Abstract
Objective
An important component of generalizing study results to patients is the extent to which study participants adequately represent individuals targeted for the study. The Spectrum study of depression in older primary care patients was utilized to consider patient characteristics associated with nonparticipation.
Method
Interviewers utilized a validated questionnaire to screen adults aged 65 years and older for depression who presented to one of the participating primary care practices in the Baltimore, Maryland area. Screening interviews included information about sociodemographic factors, functioning, health, and attitudes about depression and its treatment in order to compare participants with persons who declined.
Results
In all, 2,560 adults aged 65 years and older were screened. Comparison of the characteristics of the patients who were eligible for the study (n = 773) with patients who participated fully in the in-home evaluation (n = 355) found that the study sample included proportionately more persons who: 1) were less than 80 years old; 2) completed high school; and 3) reported two or more visits to the practice site within six months of the interview. Among patients who were depressed, no significant differences were found in the characteristics of those who met study eligibility criteria and those who agreed to participate.
Conclusions
Persons over the age of 80 years of age or those with less than a high school education may require tailored strategies for recruitment even when approached by a trained interviewer in a primary care doctor's office.
Keywords: aged, depression, patient participation, primary health care, research design
Introduction
Depression is associated with enormous suffering and disability. According to a recent report by the World Health Organization, Major Depression, which was the fourth leading cause of disability worldwide in 1990, will be second only to heart disease in 2020 as a cause of disability [1]. Depression is a treatable illness that disproportionately places older adults at increased risk for functional and cognitive decline [2]. Suicide rates increase with advancing age and appear to be increasing among the elderly throughout the world [3, 4]. For older adults, primary care providers will continue to play a pivotal role in initial management of depression [5, 6]. From the view of public health, if disability due to depression is to be minimized in the population, identification and management in the primary care setting is critical [7-9].
In this article we describe a study that was designed to investigate depressive symptoms among older primary care patients seen in community primary care practices. Practice-based research has the potential to answer clinically-relevant questions about depression in late life in community settings, and may provide information that is applicable to everyday practice settings [10]. We describe the process of recruitment of primary care practices and patients to the Spectrum Study, an in-home assessment and follow-up study of depression in late life. A similar study protocol could be employed to investigate other conditions in primary care settings. The design involves screening in the doctor's office with subsequent in-home assessment and follow-up in order to minimize interference with patient care. Specifically, previous investigators have observed that older ethnic minority adults may be reluctant to participate in research [11, 12]. Recruiting patients in person in the doctor's office, in contrast to screening patients with more impersonal methods such as the telephone [13, 14], was expected to result in a sample that was representative of the patients who were attending the participating practices and would not lead to higher nonparticipant rates for ethnic minority patients.
The Spectrum Study focuses on the presentation and course of depression in older primary care patients. The Spectrum study consists of three closely-linked projects whose purpose is to investigate: 1) depressive symptoms that do not meet standard criteria for major depression; 2) how depressive symptoms, cognitive change, and apolipoprotein E (APOE) genotype may interact to increase risk for functional impairment; and 3) the construct of depression and its treatment from the patient's point of view, mixing epidemiological and anthropological methods to contrast perspectives across ethnic groups. We attempted to obtain demographic and other information on all patients who agreed to answer a few questions in order that we could compare the characteristics of participants and non-participants in the final household sample. An understanding of which patients are likely to participate in studies of depression carried out in primary care settings can assist planning research in real world settings. We hypothesized that functional status and self-rated health as well as attitudes toward depression might be important determinants of the decision to participate in a research study about depression in older adults [15], even after controlling for sociodemographic characteristics.
Method
Overview of the Design of the Spectrum Study
The design of the Spectrum Study called for screening patients in the offices of primary care physicians for depression. Patients who were eligible based on several criteria were asked to participate in an initial in-home and subsequent follow-up interviews. The same interviewer who screened the patient in the doctor's office completed the follow-up interviews. Specifically, we invited the screened patients with the following sampling probabilities: 1) 100% who scored above threshold on a standard assessment of depressive symptoms (described below); 2) 50% who scored below threshold but were currently taking medications for sleep, pain, or an emotional problem; and 3) 10% who scored below threshold and were not currently taking medications for sleep, pain, or an emotional problem. The rationale for the different sampling probabilities was to develop a sample of older adults which was enriched with patients with depressive symptoms and with patients who may not currently be depressed but who may nonetheless be at risk for depression or whose depression may be in remission. Specifically, persons who are currently taking medication for sleep, pain, or an emotional problem might have or be at risk for significant depressive symptoms but might not meet standard criteria for depression over time. Persons in this group might be less willing to participate in a research study targeting depression. Patients who were eligible and agreed to the in-home interview and follow-up study were interviewed in their home concerning their psychological, cognitive, and physical health. The patient was asked to complete a questionnaire on personality and memory functioning, an informant who knows the patient was identified and interviewed on the telephone, and a buccal swab was requested for APOE genotyping and DNA banking [16]. Physicians also completed a brief questionnaire assessing their opinion of the patient's mental and physical health. The study protocols were approved by the Institutional Review Board of the University of Pennsylvania School of Medicine. A Certificate of Confidentiality was obtained from the Department of Health and Human Services as an additional safeguard for survey and genetic data.
