Abstract
The post cardiac injury syndrome is characterized by the development of a fever, pleuropericarditis, and parenchymal pulmonary infiltrates in the weeks following trauma to the pericardium or myocardium. According to previous reports, almost all cases develop after major cardiac surgery or a myocardial infarction. Recently, a few reports have described post cardiac injury syndrome as a complication of endovascular procedures such as percutaneous cardiac intervention. Here we describe an unusual case of post cardiac injury syndrome after a percutaneous coronary intervention.
Keywords: Post cardiac injury syndrome, percutaneous cardiac intervention
INTRODUCTION
Post cardiac injury syndrome (PCIS) is a clinical entity that occurs as a complication of cardiac surgery or a myocardial infarction.1 It is also referred to as post pericardiotomy syndrome and Dressler's syndrome. The disease is characterized by inflammation of the pericardium, pleura, and pulmonary parenchyma following a cardiac injury.2 PCIS occurs whenever the heart is injured. However, PCIS following percutaneous cardiac intervention (PCI) is relatively rare. Here, we report a rare case of PCIS that occurred after a PCI with an atypical early onset.
CASE REPORT
A-50-year-old male was admitted to the hospital because of stable angina, with onset one month prior to admission. The medical history was unremarkable. The findings on the physical examination and the blood tests upon admission were normal. Electrocardiography showed no specific findings (Fig. 1A). A coronary angiogram revealed diffuse irregular, up to 90%, luminal narrowing of the middle segment of the anterior descending artery (m-LAD) (Fig. 2A). A Judkins left catheter was engaged at the left coronary artery. The m-LAD lesion was wired with a High Torque PILOT 0.014 guidewire (Guidant). A 2.5×20 mm Ryujin plus (Terumo) balloon dilatation was performed. A follow-up angiography after the balloon dilation revealed a 60% residual stenosis. A 3.0×28 mm TAXUS stent (Boston scientific) was deployed to the m-LAD lesion. A final angiogram revealed that the procedure was successful (Fig. 2B). There were no immediate clinical or angiographic signs of complications throughout the procedure. Three hours after the procedure the patient developed dyspnea, mild chest pain, and deep breathing. However, blood pressure and arterial oxygen saturation levels were stable; the electrocardiography indicated no significant changes from the reference electrocardiography before the PCI. Sixteen hours after the procedure, pleuritic chest pain and dyspnea increased and a fever developed. On the physical examination, blood pressure was 90/40 mmHg, respiratory rate was 30 breaths per minute, and heart rate was 60 beats per minute. On auscultation, a harsh pericardial friction rub could be heard. The chest X-ray showed a left pleural effusion as a result of an acute pleuritis (Fig. 3). The electrocardiography showed widespread concave ST segment elevations (Fig. 1B). The blood tests indicated inflammation: the leukocyte count (1.6×109/L), erythrocyte sedimentation rate (28 mm/hr), and serum C-reactive protein concentration (7.95 mg/dL) were all elevated. The serum creatinine kinase and Creatine-kinase-MB levels remained within the normal range. An emergency echocardiogram was performed. A moderate pericardial effusion was surrounding the heart on the echocardiography. We concluded that the patient had an acute pleuropericarditis. He was given 500 mg of aspirin two times a day until discharge. For control of the pericardial effusion and the differential diagnosis of the cause of pericarditis, a pericardiocentesis was performed. A total of 1,100 mL of brown sterile fluid was drained over three days. The cytology indicated that the nucleated cells (1.520×103/mm3) were mostly polymorphonuclear leukocytes (70%); there were no malignant cells. There were some red blood cells noted (1.525 ×104/mm3). The pericardial effusion was exudative. The pericardial effusion had resolved by the follow-up echocardiography four days after the pericardiocentesis. The patient was symptom-free and the ST segment elevations returned to baseline during the rest of the hospitalization. The CRP and ESR levels normalized in 14 days. The patient was discharged.
Fig. 1.

A 12-lead electrocardiogram of the patient. (A) The ECG before the percutaneous coronary intervention, (B) The ECG after the percutaneous coronary intervention. The ECG showed widespread concave ST segment elevations.
Fig. 2.
