Abstract
Objective
Our purpose was to determine the personal characteristics associated with different patterns of adherence to the antidepressant citalopram in a primary care trial of depression management.
Method
The study sample consisted of 228 adults aged 60 years and older recruited from primary care settings and who participated in a depression intervention. The intervention consisted of services of trained care managers, who offered recommendations to physicians following a clinical algorithm and helped patients with treatment adherence. Adherence to the antidepressant citalopram was measured using pill counts. We employed the latent class model to classify patients according to the pattern of adherence to citalopram over time. We examined the association of sociodemographic characteristics, depression status, cognitive status, and medical comorbidity with the resulting classes of adherence.
Results
The latent class model generated three classes of adherence: known to be adherent, unknown adherence, and known to be nonadherent. Participants who were white were more likely to be in the known to be adherent class than in the known to be nonadherent class (odds ratio (OR) = 10.38, 95% confidence interval (CI) [3.47, 31.12]). Married participants were less likely to be in the unknown adherence class than the known to be nonadherent class (OR = 0.28, 95% CI [0.09, 0.85]). No associations between age, gender, education level, depression status, cognitive status, or medical comorbidity and classes of adherence were found.
Conclusions
We found stronger relationships between ethnicity and marital status with patterns of adherence to citalopram than we did other personal characteristics. Identification of a subgroup of patients at particularly high risk of nonadherence is important for the development of adherence interventions.
Keywords: aged, primary health care, patient compliance, adherence, compliance interventions
Introduction
Epidemiologic and clinical studies over the past two decades have provided ample evidence that the primary care setting is pivotal to improving depression treatment over a population level [1-3]. Primary care occupies a strategic position for the evaluation and treatment of depression in late life [4]. Nevertheless, many older patients with depression do not receive adequate treatment and do not complete recommended regimens for depression. Recent epidemiological studies have confirmed on average one in three patients does not complete depression treatment [5-7]. Early nonadherence to depression treatment is of special concern because data have shown that 28% of patients have stopped their antidepressant medication within the first month of treatment and 44% of patients were no longer taking the antidepressant after 3 months [8].
Haynes [9] and others [10, 11] reviewed the factors associated with adherence to medical regimens. All the factors associated with adherence have yet to be fully elucidated but patient knowledge of a condition is not enough to change adherence behavior [12-14]. These reviews have not specifically considered the issue of adherence to depression treatment among older adults in primary care. Studies on adherence to antidepressant medications have found that improved antidepressant adherence is associated with greater social support among patients who believe they have control over their health [15], patients' beliefs about the medications [16], perceived stigma and benefits of treatment [17], and travel time less than 30 minutes, preference for medicine treatment as well as perceived greater benefits [18]. One study of Black and Latino elderly patients found the two ethnic minority groups had similar barriers to adherence and that intentional nonadherence (e.g., alteration of medication regimen to fit one's needs) was associated with negative beliefs about antidepressant medications whereas unintentional nonadherence (e.g., difficulties keeping track of a medication regimen) was associated with cognitive impairment [19]. A review of interventions for improving medication adherence among older adults concluded that a combination of interventions addressing a wider range of barriers is more effective than an intervention focused on a single barrier. In addition, an individual approach consisting of a specifically tailored intervention also appears to be effective [20]. Because a combination of interventions or a specifically tailored intervention is both costly and time intensive, we sought to identify which patients might benefit the most from an intervention for adherence using readily identifiable or measurable characteristics. In addition, information is lacking on the patterns of adherence to antidepressant medications over time which would help determine the optimal timing for intervention deployment.
Our goal was to investigate the patterns of adherence to the antidepressant citalopram in a primary care study. The sample derives from a large ethnically diverse sample of older adults in the primary care setting. Our conceptual model incorporated cultural influences as well as mental and physical health states in characterizing patient adherence to antidepressants. Consistent with prior work, we hypothesized that patients who were cognitively impaired [19, 21, 22], were not married [15], or had a greater medical burden [23, 24] would be less likely than others to adhere.
To our knowledge, this is the first investigation to classify patterns of adherence to antidepressants using latent class statistical methods. The underlying principle of latent class analysis is to search for an unobserved latent categorical variable that explains the pattern of adherence measurements over time [25] (see Figure 1). The latent class model has several advantages. First, the model does not demand that we assign patients to a specific class, as each patient receives an estimated probability of class membership. In other words, misclassification error is minimized. Second, prior status is often a powerful predictor of subsequent status and the latent class model takes into account non-independence of assessments across time. Third, the latent class model also lets us, simultaneously, take into account baseline covariates other than the key variables under study in assessing their independent relationship to adherence, such as patient cognitive status and medical comorbidity.
Figure 1.
