Abstract
The rise in obesity levels in the U.S. in the past several decades has been dramatic, with serious implications for public health and the economy. Experiences in tobacco control and other public health initiatives have shown that public policy may be a powerful tool to effect structural change to alter population-level behavior. In 2007, the National Cancer Institute convened a meeting to discuss priorities for a research agenda to inform obesity policy. Issues considered were how to define obesity policy research, key challenges and key partners in formulating/implementing an obesity policy research agenda, criteria by which to set research priorities, and specific research needs and questions. Themes that emerged were: (1) the embryonic nature of obesity policy research, (2) the need to study “natural experiments” resulting from policy-based efforts to address the obesity epidemic, (3) the importance of research focused beyond individual-level behavior change, (4) the need for economic research across several relevant policy areas, and (5) the overall urgency of taking action in the policy arena. Moving forward, timely evaluation of natural experiments is of especially high priority. A variety of policies intended to promote healthy weight in children and adults are being implemented in communities and at the state and national levels. Although some of these policies are supported by the findings of intervention research, additional research is needed to evaluate the implementation and quantify the impact of new policies designed to address obesity.
Introduction
In June 2007, the National Cancer Institute (NCI) convened a half-day meeting aimed at identifying research priorities and other issues related to environmental and policy influences on diet, physical activity, energy balance, and health behavior that could effect positive change in the obesity epidemic at the population and societal levels. This paper provides an overview of the meeting's background and structure, reports on the outcomes from the meeting, and concludes with a discussion of obesity policy research topic areas, key themes from the meeting discussions, and implications for obesity policy research.
The rise in obesity levels in the U.S. in the past several decades has been dramatic, with alarming implications for public health and the economy. By the metrics developed in the Healthy People 2010 initiative,1 the prevalence of obesity is unacceptably high in all social and economic groups, in both genders and in all age groups. Sustained, corrective shifts in energy intake and expenditure will be needed to reduce current obesity levels.
Obesity has serious health and economic implications. It is a known risk factor for a wide range of chronic diseases, debilitating conditions, and psychosocial problems.2–4 Widespread obesity has not only devastating human costs, but also growing direct and indirect costs that threaten to overwhelm public and private healthcare budgets and broadly affect the economy. Researchers have estimated that 9.1% of U.S. healthcare spending in 1998—$78.5 billion ($105.9 billion in 2008 dollars)—was the result of conditions related to overweight and obesity. Half of this sum was financed by Medicare and Medicaid.5 General healthcare spending in the U.S. has increased from 7.2% of gross domestic product (GDP) in 1970 to 16% in 2006,6 and it is projected to rise to 19.5% of GDP by 2017.7 A study by Thorpe and colleagues8 estimated that 27% of the rise in healthcare spending between 1987 and 2001 was explained by obesity. In addition to direct healthcare costs, obesity increases indirect costs, such as disability, absenteeism, and decreased productivity.9
The causes of the rise in obesity levels are simultaneously straightforward and complex. Weight gain is the result of energy intake exceeding expenditure over time, and energy balance has obviously been positive for many people. Evidence suggests that average caloric intake in the U.S. has increased in recent decades10,11 and that the per-capita energy available in the nation's food supply is higher now than during any period in the past century.12 In addition, it is clear that the total energy expenditure associated with physical activity has not compensated for this increase in intake. 13–16
The understanding of the contribution of genetics to obesity is increasing rapidly. However, genetics alone cannot explain the increase in overweight and obesity rates. Instead, it seems likely that the rise in obesity prevalence stems from a complex array of environmental factors that—in combination with genetics—affect diet, physical activity, sleep, and other human behaviors that are currently understood to influence weight change. Environmental correlates of increasing obesity prevalence span the community, societal, national, and international environments. These correlates include: increased portion sizes17,18; school food and physical activity environments19–21; the physical form of communities, or the built environment15,22,23; the community food environment24–28; relatively high costs of fresh produce and other nutrient-dense foods29; technologic advances leading to decreased costs of food and reduced requirements for physical activity30,31; and marketing of high-calorie and low-nutrient food, especially to children.20,32
