Abstract
Understanding the impact of prior substance misuse on emergent health problems is important to the implementation of effective preventive care. This study examined 5-year incidence rates using a sample of middle-aged adult adoptees (N = 309, Mage = 44.32, SDage = 7.28). Subjects reported on health problems at two waves of study. DSM-IV diagnoses of substance misuse were obtained using a semi-structured diagnostic interview. Finally, health services utilization and perceived health status were collected. Lifetime diagnoses of marijuana and other non-marijuana substance misuse significantly predicted new occurrences of cardiovascular and metabolic disease. Alcohol misuse predicted earlier onset of cardiovascular disease among men. Marijuana and other non-marijuana drugs predicted earlier onset of CVD for men and women. Finally, marijuana and other non-marijuana drugs predicted earlier onset of metabolic disease among men. Substance misuse did not predict health services utilization despite higher rates of disease. These findings emphasize the need to assess lifetime substance misuse when evaluating health risks associated with use.
Introduction
Substance misuse has been linked with a variety of health problems including respiratory problems1-4, cardiovascular disease5-9, thyroid functioning 10, cancer4 and metabolic syndrome11 12. The majority of the observed substance-induced health problems are acute events related to active metabolism of the substance of interest. Few studies have prospectively examined substance-related health problems following sustained abstinence. Previous analysis of the Iowa Adoption Studies data13 showed few associations between substance misuse and health problems among individuals reporting an average abstinence period of 13 years for marijuana and other non-marijuana drugs. In fact, the only significant findings involved alcohol misuse among men with higher rates and earlier onset of CVD among problem drinkers. Neither use or diagnoses of misuse for marijuana and other non-marijuana drugs predicted health problems in this sample. The average of the sample was 41 years (SD = 7.60) with 76% of the subjects below the age of 46 years.
In addition to objective measures of health status, studies have compared perceived health status and healthcare utilization among substance users. The findings have been mixed. In a study comparing heavy marijuana users to a comparison sample of nonusers, Bourque14 failed to show significant differences in perceived health problems. More recently, Eisen et al15 used a twin control design to compare health problems in a sample of adult twins. Rates of self-reported health problems were compared between twins discordant (i.e., one twin used and the co-twin did not use) for marijuana use. The co-twin design controls for familial influences (e.g., genetic or environmental) on health status. Subjects had been abstinent for an average period of 20 years and did not report other non-marijuana drug use. The average age of the participants was 46 years (SD=3.2). Outcome measures included perceived impact of health problems on daily functioning and health service utilization. No differences were found for health services utilization or perceived health quality. This study did not report on prevalence rates for diseases or marijuana diagnosis. A report by Falck et al16 showed significant associations between crack cocaine diagnosis, but not amount of use, and perceived poorer health status. Finally, De Alba et al 17 report lower perceived health among patients admitted to a detoxification unit.
In this paper, we examined the associations between substance misuse and 5-year incidence rates of emergent health problems. We predicted substance misuse would be associated with higher rates of disease. To test our hypotheses, we identified a group of individuals that did not report health problems at the previous interview but did so at a 5-year follow-up interview. We then tested associations between incidence rates (i.e., new cases) and lifetime substance misuse of alcohol, tobacco, marijuana, and other non-marijuana drugs. This study has several advantages over prior research on the health consequences of substance misuse. First, repeated assessment allows for more precise evaluation of substance-induced health problems because the within-subject design controls for individual factors (e.g., lifestyle choices) that may influence disease independent of substance use. Second, the subjects were in middle adulthood at the time of initial assessment and had not reached the age of risk for most of the diseases examined making it possible to evaluate new occurrences of disease within a defined period of time. This study is well equipped to examine whether substance misuse accelerates the natural disease process by controlling for baseline health status. Finally, we examined both perceived health outcomes and service utilization to evaluate possible under treatment of a high risk group of individuals.
Methods
Sample Description
The adoptees for the prior study wave (i.e., Wave 1) were originally interviewed as part of a follow-up study of previous participants (Total n = 772) from five separate studies that took place between 1975 and 1994 (for a description of methods see18). Adoptees were originally selected by the absence or presence of biological parent diagnoses (e.g., substance misuse, antisocial personality, and criminality). Approximately half were recruited due to the presence of a diagnosis in at least one birth parent, while the remaining participants were selected due to the absence of any known psychopathology in either parent. The average age at adoption was 2.42 months (SD = 6.39) with 71% of the adoptees placed with the adoptive parents before one month of age and 82% before 3 months of age. Adoptive parents were predominantly upper (20%) and middle class (76%). Average adoptee household income was $40,000 to $49,999 per year. Subjects were predominantly White, non-Hispanic (N = 304, 94%) with the remainder of the participants African American, non-Hispanic (N = 7, 2%), African American, Hispanic (N = 2, ∼1%), Caucasian, Hispanic (N = 8, 3%), or mixed race (N = 2, ∼1%). For the continuation (Wave 2), we recruited from a subset of participants with available school achievement data on file to examine the cognitive impact of substance use (N = 463).
We successfully updated substance use histories, psychiatric problems, and health problems, as well as administered a through cognitive assessment for 330 adoptees. Average age at follow-up was 44.32 years (SD = 7.28) with an average of 5 years (SD = 1.34) between assessments. Mean education was 14.19 years (SD = 1.84). Of those subjects who failed to participate, we were unable to locate 38 (8%), 5 were deceased (1%), 5 (1%) were in prison, and 84 (18%) declined participation. Comparing participants and non-participants, we found no differences on biological parent antisocial or alcohol background (χ2(1) = 0.01, p = .91 and χ2(1) = 2.39, p = .12, respectively). Recruitment status was also not associated with participant diagnoses for alcohol (χ2(1) = 0.05, p = .82), marijuana (χ2(1) = 1.54, p = .51), or non-marijuana drugs (χ2(1) = 0.80, p = .37), antisocial personality disorder (χ2(1) = 0.24, p = .62), or Major Depressive Disorder (χ2(1) = 1.25, p = .26). Tobacco abuse/dependence was slightly lower among participants (64% versus 74%, χ2(1) = 4.06, p = .04).
