Abstract
Objective
To compare the clinical effectiveness of local corticosteroid injection, standard non-steroidal anti-inflammatory drugs, and simple analgesics for the early treatment of lateral epicondylitis in primary care.
Design
Multicentre pragmatic randomised controlled trial.
Setting
23 general practices in North Staffordshire and South Cheshire.
Participants
164 patients aged 18-70 years presenting with a new episode of lateral epicondylitis.
Interventions
Local injection of 20 mg methylprednisolone plus lignocaine, naproxen 500 mg twice daily for two weeks, or placebo tablets. All participants received a standard advice sheet and co-codamol as required.
Main outcome measures
Participants’ global assessment of improvement (five point scale) at four weeks. Pain, function, and “main complaint” measured on 10 point Likert scales at 4 weeks, 6 months, and 12 months.
Results
Over 2 years, 53 subjects were randomised to injection, 53 to naproxen, and 58 to placebo. Prognostic variables were similar between groups at baseline. At 4 weeks, 48 patients (92%) in the injection group were completely better or improved compared with 30 (57%) in the naproxen group (P<0.001) and 28 (50%) in the placebo group (P<0.001). At 12 months, 43 patients (84%) in the injection group had pain scores ⩽3 compared with 45 (85%) in the naproxen group and 44 (82%) in the placebo group (P>0.05).
Conclusions
Early local corticosteroid injection is effective for lateral epicondylitis. Outcome at one year was good in all groups, and effective early treatment does not seem to influence this.
Key messages
Most lateral epicondylitis is managed by general practitioners, but optimum treatment is unclear
This large pragmatic randomised trial showed that corticosteroid injection was significantly better than non-steroidal anti-inflammatories or placebo tablets at four weeks
A two week course of a standard non-steroidal anti-inflammatory was no better than placebo
A few patients who respond well initially to injection relapse by six months.
Long term outcome was good, irrespective of initial treatment allocation
Introduction
Lateral epicondylitis (tennis elbow) is a painful condition that affects about 4 adults per 1000 annually.1 Most cases are managed in primary care, and more than 40 possible treatments have been proposed,2 reflecting a lack of consensus about optimal management. General practitioners commonly use non-steroidal anti-inflammatory drugs to treat tennis elbow, but there are no trials comparing them with painkillers and one study found no clinically important benefit over placebo.3 Two reviews of corticosteroid injections concluded that there was insufficient evidence to support their use in treating tennis elbow, but the methodological quality of most trials was poor.4,5 Only two primary care studies were identified, both with methodological shortcomings, including small sample sizes. One, in an occupational health centre, showed no difference between injection, indomethacin, and a wrist brace over 12 months.6 The second, conducted in an army clinic, found no difference between ultrasound, transcutaneous nerve stimulation, and local injection five days after intervention.7
We conducted a large pragmatic randomised trial comparing three conventional treatments for lateral epicondylitis in primary care. The aims of the study were to determine whether local corticosteroid injection, a two week course of naproxen, or simple analgesia provides the best short term treatment for new episodes and which of these treatments provides best long term relief of symptoms.
Methods
Study design
The study was a multicentre, pragmatic randomised trial in primary care. We recruited consecutive patients aged 18-70 years who consulted their general practitioner with a new episode of lateral epicondylitis (pain and tenderness in the lateral region of the elbow and no consultation with symptoms in the same elbow during the preceding 12 months) during November 1995 to December 1997. Exclusion criteria were a history of inflammatory arthritis or gross structural abnormality of the elbow; contraindications to non-steroidal anti-inflammatories or local steroid injection; and pregnancy or breast feeding. The trial was explained to patients by their general practitioner, who gave participants an information leaflet and faxed a registration form to the research centre. Baseline assessments were performed by a study nurse (usually in the patients’ homes) within two working days of registration. Written informed consent was obtained, and the study was approved by the local research ethics committees of North Staffordshire and South Cheshire.
Randomisation
Treatment allocation was according to the study number given to the patient at the baseline assessment. Numbers were issued in a predetermined random sequence in blocks of six by general practice and generated with a random number table. The number corresponded with that on identical treatment packs kept in the general practitioners’ surgeries.
Treatment protocols
Patients returned to their general practitioner after the baseline assessment to receive one of three treatments.