The rapid rise in obesity rates and the evidence of environmental influences have stimulated interest in examining the potential for broad systemic changes, including policy initiatives, to modify the food and physical activity environments in ways that may foster the sustained changes needed to reduce obesity at the population level. Policy is recognized as a powerful instrument to influence public health generally,33,34 and public health policies aimed at reducing tobacco use (e.g., tobacco tax increases; smoke-free air laws; restrictions on product packaging, labeling, promotion, and youth access; changes to subsidies and agricultural policies; counter-advertising) have altered the environment in which individuals make choices about tobacco use and cessation. Policy-based strategies have been very effective as methods of tobacco control,35,36 and they have formed the basis of many other successful public health initiatives, including seat belt use, vaccinations, and occupational safety.34,37,38
A growing number and variety of policies are being implemented that are intended to promote healthy eating and physical activity patterns in order to achieve healthy body weight at local and state levels of government. Many of these have targeted the food environment and activity requirements in schools. Although there are promising findings from research interventions at school, community, and state levels, relatively little is known about the absolute and relative effects of policy changes on diet and physical activity behavior and health outcomes. Additional research is clearly needed to examine the potential impact of proposed policies and to evaluate and quantify the effects of newly implemented policies designed to address obesity. Findings from these and other studies may help to inform future policy decision-making and resource allocation.
In light of (1) the link between obesity and adverse health conditions, (2) the paucity of existing research, and (3) the powerful effects of policy interventions seen in tobacco control, NCI and other NIH groups are interested in identifying promising research directions that can contribute to the evidence base of how best to effect positive population-level change to reduce obesity and promote improved health among Americans. Strategies to foster such shifts will need to address environmental and policy influences on nutrition and physical activity behaviors in addition to influences that act at the individual level. Some initial research activities have begun at NCI to foster research that may be relevant to policy in this area (see, for instance, www.appliedresearch.cancer.gov/funding/econ_diet_act_ener_fact_sheet.pdf and www.appliedresearch.cancer.gov/funding/geog_cont_energy_bal_pa_fact_sheet.pdf). In addition, NIH, the CDC, and the Robert Wood Johnson Foundation (RWJF) are working together to identify areas for collaborative efforts on this topic. Leadership in research in this area is consistent with the component of the NIH mission that calls for applying knowledge to extend healthy life and reduce the burdens of illness and disability. The following sections discuss the process and outcomes of the meeting convened by NCI.
Process
The 27 participants in the meeting included experts in medicine, public health, nutrition, physical activity, economics, health policy and legislation, and healthcare delivery systems. The participants represented a range of organizations, including academic research institutions, health organizations, private and federal research funding agencies, and state and federal government agencies. Meeting planners intentionally crafted this diversity of expertise and representation in order to address the complexity of the issue and reflect the need for solutions at multiple levels. Several participants were and continue to be involved directly in policymaking, which helped focus the discussions on research needed for real world concerns. In the weeks before the meeting, a professional meeting facilitator conducted semistructured telephone interviews with 11 nongovernment experts who had been invited to the meeting. The issues and information that emerged from these interviews were used to refine the meeting agenda and provided an important starting point for many of the discussions.
The meeting was structured around a series of facilitated brainstorming discussions on the following topics: defining obesity policy research, enumerating key challenges in formulating and/or implementing an obesity policy research agenda, and identifying key partners. Participants also proposed criteria by which to set research priorities, then identified broad obesity policy research categories. Using a modified nominal group process,39 participants developed a prioritized list of specific research needs and questions within each category. A conference call was held by NCI after the meeting to clarify certain points. The results of these discussions and deliberations are reported below.
Results
Obesity Policy Research Definition
The term “obesity policy research” can be interpreted in many ways. After extensive discussion, participants recommended defining the term as: the application of quantitative and qualitative research methods to (1) understand the policy-related determinants of obesity and its population-level health and economic consequences and (2) inform policy-based strategies intended to modify obesity's prevalence and trends. Although not explicitly included, the definition should encompass the following: analysis of existing policies; the direct and indirect effect of policy on diet, physical activity, weight, and energy-balance behavior; the impact of policy on social norms; sustainability of activities and behavior; multiple or various policy impacts on specific population groups; and the effects of terminated policies.