Measures
Demographic information, medical history, and Axis I substance abuse/dependence diagnoses were collected using the Semi-Structured Assessment for the Genetics of Alcoholism SSAGA-II,19 (see Table 1). Medical diagnoses were classified into the presence of any disorder within the following categories: 1) cardiovascular disease (e.g., high blood pressure, stroke, or heart disease) and 2) metabolic disorders (e.g., liver disease, thyroid disease, diabetes, or cancer). In order to examine substance-induced health problems, participants reporting onset of health problems prior to substance misuse were omitted from the analyses (n = 21). Lifetime substance abuse/dependence was determined using DSM-IV criteria. Finally, subjects reported on current health status, number of visits to the ER, and number of hospitalizations.
Table 1. Descriptives for Study Variables.
| Study Variables | Total Sample (n=309) |
Men (n=130) |
Women (n=179) |
p* | |||
|---|---|---|---|---|---|---|---|
| Demographics | |||||||
| Current Age (M, SD) | 44.32 | 7.28 | 44.55 | 7.30 | 44.15 | 7.29 | .638 |
| Education (M, SD) | 14.20 | 1.76 | 14.02 | 1.87 | 14.35 | 1.76 | .113 |
| Number of ER visits (M, SD) | 4.09 | 7. 23 | 5.30 | 8.34 | 3.21 | 6.18 | .001 |
| Poor Perceived Health (n, %) | 27 | 9 | 13 | 10 | 14 | 8 | .503 |
| Cardiovascular Disease (n, %) | 83 | 27 | 45 | 35 | 38 | 21 | .009 |
| High Blood Pressure (n) | 76 | 42 | 34 | .007 | |||
| Stroke (n) | 7 | 4 | 3 | .414 | |||
| Heart Disease (n) | 12 | 9 | 3 | .018 | |||
| Metabolic Disease (n, %) | 72 | 23 | 23 | 18 | 49 | 27 | .047 |
| Liver Disease (n) | 12 | 6 | 6 | .570 | |||
| Thyroid Disease (n) | 33 | 8 | 25 | .028 | |||
| Diabetes (n) | 21 | 7 | 14 | .401 | |||
| Cancer (n) | 22 | 7 | 15 | .312 | |||
| Substance Diagnoses | |||||||
| Alcohol (n, %) | 146 | 47 | 74 | 57 | 72 | 40 | .004 |
| Tobacco (n, %) | 74 | 24 | 28 | 22 | 46 | 26 | .398 |
| Marijuana (n, %) | 44 | 17 | 25 | 19 | 19 | 11 | .032 |
| Other Non-Marijuana Drugs (n, %) | 38 | 12 | 26 | 20 | 12 | 7 | .001 |
| Length of Substance Use (years) | |||||||
| Alcohol (n, %)a | 233 | 24.69 (7.41) | 100 | 25.65 (8.24) | 133 | 23.96 (6.65) | .085 |
| Tobacco (n, %) | 264 | 17.63 (13.52) | 106 | 19.82 (14.25) | 158 | 16.16 (12.84) | .031 |
| Marijuana (n, M(SD)) | 198 | 10.95 (10.36) | 89 | 13.24 (10.90) | 109 | 9.09 (9.55) | .005 |
| Other Non-MJ Drugs (years) (n, M(SD)) | 117 | 10.03 (8.80) | 58 | 12.05 (8.50) | 59 | 8.05 (8.71) | .013 |
| Abstinence from Substance Use (years) | |||||||
| Alcohol (n, %) | 300 | 1.78 (5.55) | 125 | 1.92 (5.93) | 175 | 1.67 (5.27) | .706 |
| Tobacco (n, %) | 264 | 12.65 (13.15) | 106 | 11.84 (13.42) | 158 | 13.20 (12.97) | .412 |
| Marijuana (n, M(SD)) | 202 | 15.78 (10.38) | 93 | 14.44 (10.64) | 109 | 16.93 (10.06) | .090 |
| Other Non-MJ Drugs (years) (n, M(SD)) | 128 | 16.83 (8.39) | 65 | 15.22 (8.60) | 63 | 18.49 (7.91) | .027 |
p-value corresponds to sex differences.
Onset age of alcohol use was age first drank regularly (at least once a month). Twenty-eight subjects reported never drinking regularly. Differences in numbers reflect missing age of onset data.
MJ = marijuana.
Analyses
Baseline and new occurrences of health diagnoses were identified at each wave of study (1999-2003 and 2004-2008, respectively). To examine baseline differences, we contrasted subjects with health problems at baseline with subjects that did not report a health problem at baseline. To compare rates of new occurrences of health problems, we compared subjects with health problems at follow-up with subjects that did not report any health problems at both assessments (i.e., subjects reporting health problems at baseline were excluded). Logistic regression was used to estimate adjusted odds ratios and their 95% confidence interval. Demographics (e.g., sex, current age, education and income) were included as covariates. Finally, Cox Regression survival analysis was used to examine substance diagnoses and age of onset for health problems.
Results
Descriptives
We examined sex differences in length of exposure to all substance (see Table 1). Men reported significantly longer use of marijuana and other non-marijuana drugs than women (t (196) = 2.85, p = .005 and t (115) = 2.51, p = .013, respectively). No sex differences were found for length of abstinence from marijuana (t (200) = -1.71, p = .090), but women reported long abstinence periods for other non-marijuana drugs than men (t (126) = -2.24, p = .027) (see Table 1). Twenty-nine subjects reported using marijuana in the past year. No one reported current use (within the past year) of other non-marijuana drugs. Men reported using tobacco significantly longer than women (t (262) = 2.17, p = .031), but no difference was found for length of abstinence (t (262) = -0.82, p = .412). Finally, men and women did not differ for length of alcohol use (t (231) = 1.73, p = .085) or abstinence (t (298) = 0.378, p = .706). Cross-tabulations between health problems and substance diagnoses are presented in Table 2.