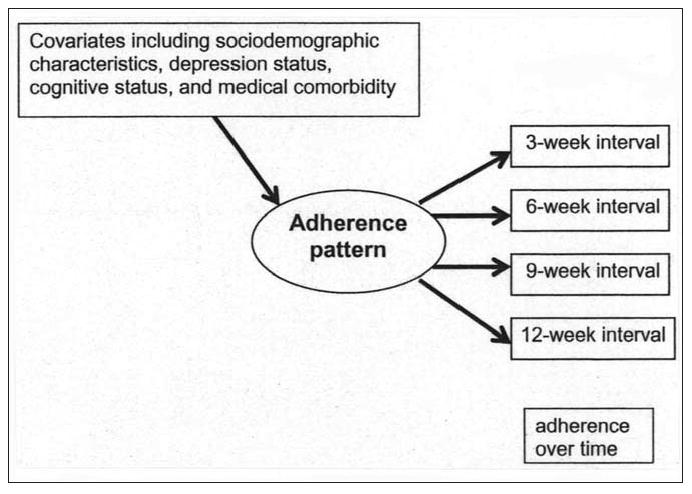
Latent class analysis of adherence to citalopram.
Method
The PROSPECT Study
The PROSPECT Study was a multisite, collaborative study designed to assess whether depression treatment in primary care settings can reduce the risk of suicide in elderly patients. A total of 20 primary care practices participated, including practices from greater New York City, Philadelphia, Pennsylvania, and Pittsburgh, Pennsylvania in the United States. Practices were paired within each region (New York, Philadelphia, Pittsburgh) by setting (urban, suburban, rural), academic affiliation (university vs. community based), size, and the ethnicity distribution of their patient populations. Within pairs, practices were randomly assigned to either enhanced care or intervention. The study used a two-stage sampling design to generate a representative sample of primary care patients with the DSM-IV diagnosis of major depression or minor depression; minor depression was defined by the study as a depression meeting at least three DSM-IV criteria, having a 24-item Hamilton Depression Rating Scale (HDRS) score of 10 or higher, and persisting for at least one month. An age-stratified (60-74 years, over 75 years), random sample was obtained of patients with an appointment with their primary care physician within two weeks. Physicians notified sampled patients, by mail, allowing patients to decline contact. Research associates telephoned the remaining sample to confirm study eligibility: age ≥ 60 years, ability to give informed consent, Mini-Mental State Examination (MMSE) ≥ 18 [26], and ability to communicate in English. Patients were interviewed in person at the primary care practices. Patients who gave oral consent were screened for depressive symptoms using the Centers for Epidemiologic Studies Depression scale (CES-D) [27]. All patients with CES-D above 20 as well as a 5% random sample of patients with lower scores were invited to enter the study. To increase the sensitivity of the screening procedure, patients with CES-D <20 and not selected for the 5% random sample were also recruited if they reported history of depression or antidepressant treatment. Details of the study design of the PROSPECT Study are available elsewhere [28-30]. The study protocols were approved by the Institutional Review Boards of the Cornell University, University of Pittsburgh, and University of Pennsylvania Schools of Medicine.
PROSPECT Intervention
The intervention was implemented by 15 depression care managers, who used the AHCPR Guidelines (after operationalization and adaptation for older patients) to provide appropriately timed and targeted recommendations to primary care physicians. The depression care managers were nurses, social workers, or psychologists trained and supervised weekly by geriatric psychiatrist investigators and functioned as collaborators to primary care physicians. The depression care managers monitored psychopathology, treatment adherence, treatment response and side effects and provided follow-up in-person or by telephone at predetermined intervals or when clinically necessary. However, the primary care physicians remained responsible for the clinical care of their patients. The intervention and the algorithm derived from the AHCPR Guidelines has been described in detail elsewhere [28, 29]. In the Intervention Condition, the cost of the first line antidepressant, the selective serotonin reuptake inhibitor (citalopram), was covered for the participants.
Measurement Strategy
Patient Adherence to Antidepressant
The primary dependent variable was patient adherence to citalopram measured by pill counts. Patients were given prescribed numbers of citalopram pills at each visit. In addition, one extra week of pills was given in case more pills might be needed (e.g., if some pills were lost). Patients were to return any leftover pills by the next visit. At each visit, health specialists recorded the number of pills brought back by patients and also recorded the expected number of pills to be returned. If a patient missed a visit, the health specialist called the patient to reschedule the visit as soon as possible. In some cases, patients were sent medications by overnight mail after a missed visit. Patients' adherence to citalopram was coded as one of three categories: 1) known to be adherent; 2) unknown adherence; and 3) known to be nonadherent.
The number of pills actually removed from the blister pak was expressed as a percentage of the number which should have been taken in the interval. If patients took at least 80% of their pills in the interval (i.e., if the ratio was between 80% and 120%) then they were considered to be adherent. Otherwise, they were considered to be nonadherent. Greater or equal to 80% adherence was used because the 80% cut-point has been used as a standard to which other measures are compared [31]. If the actual number of pills returned and/or the expected number of pills to be returned were not recorded, patients were considered to have unknown adherence. We considered patient adherence to citalopram at 3-week, 6-week, 9-week, and 12-week intervals. Some patients were prescribed citalopram for more than 12 weeks but this article focuses on early adherence.
Sociodemographic Characteristics
We used standard questions to obtain information from the participants on age, gender, self-reported ethnicity, marital status, and education.
