Abstract
Background:
Symptoms of inattention and hyperactivity/impulsivity that fall below the DSM-IV diagnostic threshold for attention-deficit hyperactivity disorder (ADHD) may be associated with the high prevalence of smoking among individuals with alcohol dependence, yet no studies to date have examined the relationship between subthreshold ADHD symptoms and cigarette smoking in this group. We hypothesized that increasing levels of ADHD symptoms would be associated with increasing risk of lifetime smoking and nicotine dependence, concentration problems secondary to nicotine withdrawal, and maintenance of smoking.
Methods:
Participants were alcohol-dependent adults (n = 242) who did not meet criteria for ADHD or a current Axis I disorder other than alcohol and nicotine dependence. All participants were involved in treatment for alcohol dependence but not smoking cessation. The Semi-Structured Assessment for the Genetics of Alcoholism was administered to collect demographic and smoking history data and to assess symptoms of ADHD and other psychiatric disorders.
Results:
A higher number of self-reported ADHD symptoms were associated with increased likelihood of ever smoking (p = .026), nicotine dependence (p = .017), and impaired concentration as a symptom of nicotine withdrawal (p = .046). There was no relationship between the number of ADHD symptoms and classification as a former versus current smoker (p = .333).
Conclusions:
Childhood symptoms of inattention and hyperactivity/impulsivity are related to cigarette smoking and nicotine dependence among alcohol-dependent individuals at levels below the ADHD diagnostic threshold. Conceptualization of ADHD symptoms as occurring on a continuum may aid identification of and early intervention for individuals who are at highest risk for initiating smoking and developing nicotine dependence.
Introduction
The relationship between attention-deficit hyperactivity disorder (ADHD) and cigarette smoking is well established as the prevalence of smoking among individuals with the disorder is roughly double that of individuals who do not have ADHD (Lambert & Hartsough, 1998; Laucht, Hohm, Esser, Schmidt, & Becker, 2007). Additionally, ADHD is associated with an increased risk of both smoking initiation and maintenance such that individuals with ADHD are more likely to become regular smokers, to develop nicotine dependence (Biederman et al., 2006; Fuemmeler, Kollins, & McClernon, 2007), and to experience more severe nicotine withdrawal, including greater problems with concentration (C. S. Pomerleau et al., 2003). Finally, studies employing both cross-sectional (O. F. Pomerleau, Downey, Stelson, & Pomerleau, 1995) and prospective (Covey, Manubay, Jiang, Nortick, & Palumbo, 2008; Humfleet et al., 2005) designs have demonstrated that smokers with ADHD tend to have a more difficult time quitting successfully than smokers without the disorder.
A number of theories to explain the link between ADHD and cigarette smoking have been proposed. Possible explanations for the linkage include shared genetic vulnerability (e.g., Laucht et al., 2007) or prenatal nicotine exposure, the latter of which may increase risk of developing both ADHD symptoms (Mick, Biederman, Faraone, Sayer, & Kleinman, 2002) and nicotine dependence (Buka, Shenassa, & Niaura, 2003) through its effects on critical periods of brain development. Also, because nicotine has stimulant-like effects that can enhance attentional capacities in both nicotine-naïve individuals as well as those who use nicotine regularly (McClernon et al., 2008; Potter & Newhouse, 2008), the self-medication hypothesis has been proposed to explain the co-occurrence of ADHD symptoms and cigarette smoking (Gehricke et al., 2007; Lerman et al., 2001). This hypothesis suggests that individuals with ADHD symptoms or other neurocognitive deficits that negatively impact attentional focus may be predisposed to use nicotine as a means of cognitive enhancement. Finally, environmental factors such as greater exposure to peers who use substances (Laucht et al.) and parental smoking (Wilens et al., 2008) have been cited as contributors to the elevated risk of smoking among individuals with ADHD.
Several lines of evidence suggest that ADHD symptoms tend to co-occur with both tobacco and alcohol use. For example, individuals with alcohol dependence and other substance use disorders have a higher prevalence of both smoking and ADHD than the general population (Arias et al., 2008), and adolescents who report even moderate levels of ADHD symptoms are more likely to use both alcohol and tobacco than same-age peers who report no ADHD symptoms (Whalen, Jamner, Henker, Delfino, & Lozano, 2002). Similar to the proposed factors underlying the ADHD and tobacco link, it is likely that some of the clustering of tobacco use, alcohol use disorders, and ADHD symptoms within individuals is attributable to common genetic, biological, and environmental influences as well as their interaction. For example, characteristics such as novelty-seeking and behavioral disinhibition tend to overlap all three of these conditions, as does conduct disorder, suggesting that there may be a common underlying vulnerability to both externalizing behaviors and substance misuse (McClernon & Kollins, 2008; Young et al., 2009).