Table 2. Column Percentages for Health Diagnoses by Substance Abuse/Dependence Diagnoses.
| Cardiovascular Disease | Metabolic Disease | ||||||
|---|---|---|---|---|---|---|---|
| Diagnoses | Row Totals | None | Baseline | New | None | Baseline | New |
| Alcohol | |||||||
| Present | 146 (47%) | 105 (46%) | 20 (42%) | 21 (40%) | 113 (48%) | 19 (48%) | 14 (44%) |
| Absent | 163 (53%) | 121 (54%) | 28 (58%) | 14 (60%) | 124 (52%) | 21 (52%) | 18 (56%) |
| Tobacco | |||||||
| Present | 74 (24%) | 54 (24%) | 9 (19%) | 11 (31%) | 54 (23%) | 12 (30%) | 8 (25%) |
| Absent | 235 (76%) | 172 (76%) | 39 (81%) | 24 (69%) | 183 (77%) | 28 (70%) | 24 (75%) |
| Marijuana | |||||||
| Present | 44 (14%) | 25 (11%) | 9 (19%) | 10 (29%) | 28 (12%) | 10 (25%) | 6 (19%) |
| Absent | 265 (86%) | 201 (89%) | 39 (81%) | 25 (71%) | 209 (88%) | 30 (75%) | 26 (81%) |
| Other Non-MJ Drugs | |||||||
| Present | 38 (12%) | 22 (10%) | 8 (17%) | 8 (23%) | 23 (10%) | 7 (18%) | 8 (25%) |
| Absent | 271 (88%) | 204 (90%) | 40 (83%) | 27 (77%) | 214 (90%) | 33 (82%) | 24 (75%) |
| Column Totals | 309 | 226 | 48 | 35 | 237 | 40 | 32 |
Baseline = health problems present at initial assessment. New Occurrences = health problems present at 5-year follow-up but not at baseline. MJ = marijuana. Similar superscripts denote significant differences.
Multivariate Analyses
Subjects that did not report health problems at baseline or follow-up were designated as the comparison group in the logistic regressions (see Table 3). The models controlled for demographics (e.g., sex, current age, and education). We also examined sex by substance diagnosis interactions for CVD and metabolic disease.
Table 3. Adjusted Odds Ratios (A.O.R.) from Logistic Regressions Predicting Health Problems from Substance Misuse Diagnoses.
| Cardiovascular Disease | Metabolic Disease | |||
|---|---|---|---|---|
| Baseline | New Occurrences | Baseline | New Occurrences | |
| A.O.R. (95% CI) | A.O.R. (95% CI) | A.O.R. (95% CI) | A.O.R. (95% CI) | |
| Alcohol | - | 2.13 (0.96, 4.76) | 1.30 (0.64, 2.65) | 1.02 (0.46, 2.26) |
| Men | 2.40 (0.85, 6.79) | - | - | - |
| Women | 0.30 (0.10, 0.96) † | - | - | - |
| Tobacco | 0.64 (0.28, 1.46) | 1.54 (0.66, 3.57) | 1.43 (0.66, 3.09) | 0.86 (0.34, 2.15) |
| Marijuana | 1.81 (0.75, 4.37) | 3.24 (1.25, 8.41)† | - | 2.12 (0.75, 5.94) |
| Men | - | - | 20.25 (3.28, 125.07) § | - |
| Women | - | - | 1.05 (0.28, 3.97) | - |
| Other MJ Drugs | 1.77 (0.70, 4.52) | 3.03 (1.13, 8.10) † | - | 4.14 (1.53, 11.21) ‡ |
| Men | - | - | 24.53 (3.47, 173.46) § | - |
| Women | - | - | 0.46 (0.06, 3.79) | - |
Covariates included sex, current age, and education. Baseline = health problems present at initial assessment. New Occurrences = health problems present at 5-year follow-up but not at baseline. MJ = marijuana. A.O.R. represents odds ratios adjusted for participants' current age, sex, and education.
p < .05.
p < .01.
p < .001.
Cardiovascular Disease
Baseline Health Problems
The interaction between sex and alcohol abuse or dependence was significant for baseline CVD (Wald = 7.58, df = 1, A.O.R. = 0.12, p = .006) (see Table 3). A lifetime diagnosis of alcohol problems was associated with a lower risk of baseline CVD among women (Wald = 4.15, df = 1, p = .034) but unassociated with CVD among men (Wald = 2.45, df = 1, p = .099). Tobacco, marijuana and non-marijuana drug diagnoses did not predict baseline CVD (p > .05).
New Occurrences of Health Problems
Diagnoses for alcohol and tobacco abuse/dependence did not predict new cases of CVD (p > .05). A higher incidence of CVD was found among subjects diagnosed with marijuana dependence (Wald = 5.84, df = 1, p = .016) (see Table 3). A lifetime diagnosis of other non-marijuana drug abuse/dependence also predicted significantly higher rates of new cases of CVD (Wald = 4.89, df = 1, p = .027). Because of the high overlap between marijuana and other non-marijuana drug abuse/dependence, we compared rates of new occurrences of CVD between individuals reporting none, one or two diagnoses (Note. The logistic regression failed to converge when the diagnoses were entered simultaneously). The chi-square was significant (χ2 (df = 2, N = 261) = 9.97, p < .01). The incidence of CVD was as follows: no diagnosis (6%), single diagnosis (21%), and dual diagnosis (40%).
