Abstract
The broadly neutralizing anti-HIV antibody 4E10 recognizes an epitope very close to the virus membrane on the glycoprotein gp41. It was previously shown that epitope recognition improves in a membrane context and that 4E10 binds directly, albeit weakly, to lipids. Furthermore, a crystal structure of Fab 4E10 complexed to an epitope peptide revealed that the centrally placed, protruding H3 loop of the antibody heavy chain does not form peptide contacts. To investigate the hypothesis that the H3 loop apex might interact with the viral membrane, two Trp residues in this region were substituted separately or in combination with either Ala or Asp by site-directed mutagenesis. The resultant IgG variants exhibited similar affinities for an epitope peptide as WT 4E10 but lower apparent affinities for both viral membrane mimetic liposomes and Env(−) virus. Variants also exhibited lower apparent affinities for Env(+) virions and failed to significantly neutralize a number of 4E10-sensitive viruses. For the extremely sensitive HXB2 virus, variants did neutralize, but at 37- to >250-fold lower titers than WT 4E10, with Asp substitutions exerting a greater effect on neutralization potency than Ala substitutions. Because reductions in lipid binding reflect trends in neutralization potency, we conclude that Trp residues in the antibody H3 loop enable membrane proximal epitope recognition through favorable lipid interactions. The requirement for lipophilic residues such as Trp adjacent to the antigen binding site may explain difficulties in eliciting 4E10-like neutralizing antibody responses by immunization and helps define a unique motif for antibody recognition of membrane proximal antigens.
Keywords: 4E10, gp41, HIV, neutralizing antibody, tryptophan
The notorious ability of HIV to rapidly mutate with successive replication cycles enables it to evade adaptive immune responses. Therefore, many T cell- and antibody-based vaccine development efforts are currently directed at targeting highly conserved epitopes that may prove more refractory to mutation. With regard to antibody-based vaccines, the rationale for targeting conserved epitopes is further supported by simian/human immunodeficiency virus challenge studies in rhesus macaques, in which the passive transfer of broadly neutralizing mAb (bnAb) achieved sterilizing immunity (i.e., protection against infection) (1). The bnAbs 2G12, 2F5, 4E10, b12, PG9, and PG16 all derive from HIV-1 infected individuals, bind to defined regions on the envelope glycoprotein, and were initially recognized for their exceptional ability to neutralize a number of genetically diverse primary HIV-1 isolates in vitro (2, 3). Recent comparative studies of bnAbs with extensive panels of diverse primary isolates show that 2F5 and 4E10, in particular, are very broadly neutralizing (3 –5).
2F5, 4E10, and Z13e1 [an affinity-enhanced variant of mAb Z13 that exhibits broad neutralization at very modest potencies (6, 7)] recognize contiguous epitopes within the membrane proximal external region (MPER) of the envelope transmembrane glycoprotein gp41 (6, 8) (Fig. 1). These core epitopes were determined by peptide mapping; however, alanine-scanning mutagenesis of the MPER in intact viruses established that only a few residues (D664/K665/W666, W672/F673/W680, and N671/D674 HXB2 numbering throughout) are essential for 2F5, 4E10, and Z13e1 neutralization, respectively (7, 9). Crystal structures of Fab 2F5, 4E10, and Z13e1 complexed with their respective epitope peptides subsequently confirmed that residues DKW, WFW, and ND are buried in the paratopes of these antibodies (10 –14).
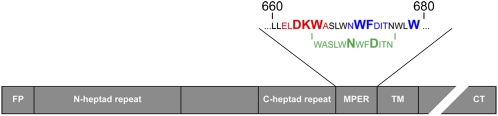
Fig. 1.
Schematic of the transmembrane glycoprotein gp41. The MPER comprises the continuous epitopes of three broadly neutralizing monoclonal antibodies: 2F5 (ELDKWA), 4E10 (NWFDIT), and Z13e1 (WASLWNWFDITN). The enlarged residues indicate essential determinants of neutralization as described in the text. FP, fusion peptide; TM, transmembrane domain; CT, cytoplasmic tail.
A tryptophan-rich MPER is highly conserved across HIV-1, HIV-2, simian immunodeficiency virus, feline immunodeficiency virus, and other membrane-fusing viruses (15). Salzwedel et al. (16) demonstrated that the MPER is essential for HIV-1 fusion, because deletion of this region (residues 666–682) abrogates both HIV-1 infectivity and cell–cell fusion (fusion between Env-expressing cells and target cells). These authors were also the first to recognize the high level of conservation of tryptophans in this region of gp41 and the transmembrane proteins of other enveloped viruses and suggested their potential for interacting with the viral membrane. Indeed, the membrane-anchoring properties of tryptophans and tyrosines are well recognized (17).
Shortly thereafter, Suarez et al. (18) reported on the ability of MPER peptides to associate with, permeabilize, and induce fusion between membranes. Since then, a number of membrane-associated MPER peptide structures have been resolved using NMR spectroscopy methods (19 –21). Given the caveat that unbound MPER NMR structures are contextually dissociated from the macromolecular structure of native, trimeric, envelope spikes, and until a high-resolution structure of Env on intact viruses is attained, in situ MPER membrane association remains an open question. However, in addition to observations that the MPER is tryptophan-rich and that MPER peptides associate with membranes, the findings by Grundner et al. (22) and Ofek et al. (12) that 2F5 and 4E10 binding to Env proteoliposomes is enhanced by the presence of lipids also suggest that the MPER is membrane associated. The question thus remains whether the membrane environment optimally configures the MPER for bnAb recognition or whether the MPER bnAbs have intrinsic lipid affinity.