Despite the clinical and theoretical relevance of research examining relationships among ADHD symptoms, cigarette smoking, and alcohol use disorders, there are few extant studies available on this topic. We are aware of only two investigations that have examined the relationship between ADHD and smoking among individuals with alcohol or other substance use disorders, and although the designs are not entirely comparable, the results are somewhat mixed. That is, one large study (Arias et al., 2008) failed to find a relationship between an ADHD and a DSM-IV diagnosis of nicotine dependence in this population, while the other (Ohlmeier et al., 2007) reported an association between ADHD comorbidity and greater severity of nicotine dependence, as measured by the Fagerström Test for Nicotine Dependence (FTND).
Most of the research to date on the linkage between ADHD and cigarette smoking or nicotine dependence, including the aforementioned studies of smoking conducted in alcohol- or substance-dependent populations, has focused on individuals who meet the full diagnostic criteria for the syndrome of ADHD. However, there is evidence that the inattention, hyperactivity, and impulsivity that are characteristic features of ADHD may be related to smoking even at levels below the threshold required for a DSM-IV diagnosis. One large prospective twin study (Elkins, McGue, & Iacono, 2007) found that, in comparison to having no symptoms of inattention or hyperactivity/impulsivity, having even one symptom of either was associated with a significant increase in the risk of developing nicotine dependence between the ages of 11 and 18 years. Additionally, data from the National Longitudinal Study of Adolescent Health provide evidence for a positive linear relationship between the number of self-reported ADHD symptoms and the odds of being a regular smoker, regardless of whether individuals meet the minimum symptom threshold for the ADHD diagnosis (Kollins, McClernon, & Fuemmeler, 2005). This finding has been replicated in at least two other reports (Upadhyaya & Carpenter, 2008; Wilens et al., 2008), and the combined results of these studies suggest that each one-unit increase in the number of reported DSM-IV ADHD symptoms is associated with a 10%–20% increase in the odds of being a regular smoker (Kollins et al.; Upadhyaya & Carpenter).
As noted previously, both the studies examining ADHD symptoms and cigarette smoking in alcohol- and drug-dependent populations (i.e., Arias et al., 2008; Ohlmeier et al., 2007) categorized individuals as either meeting the full DSM-IV criteria for ADHD or not, thus overlooking potentially important relationships between subthreshold ADHD symptoms during childhood and cigarette smoking in this population. Additionally, these studies focused primarily on the diagnosis or severity of nicotine dependence and heaviness of smoking in ADHD versus non-ADHD controls and did not explore the relationship between ADHD symptoms and smoking cessation. We are aware of no studies to date that have provided a comprehensive examination of the extent to which self-reported inattention and hyperactivity/impulsivity during childhood are associated with cigarette smoking and smoking cessation among alcohol-dependent adults who do not meet DSM-IV criteria for ADHD. As such, we used information collected from semi-structured clinical interviews with 242 individuals who were seeking or already involved in treatment for alcohol dependence as a means of investigating the relationship between subthreshold ADHD symptoms and smoking in this population. On the basis of previous findings in general population samples, we predicted that
a greater number of total ADHD symptoms would be associated with an increased risk of both ever smoking and nicotine dependence and
among ever-smokers, an increasing number of ADHD symptoms would correlate with a greater likelihood of experiencing concentration problems following smoking reduction or abstinence and decreased odds of successful quitting.