Key Challenges in Formulating/Implementing an Obesity Policy Research Agenda
Policy research, whether on education, health, national security, or other areas, is different in many respects from research typically conducted in health behavior research and poses different methodologic challenges. In the context of policy research, interventions, specific behavioral modifiers, and the general environment under study are often outside the direct control of researchers. Changes in these factors may occur for reasons that—although affecting diet and/or physical activity—are not undertaken with these outcomes in mind. In addition, when research is sought to inform policy decisions, relevant data may not exist or may be insufficient for evaluation. Alternatively, access to critical data may be constrained. The group identified the following systemic issues in addressing obesity policy research questions in particular: timing, measures, data access and use, publication and peer review challenges, and tailoring communications for policymakers and the public.
Timing
Vigilance and responsiveness are required for researchers to evaluate obesity control policy initiatives. Policy changes may be enacted more quickly than research funding can be secured to evaluate their effects. For the purposes of evaluation, baseline data must be collected before a policy is implemented, in order to study its effect. However, rapid funding to enable the collection of such baseline data may not be feasible given the timing of standard grant review and funding cycles. More flexible and rapid systems or mechanisms that respond to these needs are required. Pilot efforts to develop novel “rapid response” funding approaches for evaluating natural experiments are being undertaken by the Canadian Institutes of Health Research (D Finegood, National Research Council Canada, personal/written communication, 2007) and by RWJF through their national research programs: Healthy Eating Research (www.healthyeatingresearch.org) and Active Living Research (www.activelivingresearch.org). The evaluations resulting from these funding programs may yield important insights into the effectiveness of policies intended to alter diet or physical activity behavior, as well as into the logistics required and potential for an accelerated review of funding requests.
Measures
Valid and reliable measures are required for obesity policy research. These include measures of dependent variables, such as BMI, diet, physical activity, and other health behavior and outcome patterns, as well as independent variables, such as the presence and characteristics of obesity-related policies operating at multiple levels—school, organizational, community, state, and national. Measures must be not only reliable and valid, as well as sensitive and specific to assess change, but also feasible to collect in a diversity of settings.
Data access and use
Another challenge in obesity policy research concerns data access. Several large federal public-use data sets, such as the Medical Expenditure Panel Survey and the National Health and Nutrition Examination Survey, have been linked and are available to researchers. But data sets from private organizations such as health plans, those focused on information collected from confidential school-based assessments, or those from assessments of key environmental factors are seldom linked to other sources of data and are not commonly available to researchers. Capacity also is required to link data from multiple sources, ideally at the level of the individual, in order to understand the effect of policy or legislative changes on specific environments, diet, physical activity behaviors, and ultimately on weight or other weight-related outcomes. Grants to improve access and the appropriate use of these data sets, and guides for analysis of the data sets, are emerging.
Even with improved access to data, however, linking physical activity, diet, and weight at the individual level to public policy requires new analytic methodologies that few people are trained to conduct. For example, the use of Bayesian statistics and computational modeling may help better manage the multiple levels of variables that need to be taken into account simultaneously. Training for researchers in cross-disciplinary and cross-sectoral research as well as complex systems methods may help advance the field.
Publication
It is desirable to disseminate the results of policy research as rapidly as possible. Mechanisms such as online publication in advance of print publication and the accelerated review and publishing of manuscripts may be beneficial, and some journals have already instituted such options. However, although it is most useful to disseminate findings even more rapidly than these mechanisms allow, researchers often hesitate to do so in ways that would limit their ability to publish in scientific peer-reviewed journals.
Tailoring communications for the public and policymakers
The scientific research community is most accustomed to and comfortable with synopsizing research results in detail, with complete statements of caveats and limitations noted for peer-reviewed journals. However, effective communication vehicles for policymakers and the public must necessarily be framed and formatted differently. Policy briefs and other such communication vehicles provide clear, focused message summaries that include concise explanations of topics and clear descriptions of the potentially differing perspectives on a specific issue. Researchers need more training in translating research results to policymakers and the public in this manner. Innovations using web and emerging communication technologies have been developed and may provide useful models. Health communication research is examining how best to adapt such technologies for public health purposes. Lessons from marketing science may be helpful in improving effectiveness in communications.