Since the initial findings by Grunder et al. and Ofek et al. (12, 22), a number of publications have also shown that 2F5, 4E10, and Z13e1 improve binding to Env and epitope peptides in a lipid environment (21, 23, 24). In addition, it has become increasingly clear that 4E10 binds to lipids in the absence of the MPER (21, 23 –29). These studies have generated models of 4E10 epitope recognition (21, 23), but they have not yet fully addressed which antibody region(s) bind lipid and, of particular importance for vaccine design, whether lipid interaction is an essential component of MPER-mediated neutralization.
Therefore, we initiated a site-directed mutagenesis study to gain insight into which region(s) of 4E10 mediates lipid reactivity and whether abrogation of this reactivity impacts neutralization, given the strong evidence for 4E10–lipid interactions. We opted to first mutate residues at the apex of the CDRH3 because previously described crystal structures of Fab 4E10 complexed to an epitope peptide revealed that this region does not form part of the antigen binding site as is often the case for a CDRH3 (14, 30). A similar study was not implemented for 2F5, because the case for 2F5–lipid interactions is less clear, its very occurrence a topic of current debate (21, 27, 31). Moreover, substitutions of hydrophobic residues at the apex of the 2F5 CDRH3 have been shown to affect antigen binding (32), which may relate to the proposed ability of 2F5 to form contacts with another region of Env on intact trimers (i.e., a region near the fusion peptide of gp41) (11, 33).
We began by introducing nonconservative mutations at residues in the apex of the CDRH3 loop that display favorable free energies of transfer from water to a bilayer interface (34). Explicitly, we substituted the most lipophilic residue in this region, tryptophan, with either alanine or aspartic acid (Table S1). The results show that these Trp residues (W100 and W100B) are essential for MPER recognition, because both double Ala and Asp substitution variants (WAWA and WDWD) exhibit undetectable neutralization activity. Moreover, it seems that lipid reactivity and neutralization activity are linked, because the neutralization potencies of the variants decrease with decreasing lipid reactivity. Explicitly, lipid reactivity decreases from WT 4E10 to Ala variants and then to Asp variants, as predicted on the basis of side chain propensities for bilayer interaction.
Results
Generation of IgG1 4E10 and Lipophilicity-Altered Variants.
As described in Materials and Methods, single-chain variable fragment (scFv) 4E10 DNA was synthesized de novo and subcloned into the phage display vector pComb3× (35). Fab 4E10 was subsequently cloned into phage display vector pComb3H (35) by overlap extension PCR using the heavy and light chain variable regions of scFv 4E10 and heavy and light chain constant regions of Fab b12 (CH1, Cκ). Site-directed mutagenesis was conducted on Fab 4E10 in pComb3H, because this vector is a more manageable size for molecular biology manipulation than pDR12 (≈6 kb vs. ≈13 kb). Fab variable regions were then cloned into pDR12, a mammalian expression vector that encodes IgG1 light chain and heavy chain from separate ORFs (36, 37). The resultant variants were transfected and expressed in 293F Freestyle cells (see Materials and Methods). Purification from tissue culture supernatants using Protein A Sepharose yielded highly pure IgG1 of the correct molecular weight (Fig. S1).
Evaluation of Epitope Peptide Binding Affinity.
Because of the caveats associated with measuring antibody affinity by direct (antigen-immobilized) ELISA (e.g., antigen can become denatured, dissociate, or occur in high local concentrations that enhance antibody avidity effects), we used an ELISA that establishes in-solution equilibrium between an antibody and epitope peptide before “capturing” the biotinylated peptide with immobilized neutravidin. Because the capture step introduces a phase change, this modified ELISA does not measure in-solution equilibrium binding constants, but improves upon a direct ELISA for the purpose of comparing apparent binding affinities among IgG1 4E10 variants. Fig. 2 shows that the affinities of the variants for an epitope peptide are as strong as, or stronger than, 4E10 within the SEM. Therefore, the lipophilic amino acid substitutions in CDRH3 have not perturbed epitope peptide binding.
Fig. 2.
Nonconservative substitutions in the CDRH3 loop of 4E10 do not significantly alter epitope peptide affinity. (A) Binding of IgG1 4E10 and variants to a biotinylated epitope peptide (bio-29) in a neutravidin capture assay. Antibody–bio-29 association was allowed to reach equilibrium before transferring to a neutravidin-coated 96-well plate for a short incubation period. Neutravidin-captured antibody–bio-29 complexes were quantified using an alkaline-phosphatase conjugated, anti-human, Fc-fragment specific antibody. IgG1 4E10 P, commercially available from Polymun Scientific, was included as a positive control. (B) Half-maximal effective concentration (log EC50) and corresponding SEM for each antibody against bio-29. Values were derived by nonlinear regression analyses from the bio-29 binding curves (GraphPad Prism 5.0 for Windows).
Surface Plasmon Resonance Experiments with Immobilized Liposomes to Assess Lipid Binding.
