Abstract
Objective
To assess the extent to which observed associations at population level between income inequality and mortality are statistical artefacts.
Design
Indirect “what if” simulation by using observed risks of mortality at individual level as a function of income to construct hypothetical state level mortality specific for age and sex as if the statistical artefact argument were 100% correct.
Setting
Data from the 1990 census for the 50 US states plus Washington, DC, were used for population distributions by age, sex, state, and income range; data disaggregated by age, sex, and state from the Centers for Disease Control and Prevention were used for mortality; and regressions from the national longitudinal mortality study were used for the individual level relation between income and risk of mortality.
Results
Hypothetical mortality, while correlated with inequality (as implied by the logic of the statistical artefact argument), showed a weaker association with states’ levels of income inequality than the observed mortality.
Conclusions
The observed associations in the United States at the state level between income inequality and mortality cannot be entirely or substantially explained as statistical artefacts of an underlying individual level relation between income and mortality. There remains an important association between income inequality and mortality at state level over and above anything that could be accounted for by any statistical artefact. This result reinforces the need to consider a broad range of factors, including the social milieu, as fundamental determinants of health.
Key messages
Evidence is accumulating that living in a society with higher inequality in income predisposes its members to higher mortality; at the same time, there is widespread evidence that, for individuals, higher income is protective
This individual level relation could “explain” the former societal level relation
The strength of observed levels of association between income inequality and mortality, however, may go well beyond what can be explained as a statistical artefact of an individual level relation between income and mortality
The empirical analysis reported here, based on 1990 data for US states, suggests that the association between income inequality and mortality is considerably stronger than can be accounted for by any statistical artefact
Research underpinning public health policy should therefore take a broad view of the importance of the social milieu as a fundamental determinant of health
Introduction
Considerable debate surrounds the impact of socioeconomic circumstances on individuals’ health. Recent results suggest that there is a link not only between individual socioeconomic circumstances and health but also between the socioeconomic milieu in which individuals live and their health. Research has shown that higher levels of inequality in income among nations, states, or cities in the United States, or other geographically defined populations, are associated with higher mortality.1–4
Concerns have been raised by Gravelle, however, that these results may be no more than a statistical artefact.5 Gravelle points out, as others have noted previously,6,7 that a “diminishing returns” protective effect of higher individual income on individual risk of death is sufficient to account for differences in mortality between populations if there are differences in the extent of wealth and poverty, hence in the degree of income inequality.
The logic of this argument is correct. At the individual level, higher income (or some closely related but unmeasured factor, such as social status, for which income is a proxy) is causally associated with greater longevity.8 Moreover, while an extra dollar or pound of income is protective, the amount of protective effect tails off as total income rises.8,9
At the level of a population there is always some mixture of people with low, middle, and high incomes. If one population has a more equal distribution of income than another, this is equivalent to there being fewer individuals with either very high or very low incomes and more with incomes closer to the middle. But if a poorer individual is £1000 better off in a second population the beneficial effect on his or her risk of mortality is larger than the adverse impact on the risk of some richer person being £1000 worse off because of the diminishing protective returns of additional income. Thus, a population with a more equal distribution of income can have a lower mortality, other things being equal, solely as a result of a generic curvilinear individual level causal relation between income and risk of mortality.
This logical possibility, however, is not a sufficient reason to dismiss the potential importance of inequality in income as an independent determinant of population level mortality. This remains an empirical question.
We approached this question indirectly by first estimating a generic individual level relation between income and mortality. We then simulated the extent to which variations in the distribution of income across populations can account for the observed population level relation between income inequality and mortality. In other words, we asked “what if” our well specified relation between individual level income and mortality were fully causal, the key step in Gravelle’s argument. We therefore applied this relation to all individuals in a population group based on its actual income distribution and then calculated expected mortality. The extent to which we reproduce the observed population level association between income inequality and mortality is then an empirical test of the statistical artefact hypothesis.
Method
The argument that the association between income inequality and mortality is artefactual depends on bringing together information at two levels. One is the level of individuals; the other level is that of populations such as US states.