Key Partners in Implementing an Obesity Policy Research Agenda
Table 1 displays an initial list of potential key partners suggested by the group to collaborate on designing, conducting, and applying obesity policy research. Because of the multisectoral nature of the issue, many partners will be needed to conduct and disseminate policy research in the varied domains. The group noted that partnerships in both “knowledge generation” and “knowledge transfer” are needed. Knowledge generation partners would help guide, fund, publish, and/or participate in research to inform actions on the issue of obesity. Knowledge transfer partners would help disseminate and apply the information once it is generated.
Table 1.
Key partners in implementing an obesity policy research agenda
| Knowledge generation | Knowledge transfer |
|---|---|
|
|
Possible Approaches for Setting Obesity Policy Research Priorities
Meeting participants proposed that the following criteria be used in setting priorities for obesity policy research:
potential impact on general and priority subpopulations (such as youth, racial and ethnic minorities, and populations of low socioeconomic status);
potential impact on health outcomes, including comorbidities and quality of life;
implementation feasibility;
preventive effect with respect to obesity development;
costs to society (including healthcare costs, reduced productivity, and other relevant economic measures), and cost effectiveness of solutions.
Participants then identified the following categories as priorities for an initial policy research agenda: capacity development, agriculture and food supply, economic research, built environment and transportation, youth settings and education policies, worksites, media and marketing, and health services and outcomes research. After this exercise, participants generated specific suggestions for research needs under each category. Participants then indicated their preferences for individual suggestions using the prioritization criteria above, using a modified nominal group process. Table 2 displays the research suggestions that the group rated most highly. For readability, these are listed by category and are not in priority order. Please note that not all of the categories listed above are represented by the research suggestions in Table 2.
Table 2.
Suggestions for priority topics in obesity policy research
| Category |
|---|
| Capacity development |
| Measures of policies and related environmental factors |
| Improved measures of policy-relevant obesity outcomes (e.g., diet, physical activity, energy balance, BMI) |
| Information about motivations of policymakers, and how issues may be framed appropriately |
| Agriculture and food supply |
| Effects of subsidies for agricultural commodities on supply and prices, and resulting effects on population-level eating patterns |
| Economic research |
| Estimated and actual cost of policies (e.g., to schools, society) including revenue consequences and relationship of cost to feasibility and acceptability and any unanticipated consequences |
| Costs (nature and level) to individuals of making behavior change recommended for obesity prevention |
| Food pricing and its influence on food consumption, and how related policies can influence obesity |
|
| Shift in focus of research from return on investment to costs associated with disease burden that may be addressed by policies |
| Built environment and transportation |
| Community design and its impact on energy-balance behaviors, including zoning policies |
| Youth settings and educational policies |
| Evaluation of the impact of school food and physical activity policies on revenues and the related costs and/or risks to schools, communities, and society |
| Evaluation of the effects of school food and physical activity environments and policies on academic achievement |
| Media/marketing |
| Effective methods of communicating diet and physical activity information to the general population to reduce obesity |
Discussion
Obesity Policy Research Topic Areas
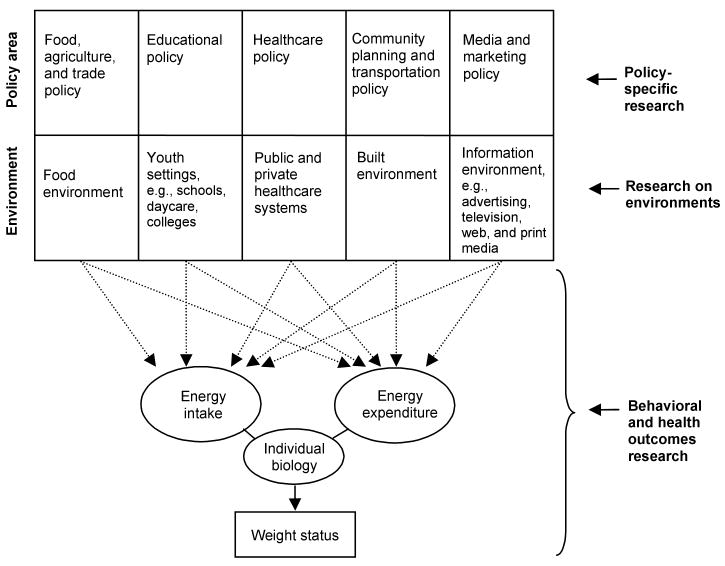
Figure 1 provides an illustration of the obesity policy research topic areas discussed in the meeting, related to both policy areas and types of environment, and the possible impacts on diet, physical activity, and weight. As with most diagrams, the need for simplicity masks the underlying complexity of the issues, and some important elements may not have been discussed at the meeting. However, a diagram offers the opportunity to develop a relational approach to increase knowledge, focus future research, and strategically address questions faced by policymakers. Clearly, additional granularity and specificity could be incorporated, but this illustration may serve as a starting point for review, revision, and enhancement.