Metabolic Disease
Baseline Health Problems
Alcohol and tobacco abuse/dependence did not significantly predict baseline metabolic disease (p > .05). A significant interaction between sex and marijuana dependence was found for baseline metabolic disease (Wald = 5.99, df = 1, p = .014) with higher rates of disease among men with a diagnosis (Wald = 10.48, df = 1, p = .001) but not women (Wald = 1.05, df = 1, p = .948) (see Table 3). The interaction between sex and diagnosis was also significant for other non-marijuana drug diagnoses (Wald = 6.69, df = 1, p = .010) with a significant main effect for men (Wald = 10.28, df = 1, p = .001) but not women (Wald = 0.53, df = 1, p = .467). Again, we compared baseline rates of metabolic disease among individuals with no diagnosis, a single diagnosis, and dual diagnoses. The comparison was significant (χ2 (df = 2, N = 117) = 29.72, p < .001). The highest rate of baseline metabolic disease (50%) was found among men meeting criteria for a dual diagnosis (marijuana plus other non-MJ drugs). None of the men with a single diagnosis reported metabolic disease and only 4% of men not meeting diagnostic criteria for abuse or dependence reported baseline metabolic disease.
New Occurrences of Health Problems
The only significant predictor of new occurrences of metabolic disease was other non-marijuana drug abuse/dependence (see Table 3). Higher rates of new cases of metabolic disease was found among men and women having a diagnosis (Wald = 7.81, df = 1, p = .005) (see Table 3).
Cox Regression Analyses
Cardiovascular Disease
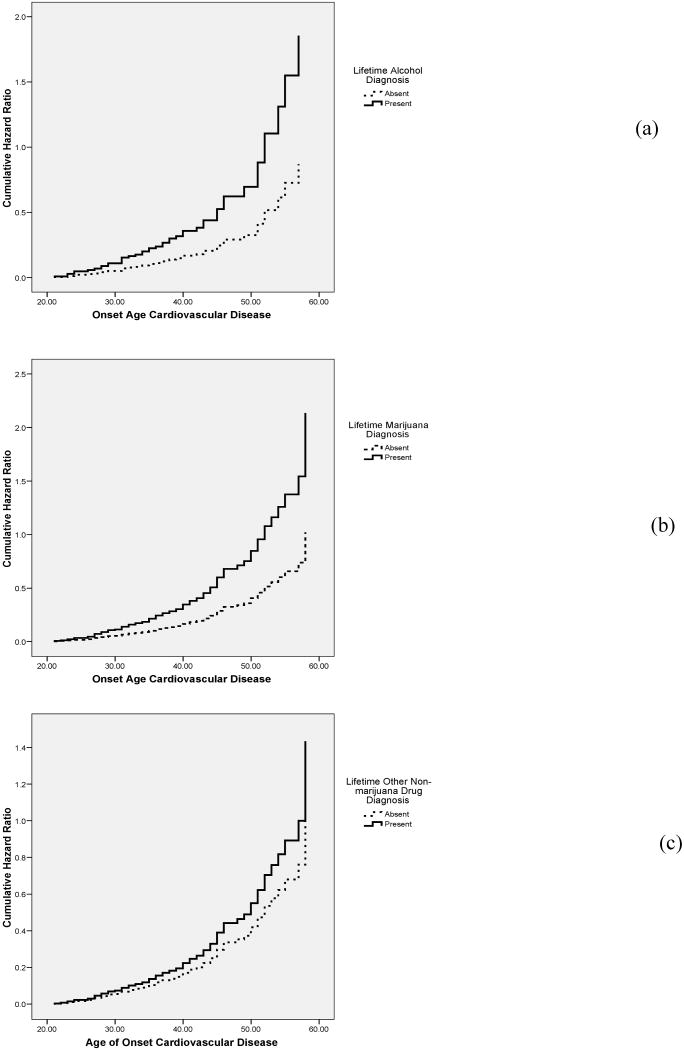
The interaction between sex and an alcohol diagnosis was significant for CVD (Wald = 7.34, df = 1, p = .007); therefore, the survival analysis was analyzed separately for men and women (see Table 4). Men, but not women, reported earlier onset of CVD disease when diagnosed with alcohol problems (see Figure 1(a)). Tobacco diagnosis was not significantly associated with age of onset for CVD (Wald = 0.04, df = 1, p = 1.11).
Table 4. Cox Regression Survival Analysis Predicting Age of Onset for Cardiovascular and Metabolic Disease.
| Cardiovascular Disease | Metabolic Disease | |||||
|---|---|---|---|---|---|---|
| Predictor | Hazard Ratio | 95% CI | p value | Hazard Ratio | 95% CI | p value |
| Alcohol | 1.14 | 0.70, 1.85 | .601 | |||
| Men | 2.13 | 1.09, 4.17 | .027 | - | - | - |
| Women | 0.54 | 0.25,1.18 | .122 | - | - | - |
| Tobacco | 0.85 | 0.51, 1.43 | .544 | 0.98 | 0.58, 1.68 | .947 |
| Marijuana | 1.78 | 1.03, 3.06 | .037 | |||
| Men | - | - | - | 4.89 | 2.03, 11.78 | <.001 |
| Women | - | - | - | 0.92 | 0.33, 2.59 | .880 |
| Other Non-Marijuana Drugs | 1.83 | 1.03, 3.24 | .038 | |||
| Men | - | - | - | 8.20 | 3.12, 21.51 | <.001 |
| Women | - | - | - | 0.65 | 0.16, 2.72 | .559 |
Covariates included sex (for main effects models), current age, and years of education.
Figure 1.
Age of onset for cardiovascular disease (CVD) by substance diagnosis. (1a) Onset age of CVD by alcohol diagnosis for men. (1b) Onset age of CVD by marijuana diagnosis for men and women combined. (1c) Onset age of CVD by other non-marijuana drug diagnosis for men and women combined.
The interactions between sex and substance diagnosis was not significant for marijuana (Wald = 1.79, df = 1, p = .181) or other non-marijuana drugs (Wald = 1.42, df = 1, p = .234) (see Table 4). However, men and women with marijuana or other non-marijuana drug diagnoses reported earlier onset of CVD than individuals with no diagnosis (see Figures 1(b) and 1(c), respectively). In order to examine whether the onset of CVD occurred during active use, we computed the difference between age at last use and age of onset for CVD. On average, men and women reported last using marijuana or other non-marijuana drugs 7 years before the onset of CVD (SD = 11.50, Median = -6.00) with 74% ceasing use before illness onset.
