Abstract
Background and Objectives
Longitudinal studies have found evidence of associations between coronary heart disease and clinical depression. We sought to understand older patients' views regarding relationships between depression and heart disease to facilitate patient-provider communication about heart disease and depression and to lay the groundwork for designing interventions.
Methods
The design was a qualitative study using semi-structured interviews. In all, 33 primary care patients 65 years and over with dysphoria, anhedonia, hopelessness, worthlessness, or sleep disturbance who were taking at least one medication targeting cardiovascular risk factors were interviewed in the office of their primary care clinician. Participants were asked open-ended questions about depression and heart disease and their treatment. A multidisciplinary research team coded the transcripts and identified key themes.
Results
Participants gave clear descriptions of how heart disease can lead to depression and depression can lead to heart disease. Participants supported treating depression immediately in the context of heart disease and generally preferred integrated care.
Conclusions
Depression treatment may be more acceptable if discussed in terms of overall cardiovascular risk. Our results support the integration of depression management with management for risk factors for cardiovascular disease.
Cardiovascular disease is associated with clinical depression, and clinical depression is an independent risk factor for cardiovascular disease.1,2 Given the associations between cardiovascular disease and depression and the prevalence of both in the primary care setting,3 researchers have called for the development of integrated interventions targeting both depression and cardiovascular disease risk in primary care.4,5 To develop an integrated intervention that will be acceptable to patients, we need to understand the ways in which patients conceptualize relationships between depression and heart disease. Evidence suggests that interventions that take into account patient understandings of illness and appropriate treatment may lead to improved outcomes.6,7 Indeed, patients' beliefs have been found to predict help-seeking behavior, evaluation of treatment suitability, treatment choices, and engagement and adherence to depression treatment.8,9 Causal attributions for coronary heart disease are associated with self-ratings of adherence to medical recommendations for behavior change.10
In this qualitative study, we explored patient beliefs about the relationship between depression and heart disease and preferences for treatment. Our study differs from prior work on three levels. First, most prior studies focused either on patients' and family members' beliefs about causes of coronary heart disease11-17 or the causal attributions of depression18-21 and do not comment on the coexistence of the conditions. We were interested in the patients' views regarding the relationship between depression and heart disease. Second, many previous studies examining the identification of depression and coronary heart disease were carried out in hospitals,12, 13,15,16 research institutes, day centers, social clubs,20 or classrooms11,14,20,21 but not in primary care settings. The primary health care setting is pivotal for initial identification and management of depression among older adults.22 Third, previous research has focused on causal attributions for heart disease and outcomes such as adherence,10,23-25 recurrence of myocardial infarction,15,26 functioning,13 and mortality15 but not on how patients' causal attributions are related to suggestions for depression management.
We sought to understand older patients' perspectives regarding the relationship between depression and heart disease to facilitate patient-provider communication and to lay the groundwork for designing integrated interventions. We focused on older patients at risk for cardiovascular disease who were early in the course of depression, since they are representative of older adults who are commonly seen in primary care and of patients at whom an integrated intervention would likely be targeted.
Methods
Sampling Strategy
Patients were recruited from a community-based primary care practice in Philadelphia. Seventy-six patients ages 65 and older with upcoming medical appointments between November 2004 and January 2006 were contacted by telephone and administered a brief screener questionnaire. The screener asked about the presence of dysphoria, anhedonia, hopelessness, worthlessness, and sleep disturbance within 6 months of the interview (these items are associated with suicidal ideation27). Patients with one screening item present who were taking one or more medications targeting a cardiovascular risk factor (eg, a medication for hypertension, hyperlipidemia, or diabetes) were invited to participate in the study. In all, 53 older persons were invited, and 33 (62.3%) agreed to participate in interviews. The research protocols were approved by the University of Pennsylvania Institutional Review Board.