Surface plasmon resonance (SPR) spectroscopy records binding events in real time, generating response curves. In cases of monovalent binding interactions that follow first-order binding kinetics, the thermodynamic equilibrium dissociation constant (K d) is equal to the quotient of dissociation (koff) and association (kon) kinetic rate constants, where koff and kon may be derived from the association and dissociation phases of the SPR response curves by nonlinear regression analysis. Unfortunately, first-order binding kinetics does not accurately describe our system (bivalent analyte binding to a saturated epitope surface), nor could we determine K d from equilibrium plateau signals and the corresponding free analyte concentrations (e.g., Scatchard analysis), because saturation as a function of analyte (antibody) concentration was not achieved in the concentration range studied. What we present instead are the maximum responses obtained when each IgG1 is incubated in the presence of viral membrane mimetic liposomes (Fig. 3). These values provide an estimation of relative binding affinities, from which we are able to draw qualitative conclusions.
Fig. 3.
Summary of Ab responses on viral membrane mimetic liposome surfaces. The maximum SPR response of each Ab on VM liposomes was averaged (n = 2) and plotted with standard deviation. IgG1 b12 was included as a negative isotype control.
The liposome SPR assay used here was originally developed to evaluate IgG1 2F5 and 4E10 binding to lamellar cardiolipin (CL) (27), and thus measures antibody binding to both immobilized liposomes containing CL (“CL-containing” liposomes) and liposomes without CL (“control” liposomes). Variant binding to control and CL-containing liposomes was evaluated for comparison with our previous characterizations of 4E10 and 2F5, and the resulting response curves are shown in Fig. S2 and Fig. S3. However, because CL is not found in HIV-1 virions, we also evaluated binding to viral membrane mimetic (VM) liposomes whose molar ratios of phospholipids resemble the distributions of major lipid components in HIV-1 virions (Fig. 3 and Fig. S4) (38 –41). CL, or diphosphatidylglycerol, is a “double” phospholipid with two negatively charged headgroups and four acyl chains that exhibits a single negative charge at neutral pH. In humans, CL distribution is limited to those membranes and tissues where CL synthetases are found (i.e., mitochondrial membranes and mitochondria-rich tissue) (42). The reason for including CL in our previous analysis of 2F5 and 4E10 lipid reactivity relates to the suggestion that 2F5 and 4E10 are autoantibodies specific for CL (25), a hypothesis that will be elaborated on further in Discussion.
Although all variants exhibited diminished SPR responses on liposome surfaces with respect to WT 4E10 (Figs. S2–S4), reductions were most notable on CL-containing liposomes and VM liposomes. For VM liposomes, if the average (n = 2) maximum response of each variant is normalized to the average maximum response obtained for 4E10 at a given concentration (e.g., 2.5 μM, 625 nM, 156 nM, and 39 nM), we find that SPR responses of variants are 4- to 19-fold lower than WT 4E10 [W(100)A, 4-fold; W(100B)A, 6-fold; WAWA, 7-fold; W(100)D, 10-fold; W(100B)D, 11-fold; WDWD, 19-fold; Fig. 3]. Moreover, the Asp variants all exhibit similar responses on VM liposomes as a negative isotype control mAb (IgG1 b12). Because the refractive index change that accompanies an injection of IgG1 b12 sets the baseline response for a given mAb concentration, this suggests that only Ala variant responses are above background.
Likewise, when variants were evaluated for their ability to bind Env(−) viral membranes using two different in vitro capture methods, all exhibited diminished abilities to capture Env(−) virus compared with WT 4E10 (Fig. S5). Only variants W(100)A and W(100B)A showed some degree of virus capture above baseline (the amount of virus captured by a negative isotype control IgG1 DEN3) (Fig. S5B).
Neutralization Assays.
To assess whether the nonconservative substitutions in CDRH3 affect binding to functional Env, variants were evaluated for neutralization activity against a panel of pseudoviruses in a single-cycle infectivity assay at Monogram Biosciences (Table 1). Surprisingly, we found that the variants were only able to neutralize HXB2, which is an order of magnitude more sensitive to WT 4E10 neutralization than other pseudoviruses examined here. Indeed, the majority of these viruses were selected on the basis of their sensitivity to 4E10 in a peripheral blood mononuclear cell assay (92HT594 and 93MW960) or single-cycle infectivity assay (92HT594, 93MW960, JRCSF, and SF162), or because they are T cell line-adapted (TCLA) viruses (HXB2 and NL43) (4). Therefore, it is readily apparent that nonconservative substitutions to tryptophan in the CDRH3 have strong negative consequences for 4E10 neutralization. It is also apparent that the most radical substitutions exert a greater effect on neutralization potency. Explicitly, single Ala variants W(100)A and W(100B)A neutralize HXB2 with greater potencies (IC50, 9.1 μg/mL and 7.5 μg/mL) than single Asp variants W(100)D and W(100B)D (18 μg/mL and 39 μg/mL, respectively); the neutralization activities of the double substitution variants, WAWA and WDWD, are below assay cutoff values (i.e., >50 μg/mL).
Table 1.
Nonconservative substitutions of tryptophan in the CDRH3 loop of IgG1 4E10 lead to large reductions in neutralization activity
| Antibody | IC50 (μg/mL) | |||||||
| HXB2 | JRFL | SF162 | 92HT594 | 93MW960 | JRCSF | NL43 | aMLV | |
| IgG1 4E10 | 0.20 | 10.45 | 7.70 | 2.07 | 2.50 | 6.47 | 5.06 | >50 |
| IgG1 4E10 P | 0.16 | 18.64 | 19.49 | 3.24 | 4.19 | 9.32 | 10.65 | >50 |
| W(100)A | 9.06 | >50 | >50 | >50 | >50 | >50 | >50 | >50 |
| W(100B)A | 7.52 | >50 | >50 | >50 | >50 | >50 | >50 | >50 |
| WAWA | >50 | >50 | >50 | >50 | >50 | >50 | >50 | >50 |
| W(100)D | 18.17 | >50 | >50 | >50 | >50 | >50 | >50 | >50 |
| W(100B)D | 39.11 | >50 | >50 | >50 | >50 | >50 | >50 | >50 |
| WDWD | >50 | >50 | >50 | >50 | >50 | >50 | >50 | >50 |
IgG1 4E10 and variants were evaluated for neutralization activity against pseudoviruses incorporating Env from two neutralization-sensitive TCLA viruses (HXB2 and NL43) and five primary isolate viruses (JRFL, SF162, 92HT594, 93MW960, and JRCSF) as described previously (4). Virions pseudotyped with Env from an amphotropic murine leukemia virus (aMLV) served as a control for nonspecific neutralization (50).