Figure 1.
Identified obesity policy research topic areas
In the diagram, policy areas are separated by broad policy topic. Each is shown in relation to its primary corresponding environment(s). Note, however, that policy areas may relate to several environments. Research areas are listed on the right side: policy-specific research, research on environments, and behavioral and health outcomes research. Policy-specific research focuses on policies themselves as they relate to diet, physical activity, and energy-balance behavior. This research may include topics such as policy instruments (e.g., regulations, taxes, and subsidies) and their potential application to altering diet and physical activity behavior; constitutive policy (focusing on improvement of existing policies and processes); policy implications or evaluation; or other topics such as ethical and social considerations of policy. Policy-specific research may use a variety of models, such as those described by Sabatier,40 and employ a number of research methods, including field survey analysis, quasi-experiments, ethnography, case-study analysis, discourse analysis, econometrics, economic modeling, and cost-benefit analysis.41 This research is performed largely by policy scholars, political scientists, and economists.
Research on environments focuses on environmental variables that may be manipulated by policy initiatives to affect obesity levels. More broadly, this research may include topics such as access, equity, and freedom of choice. This research is performed largely by behavioral and social researchers and epidemiologists. Behavioral and health outcomes research focuses on diet and physical activity behavior, weight, and health outcomes. Policy-specific research may examine the effects of policy on environments, and vice versa. Both policy-specific research and research on environments may examine the respective impact of policy or environment on diet, physical activity, and energy-balance behavior. All of the research areas may be used to inform policymaking.
Meeting Themes
Several recurring themes emerged from the meeting discussions. The first theme relates to the embryonic nature of obesity policy research. Surprisingly, given the extent and global nature of the issue, very little is known currently about policies that may be effective in altering dietary habits and physical activity on a broad scale. Policymakers and researchers appear to be in a similar position in many ways to the one they were in during the early days of tobacco control, in which knowledge about the effectiveness of proposed or implemented policies was very limited. As noted above, improved policy surveillance and measures of dependent and independent variables would aid in assessing the current status of policy interventions and are needed to assess policy effectiveness.
A second and related theme centers on the need to take advantage of the grass-roots or so-called natural experiments that may affect obesity prevalence or trends, such as requirements for calorie labeling in restaurants. Many of these environmental changes may be impractical and/or unethical to randomize. Policymakers are now implementing legislation concerning a host of issues related to diet and physical activity, and the precise effects of these changes are not known. Traditional research designs have focused on careful translation of evidence to action; however, as noted by Dr. Lawrence Green: “to get more evidence-based practice, we need more practice-based evidence.”42 Recent reports and research groups have also emphasized the need for studies with a focus on effectiveness rather than efficacy (impact of the intervention), and strong external as well as internal validity.43,44 Evaluations of natural experiments, which may require rapid funding mechanisms, would broaden our knowledge base and inform the policymaking process.
