | 10 (22) | 31 (66) | 44 (24 to 64) | <0.001 |
| Minor wound | 6 (13) | 9 (19) | 6 (−12 to 27) | >0.01 |
| Clinically important wound | 1 (2) | 12 (26) | 23 (7 to 43) | <0.002 |
| Other | 3 (7) | 10 (21) | 15 (−2 to 35) | <0.07 |
| Antibiotic use* | 6 (13) | 24 (51) | 38 (19 to 58) | <0.001 |
Includes patients who were given new antibiotics within 7 days after percutaneous endoscopic gastrostomy.
Antibiotics were required in the week after the procedure by six patients (24%) in the co-amoxiclav arm and 24 (51%) in the placebo arm (P<0.001). The numbers include two patients in each arm who received antibiotics without adequate reason.
Adverse events
A total of 20 adverse events were reported in 19 patients who received co-amoxiclav and 26 in 18 patients who received placebo. Adverse events that were possibly or probably related to the study medication included nausea (one patient) and seizure (one) in the co-amoxiclav group and vomiting (one) and suspected allergic exanthema (one) in the placebo group. Seven patients in the antibiotic arm and eight in the placebo arm died within 30 days after gastrostomy. One patient in the antibiotic arm died of pneumonia (on day 16) compared with three in the placebo arm (days 5, 10, and 21); the remaining deaths were due to underlying disease.
Discussion
Our study shows that antibiotic prophylaxis with a single dose of co-amoxiclav reduces infection after percutaneous endoscopic gastrostomy. The study was larger than previous studies of antibiotic prophylaxis in percutaneous endoscopic gastrostomy,8–11 two of which found no reduction in the incidence of peristomal wound infection.8 11
Infection rate and patient selection
We studied mainly patients at increased risk of infection such as cancer patients and patients admitted to hospital for various reasons. Many of our ambulatory, healthier patients were not randomised because they could not be followed up for at least 7 days. Malignancy has previously been associated with an increased risk of complication after percutaneous endoscopic gastrostomy.14,15 Other studies indicate that patients with neurological disease may be more prone to infection than patients with cancer.8 Several previous studies noted a high risk of infectious complications. In a study in which over half the patients had cancer the overall incidence of infection after percutaneous endoscopic gastrostomy was 42%,10 and Jain et al found that patients receiving placebo had a 32% increased risk of wound infection.9
Diagnostic criteria for wound infection
Jain et al’s criteria to define wound infection9 seemed helpful in the daily monitoring of study subjects, but, as reported previously,11 the score was not better than purulent secretion alone as a diagnostic criterion. Purulent secretion, on the other hand, may be non-specific. Patients who had sterile cultures and required no medical or surgical treatment may have had inflammatory reactions associated with foreign material rather than true infection. Such minor or presumed wound infections occurred with a similar frequency among patients given antibiotics and placebo. Previous studies have reported low rates of wound infection requiring treatment among patients given antibiotic prophylaxis.9,10 These rates are comparable with the 2% that we observed.
Choice of drug and dose
The choice of prophylactic regimen is unlikely to account for the differing results of previous trials. Jonas et al used three doses of cefoxitin and found no effect on wound infection,8 whereas Jain et al reported significant protection with a single dose of cefazolin,9 a drug less effective against anaerobic bacteria than cefoxitin or co-amoxiclav but similarly effective against aerobic organisms from the upper gastrointestinal tract and mouth flora. A single dose of co-amoxiclav (and probably of other comparable antibiotics) may be sufficient prophylaxis against wound infections after percutaneous endoscopic gastrostomy, as it is for prophylaxis in gastrointestinal surgery.16
Outcome and survival
The mortality within 30 days after gastrostomy was 14% in both groups, a similar rate to that reported in other studies.17–19 Although we observed a lower rate of non-wound infections (including pneumonia) in antibiotic recipients than placebo recipients, this did not seem to affect survival. This is not surprising since a single dose of an antibiotic is unlikely to affect rates of infection and associated complications several weeks later. In addition, many of our patients died because of their underlying malignant disease.
Conclusion
We recommend giving antibiotic prophylaxis before percutaneous endoscopic gastrostomy. It is well tolerated, easy to perform, and reduces morbidity and the need for treatment because of infection. Our results show that a single intravenous dose of co-amoxiclav is effective.
Acknowledgments
We thank Birgit Hay and Beate Maute for data management and Martina Kron, department of clinical documentation and biometry, University of Ulm, for performing the interim analysis.
Footnotes
Funding: The study was in part supported by a clinical research grant from SmithKline Beecham Pharma, München, Germany.
Competing interests: KM is employed by SmithKline Beecham, which makes co-amoxiclav.