To understand whether CDRH3 substitutions affect epitope affinity in a membrane context, we also measured apparent antibody affinities for intact JR-FL virus using an in-solution competition assay (Fig. S6A). We found that the apparent affinity of WT 4E10 for JR-FL virus particles (IC50 7.4–7.8 μg/mL) is stronger than Ala variant affinities [W(100)A, 13.3 μg/mL; W(100B)A, 26.5 μg/mL; WAWA, 91.3 μg/mL], which are stronger than Asp variant affinities (all >200 μg/mL) (Fig. S6B). It should also be noted that the apparent affinity of WAWA for JR-FL virus particles is below the highest concentration of antibody used in the neutralization assay.
Discussion
In this study we generated variants of IgG1 4E10 with nonconservative substitutions of tryptophan in the CDRH3 that exhibit similar apparent affinities for an epitope peptide compared with WT 4E10 (within SEM) but markedly diminished neutralization activities. Because the neutralization activities of these variants positively correlate with their binding to viral membrane surfaces and epitope affinities in a membrane context (JR-FL virus particles), we suggest that Trp residues at the apex of the CDRH3 loop play a crucial role in 4E10 neutralization by enabling 4E10–lipid interactions. Quantitative discrepancies between virus binding affinities and neutralization potencies (Table 1 and Fig. S6B) may reflect uncleaved gp160 monomers or other nonnative forms of Env on the surface of HIV-1 that present the cognate epitope of 4E10 but do not enable virus entry. In this case, antibody affinity for a virus particle could exceed its neutralization potency, which measures binding to functional Env.
Ala and Asp substitutions introduce residues with positive free energies of transfer from water to the bilayer interface (34). Therefore, it is likely that these interactions (Ala–lipid, Asp–lipid) are unfavorable and disrupt in situ epitope recognition. This may also explain why single Asp substitutions [W(100)D and W(100B)D] have a more deleterious effect on neutralization than single Ala substitutions [W(100)A and W(100B)A] and why double substitutions (WAWA and WDWD) seem to act cooperatively.
This unique mechanism of 4E10 epitope recognition (i.e., lipophilic residues at the periphery of the antigen binding site) may explain difficulties in eliciting neutralizing antibody responses to immunogens based on the 4E10 epitope. It has been previously proposed that these difficulties related to the suggested reactivity of 2F5 and 4E10 with cardiolipin, an endogenous phospholipid (25, 43). Explicitly, the hypothesis is that the MPER antigenically mimics cardiolipin, an autoantigen; therefore, MPER immunogens fail to induce neutralizing anti-MPER antibodies because B cells with autoreactive antibody specificities are negatively regulated by tolerance mechanisms. However, we and others have found that 2F5 does not bind to CL in diagnostic assays of antiphospholipid syndrome or to liposome surfaces (21, 25, 28), which suggests that difficulties in eliciting neutralizing antibodies against MPER immunogens is not generally related to CL reactivity. Furthermore, it has been shown that antibody responses can be elicited to MPER immunogens, only that these antibodies are not potently neutralizing (44), suggesting again that tolerance is not the issue, but some qualitative difference between neutralizing and “nonneutralizing” MPER antibodies. For example, Song et al. (20) showed that a nonneutralizing MPER mAb elicited against a soluble MPER immunogen cannot recognize the MPER in a membrane context and therefore fails to neutralize the MPER.
MAb 4E10 may provide clues as to a general solution for antibody recognition of membrane proximal antigens. For example, a recent crystal structure of the Fab fragment of ofatumumab, a therapeutic human mAb directed against CD20, reveals that the antibody combining site is delimited by a number of hydrophobic residues (Ile, Trp, and Tyr) (45). The authors propose that its lipophilic binding site may enable ofatumumab to recognize a membrane proximal CD20 epitope, leading to increased antibody-dependent complement deposition on target cell membranes compared with another anti-CD20 therapeutic mAb, rituximab, which recognizes a seemingly more solvent-exposed CD20 epitope. To our knowledge, no published study has examined ofatumumab for direct lipid interactions; however, its structure suggests that the coupling of lipophilic binding sites to membrane proximal epitope recognition may impart additional therapeutic benefits.
Materials and Methods
Recombinant IgG1 b12 (37) was expressed and purified as previously described (46). IgG1 4E10 (47, 48) and IgG1 2F5 (8) were produced at Polymun Scientific and provided by the International AIDS Vaccine Initiative Neutralizing Antibody Consortium. Peptide bio-29 [SLWNWFDITNWLWK-(biotin)-NH2] was provided by P. Dawson as previously described (7). The following antibodies were purchased commercially: alkaline phosphatase conjugated goat anti-human IgG Fc fragment specific from Pierce.
scFv Cloning.