The first step is to derive a reliable individual level relation between income and risk of mortality. This generic relation was estimated for the US population by using the national longitudinal mortality study. 10 This data set matched files containing household income and other demographic information from the US Census Bureau’s current population survey to the National Death Index to provide about 7.6 million person years of mortality exposure from 10 years of follow up.
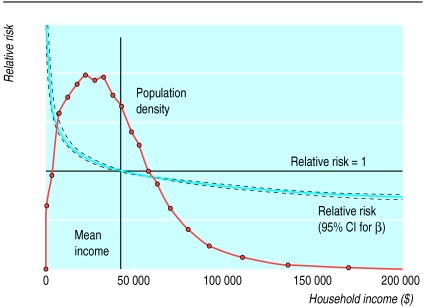
The downward sloping curves (close together) in figure 1 show the results—the estimated relation between household income and the relative risk of mortality, plus a 95% confidence interval, after age and sex were controlled for. The relation is highly significant both statistically and substantively and is clearly consistent with a diminishing returns individual level relation between income and risk of mortality. (While we assumed logarithmic specification, other analyses determined that this was a reasonable functional form.)
Figure 1.
Relative risk of dying and population distribution for US individuals by household income ($)
The remaining steps in the analysis complement this individual level relation with consistent population level data from the 1990 census on income inequality and mortality for each of the 50 US states plus Washington, DC. Special Census Bureau tabulations provided counts of the numbers of individuals living in households by state, sex, detailed age groupings, and detailed income ranges. The other “humped” curve in figure 1 shows the resulting distribution of individuals by household income for the whole of the United States. Finally, 3 years of mortality data by state, sex, and age centred on 1990 were downloaded from the Centers for Disease Control and Prevention CDC Wonder site (http://wonder.cdc.gov/).
Given these data, a series of hypothetical standardised mortalities specific for states was constructed. For each state, the generic relation between individual level income and risk of mortality, shown by the income-mortality curve in figure 1, was applied to the actual income distribution within the state. In other words, a set of expected relative risks of mortality was calculated for each detailed age-sex-income-state category. These relative risks were next averaged over income groups, within each age-sex-state group, taking account of number of individuals in each income interval (within age-sex-state groups). The result is a set of relative risks of dying as if the only reason for differences between states in risks of mortality were differences in income inequality between states (that is, differences in the composition of each state’s population by income group).
We then multiplied these relative risks by corresponding national mortality specific for age-sex and then standardised the rates by age-sex to the overall US population. The result is a set of hypothetical state specific mortalities where the only reason a state’s mortality experience should differ from the national pattern is that its population has a different income distribution. These hypothetical mortalities are thus, by construction, exactly those we should observe if Gravelle’s artefact hypothesis were 100% correct.
Results
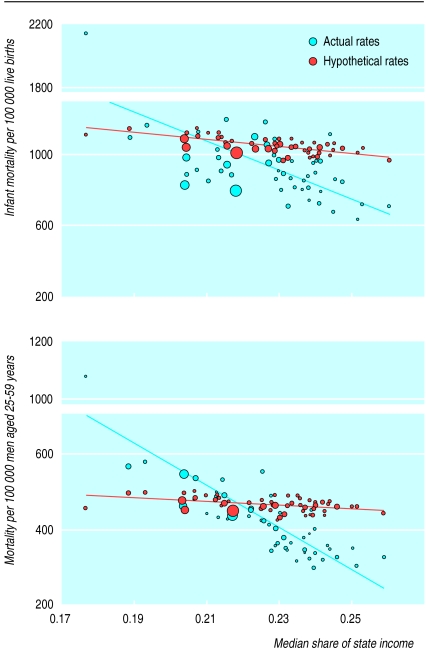
Some of the main results are shown in figures 2a-b for mortality in infants and working age (25 to 59) men, respectively. Mortality is on the y axis, with income inequality, measured by the proportion of total household income accruing to the bottom half of the population (the “median share”) along the x axis. Each point in these scatter plots represents one of the 50 US states plus Washington, DC, with the area of each circle proportional to the state’s population.
Figure 2.