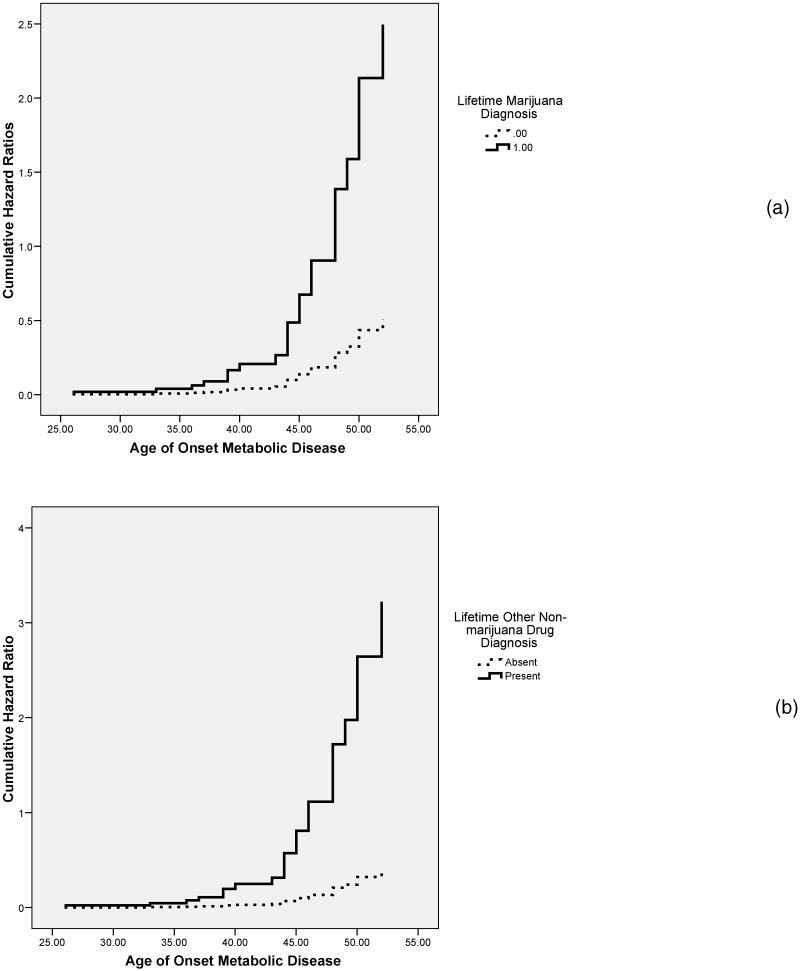
Metabolic Disease
Alcohol and tobacco misuse did not predict age of onset for metabolic disease (Wald = 0.27, df = 1, p = .601 and Wald = 0.004, df = 1, p = .947, respectively) (see Table 4). Significant differences between men and women were found for the association between marijuana (Interaction: Wald = 5.52, df = 1, p = .019) and other marijuana drug diagnoses and metabolic disease (Interaction: Wald = 6.87, df = 1, p = .009). Metabolic disease was diagnosed earlier among men reporting lifetime misuse of marijuana (Wald = 12.53, df = 1, p < .001) or non-marijuana drugs (Wald = 18.26, df = 1, p < .001) (see Figures 2(a) and 2(b)). Neither association was significant for women (Marijuana: Wald = .02, df = 1, p = .880 and Non-marijuana drugs: Wald = 0.34, df = 1, p = .654). As with CVD, 74% of men reported quitting active use of illicit drugs prior to the onset of metabolic disease (M = -6.65, SD = 13.47, Median = -7.50).
Figure 2.
Age of onset for metabolic disease by substance diagnosis. (2a) Onset age of metabolic disease by marijuana diagnosis for men. (2b) Onset age of metabolic disease by other non-marijuana drug diagnosis for men.
Perceived Health Problems and Service Utilization
Our final set of analyses examined the impact of substance diagnoses on health services utilization and perceived health (see Table 5). Subjects reported on the number of lifetime emergency room (ER) visits and perceived current health. Men and subjects diagnosed with alcohol misuse reported a significantly higher number of ER visits. A trend was found for marijuana and other non-marijuana drugs with more ER visits among subjects reporting misuse (see Table 5). Subjects with marijuana or other non-marijuana drug diagnoses reported significantly poorer health with nearly a quarter of subjects with a substance misuse diagnosis viewing their current health status as poor compared to 8% of subjects without a diagnosis.
Table 5. Health Service Utilization and Perceived Health by Demographics and Substance Diagnosis.
| ER Visits* | Current Poor Health† | ||||||
|---|---|---|---|---|---|---|---|
| N | M | SD | p value | N | % | p value | |
| Sex | .001 | .503 | |||||
| Male | 130 | 5.30 | 8.34 | 130 | 10% | ||
| Female | 179 | 3.21 | 6.18 | 179 | 8% | ||
| Alcohol | .006 | .530 | |||||
| Absent | 170 | 3.18 | 5.15 | 15 | 9% | ||
| Present | 156 | 5.17 | 8.89 | 17 | 10% | ||
| Tobacco | .242 | .058 | |||||
| Absent | 248 | 3.70 | 6.19 | 20 | 8% | ||
| Present | 78 | 5.50 | 9.81 | 12 | 15% | ||
| Marijuana | .059 | .020 | |||||
| Absent | 279 | 3.69 | 5.69 | 23 | 8% | ||
| Present | 47 | 6.74 | 12.93 | 9 | 19% | ||
| Non-Marijuana Drugs | .066 | .001 | |||||
| Absent | 284 | 3.83 | 6.72 | 22 | 8% | ||
| Present | 42 | 6.14 | 9.97 | 10 | 24% | ||
Mann-Whitney U tests of association.
Chi-square analysis.
ER = Emergency Room. n = sample size. M = mean. SD = standard deviation.