Depression Diagnoses
Trained research assistants (Ph.D., M.A., or experienced B.A. level) assigned depression diagnoses to patients using the Structured Clinical Interview for Axis I DSM-IV Diagnoses (SCID) [32]. Study psychiatrists reviewed all the SCID ratings. Severity of depression was assessed using the 24-item Hamilton Depression Rating Scale (HDRS) [33]. HDRS scores were analyzed as a continuous variable.
Mini-Mental State Examination
Cognitive status was assessed with the Mini-Mental State Examination (MMSE) which is a short standardized mental status examination that has been widely employed for clinical and research purposes [26]. The MMSE has been extensively studied, as reviewed by Tombaugh and McIntyre [34] and by Crum and her colleagues [35]. The MMSE assesses orientation to time and place, registration, memory, attention and concentration, praxis, and constructional and language capacity. MMSE scores were analyzed as a continuous variable.
Medical Comorbidity
Persons were classified as having a medical comorbidity by self-report. The questionnaire used was based on the Charlson Comorbidity Index, supplemented by questions about the common disabling conditions of late life [36]. Medical comorbidity was analyzed as a continuous variable. Participants were asked about myocardial infarction, heart failure, angina, angioplasty or coronary artery bypass surgery, atrial fibrillation, stroke, peripheral vascular disease, high blood pressure, diabetes, cancer, chronic pulmonary disease, as well as other conditions. Persons were considered to have a medical comorbidity if they gave a positive response to any of the medical conditions.
Analytic Strategy
There were two phases of analysis. In the first phase we examined means and proportions in a descriptive analysis. In phase 2, we estimated an exploratory latent class model, since we had no prior hypothesis for the adherence pattern structure. Patterns of adherence were based on the results from the latent class analysis. Patient characteristics among the different patterns were compared using the regression component of the model.
Latent class analysis of indicators of adherence to depression medication over the 12-week period was applied to identify different adherence patterns [25]. In this case, the adherence measurements were based on pill counts during four time intervals within a 12-week period. Let U denote an adherence pattern. The probability of adherence pattern equals
where C denotes the latent class indicator [37]. Pr (U = u | C = k) was estimated with ordered polychotomous logistic regression. In polychotomous logistic regression, the order of the categories is important. The model assumes the categorical variable is ordinal. Therefore, the adherence measure at each time point was assumed to be ordinal. The ordered three level adherence measure was categorized as: 1 = known to be adherent, 2 = unknown adherence, and 3 = known to be nonadherent because unknown adherence is neither an indication that an individual was adherent nor nonadherent at a given time point.
Simultaneously, we estimate a regression model predicting latent class membership. Specifically, let X denote the baseline covariates. Logistic regression was used to estimate latent class membership probabilities.
Data analysis was performed using Mplus, which utilizes an efficient estimation-maximization (EM) algorithm [38] for maximum likelihood estimation. Results are reported in terms of probability of adherence at a given time point conditional on class membership and odds ratios with 95% confidence intervals comparing patient characteristics among the classes. Model choice, in terms of the number of classes was determined through examination of fit indices as well as for clinically interpretable results. Akaike Information Criteria (AIC) [39] and Bayesian Information Criteria (BIC) [40] were used to assess the model goodness of fit. Both measures assess improvements in fit while adjusting for the number of parameters.
In summary, the estimation procedure of a latent class model yields two sets of parameters. The latent class probabilities (unconditional probabilities) estimate the probability of adherence pattern using multinomial logistic regression. The conditional probabilities estimate the probability of the observed variables, given that the individual is a member of an unobserved class using polychotomous logistic regression. In other words, the conditional probabilities represent the probability that an individual is known to be adherent, has unknown adherence, or is known to be nonadherent at a specific time point given the class. In addition, the regression part of the model yields estimates of latent class membership given a personal characteristic (e.g., age or gender).
Results
Study Sample
The sample included 235 persons in the PROSPECT intervention condition who had been prescribed citalopram. Seven people were excluded because they did not have complete information on the covariates, leaving a study sample size of 228 for this analysis. The age range of our study sample was 60 to 94 years. In all, 141 persons (61.8% of the study sample) had a diagnosis of major depression and 61 persons (26.8% of the study sample) had a diagnosis of minor depression. The sociodemographic characteristics, depression status, cognitive status, and medical comorbidity of the study sample are described in Table 1. The overall observed adherence in the study sample is presented in Table 2. At the 3-week interval, 131 persons (57.5% of the study sample) were known to be adherent and 92 persons (40.4% of the study sample) were known to be nonadherent. Both the observed adherence and nonadherence decreased over time. On the other hand, at the 3-week interval, five persons (2.1% of the study sample) had unknown adherence and unknown adherence increased over time.
Table 1.
Patient Sociodemographic Characteristics, Depression Status, Cognitive Status, and Medical Comorbidity (n = 228)
| Patient characteristics | |
|---|---|
| Age in years, mean ± standard deviation | 70.2 ± 7.59 |
| Women, n (%) | 162 (71.1%) |
| White, n (%) | 59 (25.9%) |
| Married, n (%) | 83 (36.4%) |
| Education in years, mean ± standard deviation | 12.5 ± 3.28 |
| HDRS, mean ± standard deviation | 17.9 ± 7.14 |
| MMSE, mean ± standard deviation | 24.4 ± 2.55 |
| Medical comorbidity, mean ± standard deviation | 2.92 ± 2.33 |
Note: Data gathered from the PROSPECT study. HDRS = Hamilton Depression Rating Scale; MMSE = Mini-Mental State Examination.