Interview Procedures
We conducted semi-structured interviews with each participant. Interviews were held in the primary care practice and designed to elicit participants' thoughts on depression and heart disease and possible relationships between the conditions. Interviews lasted approximately 60 minutes. Saturation for the themes presented in the results was achieved after 18 interviews. Because we continued to conduct interviews to investigate other themes, we identified additional examples of the themes among the remaining interviews. In total, 30 (90%) of the 33 interviews contained a variant of the themes about particular pathways between depression and heart disease presented. All interviews were taperecorded, transcribed, and entered into QSR N6 text management software for coding and analysis.28
Measurements
We used standard questions to obtain information from participants on age, gender, self-reported ethnicity, education, marital status, and living arrangements. Depression was measured using the Center for Epidemiologic Studies Depression Scale (CES-D), developed by the National Institute of Mental Health for use in studies of depression in community samples.29-35 Information about chronic medical conditions and medications were obtained by self-report.
Data Analysis
Interviews were discussed at weekly meetings with an interdisciplinary team including a medical anthropologist, a geriatrician, and a family physician. Three of the authors read transcripts independently to code for themes about relationships or contrasts between heart disease and depression. We used the constant comparative method,36 taking one piece of data (eg, one theme) and comparing it with all others to identify similarities and differences across transcripts and connections between themes. Through the constant comparative method and discussion among authors, we arrived at consensus and established that the themes presented are representative of transcripts. The pathways between depression and heart disease described in the results reflect these main themes that emerged from the transcripts.
Results
Sample Characteristics
Participants ranged from 65 to 85 years, with an average age of 73 years. Twenty (61%) of the 33 participants were women. Twenty-five (76%) participants self-identified as African American, and eight (24%) self-identified as white. Sociodemographic characteristics of the participants are summarized in Table 1. The mean CES-D score was 11.1 with a standard deviation of 8.8, indicating mild to moderate depressive symptoms.
Table 1.
Characteristics of Persons Participating in Semi-structured Interviews (n=33)
| Sociodemographic Characteristics | |
| Age, mean (SD) | 72.6 (5.2) |
| Women, n (%) | 20 (60.6%) |
| African American, n (%) | 25 (75.8%) |
| Education less than high school, n (%) | 12 (36.4%) |
| Married, n (%) | 13 (39.4%) |
| Lives alone, n (%) | 15 (45.5%) |
| Psychological Status | |
| CES-D (depression) score, mean (SD) | 11.1 (8.8) |
| Taking an antidepressant, n (%) | 5 (15.2%) |
| Medical Comorbidity and Physician Visits | |
| Number of medical conditions, mean (SD) | 4.5 (1.7) |
| Total number of medications, mean (SD) | 6.4 (3.7) |
| Number of medical visits within 6 months, mean (SD) | 2.7 (2.5) |
| Risk Factors for Cardiovascular Disease | |
| Hypertension, n (%) | 25 (75.8%) |
| Hypercholesterolemia, n (%) | 23 (69.7%) |
| Diabetes/high blood sugar, n (%) | 15 (45.5%) |
SD—standard deviation
CES-D—Center for Epidemiologic Studies Depression Scale
Pathways Between Depression and Heart Disease
Heart Disease Leads to Depression
Participants said that heart disease could cause depression through several pathways (Figure 1). Most participants emphasized that heart disease diagnosis could lead directly to depression: “If you been told heart disease…I think it occurs almost immediately.” “You've got this condition [heart disease] and maybe there's no cure…that can cause depression.” Many older adults said that learning they had heart disease led to feelings of doubt, fear of death, loss of control, and helplessness: “…a person with heart disease is going to…experience doubt about whether they are going to live forever.”
Figure 1.
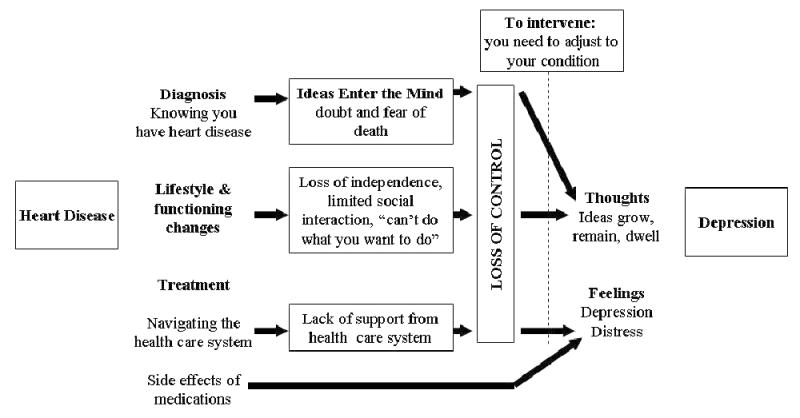
Summary of Older Adults' Descriptions of How Heart Disease Can Lead to Depression
Heart disease can limit daily activities, and participants said such limitations could also lead to depression: “I'm afraid…of being an invalid…not doing the things I want to do.” Participants said that lifestyle changes were most difficult when they threatened independence and ability to engage in personally important activities: “I wouldn't like that [heart disease] too well because I do everything for myself. I cook, I wash, I clean, I go to church and everything.”