Discussion
The present paper examined 5-year incidence rates of CVD and metabolic disease among individuals reporting lifetime substance abuse or dependence. Associations between lifetime diagnoses of substance misuse and health problems were tested for both baseline and new cases of disease. Data collection was completed in two phases. Baseline rates of disease were estimated from the first assessment and new cases of disease were those health events that occurred in the 5-year interval between the first and second phases of data collection.
We found few significant associations between lifetime alcohol and tobacco diagnoses and baseline health problems. Among women, a lifetime diagnosis of alcohol abuse or dependence was protective with fewer cases of CVD among women with a diagnosis. Among men, CVD had an earlier onset in the presence of alcohol abuse/dependence even though having a lifetime alcohol diagnosis did not predict the occurrence of CVD. Although initially counterintuitive, the protective effect observed among women and absence of effect observed among men could be a function of reduced consumption with age. Unfortunately, we did not have a comprehensive assessment of current drinking at follow-up. The only questions asked were the number of days drank and number of drinks consumed on an average day during the week of heaviest drinking in the preceding six months. The modal number of days drank was one and the modal number of drinks was two for men and women. Therefore, current levels of consumption were low despite prior diagnoses of alcohol abuse/dependence. Finally, tobacco dependence was not associated with health problems for men or women.
Significant associations were found between illicit drugs (e.g., marijuana or other no-marijuana drugs) and health problems. Men diagnosed with lifetime abuse or dependence on illicit drugs were more likely to be diagnosed with a metabolic disease at baseline. This increased occurrence was primarily due to men with dual drug diagnoses (i.e., marijuana plus other non-marijuana drug abuse/dependence). Significantly higher 5-year incidence rates of CVD and metabolic disease were found among men and women reporting lifetime marijuana or other non-marijuana drug misuse. Again, subjects having a dual diagnosis were more likely to report new cases of disease. CVD was also diagnosed earlier for men and women reporting illicit drug abuse/dependence and metabolic disease occurred earlier among men with a diagnosis of illicit drug abuse/dependence.
Our findings have multiple implications for predicting the future health of individuals with diagnosable substance abuse/dependence. The first implication deals with recommendations of moderate alcohol consumption in the prevention of CVD by the American Medical Association (AMA). The association between alcohol consumption and health problems is typically characterized as quadratic with low and high consumption characterized as not protective against disease and moderate drinking characterized as reducing risk for disease20, 21; although contradictory evidence has also been reported suggesting a protective effect of heavy drinking among older individuals22. Furthermore, certain patterns of drinking (e.g., binge drinking versus regular consumption) have been shown to have differential effects on health with greater protective effects observed among steady drinkers20, 23. Our data is limited in directly testing the AMA recommendation due to the fact that we relied on diagnoses determined at baseline and current alcohol consumption could not be adequately quantified at follow-up. The reliance on a single lifetime assessment of alcohol diagnosis could underestimate the harmful effects of alcohol consumption in this sample23. Therefore, our findings can not speak directly to the recommendation of the AMA that moderate alcohol intake reduces certain health risks. We can suggest, however, that a lifetime diagnosis of alcohol abuse or dependence is not deterministic of future health problems24 when current consumption is low.
The second implication is the predictive utility of lifetime diagnoses of tobacco dependence independent of current smoking exposure in predicting health status. We failed to find significant associations between lifetime tobacco dependence and CVD or metabolic disease. The lack of significant findings should not be interpreted as minimizing the effects of tobacco dependence on health, but rather that exposure independent of a dependence diagnosis may carry greater health risks. As with alcohol, the SSAGA-II focuses on collecting information about use during periods of heaviest use. Thus, current exposure could not be determined from these data. An additional caveat is the use of smokeless tobacco which has also been shown to influence cardiovascular health25-27. As the data are currently analyzed, individuals reporting use of smokeless tobacco are included in the non-dependent comparison group thereby possibly minimizing group differences. Conversely, individuals diagnosed with lifetime tobacco dependence but who are currently non-smokers are grouped in the positive group which may further reduce differences due to the recovery from smoking-related health problems upon cessation28-30.
The final implication of our data is the role of a dual (polydrug) diagnosis in predicting health problems. Men and women were equally susceptible to the effects of illicit drug use on CVD both in terms of the emergence of problems and the onset of problems at an earlier age. These findings suggest that women might be more susceptible to the cardiovascular effects of illicit drugs at lower levels of exposure due to the significant differences in exposure length and prevalence of substance diagnoses between men and women. This same interpretation does not hold true for metabolic disease in which men were more affected by polydrug use than women. Although formal statistical testing could not be conducted liver disease was the metabolic condition most common among men endorsing illicit drug abuse/dependence. Cocaine (the drug most commonly reported by our subjects) targets the liver31 and alcohol intensifies this effect32. It is possible that men are more likely to engage in polydrug use, including combining other drug use with alcohol, which results in greater insult to physical health. Finally, unlike the possible transient effects of alcohol and tobacco, polydrug abuse/dependence appears to carry health risks even after substantial periods of abstinence.
Health Services Utilization
Subjects with alcohol problems reported more frequent visits to the emergency room. In contrast, diagnoses for marijuana or other non-marijuana drugs were not associated with health service utilization despite poorer subjective ratings of current health and higher rates of objective health diagnoses. The disparity between presence of health problems and cost utilization of healthcare is not new in the substance abuse literature33-35. These data suggest that probing about past substance use history may be necessary to ensure individuals with prior misuse actively pursue preventive care especially among individuals reporting polydrug abuse/dependence.
Limitations
The current study was limited by sample size which precluded examination of specific health problems rather than classes of diseases (e.g., CVD, metabolic). CVD consisted primarily of high blood pressure (92%); a major (although nonspecific) precursor to heart disease and other systemic disease (e.g., kidney failure). Metabolic disease was less clear cut consisting predominantly of thyroid disease (46%) followed by liver disease (31%), and diabetes (29%). Similarly, the sample size did not allow for separation of marijuana from other-non-marijuana effects on health problems with roughly half of either reporting use of the other substance nor were we able to examine specific classes of drugs. Men reported using an average of six different non-marijuana drugs compared to women who reported using an average of four different classes of drugs. It is not possible to determine whether these drugs were taken concurrently, simultaneously, or at different times throughout the period of use. Each pattern of use may have different consequences on health that we were not able to examine with these data. Similar confounds were present between alcohol and tobacco. Furthermore, there were only seven women meeting diagnostic criteria for illicit drug use limiting informative analyses for women. The information collected about health service utilization was rudimentary at best. Non-emergent care was not probed so information about current preventive efforts was not available.