Recruitment of Practices
We were interested in recruiting physicians who were not residents or faculty in residency training programs. We used the membership list of the Maryland Academy of Family Physicians (MAFP) and focused our recruiting efforts on physicians whose address fell within Baltimore City or one of four surrounding Maryland counties (Anne Arundel, Harford, Carroll, and Baltimore County). The geographic area was limited to central Maryland in order to avoid extensive travel time and costs of interviewing. A mailing sent to 469 physicians in the target area included a flyer describing the project, articles about the study that appeared in Maryland Family Doctor (the professional publication of the MAFP), a copy of the physician assessment form to be used in the study, and a fax page requesting that interested physicians contact the Academy. We also randomized the list of 469 members whose address was in the target area and stratified the sampling frame according to whether the address was in Baltimore City or in the surrounding counties. We then called the members in randomized order. We offered $200 per 100 patients screened for each participating physician and a discount on CME programs offered by MAFP as a token of appreciation.
At each of 27 practices where a physician expressed an interest in the study, the Principal Investigator, study staff, and the Project Director from the Battelle Memorial Institute's Center for Public Health Research and Evaluation met with the physicians and office staff to discuss the study aims and how the screening might be carried out in the practice setting without interfering with patient care. We recruited 16 practices into the study but, in three practices, no satisfactory arrangement could be arranged despite initial enthusiasm to participate. In all, 47 physicians (28 family physicians and 19 internists) from 13 practices contributed patients who participated in the Spectrum study. Because many family physicians practice with internists, the sample of participating physicians included both family physicians and internists.
Recruitment of Patients
Experienced lay interviewers were instructed in screening and study interviews. Training occurred over a two-day period and involved review of the rationale and procedures for administering the questionnaires and performance tests, with role play until the interviewers could competently carry out the combination of computerized interview and paper-and-pencil tests. Interviewers worked with front office staff at each practice to identify all patients aged 65 years and older. All such patients who came to a participating office were approached and asked to participate in a study of health and aging among patients in primary care settings. Patients were told their doctor had agreed to participate. Interviewers were trained not to interfere with the patient flow in the practice—patient care was to remain the top priority. At each practice, interviewers negotiated the procedures for screening patients in a private area and for obtaining a completed brief written patient assessment from the physicians.
An attempt was made to approach every patient aged 65 years and older who had an appointment during the time that the interviewer was in the waiting room. Patients were asked if they would answer a few questions to see if they qualified for the study. Each patient who was approached was assigned a unique identification number by the interviewer, even if the patient refused any additional interviews in order to have an accurate denominator for calculating response rates. Patients were not paid for participating in the screening portion of the study; however, patients were told that $50 would be offered to them as a token of appreciation for each of two completed in-home interviews. Patients who completed the interview could decline to provide a buccal swab for APOE genotyping without forfeiting payment [16].
Screening Interview Measurement Strategy
The screening interview was designed to be administered in a private area in the physician's office and needed to be brief. We balanced the need for brevity with the desire to obtain some information with which to compare persons who were eligible for the study but who declined to participate. We used standard questions to obtain information from the respondents on age, gender, self-reported ethnicity, marital status, living arrangements, and level of educational attainment.
Centers for Epidemiologic Studies Depression Scale
The Centers for Epidemiologic Studies Depression (CES-D) scale was developed by the Center for Epidemiologic Studies at the National Institute of Mental Health for use in studies of depression in community samples [17-19]. The CES-D contains 20 items, and has been employed in studies of older adults [e.g., 20, 21]. Somatic complaints on the CES-D increase as medically ill patients experience depression, but do not necessarily increase “false-positives” [22, 23]. Screening instruments that give undue weight to sadness would miss potentially important presentations of depression in primary care, especially among older patients. In the Spectrum Study, we employed a threshold of 17 or above as indicative of significant depressive symptoms [24].
Functional and Health Status
Questions were adapted from the SF-36 to assess functional status [25]. Specifically, all screened patients were asked about their ability to walk and to climb stairs. In addition, a single question on self-rated health was asked. We also asked patients to report how often they had been to the primary care doctor office in the six months prior to the screening interview.