The third theme relates to the need for research that reaches beyond individual-level behavior change. Policy research relating to structural changes in systems, communities, worksites, and other population-level and environmental foci is urgently needed, as these large systems play a critical role through influencing, shaping, and facilitating individual-level behavior change.
The fourth theme emerging from the discussions, which is evident in Table 2, is the strong need for increased economic research across many policy areas that relate to obesity. Research is needed that focuses on micro-level economic questions, such as economic incentives and disincentives to alter diet and physical activity behavior, or the cost effectiveness and cost– benefit analysis of specific policies. These cost–benefit analyses may be expanded to include benefits not typically seen in these estimates, using hedonic valuation methods. For example, in the case of developing a park, benefits might include aesthetic appeal or proximity to community residents. Research on macro-level economic questions is also needed, such as the effect of agricultural and trade policies on food supply and the subsequent determinants of obesity.
The final theme from the meeting is the urgency with which the issue of obesity ought to be addressed. The consequences of widespread obesity are being experienced and will have devastating future effects on public health and healthcare systems, with the potential for even broader economic ramifications. Evidence from other public health initiatives suggests that environmental and policy changes will be essential aspects of the overall effort to reduce obesity prevalence.45,46
Conclusion
This paper is a call to action for the research community. The health and economic impacts of rising obesity levels are already evident, and in the absence of corrective action at many levels and by many actors, the impact on public health and healthcare systems is expected to grow considerably over time—with far-reaching societal consequences. Given the experiences in tobacco control and other public health initiatives, and the environmental associations with rising obesity rates that are potentially addressable by policymakers, public policy may be a powerful tool to effect structural change in order to alter population-level diet and physical activity behavior. Such systemic change may modify social norms and create optimal defaults where the default option is the healthy choice, thus facilitating and reinforcing individual behavior change. A critical next step in moving the research agenda forward will be to begin the work of building the evidence base for obesity policy, by evaluating the effects of new and existing policies. The research community now has the opportunity to work and act collectively in order to inform policymaking and resource allocation to address one of the most important public health challenges of the twenty-first century.
Acknowledgments
Special gratitude is extended by NCI for the meeting participants' valuable contributions, and for the meeting facilitation of Dr. Marianne Alciati. In addition, the authors gratefully acknowledge the editorial assistance of Anne Brown Rodgers in preparation of the manuscript, and the helpful comments by Dr. William Ascher and Dr. Terry T-K Huang on the manuscript overall, and on new methods of analysis, respectively.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.U.S. DHHS. With understanding and improving health and objectives for improving health. 2nd. Vol. 2. U.S. Government Printing Office; 2000. Healthy People 2010. [Google Scholar]
- 2.Kumanyika SK, Jeffery RW, Morabia A, Ritenbaugh C, Antipatis VJ. Obesity prevention: the case for action. Int J Obes. 2002;26:425–36. doi: 10.1038/sj.ijo.0801938. [DOI] [PubMed] [Google Scholar]
- 3.Must A, Spadano J, Coakley E, Field A, Colditz C, Dietz W. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523–9. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 4.Pi-Sunyer F. The obesity epidemic: pathosphysiology and consequences of obesity. Obes Res. 2002;10(2):97S–104S. doi: 10.1038/oby.2002.202. S. [DOI] [PubMed] [Google Scholar]