Summary
Analyses presented above support our proposition that individuals reporting previous substance misuse develop significantly higher rates of emergent health problems within a shorter period of time. These health risks remain even after long periods of abstinence suggesting physicians, including those in emergent care settings, should inquire about prior substance use33. Our data also suggest that longitudinal studies with long-term follow-ups may be the most effective and sensitive approach to characterizing substance-induced health problems; especially for the detection of precursors to more serious and irreversible health problems. Future studies should utilize well-defined samples comprehensive in their assessments of all substance use, current and past, to examine physiological markers associated with acute substance misuse7, 9, 36, 37 and determine whether the observed changes persist among individuals no longer actively using the substance.
Acknowledgments
Funding Source: National Institutes on Drug Abuse (NIDA) grant # R01 DA005821, Gene × Environment Interactions in the Development of Drug Abuse.
References
- 1.Tetrault JM, Crothers K, Moore BA, Mehra R, Concato J, Fiellin DA. Effects of marijuana smoking on pulmonary function and respiratory complications: a systematic review. Arch Intern Med. 2007;167:221–8. doi: 10.1001/archinte.167.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moore BA, Augustson EM, Moser RP, Budney AJ. Respiratory effects of marijuana and tobacco use in a U.S. sample. J Gen Intern Med. 2005;20:33–7. doi: 10.1111/j.1525-1497.2004.40081.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tashkin DP, Baldwin GC, Sarafian T, Dubinett S, Roth MD. Respiratory and immunologic consequences of marijuana smoking. J Clin Pharmacol. 2002;42:71S–81S. doi: 10.1002/j.1552-4604.2002.tb06006.x. [DOI] [PubMed] [Google Scholar]
- 4.Mehra R, Moore BA, Crothers K, Tetrault J, Fiellin DA. The association between marijuana smoking and lung cancer: a systematic review. Arch Intern Med. 2006;166:1359–67. doi: 10.1001/archinte.166.13.1359. [DOI] [PubMed] [Google Scholar]
- 5.Gaziano JM. Marijuana use among those at risk for cardiovascular events. Am Heart J. 2008;155:395–6. doi: 10.1016/j.ahj.2007.12.016. [DOI] [PubMed] [Google Scholar]
- 6.Aryana A, Williams MA. Marijuana as a trigger of cardiovascular events: speculation or scientific certainty? Int J Cardiol. 2007;118:141–4. doi: 10.1016/j.ijcard.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Sidney S. Cardiovascular consequences of marijuana use. J Clin Pharmacol. 2002;42:64S–70S. doi: 10.1002/j.1552-4604.2002.tb06005.x. [DOI] [PubMed] [Google Scholar]
- 8.Afonso L, Mohammad T, Thatai D. Crack whips the heart: a review of the cardiovascular toxicity of cocaine. Am J Cardiol. 2007;100:1040–3. doi: 10.1016/j.amjcard.2007.04.049. [DOI] [PubMed] [Google Scholar]
- 9.Velasquez EM, Anand RC, Newman WP, 3rd, Richard SS, Glancy DL. Cardiovascular complications associated with cocaine use. J La State Med Soc. 2004;156:302–10. quiz 311. [PubMed] [Google Scholar]
- 10.Herning RI, Better W, Cadet JL. EEG of chronic marijuana users during abstinence: relationship to years of marijuana use, cerebral blood flow and thyroid function. Clin Neurophysiol. 2008;119:321–31. doi: 10.1016/j.clinph.2007.09.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Griffing GT. Endocannabinoids--the brain's own marijuana--may be linked to the metabolic syndrome. Med Gen Med. 2006;8:7. [PMC free article] [PubMed] [Google Scholar]
- 12.Wadland WC, Ferenchick GS. Medical comorbidity in addictive disorders. Psychiatric Clinics of North America. 2004;27:675–687. doi: 10.1016/j.psc.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 13.Spinks R, Caspers K, Langbehn D, Yucuis R, McKirgan LW, Arndt S, Pfalzgraf CJ, Cadoret R. Co-morbid health conditions at mid-life in the Iowa adoptees. Addict Behav. 2007;32:991–1002. doi: 10.1016/j.addbeh.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 14.Bourque L, Tashkin D, Clark V, Schuler R. Demographic and health characteristics of heavy marijuana smokers in Los Angeles County. International Journal of Addiction. 1991;26:739–755. doi: 10.3109/10826089109058917. [DOI] [PubMed] [Google Scholar]
- 15.Eisen S, Chantarujikapong S, Xian H, Lyons M, Toomey R, True W, Scherrer J, Goldberg J, Tsuang M. Does marijuana use have residual adverse effects on self-reported health measures, socio-demographics and quality of life? A monozygotic co-twin control study in men. Addiction. 2002;97:1137–1144. doi: 10.1046/j.1360-0443.2002.00120.x. [DOI] [PubMed] [Google Scholar]
- 16.Falck RS, Wang J, Carlson RG, Siegal HA. Crack-cocaine use and health status as defined by the SF-36. Addict Behav. 2000;25:579–84. doi: 10.1016/s0306-4603(99)00040-4. [DOI] [PubMed] [Google Scholar]
- 17.De Alba I, Samet JH, Saitz R. Burden of medical illness in drug- and alcohol-dependent persons without primary care. Am J Addict. 2004;13:33–45. doi: 10.1080/10550490490265307. [DOI] [PubMed] [Google Scholar]