Injection group—Patients were given a local corticosteroid injection of methylprednisolone 20 mg and 0.5 ml 1% lignocaine according to a standard technique. The injection was performed with the patient’s arm resting flexed on a firm surface. The methylprednisolone and lignocaine were drawn up in separate syringes. After the skin was cleaned, lignocaine was injected deep into the subcutaneous tissues and muscles 1 cm distal to the lateral epicondyle and aiming towards the tender spot. The syringes were then exchanged and methylprednisolone injected radially. The needle was withdrawn cleanly and firm pressure applied.
Naproxen group—Patients were prescribed enteric coated naproxen 500 mg twice daily for two weeks. Standard advice was given to take the drug with food and about potential side effects.
Placebo group—Patients were give placebo tablets (unmarked vitamin C) twice daily for two weeks. Standard advice was given as for the naproxen group.
Participants were provided with co-codamol for additional pain relief and an information leaflet about “tennis elbow” based on the Arthritis Research Campaign publication but omitting specific treatment recommendations.
Outcome measures
Outcome assessments were performed by a blinded study nurse before randomisation and at four weeks, six months, and 12 months. The baseline assessment also included demographic variables, medical history, and potential prognostic variables. Case notes were reviewed after completion of follow up.
The primary outcome was patients’ global assessment of change measured on a 5 point scale (complete recovery, improved, no change, worse, much worse) at four weeks. Secondary outcomes were pain severity (10 point Likert scale); impairment of function (10 point Likert scale); severity of “main complaint” (10 point Likert scale)8; disability (validated tennis elbow disability questionnaire)9; pain free grip strength in affected arm (average of two readings with hand held dynamometer); local tenderness of lateral epicondyle (3 point scale: none, some, definite with flinch); pain on resisted extension of middle finger and wrist with arm extended (3 point scale: none, some, definite with flinch); number and type of co-interventions (questionnaire and case note review); time off paid employment; complications of treatment (post-intervention exacerbation of pain (daily 10-point pain scale measured for five days), local skin atrophy, gastrointestinal side effects).
Analysis
Sample size calculations were based on publications which describe a 70% recovery or improvement with non-steroidal anti-inflammatory drugs after four weeks (two tailed α=0.05, β=0.2).10 Overall success was defined a priori as a 20% difference between treatment groups in the primary outcome measure. A total sample size of 180 patients was required.
Intention to treat analysis was performed blind to treatment group. All hypothesis tests were two tailed with α=0.05. We compared groups with χ2 test for nominal variables or Fisher’s exact test where appropriate for small samples. Ordinal variables were compared by Mann-Whitney U tests. Area under the curve slopes were compared by the methods of Matthews et al.11 Analyses were carried out with spss version 8.0.
Results
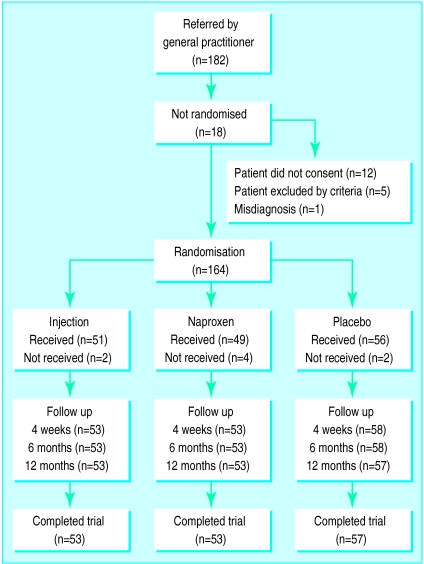
Thirty seven general practitioners from 23 practices registered 182 patients. Of these patients, 164 (78 women) were randomised: 53 to receive local injection, 53 to naproxen, and 58 to placebo. Eleven of the 37 general practitioners recruited six or more patients, accounting for 94 (57%) of the 164 in the study population (overall range recruited 1-17). Allocation of intervention and baseline patient characteristics were similar in high recruiting and low recruiting practices. The figure shows the progress of patients through the trial, and table 1 shows the baseline characteristics of the study sample.
Table 1.