Attitudes toward Depression and Its Treatment
We asked patients whether they agreed or disagreed with three statements about depression and its treatment [26]. The statements were “I believe depression is a medical problem,” “If my doctor told me I had depression, I could accept that,” and “I would take a medicine for depression if my doctor told me to.”
Analytic Strategy
Our analytic strategy was primarily descriptive and proceeded in two phases. First, we compared the characteristics of patients who were eligible for the study with characteristics of the subset of patients who comprised the final household sample for home interview and follow-up. Second, we examined which patient characteristics were associated with participation among eligible patients who had one of the three reasons for sampling (namely, scored above the CES-D threshold, used medications for sleep, pain, or an emotional problem, or randomly sampled). We employed simple χ2 tests for comparison of proportions. We have used exact methods based on marginal distributions to avoid reliance on large sample theory [27]. Multivariate logistic regression was used to adjust measures of association when appropriate [28]. In these analyses, we have employed a level of statistical significance set at α = 0.05, recognizing that tests of statistical significance are approximations that serve as aids to interpretation and inference.
Results
Study Sample
In all, 3,903 persons were approached and 3,542 agreed to answer a question about their age (91% participation rate). Of 3,459 persons aged 65 years and older, 2,560 answered the screening questionnaire (74% participation rate). We have no further information for the 899 persons over age 65 years who declined further participation. The disposition of the 2,560 persons who allowed additional questions in the doctor's office is shown in Figure 1. We asked 773 to participate based on their responses to the screening interview and 357 were interviewed in their homes (46% participation rate). Two persons broke off the interview before it was completed, leaving a sample of 355 persons. The modal time for the screening interview was 4 minutes, and 92% of the 2,560 screened patients were screened in 20 minutes or less. To obtain this sample who participated, four interviewers worked in the 13 practices for a mean of 20.6 weeks (standard deviation 13.5 weeks). The screening interviews took place over a total period of 66 weeks.
Figure 1.
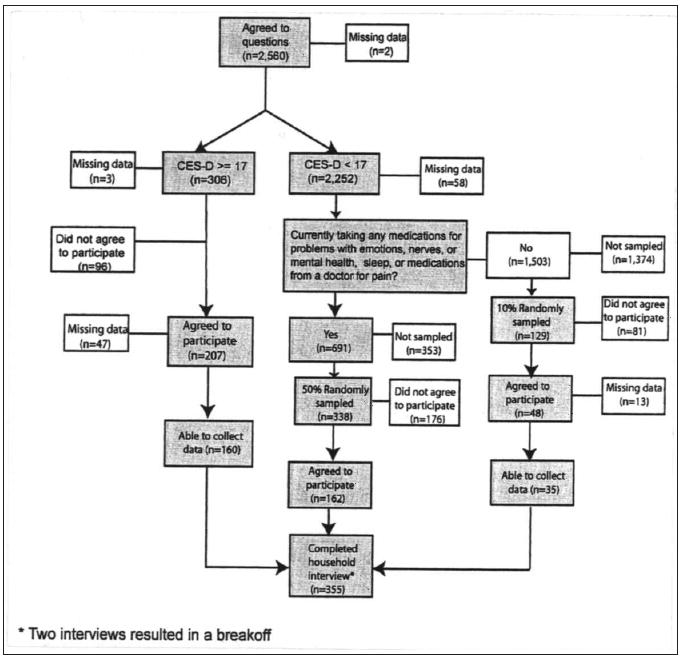
Patient recruitment in practice-based study. In all, 3,459 patients aged 65 years and older were approached and 2,560 gave permission for additional questions. CESD, Centers for Epidemiologic Studies Depression Scale.
Representativeness of the Patient Study Sample
Comparison of the characteristics of the patients who met criteria for the study with the patients who actually participated in the in-home evaluation revealed several differences. Participants were more likely to be younger than 80 years of age and were more likely to have attained a high school education (Table 1). Patients who reported two or more visits to the practice site within six months of interview were more likely than others to have participated in the study. There was a tendency for the study sample to include more patients who endorsed a willingness to take medication if recommended by their doctor (p = 0.05). Ethnicity, gender, living arrangements, and marital status were not significantly associated with participation. Functional status, self-rated health, and attitudes about depression were not strongly related to participation. In multivariate models, education was independently associated with participation even after adjustment for age, number of visits to the practice in the six months prior to interview, and attitude toward taking medication for depression.
Table 1.