Table 2.
Observed Adherence to the Antidepressant Citalopram at the 3-Week, 6-Week, 9-Week, and 12-Week Interval (n = 228)
| Time interval | Known to be adherent n (%) |
Unknown adherence n (%) |
Know to be nonadherent n (%) |
|---|---|---|---|
| 3-week interval | 131 (57.5%) | 5 (2.2%) | 92 (40.4%) |
| 6-week interval | 91 (39.9%) | 57 (25.0%) | 80 (35.1%) |
| 9-week interval | 81 (35.5%) | 86 (37.7%) | 61 (26.8%) |
| 12-week interval | 67 (29.4%) | 109 (47.8%) | 52 (22.8%) |
Note: Data gathered from the PROSPECT study.
Patterns Derived from Latent Class Analyses
A series of latent class models was fitted to the pill counts. The three-class model presented in Figure 2 improved the model fit over the two- and four-class models. The three-class model was also clinically most relevant. The number of persons assigned to each class is presented at the top of Figure 2. Participants were assigned to each latent class according to their maximal posterior probabilities in each class. Persons in class 1 (49% of the entire sample, “known adherent”) had a high probability of adherence at each time point. In class 1, the conditional probabilities for known adherence at each time point were all above 0.5. Participants in class 2 (29% of the entire sample, “unknown adherence”) were much more likely to have adherence status unknown after the 3-week time point as shown by the conditional probabilities for unknown adherence at 6, 9, and 12 weeks of 0.79, 0.97, and 1.00, respectively. Persons in class 3 (22% of the entire sample, “known nonadherent”) have a high probability of pill counts indicating nonadherence over time. In class 3, the conditional probabilities for known nonadherence at each time point were all above 0.5. Looking at the overall observed adherence compared to the latent classes, illustrates how the classes have identified subgroups differing in patterns of adherence.
Figure 2.
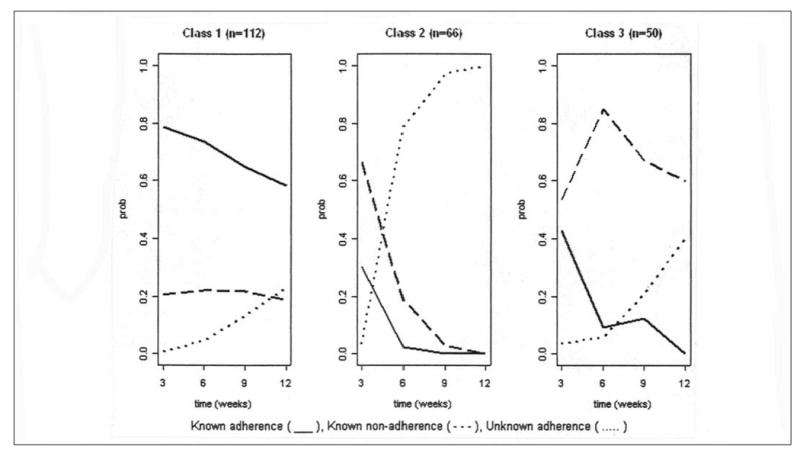
Latent class analysis of adherence to citalopram (number of individuals in each class with plotted conditional probabilities). Note: Data gathered from the PROSPECT study.
Regression of Classes on Covariates
Table 3 compares eight personal characteristics among the three classes. Class 3 (known nonadherent) was the reference group. The adjusted odds ratios (OR) represent ORs adjusted for all the variables in the table (95% confidence intervals (CI) are shown in brackets). Individuals in class 1 (known adherent) compared to individuals in class 3 (known nonadherent) were more likely to be white (OR = 10.38, 95% CI [3.47, 31.12]). Individuals in class 2 (unknown adherence) compared to individuals in class 3 (known nonadherent) were less likely to be married (OR = 0.28, 95% CI [0.09, 0.85]).
Table 3.
Comparison of Patient Characteristics among Adherence Classes Generated from the Latent Class Model (n = 228)
| Patient characteristics | Class 1 vs. 3 OR [95% CI] |
Class 2 vs. 3 OR [95% CI] |
|---|---|---|
| Age in years | 1.02 [0.97, 1.08] |
1.01 [0.96, 1.07] |
| Gender (reference: male) |
0.66 [0.23, 1.94] |
0.60 [0.17, 2.07] |
| Ethnicity (reference: minority) |
10.38 [3.47, 31.12] |
2.48 [0.85, 7.25] |
| Marital status (reference: not married) |
0.57 [0.21, 1.57] |
0.28 [0.09, 0.85] |
| Education in years | 0.94 [0.80, 1.10] |
0.95 [0.79, 1.14] |
| HDRS | 0.97 [0.89, 1.04] |
0.92 [0.84, 1.00] |
| MMSE | 1.04 [0.82, 1.31] |
1.02 [0.80, 1.31] |
| Medical comorbidity | 1.09 [0.90, 1.33] |
1.08 [0.87, 1.33] |
Note: Data gathered from the PROSPECT study. HDRS = Hamilton Depression Rating Scale; MMSE = Mini-Mental State Examination. OR = odds ratio; CI = confidence interval.