- 18.Yates W, Cadoret R, Troughton E. The Iowa Adoption Studies: Methods and results. In: LaBuda M, Grigorenko E, editors. On The Way to Individuality: Current Methodological Issues in Behavioral Genetics. Commack, NY: Nova Science Publishers, Inc; 1999. pp. 95–121. [Google Scholar]
- 19.Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI, Jr, Reich T, Schmidt I, Schuckit MA. A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. J Stud Alcohol. 1994;55:149–58. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- 20.Gronbaek M. Factors influencing the relation between alcohol and cardiovascular disease. Curr Opin Lipidol. 2006;17:17–21. doi: 10.1097/01.mol.0000203889.50138.98. [DOI] [PubMed] [Google Scholar]
- 21.Rehm J, Sempos CT, Trevisan M. Alcohol and cardiovascular disease--more than one paradox to consider. Average volume of alcohol consumption, patterns of drinking and risk of coronary heart disease--a review. J Cardiovasc Risk. 2003;10:15–20. doi: 10.1097/01.hjr.0000051961.68260.30. [DOI] [PubMed] [Google Scholar]
- 22.Mukamal KJ, Chung H, Jenny NS, Kuller LH, Longstreth WT, Jr, Mittleman MA, Burke GL, Cushman M, Psaty BM, Siscovick DS. Alcohol consumption and risk of coronary heart disease in older adults: the Cardiovascular Health Study. J Am Geriatr Soc. 2006;54:30–7. doi: 10.1111/j.1532-5415.2005.00561.x. [DOI] [PubMed] [Google Scholar]
- 23.Emberson JR, Shaper AG, Wannamethee SG, Morris RW, Whincup PH. Alcohol intake in middle age and risk of cardiovascular disease and mortality: accounting for intake variation over time. Am J Epidemiol. 2005;161:856–63. doi: 10.1093/aje/kwi111. [DOI] [PubMed] [Google Scholar]
- 24.Friesema IH, Zwietering PJ, Veenstra MY, Knottnerus JA, Garretsen HF, Kester AD, Lemmens PH. The effect of alcohol intake on cardiovascular disease and mortality disappeared after taking lifetime drinking and covariates into account. Alcohol Clin Exp Res. 2008;32:645–51. doi: 10.1111/j.1530-0277.2007.00612.x. [DOI] [PubMed] [Google Scholar]
- 25.Gupta R, Gurm H, Bartholomew JR. Smokeless tobacco and cardiovascular risk. Arch Intern Med. 2004;164:1845–9. doi: 10.1001/archinte.164.17.1845. [DOI] [PubMed] [Google Scholar]
- 26.Arabi Z. Metabolic and cardiovascular effects of smokeless tobacco. J Cardiometab Syndr. 2006;1:345–50. doi: 10.1111/j.1559-4564.2006.05930.x. [DOI] [PubMed] [Google Scholar]
- 27.Gupta BK, Kaushik A, Panwar RB, Chaddha VS, Nayak KC, Singh VB, Gupta R, Raja S. Cardiovascular risk factors in tobacco-chewers: a controlled study. J Assoc Physicians India. 2007;55:27–31. [PubMed] [Google Scholar]
- 28.Bakhru A, Erlinger TP. Smoking cessation and cardiovascular disease risk factors: results from the Third National Health and Nutrition Examination Survey. PLoS Med. 2005;2:e160. doi: 10.1371/journal.pmed.0020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bullen C. Impact of tobacco smoking and smoking cessation on cardiovascular risk and disease. Expert Rev Cardiovasc Ther. 2008;6:883–95. doi: 10.1586/14779072.6.6.883. [DOI] [PubMed] [Google Scholar]
- 30.Gratziou C. Respiratory, cardiovascular and other physiological consequences of smoking cessation. Curr Med Res Opin. 2009;25:535–45. doi: 10.1185/03007990802707642. [DOI] [PubMed] [Google Scholar]
- 31.Wang JF, Ren X, DeAngelis J, Min J, Zhang Y, Hampton TG, Amende I, Morgan JP. Differential patterns of cocaine-induced organ toxicity in murine heart versus liver. Exp Biol Med (Maywood) 2001;226:52–60. doi: 10.1177/153537020122600108. [DOI] [PubMed] [Google Scholar]
- 32.Roberts SM, Harbison RD, James RC. Inhibition by ethanol of the metabolism of cocaine to benzoylecgonine and ecgonine methyl ester in mouse and human liver. Drug Metab Dispos. 1993;21:537–41. [PubMed] [Google Scholar]
- 33.Alexandre PK, French MT, Matzger H, Weisner C. Addiction treatment history, medical services utilization, and cost: a longitudinal analysis of problem drinkers. J Addict Dis. 2006;25:105–20. doi: 10.1300/J069v25n01_13. [DOI] [PubMed] [Google Scholar]
- 34.Druss BG, von Esenwein SA. Improving general medical care for persons with mental and addictive disorders: systematic review. Gen Hosp Psychiatry. 2006;28:145–53. doi: 10.1016/j.genhosppsych.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 35.Friedmann PD, Hendrickson JC, Gerstein DR, Zhang Z, Stein MD. Do mechanisms that link addiction treatment patients to primary care influence subsequent utilization of emergency and hospital care? Med Care. 2006;44:8–15. doi: 10.1097/01.mlr.0000188913.50489.77. [DOI] [PubMed] [Google Scholar]
- 36.Jones RT. Cardiovascular system effects of marijuana. J Clin Pharmacol. 2002;42:58S–63S. doi: 10.1002/j.1552-4604.2002.tb06004.x. [DOI] [PubMed] [Google Scholar]
- 37.Ponto LL, O'Leary DS, Koeppel J, Block RI, Watkins GL, Richmond JC, Ward CA, Clermont DA, Schmitt BA, Hichwa RD. Effect of acute marijuana on cardiovascular function and central nervous system pharmacokinetics of [(15)O]water: effect in occasional and chronic users. J Clin Pharmacol. 2004;44:751–66. doi: 10.1177/0091270004265699. [DOI] [PubMed] [Google Scholar]