Characteristics of the Patients in the Spectrum Study
| Screened (n = 2,560) |
Eligible (n = 773) |
Study sample (n = 355) |
p-Valuea | |
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Gender | ||||
| Women | 1,806 (72%) | 577 (75%) | 270 (76%) | .71 |
| Age in years | ||||
| 65 to 69 | 408 (16%) | 118 (15%) | 67 (19%) | .02 |
| 70 to 79 | 1,286 (51%) | 398 (52%) | 204 (57%) | |
| 80 and older | 866 (34%) | 257 (33%) | 84 (24%) | |
| Ethnicity | ||||
| African American | 779 (30%) | 228 (30%) | 117 (33%) | .51 |
| Educational attainment | ||||
| Less than high school | 1,164 (46%) | 382 (50%) | 145 (41%) | .01 |
| Living arrangements | ||||
| Lives alone | 946 (38%) | 308 (40%) | 134 (38%) | .51 |
| Marital status | ||||
| Married | 1,039 (41%) | 294 (38%) | 141 (40%) | .81 |
| Depressive symptoms | ||||
| CES-D score | ||||
| Above threshold 16/17 | 306 (12%) | 306 (40%) | 160 (45%) | .09 |
| Functional status | ||||
| Health limits my ability to climb stairs | 694 (28%) | 320 (42%) | 164 (46%) | .14 |
| Health limits my ability to walk | 957 (38%) | 406 (53%) | 200 (56%) | .25 |
| Self-rated health | ||||
| Excellent, very good, or good | 1,696 (68%) | 409 (53%) | 193 (54%) | .93 |
| Fair or poor | 806 (32%) | 357 (47%) | 160 (46%) | |
| Visits to the practice in the last six months | ||||
| 1 visit | 517 (20%) | 127 (16%) | 58 (16%) | .03 |
| 2 visits | 1,279 (50%) | 352 (46%) | 134 (38%) | |
| More than 2 visits | 748 (29%) | 294 (38%) | 163 (46%) | |
| Attitudes about depression (agreement with statement) | ||||
| I believe depression is a medical problem. | 1,702 (67%) | 541 (70%) | 257 (72%) | .44 |
| If my doctor told me I had depression I could accept that. | 1,889 (74%) | 610 (79%) | 291 (82%) | .26 |
| I would take a medicine for depression if my doctor told me to. | 1,994 (78%) | 640 (83%) | 310 (87%) | .05 |
The p-values represent comparison of the eligible sample with the study sample.
Representativeness of Patient Sample According to Reason for Recruitment
We compared the characteristics of patients who were eligible for the study with the patients who participated according to the reason for recruitment into the study. Factors related to participation differed according to the reason the person was being recruited into the sample (Table 2). Among persons who scored above the threshold on the CES-D, characteristics of participants were not significantly different from persons who were eligible but declined the invitation to participate. Among persons who were sampled because they were taking medication for sleep, pain, or an emotional problem, participants were younger and more likely to have completed high school than were persons who declined participation. Among persons who were selected from the remainder of the screened patients and had no definite depression, men and persons who had completed high school were more likely to participate. Ethnicity, living arrangements, marital status, functional status, self-rated health, and attitudes about depression were not related to participation in any of the three components of the sample.
Table 2.
Characteristics of Patients Aged 65 Years and Older Who Agreed to Participate in the Spectrum Study, According to Reason for Recruitment into the Samplea
| Above CES-D threshold | Below CES-D threshold, but currently taking medication for sleep, pain, or an emotional problem | Sampled from remainder of screened participants | ||||
|---|---|---|---|---|---|---|
| Sociodemographics | Eligible (n = 306) |
Participated (n = 160) |
Eligible (n = 338) |
Participated (n = 160) |
Eligible (n = 129) |
Participated (n = 35) |
| Gender | ||||||
| Women | 242 (79%) | 130 (81%) | 253 (75%) | 119 (74%) | 82 (64%) | 14 (40%) |
| exact p-value = 0.81 | exact p-value = 0.91 | exact p-value = 0.02 | ||||
| Age in years | ||||||
| 65 to 69 | 55 (18%) | 33 (21%) | 40 (12%) | 29 (18%) | 23 (18%) | 5 (14%) |
| 70 to 79 | 117 (52%) | 85 (53%) | 182 (53%) | 96 (60%) | 63 (49%) | 23 (66%) |
| 80 and older | 98 (32%) | 42 (26%) | 116 (34%) | 35 (22%) | 43 (33%) | 7 (20%) |
| exact p-value = 0.62 | exact p-value = 0.02 | exact p-value = 0.30 | ||||
| Ethnicity | ||||||
| African American | 82 (27%) | 55 (34%) | 102 (30%) | 48 (30%) | 44 (34%) | 14 (40%) |
| exact p-value = 0.21 | exact p-value = 0.81 | exact p-vlaue = 0.81 | ||||
| Educational attainment | ||||||
| Less than high school | 151 (49%) | 69 (43%) | 176 (52%) | 68 (43%) | 55 (43%) | 8 (23%) |
| exact p-value = 0.17 | exact p-value = 0.05 | exact p-value = 0.05 | ||||
| Living arrangements | ||||||
| Lives alone | 129 (42%) | 68 (43%) | 130 (39%) | 54 (34%) | 49 (38%) | 12 (34%) |
| exact p-value = 0.99 | exact p-value = 0.07 | exact p-value = 0.70 | ||||