The variable domains of 4E10 heavy and light chains (VH and VL) were synthesized de novo as an scFv with flanking asymmetrical SfiI restriction sites by Blue Heron Biotechnology. The scFv 4E10 cassette was PCR amplified with an M13 primer set and subcloned into the phage display vector pComb3X (35) at complementary SfiI restriction sites. In addition, framework residues Q(VL11)L, E(VH6)Q, Q(VH43)R, S(VH70)T, N(VH73)R, N(VH76)S, Q(VH81)E, and K(VH83)R (Kabat numbering) were altered by site-directed mutagenesis (QuikChange site-directed mutagenesis kit; Stratagene) to yield the correct 4E10 amino acid sequence (47).
Fab Cloning.
4E10 variable domains and human IgG1 constant domains (Cκ and CH1) were amplified from scFv 4E10 and Fab b12 and annealed together by overlap extension PCR (49) using primer sets described in SI Materials and Methods. The resulting hybridization product encoding Fab 4E10 with flanking asymmetrical SfiI restriction sites was subcloned into the phage display vector pComb3H (35). In addition, light chain framework residue T109, which is not present in scFv 4E10, was inserted into Fab 4E10 by site-directed mutagenesis (QuikChange site-directed mutagenesis kit; Stratagene).
Fab Mutagenesis.
Before IgG1 4E10 cloning, the following mutations were introduced into the CDRH3 of 4E10 (QuikChange II site-directed mutagenesis kit; Stratagene): W(100)A, W(100B)A, W(100)A/W(100B)A (WAWA), W(100)D, W(100B)D, and W(100)D/W(100B)D (WDWD).
IgG Cloning.
The light and heavy chains of 4E10 and adjoining sequences in pDR12 were PCR amplified and annealed by overlap extension PCR using primer sets described in SI Materials and Methods. The resulting light chain and heavy chain cassettes were subcloned into HindIII/EcoRI (light chain) and Xba/SacI (heavy chain) restriction sites in vector pDR12 (37). It contains a full light-chain and heavy-chain expression cassette in which transcription is driven from a human cytomegalovirus promoter. The heavy-chain expression cassette contains the genomic human IgG1 gene. Selection and amplification of the plasmid was done on the basis of expression of the gene for glutamine synthetase (36).
IgG1 Expression and Purification.
IgG1 4E10, W(100)A, W(100B)A, WAWA, W(100)D, W(100B)D, and WDWD in pDR12 were transfected in FreeStyle 293-F cells (Invitrogen) according to the manufacturer’s instructions. Explicitly, for each IgG1 clone, 50 μg antibody in pDR12 and 5 μg pAdVAntage vector (Promega) were diluted in 1 mL (final volume) Opti-MEM I reduced-serum medium (Invitrogen). Simultaneously, 110 μL transfection reagent (293fectin; Invitrogen) were diluted in 1 mL Opti-MEM (final volume). The DNA/Opti-MEM solution was added to the 293fectin/Opti-MEM, incubated for 30 min at room temperature, and added to 1 × 106 cells/mL 293F cells in 48 mL FreeStyle 293 expression medium (Invitrogen). Supernatants were harvested 72 h and 144 h after transfection. Antibodies were purified using rProtein A Sepharose Fast Flow (GE Healthcare) and then dialyzed against PBS. Purity was verified by SDS-PAGE and Coomassie blue staining.
ELISA.
A neutravidin capture assay was adopted from Nelson et al. (7). Explicitly, 100 ng neutravidin (Pierce) were coated per well in 50 μL PBS at room temperature for 3 h. Plates were washed three times with PBS–0.05% Tween-20 before blocking with 130 μL 4% nonfat dry milk (NFDM)–PBS–0.02% Tween-20 for 2 h at 37°C. At the same time, a preassayed amount of bio-29 (67.6 ng per well in 30 μL 0.8% NFDM–PBS–0.02% Tween-20) was incubated at room temperature with 3-fold dilutions of antibody in 30 μL PBS (starting concentration, 1 μM). [n.b., the 67.6 ng per well bio-29 value was determined by varying the concentration of biotinylated peptide in the presence of saturating amounts of IgG1 4E10 (1 μM) and determining the concentration at which the absorbance signal was below 1.0 and within the linear range.] Plates were washed three times, and then all 60 μL of the preincubation solution were added to a neutravidin-coated plate and incubated for 15 min at room temperature. Plates were then washed four times before adding 50 μL of anti-human Fc diluted 1:1,000 in 0.4% NFDM–PBS–0.02% Tween-20 and incubating at room temperature for 1 h. Plates were washed four times before developing with 100 μL of p-nitrophenyl phosphate (Sigma-Aldrich) at room temperature. Absorbance was recorded at 405 nm.
SPR Spectroscopy.
SPR measurements were conducted at 25°C in PBS buffer using L1 sensor chips and a Biacore 2000 system (GE Healthcare).
Liposomes were prepared from commercially available bovine heart CL, 1,2-dioleoyl-sn-glycero-3-phosphoethanolamine (DOPE), egg L-α-phosphatidlycholine (PC), 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphocholine (POPC), 1-stearoyl-2-oleoyl-sn-glycero-3-phosphoserine (PS), N-palmitoyl-D-erythro-sphingosylphosphorylcholine (SM), ovine wool cholesterol (chol), and HPLC grade chloroform (Avanti Polar Lipids) using a miniextruder and 0.1 μm polycarbonate membranes (Avanti Polar Lipids). Control liposomes [4:1 (wt/wt) PC:chol], liposomes containing cardiolipin [1:7:2 (wt/wt) CL:PC:chol], and VM liposomes [6.7:2:2.3:2.3:1 (mol/mol) chol:POPC:SM:DOPE:PS] were prepared as previously described (26) and diluted to 0.25 mg/mL in PBS.