Participants said patients should be prepared for side effects from heart medications that can cause depression, and they should manage side effects with their doctors: “I've noticed when I first started taking it [heart medication], they had me on a tablet and a half…they were making me feel down a lot. So I explained that to my doctor and he cut me down to one.” One participant's interactions with the health care system for heart disease contributed to his distress: “The voice mail is a horror. When it's 10 o'clock at night and all of a sudden your blood pressure is going up to 190/110 and you try to call and can't get anybody.” This participant tied his experiences of seeking care for heart disease with a broader sense of losing control, which he and other participants experienced when diagnosed.
Depression Leads to Heart Disease
Older adults described depression as adding a weight to the body (Figure 2) that can lead to heart disease. Participants described depression as a “weight,” as “weighing the body down,” causing a “heavy heart,” “putting too much strain on your heart,” and as a “burden.” Participants understood lasting distressing emotions as leading to increased heart rate and blood pressure: “Don't let it hang on, ‘cause that will cause a heart attack—too much strain on your heart.” Participants also felt that acute episodes of heightened emotion could cause a heart attack: “[Heart disease] has a lot to do with your blood pressure and your emotions running high sometime. Getting excited…could be [cause] a heart attack.”
Figure 2.
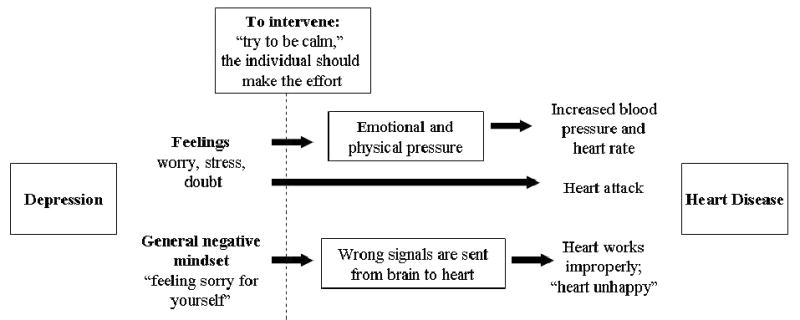
Summary of Older Adults' Descriptions of How Depression Can Lead to Heart Disease
Older adults also described emotions as affecting their physical health through the mind's control over the body: “…your mind is the controller and if your mind is not functioning as well as it should be or could be, then other things in your body might not function.” Another participant stated “I believe that a person who is constantly depressed—that's a very easy case for the heart to go down…If you're happy, your heart is happy” and warned if you got “too depressed” the brain would be sending the “bad, wrong signals to the heart” that could cause a heart attack.
Treatment of Depression and Heart Disease
Participants suggested intervening at particular junctures in the pathways between depression and heart disease (Figures 1 and 2). Participants suggested finding ways to adjust to life with heart disease to prevent depression (Figure 1). Participants said that physicians treating heart disease could help the patient anticipate and ameliorate depression when facing heart problems: “As soon as they find out they have heart disease. If they don't have depression and they find out they have heart disease, someone should start counseling them about it. Don't worry, don't think about it.” A support group helped one participant adjust to a diagnosis of heart disease: “I think being part of a group who shared common experiences in both the way they were treating it and what they were doing. It was very, very useful.”
Other participants emphasized regulating emotions to prevent distress from leading to the constant pressure in the body that could lead to heart disease (Figure 2): “When you are depressed, you are sad. It don't take anything too much to start your heart pumping faster—so I try to be calm.” Many participants talked about personally regulating depressed feelings, while others emphasized the need for people to talk with their physician about depression: “…you've got to open up with the physician, you got to let him know what's going on and how you feel and then he can take it from there.” Participants felt depression should be treated immediately in the context of heart disease: “I believe you should be treated immediately [for depression] if you have heart disease…because treating the heart disease and leaving the depression not treated or wait for a while, that could backfire.”