| Marital status | ||||||
| Married | 101 (33%) | 52 (33%) | 134 (40%) | 73 (46%) | 59 (46%) | 16 (46%) |
| exact p-value = 0.97 | exact p-value = 0.58 | exact p-value = 0.70 | ||||
| Functional status | ||||||
| Health limits my ability to climb stairs | 172 (56%) | 203 (66%) | 117 (35%) | 57 (36%) | 31 (24%) | 14 (40%) |
| exact p-value = 0.69 | exact p-value = 0.84 | exact p-value = 0.09 | ||||
| Health limits my ability to walk | 203 (66%) | 110 (69%) | 168 (50%) | 79 (49%) | 35 (27%) | 11 (31%) |
| exact p-value = 0.61 | exact p-value = 0.99 | exact p-value = 0.67 | ||||
| Self-rated health | ||||||
| Excellent, very good, or good | 103 (34%) | 60 (47%) | 211 (62%) | 110 (69%) | 95 (73%) | 23 (68%) |
| Fair or poor | 198 (65%) | 100 (63%) | 126 (37%) | 49 (31%) | 33 (26%) | 11 (32%) |
| exact p-value = 0.61 | exact p-value = 0.99 | exact p-value = 0.67 | ||||
| Visits to the practice in the last six months | ||||||
| 1 visit | 40 (13%) | 17 (11%) | 53 (16%) | 33 (21%) | 34 (26%) | 8 (23%) |
| 2 visits | 111 (36%) | 54 (34%) | 173 (51%) | 65 (41%) | 68 (53%) | 15 (43%) |
| More than 2 visits | 155 (51%) | 89 (56%) | 112 (33%) | 62 (39%) | 27 (21%) | 12 (34%) |
| exact p-value = 0.55 | exact p-value = 0.08 | exact p-value = 0.27 | ||||
| Attitudes about depression (agreement with statement) | ||||||
| I believe depression is a medical problem. | 217 (71%) | 118 (74%) | 236 (70%) | 118 (74%) | 88 (68%) | 21 (60%) |
| exact p-value = 0.59 | exact p-value = 0.40 | exact p-value = 0.42 | ||||
| If my doctor told me I had depression, I could accept that. | 254 (83%) | 138 (86%) | 262 (78%) | 132 (83%) | 94 (73%) | 21 (60%) |
| exact p-value = 0.42 | exact p-value = 0.24 | exact p-value = 0.15 | ||||
| I would take a medicine for depression if my doctor told me to. | 245 (80%) | 134 (84%) | 299 (89%) | 150 (94%) | 96 (74%) | 26 (74%) |
| exact p-value = 0.38 | exact p-value = 0.08 | exact p-vlaue = 0.99 | ||||
Numbers in parentheses are percent of persons with specific characteristics (in rows) who participated from a given recruitment category (in columns). CES-D, Center for Epidemiologic Studies Depression scale.
Discussion
Our expectations about patient characteristics that might be associated with participation, such as diminished functional status, were not supported. Younger age and higher level of educational attainment were the primary predictors of participation. This investigation differs from other descriptions of practice-based research because: 1) our study focused on older adults [c.f., 29]; 2) the participating doctors work in practices that were not affiliated with academic or training settings [c.f., 30, 31]; and 3) older patients were not asked to participate in a study with an intervention which might have introduced selection bias due to reluctance to be identified as depressed or to accept random assignment to an intervention [e.g., 13, 32, 33]. Only advanced age and educational status less than high school were characteristics associated with patients being less likely to participate. We did not find that African Americans or persons with functional impairment were less likely than others to participate in contrast to other research [11, 12, 34]. We suspect that approaching patients in person in the doctor's office may have increased willingness to be asked an initial set of screening questions. Nevertheless, patients aged 80 years and older and persons with less than a high school education were reluctant to permit the interviewer into their home (even an interviewer with whom they had developed some rapport).
This study has limitations which must be acknowledged before discussing findings. First, it was carried out in a single metropolitan area. Second, practices and patients who participated may differ in unmeasured ways from practices and patients who did not participate. Our ability to assess the characteristics of the practices and physicians who participated was limited. We did not ask patients to be randomized or to participate in a treatment trial, so these results may not be applicable to patients who would participate in treatment trials. Patients who made more visits to their primary care physician and who therefore more likely to be exposed to screening in the study may differ in health from older patients who made fewer visits but were more likely to be exposed to screening in the study. Investigators that employ this design must recognize that the sample will consist of persons who have made multiple visits to the practice. Investigators that employ this design must decide whether the sample should be representative of the practice in terms of visits or persons.