Baseline characteristics of participants according to treatment group. Values are numbers (percentages) of participants*
| Injection (n=53) | Naproxen (n=53) | Placebo (n=58) | |
|---|---|---|---|
| Demography | |||
| Age (⩾45 years) | 37 (70) | 36 (68) | 36 (62) |
| Sex (male) | 31 (59) | 25 (47) | 30 (52) |
| Social class (manual) | 27 (66) | 22 (51) | 28 (57) |
| Pain | |||
| Elbow pain today | 50 (94) | 51 (96) | 57 (98) |
| Pain every day for 1 week | 50 (94) | 47 (89) | 50 (86) |
| Duration of pain >3 months | 19 (36) | 13 (25) | 18 (31) |
| Both elbows affected | 7 (13) | 4 (8) | 4 (7) |
| Previous episode(s) | 10 (19) | 11 (21) | 11 (19) |
| Belief that current episode was activity induced | 30 (57) | 25 (47) | 30 (52) |
| Work | |||
| Employed | 38 (72) | 38 (72) | 48 (83) |
| Time off work | 6 (16) | 0 (0) | 7 (15) |
| General health | |||
| Long standing medical condition | 25 (47) | 24 (45) | 18 (31) |
| Medication or pain killers in past 48 hours | 41 (77) | 36 (68) | 41 (71) |
| Appearance | |||
| Superficially normal joint | 49 (93) | 49 (93) | 55 (95) |
| Skin atrophy present | 0 (0) | 0 (0) | 0 (0) |
| Movement and strength | |||
| Grip strength >300 mm Hg | 3 (6) | 1 (2) | 1 (2) |
| Definite pain on resisted extension of middle finger | 18 (34) | 24 (45) | 20 (35) |
| Definite pain on resisted extension of wrist | 22 (42) | 25 (47) | 28 (48) |
| Definite tenderness | 23 (43) | 15 (28) | 24 (41) |
| Disability | |||
| Dressing | 32 (63) | 29 (55) | 31 (57) |
| Feeding | 41 (79) | 44 (85) | 42 (72) |
| Washing | 38 (76) | 41 (77) | 45 (80) |
| Household tasks | 50 (94) | 49 (93) | 55 (95) |
| Opening doors | 24 (47) | 24 (48) | 26 (47) |
| Carrying objects | 51 (96) | 49 (93) | 57 (98) |
| With work | 46 (90) | 47 (90) | 52 (91) |
| With sport | 36 (77) | 35 (85) | 42 (82) |
Percentages may not calculate exactly because of missing data.
At four weeks, outcome in the injection group was significantly better than in the naproxen and placebo groups (table 2). Naproxen showed no advantage over placebo. Recovery or improvement was reported in 48 patients (92%) in the injection group, 30 patients (57%) in the naproxen group, and 28 patients (50%) in the placebo group.
Table 2.
Outcome at four weeks after invention according to treatment group. Values are numbers (percentages) of patients
| Change in elbow | Injection* (n=52) | Naproxen (n=53) | Placebo (n=56) | Total (n=161) |
|---|---|---|---|---|
| Complete recovery | 22 (42) | 3 (6) | 2 (4) | 27 (17) |
| Some improvement | 26 (50) | 27 (51) | 26 (46) | 79 (49) |
| No change | 3 (6) | 16 (30) | 23 (41) | 42 (26) |
| Worse | 1 (2) | 7 (13) | 4 (7) | 12 (7) |
| Much worse | 0 (0) | 0 (0) | 1 (2) | 1 (1) |
P<0.05 compared with naproxen and with placebo.
Table 3 shows median scores for the Likert scales for pain, function, and “main complaint” at each follow up assessment. At four weeks, injection showed a clear advantage over naproxen and placebo. There were some small but significant differences in favour of naproxen or placebo at 6 and 12 months.
Table 3.
Median (interquartile range) pain and disability self assessment scores (Likert scale 0-9) in patients with lateral epicondylitis according to treatment group
| Time of assessment | Injection | Naproxen | Placebo |
|---|---|---|---|
| Elbow pain | |||
| Baseline | 6.0 (4.0-7.0) | 4.0 (2.75-6.25) | 5.0 (4.0-7.0) |
| 4 weeks*† | 1.0 (0.0-3.0) | 4.0 (2.0-6.0) | 3.5 (2.0-6.0) |
| 6 months*† | 2.0 (1.0-5.0) | 1.0 (0.0-3.0) | 1.0 (0.0-2.25) |
| 12 months | 1.0 (0.0-2.0) | 0.0 (0.0-2.0) | 0.0 (0.0-2.0) |
| Total score‡ | 221 (158-351) | 201 (131-312) | 188 (138-277) |
| Function | |||
| Baseline | 4.0 (2.0-5.0) | 4.0 (2.0-5.0) | 4.0 (2.0-5.0) |
| 4 weeks*† | 0.0 (0.0-2.0) | 3.0 (1.0-5.0) | 2.0 (1.0-4.0) |
| 6 months* | 1.0 (0.0-3.0) | 0.0 (0.0-2.75) | 0.5 (0.0-2.75) |
| 12 months† | 0.0 (0.0-2.0) | 0.0 (0.0-1.0) | 0.0 (0.0-0.0) |
| Total score‡ | 153 (91-234) | 157 (99-257) | 139 (106-227) |
| Main complaint | |||
| Baseline | 6.0 (4.0-7.0) | 5.0 (4.0-7.0) | 5.5 (3.0-7.0) |
| 4 weeks*† | 1.0 (0.0-2.0) | 4.0 (1.0-6.0) | 3.0 (1.0-5.0) |
| 6 months* | 2.0 (0.0-4.0) | 0.0 (0.0-3.0) | 1.0 (0.0-4.0) |
| 12 months* | 1.0 (0.0-3.75) | 0.0 (0.0-1.25) | 1.0 (0.0-3.75) |
| Total score‡ | 222 (129-340) | 180 (116-275) | 195 (141-361) |
P<0.05 for injection versus naproxen.