Method
Participants
Participants were 242 alcohol-dependent men (n = 144, 59.5%) and women (n = 98, 40.5%) who were involved in one of two concurrently enrolling studies: (a) a pharmacogenetic investigation of citalopram as a treatment for alcohol dependence (Protocol 1; ClinicalTrials.gov identifier: NCT#00249405; n = 167, 69.0%) or (b) a laboratory study examining the role of gender and alcohol dependence diagnosis in physiologic stress response to pharmacological probes (Protocol 2; ClinicalTrials.gov identifier: NCT#00226694; n = 75, 31.0%). The inclusion/exclusion criteria for the two studies were similar, involving individuals aged 21–65 years who met DSM-IV criteria for alcohol dependence and did not have a current independent Axis I disorder other than nicotine dependence. Individuals with a history of other substance abuse or dependence were included so long as the symptoms of these disorders were in full remission for at least 60 days. Individuals with past psychiatric diagnoses were eligible to participate, with some exceptions (e.g., lifetime diagnosis of a psychotic disorder was exclusionary in both protocols). With the exception of antisocial personality disorder (ASPD), Axis II disorders were not comprehensively assessed. None of the participants were seeking or participating in treatment for smoking cessation.
The majority of the participants were Caucasian (n = 181, 74.8%), with a mean age of 45.4 (SD = 8.9) years. The average highest grade level achieved was postsecondary (M = 13.8, SD = 2.1). Seventy-two participants (29.8%) had a lifetime diagnosis of a cannabis use disorder, and 58 (24.0%) met criteria for abuse or dependence on a drug other than cannabis. A small portion of the participants met criteria for ASPD (n = 14, 5.8%) or had a history of conduct disorder without ASPD (n = 11, 4.5%). Other lifetime psychiatric comorbidity included major depressive disorder (n = 4, 1.7%), posttraumatic stress disorder (PTSD) (n = 1, 0.4%), an anxiety disorder other than PTSD (n = 1, 0.4%), and alcohol- or other substance-induced mood disorders (n = 52, 21.5%).
Assessments
Assessments included the Semi-Structured Assessment for the Genetics of Alcoholism–Version 2 (SSAGA-II; Bucholz et al., 1994), FTND (Heatherton, Kozlowski, Frecker, & Fagerström, 1991), and the tobacco form of the Family History Assessment Module (FHAM; Rice et al., 1995). The SSAGA-II is a diagnostic interview containing sections that assess substance use disorders as well as major Axis I psychiatric disorders (e.g., mood and anxiety disorders, psychotic disorders, ADHD and conduct disorder) and ASPD. Developed for the Collaborative Study on the Genetics of Alcoholism, the SSAGA-II has been demonstrated to be a valid and reliable assessment instrument in research settings and is particularly useful in differentiating substance induced from independent psychiatric diagnoses (Bucholz et al.). The SSAGA-II was administered by trained nonclinician interviewers and reviewed by either a board-certified psychiatrist or a doctoral-level clinical psychology fellow working under the supervision of a licensed psychologist to achieve diagnostic consensus.
The ADHD section of the SSAGA-II assesses symptoms of inattention (10 items, 9 of which cover DSM-IV criteria and 1 of which covers DSM-III-R criteria) and hyperactivity/impulsivity (11 items, 10 of which cover DSM-IV criteria and 1 of which covers DSM-III-R criteria) of at least 6 months duration that occurred consistently during that 6-month period and were notable during the first few years of school (e.g., ages 6–10 years). Total ADHD scores were obtained by summing the number of DSM-IV criteria met on the basis of responses to the SSAGA-II items.
Participants’ age, sex, race, smoking status, and history of concentration problems secondary to nicotine withdrawal were recorded as part of the SSAGA-II interview. Age at onset of alcohol dependence was also derived from SSAGA-II data and defined as the age at which the participant first met the three required criteria for a DSM-IV diagnosis. Substance use disorder comorbidity was based on SSAGA-II lifetime diagnosis of a nonnicotine drug use disorder. Finally, a diagnosis of conduct disorder (with or without later progression to ASPD) was established on the basis of the SSAGA-II interview.
The FTND (Heatherton et al., 1991), a six-item measure of the severity of nicotine dependence, was also completed by participants during the screening portion of the two studies. This measure has been shown to have adequate psychometric properties when administered in an alcohol-dependent population (Burling & Burling, 2003). The tobacco form of the FHAM (Rice et al., 1995) was administered by a trained research assistant during screening to assess history of regular smoking in relatives and spouses/partners. A dichotomized variable representing history of regular smoking in biological parents and/or siblings was created to model the influence of family history factors in the initiation and maintenance of smoking.