- 5.Finkelstein EA, Fiebelkorn IC, Wang G. National medical spending attributable to overweight and obesity: how much and who's paying? Health Aff. 2003;W3:219–26. doi: 10.1377/hlthaff.w3.219. [DOI] [PubMed] [Google Scholar]
- 6.Catlin A, Cowan C, Hartman M, Heffler S. National healthcare spending in 2006. Health Aff. 2008;27(1):14–29. doi: 10.1377/hlthaff.27.1.14. [DOI] [PubMed] [Google Scholar]
- 7.Keehan S, Sisko A, Truffer C, et al. Health spending projections through 2017: the baby-boom generation is coming to medicare. Health Aff. 2008;27(2):w145–w155. doi: 10.1377/hlthaff.27.2.w145. [DOI] [PubMed] [Google Scholar]
- 8.Thorpe KE, Florence CS, Howard DH, Joski P. The impact on obesity of rising medical spending. Health Aff. 2004 October 20; doi: 10.1377/hlthaff.W4.480. Web Exclusive. [DOI] [PubMed] [Google Scholar]
- 9.Finkelstein EA, Fiebelkorn IC, Wang G. The costs of obesity among full-time employees. Am J Health Promot. 2005;20(1):45–51. doi: 10.4278/0890-1171-20.1.45. [DOI] [PubMed] [Google Scholar]
- 10.CDC. Trends in intake of energy and macronutrients—United States, 1971–2000. Morb Mortal Wkly Rep. 2004;53(4):80–2. [PubMed] [Google Scholar]
- 11.USDA. Agriculture fact book 2001–2002. Washington DC: U.S. Government Printing Office; 2003. [Google Scholar]
- 12.Hiza HAB, Bente L. Nutrient content of the U.S. food supply, 1909–2004: a summary report. USDA, Center for Nutrition Policy and Promotion; 2007. [Google Scholar]
- 13.U.S. DHHS. Physical activity and health: a report of the Surgeon General. US DHHS, CDC National Center for Chronic Disease and Health Promotion; 1996. [Google Scholar]
- 14.CDC. Physical activity trends—United States, 1990–1998. Morb Mortal Wkly Rep. 2001;50(9):166–9. [PubMed] [Google Scholar]
- 15.IOM. Does the built environment influence physical activity: examining the evidence. Washington DC: National Academies Press; 2005. [Google Scholar]
- 16.Brownson RC, Boehmer TK, Luke DA. Declining rates of physical activity in the United States: what are the contributors? Annu Rev Public Health. 2005;26:421–43. doi: 10.1146/annurev.publhealth.26.021304.144437. [DOI] [PubMed] [Google Scholar]
- 17.Young LR, Nestle M. The contribution of expanding portion sizes to the U.S. obesity epidemic. Am J Public Health. 2002;92(2):246–9. doi: 10.2105/ajph.92.2.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nielsen SJ, Popkin BM. Patterns and trends in food portion sizes, 1977–1996. JAMA. 2003;289(4):450–3. doi: 10.1001/jama.289.4.450. [DOI] [PubMed] [Google Scholar]
- 19.Burgeson CR, Weschler H, Brener ND, Young J, Spain CG. Physical education and activity: results from the School Health Policies and Programs Study 2000. J Sch Health. 2001;71(7):279–93. doi: 10.1111/j.1746-1561.2001.tb03505.x. [DOI] [PubMed] [Google Scholar]
- 20.McGinnis JM, Gootman JA, Kraak VI, editors. Food marketing to children and youth: threat or opportunity? Washington DC: The National Academies Press; 2005. [Google Scholar]
- 21.Kubik M, Lytle L, Hannan P, Perry C, Story M. The association of the school food environment with dietary behaviors of young adolescents. Am J Public Health. 2003;93(7):1168–73. doi: 10.2105/ajph.93.7.1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Frank LD. Land use and transportation interaction: implications on public health and quality of life. Journal of Planning Education and Research. 2000;20(1):6–22. [Google Scholar]
- 23.Koplan JP, Liverman CT, Kraak VI, editors. Preventing childhood obesity: health in the balance. Washington DC: The National Academies Press; 2005. [PubMed] [Google Scholar]
- 24.Block JP, Scribner RA, DeSalvo KB. Fast food, race/ethnicity, and income: a geographic analysis. Am J Prev Med. 2004;27(3):211–7. doi: 10.1016/j.amepre.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 25.Lewis LB, Sloane DC, Nascimento LM, et al. African Americans' access to healthy food options in South Los Angeles restaurants. Am J Public Health. 2005;95(4):668–73. doi: 10.2105/AJPH.2004.050260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson ML. Fruit and vegetable access differs by community racial composition and socioeconomic position in Detroit Michigan. Ethn Dis. 2006;16(1):275–80. [PubMed] [Google Scholar]