Discussion
Patterns of medication adherence fell into three classes (known adherent, unknown adherence, and known nonadherent) with different personal characteristics associated with each class. Participants who were white were more likely to be in the known adherent class than the known to be nonadherent class compared to persons who self-identified as an ethnic minority. Married participants compared to unmarried participants were less likely to be in the unknown adherence class than the known nonadherent class, meeting with the depression care managers even if they were not adherent to the pills. Our use of latent class analysis enabled us to examine distinct courses of adherence as compared to assessing adherence through proportions which reveal only a quantitative gradient with no group standing out with a distinct course. Information about patterns of medication adherence and associated personal characteristics informs clinicians and researchers about possible adherence interventions.
Before discussing our findings, the results must first be considered in the context of some potential study limitations. First, we obtained our results only from primary care sites in greater New York City, Philadelphia, and Pittsburgh whose patients may not be representative of other primary care practices in the Northeastern United States. However, these practices were both community-based and academically affiliated and are therefore probably similar to the range of other practices in that region. Second, participants' responses in the study may be affected by depression and cognitive status. Third, selection bias is a potential limitation because, although the larger project was based on a random sample of primary care patients, the data on adherence consisted of all who were selected for the larger project, agreed to participate, and had complete information. Fourth, although more frequent follow-up would have been desirable, concerns about participant burden and cost led us to select few, yet clinically meaningful, follow-up times. Fifth, we used a validated measure of adherence but recognize the limitations of only one data source. By using a measure of adherence based on pill counts, we may have misclassified some nonadherent patients as adherent, such as those who brought back empty blister paks but may not have taken all the medication. In addition, we were not able to evaluate other types of nonadherence, such as inappropriate timing of dosages if a patient was trying to make up for missed dosages. Finally, because of the sample size we were unable to examine site differences in adherence patterns with the latent class model.
Nonetheless, despite limitations our results deserve attention because we attempted to characterize patterns of adherence to the antidepressant citalopram and the association of patient-level factors with those patterns. Our results were not wholly consistent with our initial hypotheses. In summary, our analysis demonstrated three classes of adherence (known adherent, unknown adherence, known nonadherent). Ethnicity and marital status were found to be associated with the adherence classes. We did not find as we had hypothesized an association between age, depression status, cognitive status, or number of medical conditions with adherence classes. The three classes we observed suggest a possible need for more intensive interventions for certain individuals. Our results also suggest that different interventions might be needed for participants who might be in the known nonadherent class, persons who may have met with the depression care managers but did not have high levels of adherence, and the unknown adherence class, persons who may have missed meetings with the depression care managers. Identifying patients who will benefit most from special attention and a more intensive intervention may be key to improving outcomes for depression in primary care.
Married participants were less likely to be in the unknown adherence class than the known nonadherent class. The strength of the association between social support and follow-up with the intervention suggests the need to involve family members in an intervention. Social support has direct and indirect effects on the adherence to therapy for depression. Seeking care is often a social process managed by social relationships (e.g., the network-episode model of the pathway to mental health services [41]), not a one-time personal cost-benefit analysis. Depressed persons with more extensive and supportive relationships improve more quickly than those who are socially isolated or in conflictful relationships [21, 42, 43]. Emotional support and regimen-specific support have been shown to increase the adherence to medical regimens across a variety of medical conditions [44-47]. High social support also reflects personal characteristics including relationship orientation and skills needed to form positive treatment relationships with physicians and others involved in care [48, 49]. Patients who are not married may need more extensive social support for improvement of adherence to the intervention.
Participants who self-identified as white were more likely to be in the known adherent class than the known to be nonadherent class. However, we wish to acknowledge that the individuals self-identified as part of a particular ethnic group are not necessarily homogeneous. Therefore, any differences we observe across ethnic groups are likely to represent measured and unmeasured differences in social class, exposures, health beliefs and practices, as well as other characteristics [50]. Other investigators have found a variation in recognition and treatment of psychiatric disturbances according to ethnicity [51], as well as ethnic differences in the acceptability of depression treatment [52]. However, studies have not typically focused on the role of ethnicity in studying observed differences in antidepressant adherence. Patients' cultural and social context is important to consider in the development of interventions for adherence. Culturally tailored interventions may improve adherence to depression treatment among ethnic minorities.
The lack of significant associations of age, depression status, cognitive status, or number of medical conditions in the intervention patients suggests that the effects of these patient-level variables did not appear to influence the patterns of adherence we found. Our results are therefore not wholly consistent with our initial hypotheses. With regard to chronic medical conditions, the type of chronic medical condition and the number of medications the patient is taking may be more important factors in adherence. In the examination of cognition more careful assessment of memory and attention or direct use of everyday performance tasks that include medication-related items [53-55] may be necessary to find a clear association with cognitive measures.