Most participants said that treating one condition required treating the other: “…once you get that [depression treatment] then you can deal with the heart problems…as long as you got the depression you are always going to have the heart problem.” Participants warned of consequences of depression in people with heart disease: “I think you're going to die from depression quicker than you die from the heart because your depression is going to drive your heart even worse.” Similarly, when the main cause of depression is the heart disease diagnosis, managing the heart disease may in fact ameliorate the depression: “I think if someone had a bad heart and then found out their heart is OK, that might change the depression.” Several participants discussed the advantages of integrating treatment of depression and heart disease: “The tendency for the cardiologist to do his job and the therapist to do her job—I ran into that just this past week in the treatment I'm getting.” Another participant said “…older people… really deserve one stop shopping.”
Discussion
Participants described clear pathways linking depression and heart disease. Participants said that heart disease could cause depression because the diagnosis is frightening, having heart disease can limit daily activities, medications can cause depressed feelings, and navigating the health system can reinforce a sense of loss of control. They suggested metaphorically that depression could cause heart disease by adding pressure to the body and creating an unhealthy environment for the body. Participants described the importance of their primary care physician and integrating depression treatment with heart disease prevention and management.
Before discussing the implications of our results, we wish to review the limitations. First, our results were obtained from patients who receive care at one primary care site that might not be representative of most primary care practices. Second, patients' remarks reflected their perceptions of the relationship between depression and heart disease and might not reflect their actual behavior, including adherence to medications for the treatment of the two conditions. Third, data on medical conditions and medications are based on self-reports and are subject to recall and response bias. Lastly, because we did not have a sample of patients who had other medical conditions such as arthritis or cancer, we could not determine whether patients' views regarding the relationship between depression and heart disease generalize to other medical conditions.
Despite those limitations, our findings have practice implications for primary care clinicians managing depression in the context of cardiovascular risk or heart disease. Consistent with research in other settings, many older primary care patients with risk factors for heart disease and symptoms of depression perceive a clear relationship between heart disease and depression. Patients emphasized trying to regulate their thoughts and emotions to prevent depression and cope with heart disease. However, when depression was thought of in terms of heart risk, patients described depression as more serious and warranting clinical attention. Older patients felt that a diagnosis of heart disease could be overwhelming and cause a sense of losing control. One man felt that joining a support group was essential to his adjustment to living with heart disease, and other participants wished their physicians had warned them about difficulties patients may have adjusting to living with heart disease. They suggested physician support in the form of listening, offering support groups or counseling, and being available for questions. Older patients emphasized the importance of recognizing depression and negotiating a treatment plan in the context of heart disease. These and other clinical actions may help patients regain some sense of power when dealing with heart disease.
Our results support the integration of depression management with management for risk factors for cardiovascular disease. Patients in our study supported the idea that depression should be treated immediately in the context of other cardiovascular risk factors and discussed integrating the care for both conditions. An integrated intervention may increase implementation and sustainability in real world practices with limited resources and competing demands. Addressing depression and cardiovascular risk simultaneously may be more acceptable to patients. An integrated intervention would need to improve adequacy of treatment and adherence as well as acknowledging competing influences. Future research should explore whether older adults are more likely to discuss depressive symptoms or consider interventions for depression if their primary care providers incorporate an explanation of the role of negative emotions in the context of overall cardiovascular risk. This message may be persuasive for patients who believe that negative emotions and life difficulties can contribute to the development of heart disease or exacerbation of heart disease or that physical symptoms are necessary for a clinical visit and treatment.
Acknowledgments
This study was supported by a NIMH Mentored Patient-oriented Research Career Development Award (MH67671-01) and a Robert Wood Johnson Generalist Physician Faculty Scholar Award (2004–2008).