Actual and hypothetical mortality for infants and working age men by income inequality. Solid and dashed lines are ordinary least squares regression fits through the actual and hypothetical data points, respectively
Discussion
The pattern of mortality generated from a literal application of Gravelle’s artefact hypothesis provides a poor fit with the observed data in the United States. If the observed association between state level standardised mortality and income inequality were completely artefactual then the two scatters of points (actual and hypothetical, solid and open circles) would be on top of one another and the two regression lines would be superimposed. This is clearly not the case. Mortality based on the artefact hypothesis shows some slope in the expected direction—a higher share of income accruing to the bottom half of the population, indicating lower inequality, is associated with lower mortality. But these slopes are considerably less than the slopes of actual mortality in relation to income inequality.
The observed associations in the United States at the state level between income inequality and mortality therefore cannot be entirely, or even substantially, explained as statistical artefacts of an underlying individual level relation between income and risk of mortality. There remains an important association between state level income inequality and mortality, over and above anything that could be accounted for by statistical artefact.
Acknowledgments
We acknowledge helpful discussions with Richard Wilkinson, George Davey-Smith, Eric Brunner, Bruce Kennedy, Ichiro Kawachi, Geoff Rowe, and Jean-Marie Berthelot; comments by two anonymous referees; participants in the conference on economic equity in Ann Arbor, 4-6 June; and members of the population health programme of the Canadian Institute for Advanced Research on earlier versions of this paper. We also thank Susan Leroux for helpful analytical assistance. We remain responsible for any errors or infelicities.
Footnotes
Funding: MCW was funded by Statistics Canada and Canadian Population Health Initiative; GK was funded by University of Michigan Initiative on Inequalities in Health NR.
Competing interests: None declared.
References
- 1.Wilkinson RG. Unhealthy societies: the afflictions of inequality. London: Routledge; 1996. [Google Scholar]
- 2.Kaplan GA, Pamuk ER, Lynch JW, Cohen RD, Balfour JL. Inequality in income and mortality in the United States: analysis of mortality and potential pathways. BMJ. 1996;312:999–1003. doi: 10.1136/bmj.312.7037.999. . (Correction in BMJ 312:1253.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kennedy BP, Kawachi I, Prothrow-Smith D. Income distribution and mortality: cross-sectional ecological study of the Robin Hood index in the United States. BMJ. 1996;312:1004–1007. doi: 10.1136/bmj.312.7037.1004. . (Correction in BMJ 312:1194.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lynch JW, Kaplan GA, Pamuk ER, Cohen RD, Heck K, Balfour JL, Yen IH. Income inequality and mortality in metropolitan areas of the United States. Am J Public Health. 1998;88:1074–1080. doi: 10.2105/ajph.88.7.1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gravelle H. How much of the relation between population mortality and unequal distribution of income is a statistical artefact? BMJ. 1998;316:382–385. doi: 10.1136/bmj.316.7128.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duleep HO. Mortality and income inequality among economically developed countries. Social Security Bull. 1995;58:34–50. [PubMed] [Google Scholar]
- 7.Lynch JW, Kaplan GA. Understanding how inequality in the distribution of income affects health. J Health Psychol. 1997;2:297–314. doi: 10.1177/135910539700200303. [DOI] [PubMed] [Google Scholar]
- 8.Wolfson M, Rowe G, Gentleman JF, Tomiak M. Career earnings and death: a longitudinal analysis of older Canadian men. J Gerontol Soc Sci. 1993;48:S167–S179. doi: 10.1093/geronj/48.4.s167. [DOI] [PubMed] [Google Scholar]
- 9.Backlund E, Sorlie PD, Johnson NJ. The shape of the relationship between income and mortality in the United States: evidence from the national longitudinal mortality study. Ann Epidemiol. 1996;6:1–9. doi: 10.1016/1047-2797(95)00090-9. [DOI] [PubMed] [Google Scholar]
- 10.Rogot E, Sorlie PD, Johnson NJ. Life expectancy by employment status, income, and education in the national longitudinal mortality study. Public Health Rep. 1992;107:457–461. [PMC free article] [PubMed] [Google Scholar]