- 27.Morland K, Diez Roux AV, Wing S. Supermarkets, other food stores, and obesity: the Atheriosclerosis Risk in Communities Study. Am J Prev Med. 2006;30(4):333–9. doi: 10.1016/j.amepre.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 28.Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ. Food store availability and neighborhood characteristics in the United States. Prev Med. 2007;44:189–95. doi: 10.1016/j.ypmed.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 29.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79(1):6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- 30.Lakdawalla D, Philipson T. The growth of obesity and technological change: a theoretical and empirical examination. National Bureau of Economic Research; 2002. [Google Scholar]
- 31.Cutler DM, Glaeser EL, Shapiro JM. Why have Americans become more obese? J Econ Perspect. 2003;17(3):93–118. [Google Scholar]
- 32.French SA, Story M, Jeffery RW. Environmental influences on eating and physical activity. Annu Rev Public Health. 2001;22:309–35. doi: 10.1146/annurev.publhealth.22.1.309. [DOI] [PubMed] [Google Scholar]
- 33.Lake A, Townshend T. Obesogenic environments: exploring the built and food environments. J R Soc Health. 2006;126(6):262–7. doi: 10.1177/1466424006070487. [DOI] [PubMed] [Google Scholar]
- 34.Mello MM, Studdert DM, Brennan TA. Obesity—the new frontier of public health law. N Engl J Med. 2006;354(24):2601–10. doi: 10.1056/NEJMhpr060227. [DOI] [PubMed] [Google Scholar]
- 35.Hopkins DP, Briss PA, Ricard CJ, et al. Reviews of evidence regarding interventions to reduce tobacco use and exposure to environmental tobacco smoke. Am J Prev Med. 2001;20(2S):16–66. doi: 10.1016/s0749-3797(00)00297-x. [DOI] [PubMed] [Google Scholar]
- 36.CDC. Strategies for reducing exposure to environmental tobacco smoke, increasing tobacco-use cessation, and reducing initiation in communities and health-care systems. Morb Mortal Wkly Rep. 2000;49(NoRR12) [PubMed] [Google Scholar]
- 37.Lake A, Townshend T. Obesogenic environments: exploring the built and food environments. J R Soc Health. 2006;126(6):262–7. doi: 10.1177/1466424006070487. [DOI] [PubMed] [Google Scholar]
- 38.Homer C, Simpson LA. Childhood obesity: what's health care policy got to do with it? Health Aff. 2007;26(2):441–4. doi: 10.1377/hlthaff.26.2.441. [DOI] [PubMed] [Google Scholar]
- 39.Delbecq A, Van de Ven AH, Gustafson DH. Group techniques for program planning. Glenview Il: Scott, Foresman and Company; 1975. [Google Scholar]
- 40.Sabatier PA. Toward better theories of the policy process. PS. 1991;24(2):147–56. [Google Scholar]
- 41.Dunn WN. Public policy analysis. 3rd. Prentice Hall; 2003. [Google Scholar]
- 42.Green LW. If we want more evidence-based practice, we need more practice-based evidence. Bethesda MD: National Institutes of Health; 2008. http://videocast.nih.gov. [Google Scholar]
- 43.Klesges LM, Dzewaltowski DA, Glasgow RE. Review of external validity reporting in childhood obesity prevention research. Am J Prev Med. 2008;34(3):216–23. doi: 10.1016/j.amepre.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 44.Patrick K, Scutchfield D, Woolf SH. External validity reporting in prevention research. Am J Prev Med. 2008;34(3):260–2. doi: 10.1016/j.amepre.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 45.Economos CD, Brownson RC, DeAngelis MA, et al. What lessons have been learned from other attempts to guide social change? Nutr Rev. 2001;59(3):S40–56. doi: 10.1111/j.1753-4887.2001.tb06985.x. [DOI] [PubMed] [Google Scholar]
- 46.Eriksen M. Lessons learned from public health efforts and their relevance to preventing childhood obesity. In: Koplan JP, Liverman CT, Kraak VI, editors. Preventing childhood obesity: health in the balance. Washington DC: Institute of Medicine; 2006. [Google Scholar]