References
- 1.Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction: impact on 6-month survival. JAMA. 1993;270(15):1819–25. [PubMed] [Google Scholar]
- 2.Aromaa A, Raitasato A, Reunanen A, et al. Depression and cardiovascular disease. Acta Psychiatr Scand. 1994 377:77–82. doi: 10.1111/j.1600-0447.1994.tb05807.x. [DOI] [PubMed] [Google Scholar]
- 3.Bogner HR, Cary M, Bruce ML, et al. The role of medical comorbidity in outcome of major depression in primary care: the PROSPECT study. Am J Geriatr Psychiatry. 2005;13(10):861–8. doi: 10.1176/appi.ajgp.13.10.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Waal HJ. Propranolol-induced depression. Br Med J. 1967;2:50. doi: 10.1136/bmj.2.5543.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gerstman BB, Jolson HM, Bauer M, Cho P, Livingston JM, Platt R. The incidence of depression in new users of beta-blockers and selected antihypertensives. J Clin Epidemiol. 1996;49:809–15. doi: 10.1016/0895-4356(96)00017-0. [DOI] [PubMed] [Google Scholar]
- 6.Sirey JA, Bruce ML, Alexopoulos GS. The Treatment Initiation Program: an intervention to improve depression outcomes in older adults. Am J Psychiatry. 2005;162(1):184–6. doi: 10.1176/appi.ajp.162.1.184. [DOI] [PubMed] [Google Scholar]
- 7.Fouad MN, Kiefe CI, Bartolucci AA, Burst NM, Ulene V, Harvey MR. A hypertension control program tailored to unskilled and minority workers. Ethn Dis. 1997;7(3):191–9. [PubMed] [Google Scholar]
- 8.Brown C, Battista DR, Bruehlman R, Sereika SS, Thase ME, Dunbar-Jacob J. Beliefs about antidepressant medications in primary care patients: relationship to self-reported adherence. Med Care. 2005;43(12):1203–7. doi: 10.1097/01.mlr.0000185733.30697.f6. [DOI] [PubMed] [Google Scholar]
- 9.Bogner HR, Cahill EC, Frauenhoffer C, Barg FK. Older primary care patients' views regarding antidepressants: a mixed methods approach. Journal of Mental Health. 2008 doi: 10.1080/09638230701677795. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Devalle MN, Norman P. Causal attributions, health locus of control beliefs and lifestyle changes among preoperative coronary patients. Psychology and Health. 1992;7(3):201–11. [Google Scholar]
- 11.French DP, Marteau TM, Senior V, Weinman J. The structure of beliefs about the causes of heart attacks: a network analysis. Br J Health Psychol. 2002;7(Part 4):463–79. doi: 10.1348/135910702320645426. [DOI] [PubMed] [Google Scholar]
- 12.French DP, James D, Horne R, Weinman J. Causal beliefs and behaviour change post-myocardial infarction: how are they related? Br J Health Psychol. 2005;10(Pt 2):167–82. doi: 10.1348/135910705X26722. [DOI] [PubMed] [Google Scholar]
- 13.Petrie KJ, Weinman J, Sharpe N, Buckley J. Role of patients' view of their illness in predicting return to work and functioning after myocardial infarction: longitudinal study. Br Med J. 1996;312(7040):1191–4. doi: 10.1136/bmj.312.7040.1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aalto AM, Heijmans M, Weinman J, Aro AR. Illness perceptions in coronary heart disease. Sociodemographic, illness-related, and psychosocial correlates. J Psychosom Res. 2005;58(5):393–402. doi: 10.1016/j.jpsychores.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 15.Affleck G, Tennen H, Croog S, Levine S. Causal attribution, perceived benefits, and morbidity after a heart attack: an 8-year study. J Consult Clin Psychol. 1987;55(1):29–35. doi: 10.1037//0022-006x.55.1.29. [DOI] [PubMed] [Google Scholar]
- 16.French DP, Marteau TM, Senior V, Weinman J. Perceptions of multiple risk factors for heart attacks. Psychol Rep. 2000;87(2):681–7. doi: 10.2466/pr0.2000.87.2.681. [DOI] [PubMed] [Google Scholar]
- 17.Day RC, Freedland KE, Carney RM. Effects of anxiety and depression on heart disease attributions. Int J Behav Med. 2005;12(1):24–9. doi: 10.1207/s15327558ijbm1201_4. [DOI] [PubMed] [Google Scholar]