Data analyses
Four logistic regression analyses were conducted to examine the relationships between ADHD symptoms of inattention and hyperactivity/impulsivity and smoking (i.e., ever smoking, nicotine dependence diagnosis, withdrawal-related concentration problems, and being a current vs. a former smoker). Prior to conducting the logistic regression analyses, we examined differences in participant characteristics between Protocol 1 (i.e., the pharmacogenetics trial in which participants were seeking outpatient treatment for alcohol dependence; see Heffner et al., in press, for a more complete description of the sample) and Protocol 2 (i.e., the laboratory study of stress responsivity, where participants were recruited primarily from residential treatment facilities; see Anthenelli, Blom, Johnson, Heffner, & Wand, 2009, for a complete sample description). Results of these analyses indicated that participants in Protocol 2 were younger; had fewer years of education, lower incomes, earlier age at onset of alcohol dependence, more severe alcohol dependence, and higher ADHD symptom levels than participants in Protocol 1 as well as being significantly more likely to be non-Caucasian; and have a history of conduct disorder and other substance use disorders (all comparisons statistically significant at the p < .001 level). In order to control for these differences in participant characteristics, a “protocol” variable was forced into each regression model prior to entry of the other predictors.
Because we found the variable protocol to be strongly correlated with almost all the predictors to be included in the regression models, we utilized a forward stepwise method to generate a final predictive model for each of the four dependent smoking variables as a means of minimizing potential problems with multicollinearity. In addition to the total number of DSM-IV ADHD symptoms, predictors included for stepwise entry in all four logistic regression analyses were age, race, sex, income, years of education, age onset of alcohol dependence, substance use disorder comorbidity (i.e., diagnosis of any lifetime substance abuse or dependence), lifetime conduct disorder (with or without ASPD), and family history of regular smoking. In the two regression analyses to predict concentration problems secondary to nicotine withdrawal and successful quitting (i.e., being a former vs. current smoker), two additional variables were included as potential covariates: lifetime nicotine dependence diagnosis and number of cigarettes per day (when the participant was smoking regularly). These variables were selected as potential covariates due to their observed relationship with smoking initiation and maintenance as well as nicotine dependence and withdrawal severity in prior studies conducted with alcohol-dependent population (e.g., Daeppen et al., 2000) or general population (e.g., Hu, Davies, & Kandel, 2006; Johnson & Novak, 2009; Piasecki, Jorenby, Smith, Fiore, & Baker, 2003) samples.
The relationship between predictors and dependent variables was analyzed using a Wald χ2 test with a two-tailed alpha level of p < .05 to establish statistical significance. Nagelkerke’s R2 values were obtained as an estimation of the predictive value of the models. Goodness of fit for each model was evaluated using procedure by Hosmer and Lemeshow (1989). Data were analyzed using SPSS v. 16.0.
Results
The prevalence of ever smoking (defined as smoking 100 or more cigarettes, consistent with established definitions utilized in epidemiological studies; e.g., Grant, 1998) in the overall sample was 71.9% (n = 174). Of the 174 ever-smokers, 124 (71.3%) reported smoking within the last month (i.e., current smokers) and 50 (28.7%) had not smoked within the past month (i.e., former smokers). The majority of the ever-smokers (n = 144, 82.8%) met lifetime criteria for nicotine dependence.
With respect to the prevalence of self-reported childhood ADHD symptoms in this sample of alcohol-dependent adults, over half of the participants (n = 132, 54.5%) reported no symptoms of inattention or hyperactivity/impulsivity during childhood. Forty participants (16.5%) endorsed a maximum of one to two symptoms in either or both categories (i.e., minimal symptoms), 39 (16.1%) endorsed a maximum of three to five symptoms in either or both categories (i.e., subthreshold symptoms), and 31 (12.8%) endorsed six or more symptoms in either or both categories (i.e., clinically significant symptoms). Of those participants who endorsed at least six symptoms of either inattention or hyperactivity/impulsivity (i.e., the minimal symptom threshold for a DSM-IV diagnosis of ADHD), the most common reasons for failure to meet full ADHD criteria were (a) onset of symptoms at age 7 years or over (n = 11), (b) symptom-related problems not reported in two areas of functioning (n = 11), or (c) both (a) and (b) (n = 8). One participant who otherwise met the criteria for ADHD was not diagnosed with the disorder due to his report that the symptoms were secondary to a medical condition.