Patterns of adherence to depression treatment may be related to certain patient-level factors. Latent class analysis appears to be an informative model for examining adherence to the antidepressant citalopram over time. The development and implementation of interventions to improve depression treatment adherence and depression outcomes may need to more intensive or tailored for certain subgroups of patients with known nonadherence and perhaps substantially different for subgroups of patients who may have missed meetings with the depression care managers.
Footnotes
Dr. Bogner was supported by a NIMH Mentored Patient-Oriented Research Career Development Award (MH67671-01) and is a Robert Wood Johnson Foundation Generalist Physician Faculty Scholar (2004-2008). PROSPECT is a collaborative research study funded by the National Institute of Mental Health. The three groups include the Advanced Centers for Intervention and Services Research of Cornell University (PROSPECT Coordinating Center; PI: George S. Alexopoulos, M.D. and Co-PIs: Martha L. Bruce, Ph.D., M.P.H.; Herbert C. Schulberg, Ph.D.; R01 MH59366, P300 MH68638), University of Pennsylvania (PI: Ira Katz, M.D., Ph.D., and Co-PIs: Thomas Ten Have, Ph.D., Gregory K. Brown, Ph.D.; R01 MH59380, P30 MH52129) and University of Pittsburgh (PI: Charles F. Reynolds, M.D., and Co-PI: Benoit H. Mulsant, M.D.; R01 MH59381, P30 MH52247). Additional small grants came from Forest Laboratories and the John D. Hartford Foundation.
References
- 1.Gallo JJ, Ryan SD, Ford D. Attitudes, knowledge, and behavior of family physicians regarding depression in late life. Archives of Family Medicine. 1999;8:249–256. doi: 10.1001/archfami.8.3.249. [DOI] [PubMed] [Google Scholar]
- 2.Gallo JJ, Rabins PV, Iliffe S. The ‘research magnificent’ in late life: Psychiatric epidemiology and the primary health care of older adults. International Journal of Psychiatry in Medicine. 1997;27:185–204. doi: 10.2190/JF9W-9Q87-KV0F-YCY4. [DOI] [PubMed] [Google Scholar]
- 3.Gallo JJ, Marino S, Ford D, Anthony JC. Filters on the pathway to mental health care: II. Sociodemographic factors Psychological Medicine. 1995;25:1149–1160. doi: 10.1017/s0033291700033122. [DOI] [PubMed] [Google Scholar]
- 4.Rabins PV. Prevention of mental disorders in the elderly: Current perspectives and future prospects. Journal of the American Geriatrics Society. 1992;40:727–733. doi: 10.1111/j.1532-5415.1992.tb01968.x. [DOI] [PubMed] [Google Scholar]
- 5.Croghan TW, Lair TJ, Engelhart L, Crown WE, Copley-Merriman C, Melfi CA, Obenchain RL, Buesching DP. Effect of antidepressant therapy on health care utilization and costs in primary care. Psychiatric Services. 1997;48(11):1420–1426. doi: 10.1176/ps.48.11.1420. [DOI] [PubMed] [Google Scholar]
- 6.Melfi CA, Chawla AJ, Croghan TW, Hanna MP, Kennedy S, Sredl K. The effects of adherence to antidepressant treatment guidelines on relapse and recurrence of depression. Archives of General Psychiatry. 1998;55(12):1128–1132. doi: 10.1001/archpsyc.55.12.1128. [DOI] [PubMed] [Google Scholar]
- 7.Tedlow JR, Fava M, Uebelacker LA, Alpert JE, Nierenberg AA, Rosenbaum JF. Are study dropouts different from completers? Biological Psychiatry. 1996;40(7):668–670. doi: 10.1016/0006-3223(96)00204-1. [DOI] [PubMed] [Google Scholar]
- 8.Lin EH, Von Korff M, Katon W, Bush T, Simon GE, Walker E, Robinson P. The role of the primary care physician in patients' adherence to antidepressant therapy. Medical Care. 1995;33:67–74. doi: 10.1097/00005650-199501000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Haynes RB, Taylor DW, Sackett DL. Compliance in health care. Baltimore: Johns Hopkins University Press; 1979. [Google Scholar]
- 10.Coons SJ, Sheahan SL, Martin SS, Hendricks J, Robbins CA, Johnson JA. Predictors of medication noncompliance in a sample of older adults. Clinical Therapeutics. 1994;16:110–117. [PubMed] [Google Scholar]
- 11.Kaplan RM, Simon HJ. Compliance in medical care: Reconsideration of self-predictions. Annals of Behavioral Medicine. 1990;12:66–71. [Google Scholar]
- 12.Becker MH. Patient adherence to prescribed therapies. Medical Care. 1985;23:539–555. doi: 10.1097/00005650-198505000-00014. [DOI] [PubMed] [Google Scholar]
- 13.German PS, Klein LE, McPhee SJ, Smith CR. Knowledge of and compliance with drug regimens in the eldery. Journal of the American Geriatrics Society. 1982;30:568–571. doi: 10.1111/j.1532-5415.1982.tb05663.x. [DOI] [PubMed] [Google Scholar]
- 14.Mazzuca SA. Does patient education in chronic disease have therapeutic value? Journal of Chronic Disease. 1982;35:521–529. doi: 10.1016/0021-9681(82)90071-6. [DOI] [PubMed] [Google Scholar]