Before liposome immobilization, an L1 sensor chip (Biacore) was prepared with two 100-μL injections of 40 mM N-octyl-β-D-glucopyranoside (CalBiochem) at a flow rate of 50 μL/min. Liposomes were immobilized in two successive 100-μL injections at a flow rate of 5 μL/min. Liposome surfaces were equilibrated in PBS for 3 h at a flow rate of 20 μL/min; this did not affect immobilization levels and served as a measure of surface stability.
Antibodies were centrifuged once at ≥100,000 × g for 15 min before use in an attempt to remove potential aggregates. To account for changes in the refraction index due to buffer, PBS was injected before each antibody sample. Both PBS and antibody solutions were injected a flow rate of 20 μL/min for 120 s. Antibody injections were followed by a 200-s dissociation phase and 1,200-s stabilization period. Once all of the flow cells had been used, the L1 surface was regenerated with detergent and liposomes immobilized anew. BIAevaluation software was used to subtract the signal contributed by PBS.
Neutralization Assay.
Neutralization assays performed at Monogram Biosciences were conducted as previously described (50) using viruses pseudotyped with BHT92594c, CMW93960, HXB2, JR-CSF, JR-FL, NL4-3, and SF162 Env (4). Briefly, pseudovirus encoding a luciferase reporter gene was incubated for 1 h at 37°C with antibody, and infectivity was determined by measuring luciferase activity in the lysates of U87.CD4.CXCR4.CCR5 cells.
Supplementary Material
Acknowledgments
We thank Jillian Sola and Niccole Schultz for assistance with antibody expression and purification. This work was funded in part through National Institutes of Health Grants AI33292 (to D.R.B.) AI069993 (to M.B.Z.), and T32 AI007606 (to M.B.Z.) and the International AIDS Vaccine Initiative through the Neutralizing Antibody Consortium.
Footnotes
Conflict of interest statement: D.R.B. serves on the Board of Calmune Corporation, which carries out research in the area of membrane proximal antibodies. Calmune did not financially support this work.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/cgi/content/full/0909680107/DCSupplemental.
References
- 1.Mascola JR. Defining the protective antibody response for HIV-1. Curr Mol Med. 2003;3:209–216. doi: 10.2174/1566524033479799. [DOI] [PubMed] [Google Scholar]
- 2.Burton DR, et al. HIV vaccine design and the neutralizing antibody problem. Nat Immunol. 2004;5:233–236. doi: 10.1038/ni0304-233. [DOI] [PubMed] [Google Scholar]
- 3.Walker LM, et al. Protocol G Principal Investigators Broad and potent neutralizing antibodies from an African donor reveal a new HIV-1 vaccine target. Science. 2009;326:285–289. doi: 10.1126/science.1178746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Binley JM, et al. Comprehensive cross-clade neutralization analysis of a panel of anti-human immunodeficiency virus type 1 monoclonal antibodies. J Virol. 2004;78:13232–13252. doi: 10.1128/JVI.78.23.13232-13252.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehandru S, et al. Neutralization profiles of newly transmitted human immunodeficiency virus type 1 by monoclonal antibodies 2G12, 2F5, and 4E10. J Virol. 2004;78:14039–14042. doi: 10.1128/JVI.78.24.14039-14042.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zwick MB, et al. Broadly neutralizing antibodies targeted to the membrane-proximal external region of human immunodeficiency virus type 1 glycoprotein gp41. J Virol. 2001;75:10892–10905. doi: 10.1128/JVI.75.22.10892-10905.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nelson JD, et al. An affinity-enhanced neutralizing antibody against the membrane-proximal external region of human immunodeficiency virus type 1 gp41 recognizes an epitope between those of 2F5 and 4E10. J Virol. 2007;81:4033–4043. doi: 10.1128/JVI.02588-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muster T, et al. A conserved neutralizing epitope on gp41 of human immunodeficiency virus type 1. J Virol. 1993;67:6642–6647. doi: 10.1128/jvi.67.11.6642-6647.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zwick MB, et al. Anti-human immunodeficiency virus type 1 (HIV-1) antibodies 2F5 and 4E10 require surprisingly few crucial residues in the membrane-proximal external region of glycoprotein gp41 to neutralize HIV-1. J Virol. 2005;79:1252–1261. doi: 10.1128/JVI.79.2.1252-1261.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cardoso RM, et al. Structural basis of enhanced binding of extended and helically constrained peptide epitopes of the broadly neutralizing HIV-1 antibody 4E10. J Mol Biol. 2007;365:1533–1544. doi: 10.1016/j.jmb.2006.10.088. [DOI] [PubMed] [Google Scholar]
- 11.Julien JP, Bryson S, Nieva JL, Pai EF. Structural details of HIV-1 recognition by the broadly neutralizing monoclonal antibody 2F5: Epitope conformation, antigen-recognition loop mobility, and anion-binding site. J Mol Biol. 2008;384:377–392. doi: 10.1016/j.jmb.2008.09.024. [DOI] [PubMed] [Google Scholar]