P<0.05 for injection versus placebo.
By area under the curve analysis.
The clinical interpretation of these differences was explored as follows. Comparison between the Likert scores for pain and participants’ global assessment of change at four weeks showed that 89% of subjects scoring ⩽3 rated themselves as completely better or improved; none had got worse. Based on this, outcome was dichotomised as “better” (pain score ⩽3) or “not better” (pain score ⩾4). This allowed us to compare the numbers of patients who had responded to treatment at each time point (table 4). Overall, 84% of recruited patients were better at 12 months, and this proportion was similar for each treatment group (injection 84%, naproxen 85%, placebo 82%). Some subjects in the injection group, however, had worsened at six months but improved again by 12 months.
Table 4.
Numbers (percentages) of patients with lateral epicondylitis who were better (pain score ⩽3) at follow up compared with baseline according to treatment group*
| Follow up | Injection (n=53) | Naproxen (n=53) | Placebo (n=58) |
|---|---|---|---|
| 4 weeks†‡ | 41 (82) | 25 (48) | 28 (50) |
| 6 months‡ | 33 (65) | 42 (81) | 47 (83) |
| 12 months | 43 (84) | 45 (85) | 44 (82) |
Percentages may not calculate exactly because of missing data.
P<0.05 for injection versus naproxen.
P<0.05 for injection versus placebo.
Details of the self reported presence of elbow pain, the nurse’s examination findings, and disability scores are given on the BMJ’s website. Injection was superior to naproxen and placebo at four weeks; the three groups were similar at 12 months with a relapse in some patients in the injection group at six months.
The numbers of patients taking time off paid employment at four weeks were five (14%) in the injection group, four (10%) in the naproxen group, and eight (17%) in the placebo group; the numbers at 12 months were five (14%), four (10%), and 10 (21%), respectively (P>0.05 for both times). The numbers of patients taking painkillers in each group at four weeks and six and 12 months were similar: 18 (35%), 22 (42%), and 29 (50%) at four weeks; 21 (40%), 19 (36%), 23 (40%) at six months, and 14 (26%), 14 (26%), and 16 (28%) at 12 months for injection, naproxen, and placebo groups respectively.
Co-interventions
Case notes were available for 160 participants; four had transferred practices. In all, 155 records (50 injection, 52 naproxen, 53 placebo) had information about the randomised treatment, and 151 records (49 injection, 50 naproxen, 52 placebo) had complete information concerning patient treatment between the date of referral and follow up.
Numbers of co-interventions did not differ significantly between groups during follow up (table 5). A second injection was received by seven (14%) patients in the injection group; 17 (34%) patients in the naproxen group and 15 (29%) in the placebo group also received an injection during follow up. Fewer patients in the injection group reconsulted their general practitioner within four weeks of the randomised intervention, but observed consultation for tennis elbow pain was similar in all three groups by 12 months.
Table 5.
Numbers (percentages) of patients recorded to have reconsulted with general practitioner and received cointerventions during follow up*
| Injection (n=53) | Naproxen (n=53) | Placebo (n=58) | |
|---|---|---|---|
| Reconsultation | |||
| 4 weeks | 9 (18) | 16 (32) | 12 (23) |
| 6 months | 20 (41) | 24 (48) | 21 (40) |
| 12 months | 25 (51) | 24 (48) | 22 (42) |
| Cointerventions | |||
| 4 weeks | 6 (12) | 9 (18) | 10 (19) |
| 6 months | 13 (27) | 18 (36) | 18 (35) |
| 12 months | 17 (35) | 19 (38) | 19 (37) |
Numbers are cumulative totals during follow up. Percentages may not calculate exactly because of missing data.