In summary, patients who were younger and who completed high school, and patients who made more frequent visits to the practice where the recruitment took place, were more likely to participate than were other patients. Ethnicity, gender, living arrangements, marital status, functional status, self-rated health, and depressive symptoms and attitudes about depression were not associated with participation. There was a tendency for persons who expressed a favorable attitude toward taking medicine for depression to be more likely to participate but this did not reach conventional levels of statistical significance. Our recruitment strategy from the offices of primary care practices resulted in a sample of patients aged 65 years and older who were similar in key characteristics to the persons who were screened and met the study eligibility requirements.
Despite limitations, we believe our experience in carrying out this field survey is important because we have tried to assess participant characteristics beyond simple demographics at each stage of the study sampling scheme. We did not include practices with academic ties because we wanted our study results to be more representative of patients in community primary care practices. We employed trained interviewers to conduct the interviews rather than asking overburdened physicians and office staff. We sought to understand how personal characteristics might be related to participation in a field study in primary care practices that can inform other work among older primary care patients.
The clinical trials literature has reported that older adults, African Americans, and persons with less than a high school education may be reluctant to participate in research [35-39]. We have reported elsewhere that patients aged 80 years and older and African Americans were less likely than others to provide a buccal swab for APOE genotyping [16]. Depressive symptoms and functional status were not significantly related to providing a genetic sample. Thus, while older African Americans were hesitant to provide a swab of the cheek for genetic analysis, they were no less likely to participate in the in-home assessment than were white patients.
We attempted to anticipate some of the issues involved in recruiting older patients, such as the use of a large font in informed consent documents and in-home interviews. Nevertheless, our results suggest that those over 80 years of age and with less than a high school education may need additional recruitment resources to be certain they are not underrepresented. This may require simplified consent procedures where less reading is needed and more involvement of trusted family members. Among older adults, about one-third of potential participants in research refused to participate because their families or physicians discouraged them from doing so [11]. Some older persons may have been reluctant to have an interviewer to their home, and increased ability to carry out interviews elsewhere may have been helpful. The terms used to describe the research during verbal recruitment may also need to be tailored for these groups. Confidentiality was mentioned as a major reason why older patients in the Spectrum Study did not want to provide a genetic sample [16], so reassurance early in the recruitment process about confidentiality of interview data might be useful.
The NIMH Clinical Treatment and Services Research Workgroup report, Bridging Science and Service, pointed out that research findings seldom leave the pages of research journals to find their way into “real world” settings [40]. We are not likely to find answers to our clinical questions based on studies carried out in specialty settings because patients in primary care have a distinct spectrum of disease, are seen early in the course of illness, and have different expectations about their care. Assessing the personal characteristics that may be associated with participation is particularly important for research on depression because the illness we are studying may itself influence participation. Primary care investigators should consider collecting data beyond study eligibility criteria or screening tests in order to better characterize participants and to increase understanding of the factors related to willingness to participate in primary care research.
Acknowledgments
The investigators gratefully acknowledge the patients who participated; the assistance of the Maryland Academy of Family Physicians, Baltimore, Maryland (Esther Barr, Executive Director); physicians and office staffs of the participating practices; and the interviewers and supervising staff of the Battelle Memorial Institute's Centers for Public Health Research, Baltimore, Maryland (Pat Lesho, Project Manager). A list of members of the Spectrum Study work groups can be found at www.uphs.upenn.edu/spectrum.
Footnotes
The Spectrum Study was supported by grants MH62210-01, MH62210-01S1, and MH67077 from the National Institute of Mental Health. Dr. Bogner was supported by a NIMH Mentored Patient-Oriented Research Career Development Award (MH67671-01) and was the Project Director for the Spectrum Study.
Contributor Information
Joseph J. Gallo, University of Pennsylvania, Philadelphia.
Hillary R. Bogner, University of Pennsylvania, Philadelphia.
Joseph B. Straton, University of Pennsylvania, Philadelphia.
Katherine Margo, University of Pennsylvania, Philadelphia.
Pat Lesho, Battelle Memorial Institute, Baltimore.
Peter V. Rabins, Johns Hopkins University, Baltimore, Maryland.
Daniel E. Ford, Johns Hopkins University, Baltimore, Maryland.