- 12.Ofek G, et al. Structure and mechanistic analysis of the anti-human immunodeficiency virus type 1 antibody 2F5 in complex with its gp41 epitope. J Virol. 2004;78:10724–10737. doi: 10.1128/JVI.78.19.10724-10737.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pejchal R, et al. A conformational switch in human immunodeficiency virus gp41 revealed by the structures of overlapping epitopes recognized by neutralizing antibodies. J Virol. 2009;83:8451–8462. doi: 10.1128/JVI.00685-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cardoso RM, et al. Broadly neutralizing anti-HIV antibody 4E10 recognizes a helical conformation of a highly conserved fusion-associated motif in gp41. Immunity. 2005;22:163–173. doi: 10.1016/j.immuni.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 15.Zwick MB. The membrane-proximal external region of HIV-1 gp41: A vaccine target worth exploring. AIDS. 2005;19:1725–1737. doi: 10.1097/01.aids.0000189850.83322.41. [DOI] [PubMed] [Google Scholar]
- 16.Salzwedel K, West JT, Hunter E. A conserved tryptophan-rich motif in the membrane-proximal region of the human immunodeficiency virus type 1 gp41 ectodomain is important for Env-mediated fusion and virus infectivity. J Virol. 1999;73:2469–2480. doi: 10.1128/jvi.73.3.2469-2480.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Killian JA, von Heijne G. How proteins adapt to a membrane-water interface. Trends Biochem Sci. 2000;25:429–434. doi: 10.1016/s0968-0004(00)01626-1. [DOI] [PubMed] [Google Scholar]
- 18.Suárez T, Nir S, Goñi FM, Saéz-Cirión A, Nieva JL. The pre-transmembrane region of the human immunodeficiency virus type-1 glycoprotein: A novel fusogenic sequence. FEBS Lett. 2000;477:145–149. doi: 10.1016/s0014-5793(00)01785-3. [DOI] [PubMed] [Google Scholar]
- 19.Schibli DJ, Montelaro RC, Vogel HJ. The membrane-proximal tryptophan-rich region of the HIV glycoprotein, gp41, forms a well-defined helix in dodecylphosphocholine micelles. Biochemistry. 2001;40:9570–9578. doi: 10.1021/bi010640u. [DOI] [PubMed] [Google Scholar]
- 20.Song L, et al. Broadly neutralizing anti-HIV-1 antibodies disrupt a hinge-related function of gp41 at the membrane interface. Proc Natl Acad Sci USA. 2009;106:9057–9062. doi: 10.1073/pnas.0901474106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sun ZY, et al. HIV-1 broadly neutralizing antibody extracts its epitope from a kinked gp41 ectodomain region on the viral membrane. Immunity. 2008;28:52–63. doi: 10.1016/j.immuni.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 22.Grundner C, Mirzabekov T, Sodroski J, Wyatt R. Solid-phase proteoliposomes containing human immunodeficiency virus envelope glycoproteins. J Virol. 2002;76:3511–3521. doi: 10.1128/JVI.76.7.3511-3521.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alam SM, et al. The role of antibody polyspecificity and lipid reactivity in binding of broadly neutralizing anti-HIV-1 envelope human monoclonal antibodies 2F5 and 4E10 to glycoprotein 41 membrane proximal envelope epitopes. J Immunol. 2007;178:4424–4435. doi: 10.4049/jimmunol.178.7.4424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huarte N, et al. The broadly neutralizing anti-human immunodeficiency virus type 1 4E10 monoclonal antibody is better adapted to membrane-bound epitope recognition and blocking than 2F5. J Virol. 2008;82:8986–8996. doi: 10.1128/JVI.00846-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Haynes BF, et al. Cardiolipin polyspecific autoreactivity in two broadly neutralizing HIV-1 antibodies. Science. 2005;308:1906–1908. doi: 10.1126/science.1111781. [DOI] [PubMed] [Google Scholar]
- 26.Sánchez-Martínez S, Lorizate M, Katinger H, Kunert R, Nieva JL. Membrane association and epitope recognition by HIV-1 neutralizing anti-gp41 2F5 and 4E10 antibodies. AIDS Res Hum Retroviruses. 2006;22:998–1006. doi: 10.1089/aid.2006.22.998. [DOI] [PubMed] [Google Scholar]
- 27.Scherer EM, Zwick MB, Teyton L, Burton DR. Difficulties in eliciting broadly neutralizing anti-HIV antibodies are not explained by cardiolipin autoreactivity. AIDS. 2007;21:2131–2139. doi: 10.1097/QAD.0b013e3282a4a632. [DOI] [PubMed] [Google Scholar]
- 28.Vcelar B, et al. Reassessment of autoreactivity of the broadly neutralizing HIV antibodies 4E10 and 2F5 and retrospective analysis of clinical safety data. AIDS. 2007;21:2161–2170. doi: 10.1097/QAD.0b013e328285da15. [DOI] [PubMed] [Google Scholar]
- 29.Matyas GR, Beck Z, Karasavvas N, Alving CR. Lipid binding properties of 4E10, 2F5, and WR304 monoclonal antibodies that neutralize HIV-1. Biochim Biophys Acta. 2009;1788:660–665. doi: 10.1016/j.bbamem.2008.11.015. [DOI] [PubMed] [Google Scholar]
- 30.Xu JL, Davis MM. Diversity in the CDR3 region of V(H) is sufficient for most antibody specificities. Immunity. 2000;13:37–45. doi: 10.1016/s1074-7613(00)00006-6. [DOI] [PubMed] [Google Scholar]