Side effects
Local skin atrophy at the lateral epicondyle was observed in only two patients at six months and one patient at 12 months. The three affected patients were from the naproxen and placebo groups, and only one had additionally received a local injection. Naproxen was discontinued in four patients because of gastrointestinal side effects. One patient on naproxen had an allergic reaction characterised by oedema. Pain diaries recorded for five days after intervention showed a minor, non-significant, increase in severity of pain after injection, lasting one day only.
Discussion
Our results have two important implications for the management of new episodes of lateral epicondylitis in general practice. Firstly, a local corticosteroid injection is an effective, safe initial treatment with a clear clinical advantage four weeks later compared with a two week course of naproxen. Naproxen had no advantage over simple analgesics and a standard advice sheet alone. Secondly, by 12 months most patients with lateral epicondylitis had improved irrespective of initial treatment. Early effective treatment with local steroid injection resulted in more rapid resolution of symptoms but did not influence long term outcome.
A small proportion of patients failed to respond to the initial injection, and some patients who had initially improved had worse symptoms at six months. These may be patients whose primary disease lay within the cervical spine or whose local injection was not accurately placed. We did not give participants specific instructions about resting or abstaining from work or sporting activities, and effective pain relief might have led to a premature return to activity in the injection group causing a temporary worsening of their symptoms. Studies of other painful musculoskeletal syndromes, such as low back pain,12 have observed similar lack of association between early response to treatment and longer term outcomes. Further research is required to investigate these issues.
Strengths and weaknesses
The main criticism of previous reviews of treatment for tennis elbow has been the lack of methodologically rigorous trials.4,5 Our pragmatic study, carried out in a routine primary care setting, included a relatively homogeneous population of patients and was sufficiently large to detect clinically important differences between treatment groups. Possible prognostic variables were equally distributed between the three treatment groups at baseline. Although patients and doctors knew which treatment was given, the nurse who assessed outcome remained unaware of the treatment allocation throughout. Home based assessment minimised loss to follow up, enabling us to perform a robust intention to treat analysis.
We recognise a number of limitations to our study. Firstly, although we aimed to enrol all eligible patients consulting their general practitioner with a new episode of tennis elbow during the recruitment period, the variability in numbers of patients recruited by each general practitioner suggests that some potential participants were lost at this point. In some of the large group practices only one or two partners participated. We do not, therefore, have an accurate knowledge of the denominator population, making it difficult to use incidence of tennis elbow in primary care1 to estimate the proportion of all eligible subjects who were included in the study. However, there were no differences in participants’ baseline characteristics between high and low recruiting practices, suggesting a lack of significant selection bias. By contrast, results from hospital based studies are difficult to generalise to primary care.3,5 Patients recruited in secondary care represent an unknown selection of all affected individuals seen by general practitioners and probably have more severe, persistent complaints. The median duration of disease in our patients (nine weeks) was shorter than in hospital based studies.4,11 This indicates that our study population consisted mainly of patients with relatively short duration of symptoms, characteristic of those seen in primary care.
Secondly, although standard treatment types and doses were used, our results apply only to the specific injection and non-steroidal anti-inflammatory regimens that we used. A two week course of a non-steroidal drug was chosen by the general practitioners as being in line with current prescribing practice for a self limiting condition and is the regimen most commonly used in other studies of this condition.10 Thirdly, general practitioners taking part in this study all had previous experience of injecting,13 and care was taken to standardise the injection procedure. Practitioners less skilled in administering soft tissue injections might not reproduce the positive results obtained in this study. However, the general practitioners were not intensively trained, their technique was not reviewed, and they were “service” general practitioners not members of specialist rheumatology groups or from designated research practices.
Time constraints in primary care make large scale trials like ours difficult to perform in the context of every day practice. We involved the general practitioners in designing the trial from an early stage to maximise ownership and commitment.14 The protocol was easy to follow, and use of a research nurse relieved general practitioners from as much of the paperwork and data recording as possible. Results from the study have been fed back to the general practitioners by post and in practice based workshops. This network of general practitioners is currently participating in further practice based intervention studies of common musculoskeletal conditions.
Conclusions
We conclude that corticosteroid injections are the initial treatment of choice for lateral epicondylitis in primary care if the objective of treatment is to obtain optimal relief of symptoms during the early weeks. Patients, however, can be reassured that regardless of their treatment the probability is high that they will get better in the longer term. Further research should determine why some patients do less well after initial pain relief by injection.