References
- 1.Murray CJL, Lopez AD. The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Cambridge, MA: Harvard University Press; 1996. [Google Scholar]
- 2.Gallo JJ, Lebowitz BD. The epidemiology of common late-life mental disorders in the community: Themes for the new century. Psychiatric Services. 1999;50:1158–1168. doi: 10.1176/ps.50.9.1158. [DOI] [PubMed] [Google Scholar]
- 3.Bruce ML, Pearson JL. Designing an intervention to prevent suicide: PROSPECT (Prevention of Suicide in Primary Care Elderly: Collaborative Trial) Dialogues in Clinical Neuroscience. 1999;1:100–112. doi: 10.31887/DCNS.1999.1.2/mbruce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taylor SJ, Kingdom D, Jenkins R. How are nations trying to prevent suicide? An analysis of national suicide prevention strategies. Acta Psychiatrica Scandinavica. 1997;95:457–463. doi: 10.1111/j.1600-0447.1997.tb10132.x. [DOI] [PubMed] [Google Scholar]
- 5.Gallo JJ, Marino S, Ford D, Anthony JC. Filters on the pathway to mental health care: II. Sociodemographic factors. Psychological Medicine. 1995;25:1149–1160. doi: 10.1017/s0033291700033122. [DOI] [PubMed] [Google Scholar]
- 6.Rabins PV. Prevention of mental disorders in the elderly: Current perspectives and future prospects. Journal of the American Geriatrics Society. 1992;40:727–733. doi: 10.1111/j.1532-5415.1992.tb01968.x. [DOI] [PubMed] [Google Scholar]
- 7.Wells KB. Treatment research at the crossroads: The scientific interface of clinical trials and effectiveness research. American Journal of Psychiatry. 1999;156:5–10. doi: 10.1176/ajp.156.1.5. [DOI] [PubMed] [Google Scholar]
- 8.Kramer M, Simonsick E, Lima B, Levav I. The epidemiological basis for mental health care in primary health care: A case for action. In: Cooper B, Eastwood R, editors. Primary health care and psychiatric epidemiology. New York: Tavistock/Routledge; 1992. pp. 69–98. [Google Scholar]
- 9.Gallo JJ, Coyne JC. The challenge of depression in late life: Bridging science and service in primary care, editorial. JAMA. 2000;284:1570–1572. doi: 10.1001/jama.284.12.1570. [DOI] [PubMed] [Google Scholar]
- 10.Nutting PA, Beasley JW, Werner JJ. Practice-based research networks answer primary care questions. JAMA. 1999;281:686–688. doi: 10.1001/jama.281.8.686. [DOI] [PubMed] [Google Scholar]
- 11.Carter WB, Elward K, Malmgren J, Martin ML, Larson E. Participation of older adults in health programs and research: A critical review of the literature. The Gerontologist. 1991;33:584–592. doi: 10.1093/geront/31.5.584. [DOI] [PubMed] [Google Scholar]
- 12.Ballard EL, Nash F, Raiford K, Harrell LE. Recruitment of Black elderly for clinical research studies of dementia: The CERAD experience. The Gerontologist. 1993;33:561–565. doi: 10.1093/geront/33.4.561. [DOI] [PubMed] [Google Scholar]
- 13.Bruce ML, Ten Have TR, Reynolds CF, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: A randomized controlled trial. JAMA. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 14.Unützer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: A randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 15.Cooper LA, Gonzales JJ, Gallo JJ, et al. The acceptability of treatment for depression among African-American and white primary care patients. Medical Care. 2003;41:479–89. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- 16.Bogner HR, Wittink M, Merz JF, et al. Personal characteristics of older primary care patients who provide a buccal swab for APOE testing and banking of genetic material: The Spectrum Study. Community Genetics. 2004;7:202–210. doi: 10.1159/000082263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 18.Comstock GW, Helsing KJ. Symptoms of depression in two communities. Psychological Medicine. 1976;6:551–563. doi: 10.1017/s0033291700018171. [DOI] [PubMed] [Google Scholar]
- 19.Eaton WW, Kessler LG. Rates of symptoms of depression in a national sample. American Journal of Epidemiology. 1981;114:528–538. doi: 10.1093/oxfordjournals.aje.a113218. [DOI] [PubMed] [Google Scholar]
- 20.Newmann JP, Engel RJ, Jensen J. Age differences in depressive symptom experiences. Journals of Gerontology: Psychological Sciences. 1991;46:224–235. doi: 10.1093/geronj/46.5.p224. [DOI] [PubMed] [Google Scholar]
- 21.Gatz M, Johansson B, Pedersen N, Berg S, Reynolds C. A cross-national self-report measure of depressive symptomatology. International Psychogeriatrics. 1993;5:147–156. doi: 10.1017/s1041610293001486. [DOI] [PubMed] [Google Scholar]