- 15.Voils CI, Steffens DC, Flint EP, Bosworth HB. Social support and locus of control as predictors of adherence to antidepressant medication in an elderly population. American Journal of Geriatric Psychiatry. 2005;13(2):157–165. doi: 10.1176/appi.ajgp.13.2.157. [DOI] [PubMed] [Google Scholar]
- 16.Aikens JE, Nease DE, Nau DP, Klinkman MS, Schwenk TL. Adherence to maintenance-phase antidepressant medication as a function of patient beliefs about medication. Annals of Family Medicine. 2005;3(1):23–30. doi: 10.1370/afm.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sirey JA, Bruce ML, Alexopoulos GS, Perlick DA, Friedman SJ, Meyers BS. Perceived stigma and patient-related severity to illness as predictors of antidepressant drug adherence. Psychiatric Services. 2001;52(12):1615–1620. doi: 10.1176/appi.ps.52.12.1615. [DOI] [PubMed] [Google Scholar]
- 18.Gonzales J, Williams JW, Jr, Noel PH, Lee S. Adherence to mental health treatment in primary care clinic. Journal of the American Board of Family Practice. 2005;18(2):87–96. doi: 10.3122/jabfm.18.2.87. [DOI] [PubMed] [Google Scholar]
- 19.Ayalon L, Arean PA, Alvidrez J. Adherence to antidepressant medications in black and Latino elderly patients. American Journal of Geriatric Psychiatry. 2005;13(7):572–580. doi: 10.1176/appi.ajgp.13.7.572. [DOI] [PubMed] [Google Scholar]
- 20.Van Eijken M, Tsang S, Wensing M, deSmet P, Grol R. Interventions to improve medication compliance in older patients living in the community. Drugs Aging. 2003;20(3):229–240. doi: 10.2165/00002512-200320030-00006. [DOI] [PubMed] [Google Scholar]
- 21.Alexopoulos GS, Meyers BS, Young RC, Kakuma T, Feder M, Einhorn A, Rosendahl E. Recovery in geriatric depression. Archives of General Psychiatry. 1996;53:305–312. doi: 10.1001/archpsyc.1996.01830040039008. [DOI] [PubMed] [Google Scholar]
- 22.Farmer ME, Kittner SJ, Abbott RD, Wolz MM, Wolf PA, White LR. Longitudinally measured blood pressure, antihypertensive medication use, and cognitive performance: The Framingham Study. Journal of Clinical Epidemiology. 1990;43:475–480. doi: 10.1016/0895-4356(90)90136-d. [DOI] [PubMed] [Google Scholar]
- 23.Rosenstock IM. Enhancing patient compliance with health recommendations. Journal of Pediatric Health Care. 1988;2:67–72. doi: 10.1016/0891-5245(88)90169-1. [DOI] [PubMed] [Google Scholar]
- 24.Cockburn J, Gibberd RW, Reid AL, Sanson-Fisher RW. Determinants of non-compliance with short-term antibiotic regimens. British Medical Journal. 1987;295:814–818. doi: 10.1136/bmj.295.6602.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCutcheon A. Latent class analysis. Beverly Hills: Sage University Press; 1987. [Google Scholar]
- 26.Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 27.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 28.Bruce ML, Ten Have TR, Reynolds CF, III, Katz IR, Schulberg HC, Mulsant BH, Brown GK, McAvay GJ, Pearson JL, Alexopoulos GS. A randomized controlled trial to reduce suicidal ideation and depressive symptoms in depressed older primary care patients: The PROSPECT study. Journal of the American Medical Association. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 29.Mulsant BH, Alexopoulos GS, Reynolds CF, III, Katz IR, Abrams R, Oslin D, Schulberg HC. Pharmacological treatment of depression in older primary care patients: The PROSPECT algorithm. International Journal of Geriatric Psychiatry. 2001;16:585–592. doi: 10.1002/gps.465. [DOI] [PubMed] [Google Scholar]
- 30.Schulberg HC, Bryce C, Chism K, Mulsant BH, Rollman B, Bruce M, Coyne J, Reynolds CF., III Managing depression in late life in primary care practice: A case study of the Health Specialist's role. International Journal of Geriatric Psychiatry. 2001;16:577–584. doi: 10.1002/gps.470. [DOI] [PubMed] [Google Scholar]
- 31.George CF, Peveler RC, Heiliger S, Thompson C. Compliance with tricyclic antidepressants: the value of four different methods of assessment. British Journal of Clinical Pharmacology. 2000;50:166–171. doi: 10.1046/j.1365-2125.2000.00244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for Axis I DSM-IV Disorders (SCID) Washington, DC: American Association Press, Inc.; 1995. [Google Scholar]
- 33.Hamilton M. A rating scale for depression. Journal of Neurology and Neurosurgical Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tombaugh TN, McIntyre NJ. The Mini-Mental State Examination: A comprehensive review. Journal of the American Geriatrics Society. 1992;40:922–935. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]
- 35.Crum RM, Anthony JC, Bassett SS, Folstein MF. Population-based norms for the Mini-Mental State Examination by age and educational level. Journal of the American Medical Association. 1993;269:2386–2391. [PubMed] [Google Scholar]