- 31.Alving CR. 4E10 and 2F5 monoclonal antibodies: Binding specificities to phospholipids, tolerance, and clinical safety issues. AIDS. 2008;22:649–651. doi: 10.1097/QAD.0b013e3282f51922. [DOI] [PubMed] [Google Scholar]
- 32.Zwick MB, et al. The long third complementarity-determining region of the heavy chain is important in the activity of the broadly neutralizing anti-human immunodeficiency virus type 1 antibody 2F5. J Virol. 2004;78:3155–3161. doi: 10.1128/JVI.78.6.3155-3161.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lorizate M, Gómara MJ, de la Torre BG, Andreu D, Nieva JL. Membrane-transferring sequences of the HIV-1 Gp41 ectodomain assemble into an immunogenic complex. J Mol Biol. 2006;360:45–55. doi: 10.1016/j.jmb.2006.04.056. [DOI] [PubMed] [Google Scholar]
- 34.White SH, Wimley WC. Hydrophobic interactions of peptides with membrane interfaces. Biochim Biophys Acta. 1998;1376:339–352. doi: 10.1016/s0304-4157(98)00021-5. [DOI] [PubMed] [Google Scholar]
- 35.Barbas CF, 3rd, Burton DR, Scott JK, Silverman GJ. Phage Display: A Laboratory Manual. Cold Spring Harbor, New York: Cold Spring Harbor Laboratory Press; 2001. [Google Scholar]
- 36.Bebbington CR, et al. High-level expression of a recombinant antibody from myeloma cells using a glutamine synthetase gene as an amplifiable selectable marker. Biotechnology (N Y) 1992;10:169–175. doi: 10.1038/nbt0292-169. [DOI] [PubMed] [Google Scholar]
- 37.Burton DR, et al. Efficient neutralization of primary isolates of HIV-1 by a recombinant human monoclonal antibody. Science. 1994;266:1024–1027. doi: 10.1126/science.7973652. [DOI] [PubMed] [Google Scholar]
- 38.Aloia RC, Jensen FC, Curtain CC, Mobley PW, Gordon LM. Lipid composition and fluidity of the human immunodeficiency virus. Proc Natl Acad Sci USA. 1988;85:900–904. doi: 10.1073/pnas.85.3.900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aloia RC, Tian H, Jensen FC. Lipid composition and fluidity of the human immunodeficiency virus envelope and host cell plasma membranes. Proc Natl Acad Sci USA. 1993;90:5181–5185. doi: 10.1073/pnas.90.11.5181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brügger B, et al. The HIV lipidome: A raft with an unusual composition. Proc Natl Acad Sci USA. 2006;103:2641–2646. doi: 10.1073/pnas.0511136103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Richieri SP, et al. Characterization of highly purified, inactivated HIV-1 particles isolated by anion exchange chromatography. Vaccine. 1998;16:119–129. doi: 10.1016/s0264-410x(97)00196-5. [DOI] [PubMed] [Google Scholar]
- 42.Schlame M. Cardiolipin synthesis for the assembly of bacterial and mitochondrial membranes. J Lipid Res. 2008;49:1607–1620. doi: 10.1194/jlr.R700018-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Haynes BF, Moody MA, Verkoczy L, Kelsoe G, Alam SM. Antibody polyspecificity and neutralization of HIV-1: A hypothesis. Hum Antibodies. 2005;14:59–67. [PMC free article] [PubMed] [Google Scholar]
- 44.Montero M, van Houten NE, Wang X, Scott JK. The membrane-proximal external region of the human immunodeficiency virus type 1 envelope: dominant site of antibody neutralization and target for vaccine design. Microbiol Mol Biol Rev. 2008;72:54–84. doi: 10.1128/MMBR.00020-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Du J, Yang H, Guo Y, Ding J. Structure of the Fab fragment of therapeutic antibody Ofatumumab provides insights into the recognition mechanism with CD20. Mol Immunol. 2009;46:2419–2423. doi: 10.1016/j.molimm.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 46.Parren PW, et al. Antibody protects macaques against vaginal challenge with a pathogenic R5 simian/human immunodeficiency virus at serum levels giving complete neutralization in vitro. J Virol. 2001;75:8340–8347. doi: 10.1128/JVI.75.17.8340-8347.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Buchacher A, et al. Generation of human monoclonal antibodies against HIV-1 proteins: Electrofusion and Epstein-Barr virus transformation for peripheral blood lymphocyte immortalization. AIDS Res Hum Retroviruses. 1994;10:359–369. doi: 10.1089/aid.1994.10.359. [DOI] [PubMed] [Google Scholar]
- 48.Kunert R, Wolbank S, Stiegler G, Weik R, Katinger H. Characterization of molecular features, antigen-binding, and in vitro properties of IgG and IgM variants of 4E10, an anti-HIV type 1 neutralizing monoclonal antibody. AIDS Res Hum Retroviruses. 2004;20:755–762. doi: 10.1089/0889222041524571. [DOI] [PubMed] [Google Scholar]
- 49.Heckman KL, Pease LR. Gene splicing and mutagenesis by PCR-driven overlap extension. Nat Protoc. 2007;2:924–932. doi: 10.1038/nprot.2007.132. [DOI] [PubMed] [Google Scholar]
- 50.Richman DD, Wrin T, Little SJ, Petropoulos CJ. Rapid evolution of the neutralizing antibody response to HIV type 1 infection. Proc Natl Acad Sci USA. 2003;100:4144–4149. doi: 10.1073/pnas.0630530100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.