- 22.Foelker GA, Shewchuk RM. Somatic complaints and the CES-D. Journal of the American Geriatrics Society. 1992;40:259–262. doi: 10.1111/j.1532-5415.1992.tb02079.x. [DOI] [PubMed] [Google Scholar]
- 23.Lyness JM, Noel TK, Cox C, King DA, Conwell Y, Caine ED. Screening for depression in elderly primary care patients: A comparison of the Center for Epidemiologic Studies-Depression Scale and the Geriatric Depression Scale. Archives of Internal Medicine. 1997;157:449–454. [PubMed] [Google Scholar]
- 24.Katon W, Schulberg HC. Epidemiology of depression in primary care. General Hospital Psychiatry. 1992;14:237–247. doi: 10.1016/0163-8343(92)90094-q. [DOI] [PubMed] [Google Scholar]
- 25.McHorney CA. Measuring and monitoring general health status in elderly persons: Practical and methodological issues in using the SF-36 health survey. Gerontologist. 1996;36:571–583. doi: 10.1093/geront/36.5.571. [DOI] [PubMed] [Google Scholar]
- 26.Cooper KG. The impact of using a partially randomised patient preference design when evaluating alternative managements for heavy menstrual bleeding. British Journal of Obstetrics and Gynaecology. 1997;104:1367–1373. doi: 10.1111/j.1471-0528.1997.tb11005.x. [DOI] [PubMed] [Google Scholar]
- 27.Armitage P, Berry G. Statistical methods in medical research. 2nd. London: Blackwell Scientific Publications; 1987. [Google Scholar]
- 28.Hosmer DW, Lemeshow S. Applied logistic regression. 2nd. New York: John Wiley & Sons; 2000. [Google Scholar]
- 29.Klinkman MS, Okkes I. Mental health problems in primary care: A research agenda. Journal of Family Practice. 1998;47:379–384. [PubMed] [Google Scholar]
- 30.Callahan CM, Nienaber NA, Hendrie HC, Tierney WM. Depression of elderly outpatients: Primary care physicians' attitudes and practice patterns. Journal of General Internal Medicine. 1992;7:26–31. doi: 10.1007/BF02599097. [DOI] [PubMed] [Google Scholar]
- 31.Shao WA, Williams JW, Lee S, Badgett RG, Aaronson B, Cornell JE. Knowledge and attitudes about depression among non-generalists and generalists. Journal of Family Practice. 1997;44:161–168. [PubMed] [Google Scholar]
- 32.Stevens T, Katona C, Manela M, Watkin V, Livingston G. Drug treatment of older people with affective disorders in the community: Lessons from an attempted clinical trial. International Journal of Geriatric Psychiatry. 1999;14:467–472. doi: 10.1002/(sici)1099-1166(199906)14:6<467::aid-gps956>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 33.Unützer J, Katon W, Callahan CM, et al. Depression treatment in a sample of 1,801 depressed older adults in primary care. Journal of the American Geriatrics Society. 2003;51(4):505–514. doi: 10.1046/j.1532-5415.2003.51159.x. [DOI] [PubMed] [Google Scholar]
- 34.Shavers-Hornaday VL, Lynch CF, Burmeister LF, Torner JC. Why are African Americans under-represented in medical research studies? Impediments to participation Ethnic Health. 1997;2:31–45. doi: 10.1080/13557858.1997.9961813. [DOI] [PubMed] [Google Scholar]
- 35.Corbie-Smith G, Viscoli C, Kernan W, Brass L, Sarrel P, Horwitz R. Influence of race, clinical, and other socio-demographic features on trial participation. Journal of Clinical Epidemiology. 2003;56(4):304–309. doi: 10.1016/s0895-4356(03)00046-5. [DOI] [PubMed] [Google Scholar]
- 36.Sateren W, Trimble E, Abrams J, et al. How sociodemographics, presence of oncology specialists, and hospital cancer programs affect accrual to cancer treatment trials. Journal of Clinical Oncology. 2002;20(8):2109–2117. doi: 10.1200/JCO.2002.08.056. [DOI] [PubMed] [Google Scholar]
- 37.Advani A, Atkeson B, Brown C, et al. Barriers to the participation of African-American patients with cancer in clinical trials: A pilot study. Cancer. 2003;97(6):1499–1506. doi: 10.1002/cncr.11213. [DOI] [PubMed] [Google Scholar]
- 38.Rimer BK, Schildkraut JM, Lerman C, Hsiang T, Audrain J. Participation in a woman's breast cancer risk counseling trial: Who participates? Who declines? Cancer. 1996;77:2348–2355. doi: 10.1002/(SICI)1097-0142(19960601)77:11<2348::AID-CNCR25>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 39.Gallagher RA, Miller C, Cronan TA, Groessi E. Gender differences in participation and responsiveness to a health intervention for older Americans. Women & Health. 1997;25:63–81. doi: 10.1300/J013v25n03_05. [DOI] [PubMed] [Google Scholar]
- 40.Report of the National Advisory Mental Health Council's Clinical Treatment and Services Research Workgroup. Bridging science and service. Washington, DC: 1998. [Google Scholar]