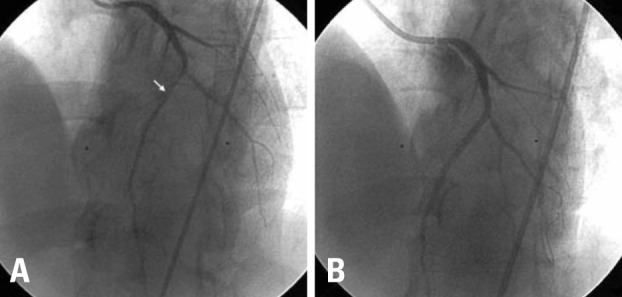
(A) Pre-intervention image: Left coronary angiogram shows significant narrowing of the middle left anterior descending artery (arrow). (B) Post-intervention image: The stent was successfully deployed to the middle left anterior descending artery and the final angiogram showed optimal result.
Fig. 3.
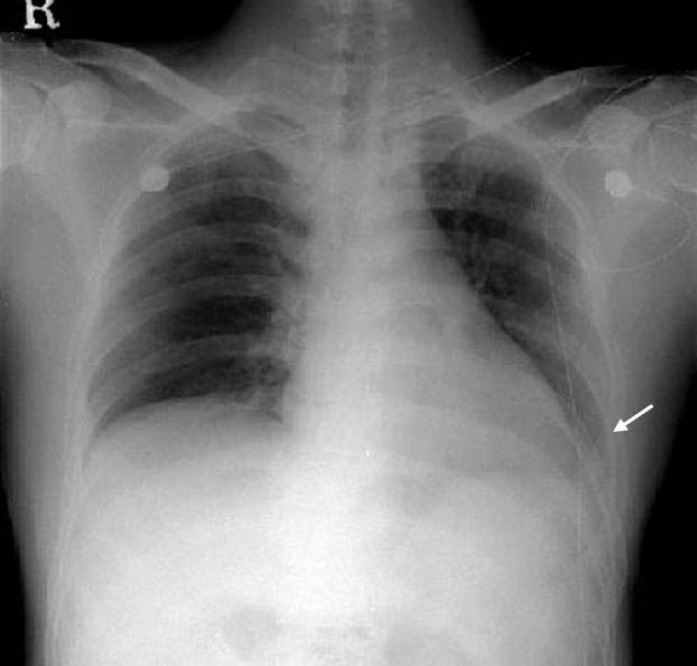
Posteroanterior chest X-ray shows a left pleural effusion (arrow).
DISCUSSION
Late pericarditis following myocardial infarction, cardiac surgery, or trauma is referred to as post myocardial infarction syndrome or post cardiotomy syndrome. PCIS includes both of these entities.3 The diagnosis of PCIS depends on the characteristic clinical features. The diagnosis is supported by the findings of fever, chest pain, pericarditis, and pulmonary involvement. Abnormal laboratory findings include a leukocytosis, elevated inflammatory markers, and chest X-ray abnormalities with or without pulmonary infiltrates.1-4 The most common cause of PCIS is major cardiac surgery.5 The reported incidence of PCIS following cardiac surgery varies from 15 to 30%.6 Although almost all of the cases follow major cardiac surgery or a myocardial infarction, unusual cases after minor cardiac insults have also been reported. According to Troughton, et al.,7 the incidence of pericardial complications after PCI is less than 0.2%. The patient reported here had typical clinical features of the PCIS. The patient had a pleural effusion, elevated inflammatory markers, and typical symptoms of pericarditis after a PCI. A similar case has been recently reported in a 79-year-old woman described by Hearne, et al., who underwent PCI for multivessel coronary artery disease; she developed signs and symptoms of PCIS within three weeks of the PCI.5
The etiology of the PCIS is still poorly understood. The most widely accepted hypothesis is that the development of an autoimmune response against heart antigens leads to a generalized pericardial inflammation and pericarditis.1-8 Dressler anticipated a contemporary theory explaining the pathophysiology of PCIS, i.e., the induction of antiheart antibodies against autoantigens that are exposed following cardiac injury.9,10 An alternative hypothesis suggests that the leakage of blood into the pericardial space causes the PCIS.2-5 In our case, the drained pericardial effusion contained some red blood cells, suggesting that bleeding into the pericardial space had occurred. It was possible that micro perforation of the coronary artery leaked into the pericardial space. This suggests that leakage of blood into the pericardial space may play an important role in PCIS. The PCIS usually has a late onset of pleuropericarditis. According to Seizner and colleagues,4 the onset of the syndrome was about 20 days after the injury. By contrast, our patient developed pericardial and pleural effusions three hours after the PCI, which is quite rare. Another case of rapid onset (4 hours) of PCIS symptoms after PCI was reported by Setoyama, et al.5 The authors explained that this rapid onset of PCIS was due to stimulation of the immune system by a recent myocardial injury prior to the PCI. In our case, the patient had chest pain for a month prior to presentation and an early onset of PCIS, which might be explained by a similar mechanism.