- 36.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longiudinal studies: Development and validation. Journal of Chronic Disease. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 37.Vermunt JK, Magidson J. Latent class analysis. In: Lewis-Beck MS, Bryman A, Liao TF, editors. The Sage Encyclopedia of Social Sciences Research Methods. Thousand Oakes, CA: Sage Publications; 2004. pp. 549–553. [Google Scholar]
- 38.Dempster AP, Laird NM, Rubin DB. Maximum liklihood from incomplete data via the EM algorithm with discussion. Journal of the Royal Statistical Society B. 1977;39:1–38. [Google Scholar]
- 39.Akaike H. A Bayesian analysis of the minimum AIC procedure. Annals of the Institute of Statistical Mathematics. 1978;30:9–14. [Google Scholar]
- 40.Schwarz G. Estimating the dimension of a model. The Annals of Statistics. 1978;6:461–464. [Google Scholar]
- 41.Pescosolido BA, Boyer CA. How do people come to use mental health services? Current knowledge and changing perspectives. In: Horwitz AV, Scheid TL, editors. A handbook for the study of mental health: Social contexts, theories, and systems. New York: Cambridge University Press; 1999. [Google Scholar]
- 42.George LK, Blazer DG, Hughes DC, Fowler N. Social support and the outcome of major depression. British Journal of Psychiatry. 1989;154:478–485. doi: 10.1192/bjp.154.4.478. [DOI] [PubMed] [Google Scholar]
- 43.Lara ME, Leader J, Klein DN. The association between social support and course of depression: Is it confounded with personality? Journal of Abnormal Personality. 1997;106:478–482. doi: 10.1037//0021-843x.106.3.478. [DOI] [PubMed] [Google Scholar]
- 44.Garay-Sevilla ME, Nava LE, Malacara JM, Huerta R, Diaz de Leon J, Mena A, Fajardo ME. Adherence to treatment and social support in patients with non-insulin dependent diabetes mellitus. Journal of Diabetes Complications. 1995;9:81–86. doi: 10.1016/1056-8727(94)00021-f. [DOI] [PubMed] [Google Scholar]
- 45.Peyrot M, McMurry JF, Kruger DF. A biopsychosocial model of glycemic control in diabetes: Stress, coping, and regimen adherence. Journal of Health and Social Behavior. 1999;40:141–158. [PubMed] [Google Scholar]
- 46.Schlenk EA, Hart LK. Relationship between health locus of control, health value, and social support and compliance of persons with diabetes mellitus. Diabetes Care. 1984;7:566–574. doi: 10.2337/diacare.7.6.566. [DOI] [PubMed] [Google Scholar]
- 47.Young P, Dewse M, Fergusson W, Kolbe J. Respiratory rehabilitation in chronic obstructive pulmonary disease: Predictors of nonadherence. European Respiratory Journal. 1999;13:855–859. doi: 10.1034/j.1399-3003.1999.13d27.x. [DOI] [PubMed] [Google Scholar]
- 48.Muran JC, Segal ZV, Samstag LW, Crawford CE. Patient pretreatment interpersonal problems and therapeutic alliance in short-term cognitive therapy. Journal of Consulting and Clinical Psychology. 1994;62:185–190. doi: 10.1037//0022-006x.62.1.185. [DOI] [PubMed] [Google Scholar]
- 49.Sarason IG, Sarason BR, Shearin EN. Social support as an individual difference variable: Its stability, origins, and relational aspects. Journal of Personality and Social Psychology. 1986;50:845–855. [Google Scholar]
- 50.Kaplan JB, Bennett T. Use of race and ethnicity in biomedical publication. Journal of the American Medical Association. 2003;289(20):2709–2716. doi: 10.1001/jama.289.20.2709. [DOI] [PubMed] [Google Scholar]
- 51.Gallo JJ, Bogner HR, Morales KH, Ford DE. Patient ethnicity and the identification and active management of depression. Archives of Internal Medicine. 2005;165:1962–1968. doi: 10.1001/archinte.165.17.1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cooper LA, Gonzales JJ, Gallo JJ, Rost KM, Meredith LS, Rubenstein LV, Wang NY, Ford DE. The acceptability of treatment for depression among African-American and white primary care patients. Medical Care. 2003;41(4):479–489. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- 53.Marsiske M, Willis SL, Goodwin PE, Maier H. Relationships among cognitive processes, intellectual abilities, and everyday task performance. Paper presented at the Fourth Cognitive Aging Conference; Atlanta, Georgia. April 9-12; 1995. [Google Scholar]
- 54.Willis SL. Everyday cognitive competence in elderly persons: Conceptual issues and empirical findings. Gerontologist. 1996;36:595–601. doi: 10.1093/geront/36.5.595. [DOI] [PubMed] [Google Scholar]
- 55.Willis SL, Jay GM, Diehl M, Marsiske M. Longitudinal change and prediction of everyday task competence in the elderly. Research on Aging. 1992;14:68–91. doi: 10.1177/0164027592141004. [DOI] [PMC free article] [PubMed] [Google Scholar]