- 18.Brown C, Dunbar-Jacob J, Palenchar DR, et al. Primary care patients' personal illness models for depression: a preliminary investigation. Fam Pract. 2001;18(3):314–20. doi: 10.1093/fampra/18.3.314. [DOI] [PubMed] [Google Scholar]
- 19.Sarkisian CA, Lee-Henderson MH, Mangione CM. Do depressed older adults who attribute depression to “old age” believe it is important to seek care? J Gen Intern Med. 2003;18(12):1001–5. doi: 10.1111/j.1525-1497.2003.30215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lawrence V, Murray J, Banerjee S, et al. Concepts and causation of depression: a cross-cultural study of the beliefs of older adults. Gerontologist. 2006;46(1):23–32. doi: 10.1093/geront/46.1.23. [DOI] [PubMed] [Google Scholar]
- 21.Marwaha S, Livingston G. Stigma, racism, or choice. Why do depressed ethnic elders avoid psychiatrists? J Affect Disord. 2002;72(3):257–65. doi: 10.1016/s0165-0327(01)00470-0. [DOI] [PubMed] [Google Scholar]
- 22.Rabins PV. Prevention of mental disorders in the elderly: current perspectives and future prospects. J Am Geriatr Soc. 1992;40:727–33. doi: 10.1111/j.1532-5415.1992.tb01968.x. [DOI] [PubMed] [Google Scholar]
- 23.Michaela JL, Wood JV. Causal attributions in health and illness. In: Kendall PC, editor. Advances in cognitive-behavioral research and therapy. New York: Academic Press; 1986. [Google Scholar]
- 24.Avis NE. Illness perceptions and behaviour change among coronary artery bypass patients. In: Kendall PC, editor. Advances in cognitive-behavioral research and therapy. New York: Academic Press; 1984. [Google Scholar]
- 25.Plotkin-Israel I. Causal attributions, perceived control, and coping among MI patients. In: Kendall PC, editor. Advances in cognitive-behavioral research and therapy. New York: Academic Press; 1984. [Google Scholar]
- 26.Low KG, Thoresen CE, Pattillo JR, Fleischmann N. Causal attributions and coronary heart disease in women. Psychol Rep. 1993;73(2):627–36. doi: 10.2466/pr0.1993.73.2.627. [DOI] [PubMed] [Google Scholar]
- 27.Cooper-Patrick L, Crum RM, Ford DE. Identifying suicidal ideation in general medical patients. JAMA. 1994;272:1757–62. [PubMed] [Google Scholar]
- 28.DiGregorio S. Strategies in qualitative research: methodological issues and practices using QSR NVIVO and NUD*IST. London: Institute of Education; 2003. Analysis as cycling: shifting between coding and memoing in using qualitative software; pp. 8–9. [Google Scholar]
- 29.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 30.Comstock GW, Helsing KJ. Symptoms of depression in two communities. Psychol Med. 1976;6:551–63. doi: 10.1017/s0033291700018171. [DOI] [PubMed] [Google Scholar]
- 31.Eaton WW, Kessler LG. Rates of symptoms of depression in a national sample. Am J Epidemiol. 1981;114:528–38. doi: 10.1093/oxfordjournals.aje.a113218. [DOI] [PubMed] [Google Scholar]
- 32.Gatz M, Johansson B, Pedersen N, Berg S, Reynolds C. A cross-national self-report measure of depressive symptomatology. International Psychogeriatrics. 1993;5:147–56. doi: 10.1017/s1041610293001486. [DOI] [PubMed] [Google Scholar]
- 33.Miller D, Malmstrom M, Joshi S, Andresen E, Morley J, Wolinsky F. Clinically relevant levels of depressive symptoms in community-dwelling middle-aged African-Americans. J Am Geriatr Soc. 2004;52:741–8. doi: 10.1111/j.1532-5415.2004.52211.x. [DOI] [PubMed] [Google Scholar]
- 34.Foley K, Reed P, Mutran E, DeVellis R. Measurement adequacy of the CES-D among a sample of older African-Americans. Psychiatry Research. 2002;109:61–9. doi: 10.1016/s0165-1781(01)00360-2. [DOI] [PubMed] [Google Scholar]
- 35.Newmann JP, Engel RJ, Jensen J. Age differences in depressive symptom experiences. Journal of Gerontology: Psychological Sciences. 1991;46:224–35. doi: 10.1093/geronj/46.5.p224. [DOI] [PubMed] [Google Scholar]
- 36.Boeije H. A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Quality and Quantity. 2002;36:391–409. [Google Scholar]