References
- 1.Gauderer MW, Ponsky JL, Izant RJ., Jr Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 1980;15:872–875. doi: 10.1016/s0022-3468(80)80296-x. [DOI] [PubMed] [Google Scholar]
- 2.Ponsky JL, Gauderer MWL, Stellato TA. Percutaneous endoscopic gastrostomy. Review of 150 cases. Arch Surg. 1983;118:913–914. doi: 10.1001/archsurg.1983.01390080021006. [DOI] [PubMed] [Google Scholar]
- 3.Beasley SW, Catto Smith AG, Davidson PM. How to avoid complications during percutaneous endoscopic gastrostomy. J Pediatr Surg. 1995;30:671–673. doi: 10.1016/0022-3468(95)90687-8. [DOI] [PubMed] [Google Scholar]
- 4.Chung RS, Schertzer M. Pathogenesis of complications of percutaneous endoscopic gastrostomy. A lesson in surgical principles. Am Surg. 1990;56:134–137. [PubMed] [Google Scholar]
- 5.Schapiro GD, Edmundowicz SA. Complications of percutaneous endoscopic gastrostomy. Gastrointest Endosc Clin N Am. 1996;6:409–422. [PubMed] [Google Scholar]
- 6.Chowdhury MA, Batey R. Complications and outcome of percutaneous endoscopic gastrostomy in different patient groups. J Gastroenterol Hepatol. 1996;11:835–839. doi: 10.1111/j.1440-1746.1996.tb00089.x. [DOI] [PubMed] [Google Scholar]
- 7.Bourdel-Marchasson I, Dumas F, Pinganaud G, Emeriau JP, Decamps A. Audit of percutaneous endoscopic gastrostomy in long-term enteral feeding in a nursing home. Int J Qual Health Care. 1997;9:297–302. doi: 10.1093/intqhc/9.4.297. [DOI] [PubMed] [Google Scholar]
- 8.Jonas SK, Neimark S, Panwalker AP. Effect of antibiotic prophylaxis in percutaneous endoscopic gastrostomy. Am J Gastroenterol. 1985;80:438–441. [PubMed] [Google Scholar]
- 9.Jain NK, Larson DE, Schroeder KW, Burton DD, Cannon KP, Thompson RL, et al. Antibiotic prophylaxis for percutaneous endoscopic gastrostomy. A prospective, randomized, double-blind clinical trial. Ann Intern Med. 1987;107:824–828. doi: 10.7326/0003-4819-107-6-824. [DOI] [PubMed] [Google Scholar]
- 10.Akkersdijk WL, van Bergeijk JD, van Egmond T, Mulder CJJ, van Berge-Henegouwen GP, ven der Werken C, et al. Percutaneous endoscopic gastrostomy (PEG): comparison of push and pull methods and evaluation of antibiotic prophylaxis. Endoscopy. 1995;27:313–316. doi: 10.1055/s-2007-1005699. [DOI] [PubMed] [Google Scholar]
- 11.Sturgis TM, Yancy W, Cole JC, Proctor DD, Minhas BS, Marcuard SP. Antibiotic prophylaxis in percutaneous endoscopic gastrostomy. Am J Gastroenterol. 1996;91:2301–2304. [PubMed] [Google Scholar]
- 12.Gutt CN, Held S, Paolucci V, Encke A. Experiences with percutaneous endoscopic gastrostomy. World J Surg. 1996;20:1006–1008. doi: 10.1007/s002689900153. [DOI] [PubMed] [Google Scholar]
- 13.Bauer P, Köhne K. Evaluation of experiments with adaptive interim analyses. Biometrics. 1994;50:1029–1041. [PubMed] [Google Scholar]
- 14.Amann W, Mischinger HJ, Berger A, Rosanelli G, Schweiger W, Werkgartner G, et al. Percutaneous endoscopic gastrostomy (PEG). 8 years of clinical experience in 232 patients. Surg Endosc. 1997;11:741–744. doi: 10.1007/s004649900440. [DOI] [PubMed] [Google Scholar]
- 15.Fox VL, Abel SD, Malas SD, Duggan C, Leichtner AM. Complications following percutaneous endoscopic gastrostomy and subsequent catheter replacement in children and young adults. Gastrointest Endosc. 1997;45:64–71. doi: 10.1016/s0016-5107(97)70304-3. [DOI] [PubMed] [Google Scholar]
- 16.Ball P, Geddes A, Rolinson G. Amoxicillin clavulanate: an assessment after 15 years of clinical application. J Chemother. 1997;9:167–198. doi: 10.1179/joc.1997.9.3.167. [DOI] [PubMed] [Google Scholar]
- 17.Raha SK, Woodhouse K. The use of percutaneous endoscopic gastrostomy in 161 consecutive elderly patients. Age Ageing. 1994;23:162–163. doi: 10.1093/ageing/23.2.162. [DOI] [PubMed] [Google Scholar]
- 18.Kohli H, Bloch R. Percutaneous endoscopic gastrostomy: a community hospital experience. Am Surg. 1995;61:191–194. [PubMed] [Google Scholar]
- 19.Light VL, Slezak FA, Porter JA, Gerson LW, McCord G. Predictive factors for early mortality after percutaneous endoscopic gastrostomy. Gastrointest Endosc. 1995;42:330–335. doi: 10.1016/s0016-5107(95)70132-x. [DOI] [PubMed] [Google Scholar]