Here we reported a rare case of PCIS that occurred after a PCI with atypical early onset. PCIS should be considered in patients that develop a fever, dyspnea, and have abnormal electrocardiography changes after a PCI.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Gungor B, Ucer E, Erdinler IC. Uncommon presentation of postcardiac injury syndrome: acute pericarditis after percutaneous coronary intervention. Int J Cardiol. 2008;128:e19–e21. doi: 10.1016/j.ijcard.2007.04.159. [DOI] [PubMed] [Google Scholar]
- 2.Tang RB, Liu XH, Dong JZ, Liu XP, Kang JP, Ma CS. Postcardiac injury syndrome complicating circumferential. Chin Med J (Engl) 2007;120:1940–1942. [PubMed] [Google Scholar]
- 3.Khan AH. The postcardiac injury syndromes. Clin Cardiol. 1992;15:67–72. doi: 10.1002/clc.4960150203. [DOI] [PubMed] [Google Scholar]
- 4.Seizner TJ, King TE, Jr, Antony VB, Sahn SA. The pleuropulmonary manifestations of the postcardiac injury syndrome. Chest. 1983;84:383–387. doi: 10.1378/chest.84.4.383. [DOI] [PubMed] [Google Scholar]
- 5.Setoyama T, Furukawa Y, Abe M, Nakagawa Y, Kita T, Kimura T. Acute pleuropericarditis after coronary stenting: a case report. Circ J. 2006;70:358–361. doi: 10.1253/circj.70.358. [DOI] [PubMed] [Google Scholar]
- 6.Light RW. Pleural effusions following cardiac injury and coronary artery bypass graft surgery. Semin Respir Crit Care Med. 2001;22:657–664. doi: 10.1055/s-2001-18802. [DOI] [PubMed] [Google Scholar]
- 7.Troughton RW, Asher CR, Klein AL. Pericarditis. Lancet. 2004;363:717–727. doi: 10.1016/S0140-6736(04)15648-1. [DOI] [PubMed] [Google Scholar]
- 8.Wessman DE, Stafford CM. The postcardiac injury syndrome: case report and review of the literature. South Med J. 2006;99:309–314. doi: 10.1097/01.smj.0000203330.15503.0b. [DOI] [PubMed] [Google Scholar]
- 9.Dressler W. The postmyocardial infarction syndrome; recurrent pericardtitis, pleurisy, and pneumonitis. Heart Bull. 1958;7:102–104. [PubMed] [Google Scholar]
- 10.Bajaj BP, Evans KE, Thomas P. Postpericardiotomy syndrome following temporary and permanent transvenous pacing. Postgrad Med J. 1999;75:357–358. doi: 10.1136/pgmj.75.884.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim S, Sahn SA. Postcardiac injury syndrome. An immunologic pleural fluid analysis. Chest. 1996;109:570–572. doi: 10.1378/chest.109.2.570. [DOI] [PubMed] [Google Scholar]
- 12.Hearne C, Forjuoh SN. Postcardiac injury syndrome after coronary angioplasty and stenting. J Am Board Fam Pract. 2003;16:73–74. doi: 10.3122/jabfm.16.1.73. [DOI] [PubMed] [Google Scholar]
- 13.Escaned J, Ahmad RA, Shiu MF. Pleural effusion following coronary perforation during balloon angioplasty: an unusual presentation of the postpericardiotomy syndrome. Eur Heart J. 1992;13:716–717. doi: 10.1093/oxfordjournals.eurheartj.a060241. [DOI] [PubMed] [Google Scholar]