Supplementary Material
Figure.
Patient recruitment, randomisation to treatment group, and follow up rates
Acknowledgments
We thank the general practitioners from the Community Musculoskeletal Research Group (see BMJ’s website for list of names) for their enthusiasm and hard work. We thank the Primary Care Rheumatology Society, Professor A Silman, and Dr P Brennan for help with the study design and early encouragement and endorsement; Gill Latham for providing holiday cover for the study nurse; and Bronwyn Montgomory for preparing the treatment packages. Finally we thank the patients who made this project possible.
Footnotes
Funding: Arthritis Research Campaign. Methylprednisolone injections were provided by UpJohn and enteric coated naproxen by Syntex.
Competing interests: None declared.
website extra: A further table and members of the the Community Musculoskeletal Research Group are given on the BMJ’s website www.bmj.com
References
- 1.Hamilton PG. The prevalence of humeral epicondylitis: a survey in general practice. J R Coll Gen Pract. 1986;36:464–465. [PMC free article] [PubMed] [Google Scholar]
- 2.Chard MD, Hazleman BL. Tennis elbow—a reappraisal. Br J Rheumatol. 1989;28:186–190. doi: 10.1093/rheumatology/28.3.186. [DOI] [PubMed] [Google Scholar]
- 3.Labelle H, Guibert R. Efficacy of diclofenac in lateral epicondylitis of the elbow also treated with immobilization. University of Montreal Orthopaedic Research Group. Arch Fam Med. 1997;6:257–262. doi: 10.1001/archfami.6.3.257. [DOI] [PubMed] [Google Scholar]
- 4.Labelle H, Guibert R, Joncas J, Newman N, Fallaha M, Rivard CH. Lack of scientific evidence for the treatment of lateral epicondylitis of the elbow. An attempted meta-analysis. J Bone Joint Surg [Br] 1992;74B:646–651. doi: 10.1302/0301-620X.74B5.1388172. [DOI] [PubMed] [Google Scholar]
- 5.Assendelft WJ, Hay EM, Adshead R, Bouter LM. Corticosteroid injections for lateral epicondylitis: a systematic overview. Br J Gen Pract. 1996;46:209–216. [PMC free article] [PubMed] [Google Scholar]
- 6.Kivi P. The etiology and conservative treatment of humeral epicondylitis. Scand J Rehabil Med. 1983;15:37–41. [PubMed] [Google Scholar]
- 7.Halle JS, Franklin RJ, Karalfa BL. Comparison of four treatment approaches for lateral epicondylitis of the elbow. J Orthop Sports Phys Ther. 1986;8:62–69. doi: 10.2519/jospt.1986.8.2.62. [DOI] [PubMed] [Google Scholar]
- 8.Beurskens AJ, de Vet HC, Lindeman E, Koke AJ, Regtop W, van der Hiejden GJ, et al. Efficacy of traction for non-specific low back pain: 5 week results of a randomised controlled trial. Lancet. 1995;346:1596–1600. doi: 10.1016/s0140-6736(95)91930-9. [DOI] [PubMed] [Google Scholar]
- 9.Stratford P, Levy DR, Gauldie S, Levy K, Miseferi D. Extensor carpi radialis tendonitis: a validation of selected outcome measures. Physiotherapy Canada. 1987;39:250–255. [Google Scholar]
- 10.Stull PA, Jokl P. Comparison of diflusinal and naproxen in the treatment of tennis elbow. Clin Ther. 1986;9:62–66. [PubMed] [Google Scholar]
- 11.Matthews JN, Altman DG, Campbell MJ, Royston P. Analysis of serial measurements in medical research. BMJ. 1990;300:230–235. doi: 10.1136/bmj.300.6719.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mitchell RI, Carmen GM. Results of a multicenter trial using an intensive active exercise programme for the treatment of acute soft tissue and back injuries. Spine. 1990;15:514–521. doi: 10.1097/00007632-199006000-00016. [DOI] [PubMed] [Google Scholar]
- 13.Lanyon P, Pope D, Croft P. Rheumatology education and management skills in general practice: a national study of trainees. Ann Rheum Dis. 1995;54:735–739. doi: 10.1136/ard.54.9.735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foy R, Parry J, McAvoy B. Clinical trials in primary care: targeted payments for trials might help improve recruitment and quality. BMJ. 1998;317:1168–1169. doi: 10.1136/bmj.317.7167.1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.