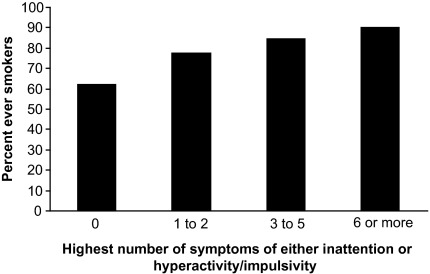
Figure 1 depicts the prevalence rate of smoking by the maximum number of ADHD symptoms endorsed in each of the two symptom categories (i.e., inattention and hyperactivity/impulsivity). As indicated by the Figure 1, an increasing number of symptoms was associated with increased prevalence of ever smoking: 62.1% for participants who reported no ADHD symptoms, 77.5% for participants who reported minimal symptoms, 84.6% for participants with subthreshold symptoms, and 90.3% for participants with clinically significant symptoms.
Figure 1.
Prevalence of ever smoking in alcohol-dependent adults by number of self-reported childhood attention-deficit hyperactivity disorder symptoms.
Results of the logistic regression analyses
Ever smoking
The full logistic regression model to predict ever smoking was significant (χ2 = 51.06, p < .001, R2 = .27). As illustrated in Table 1, outside of the protocol variable, the only significant predictor of ever smoking among the independent variables considered for inclusion in the model was the ADHD symptom total (p = .026). Based upon the estimated odds ratio (OR = 1.12), each one-symptom increase in the number of childhood ADHD symptoms was associated with a 12% increase in the odds of ever smoking.
Table 1.
Results of logistic regression analyses to predict cigarette smoking characteristics
| Dependent variable | Predictora | β | SE | p Value | OR | 95% CI |
| Ever-smoker | Protocol | 3.01 | 0.74 | <.001 | 20.30 | 4.78–86.16 |
| ADHD symptom total | 0.11 | 0.05 | .026 | 1.12 | 1.01–1.24 | |
| Nicotine dependence | Protocol | 2.06 | 0.47 | <.001 | 7.88 | 3.15–19.70 |
| Race (Caucasian) | 1.18 | 0.42 | .005 | 3.26 | 1.44–7.40 | |
| Age | 0.04 | 0.02 | .033 | 1.04 | 1.01–1.09 | |
| Age at onset of AD | −0.06 | 0.02 | .005 | 0.95 | 0.91–0.98 | |
| ADHD symptom total | 0.11 | 0.04 | .017 | 1.11 | 1.02–1.21 | |
| Postcessation concentration problems | Protocol | −0.02 | 0.37 | .955 | 0.98 | 0.47–2.02 |
| Age | −0.04 | 0.02 | .044 | 0.96 | 0.92–0.99 | |
| Nicotine dependence (lifetime criteria met) | 2.58 | 0.77 | .001 | 13.13 | 2.92–59.09 | |
| ADHD symptom total | 0.08 | 0.04 | .046 | 1.08 | 1.01–1.17 | |
| Successfully quit (former vs. current smoker) | Protocol | 0.74 | 0.64 | .250 | 2.09 | 0.60–7.30 |
| Sex (female) | 0.90 | 0.46 | .048 | 2.47 | 1.01–6.04 | |
| Age | 0.09 | 0.03 | .003 | 1.09 | 1.03–1.16 | |
| Income | 0.37 | 0.11 | .001 | 1.44 | 1.17–1.78 | |
| Nicotine dependence (lifetime criteria met) | −1.96 | 0.57 | .001 | 0.14 | 0.05–0.43 | |
| Cigarettes per day | 0.05 | 0.02 | .001 | 1.05 | 1.02–1.09 |
Note. OR = odds ratio; AD = alcohol dependence; ADHD = attention-deficit hyperactivity disorder.
Based on stepwise selection of predictors, with the exception of protocol variable, which was forced into each model. Predictors included age, sex, race, years of education, income, age at onset of alcohol dependence, lifetime diagnosis of a substance use disorder, lifetime conduct disorder, family history of smoking, and ADHD symptom total. Cigarettes per day and nicotine dependence were included as predictors only in the regression analyses to predict postcessation concentration problems and successful quitting.
Nicotine dependence
In the logistic regression model predicting a lifetime diagnosis of nicotine dependence (χ2 = 62.73, p < .001, R2 = .31), after controlling for protocol (p < .001), older age (p = .033), earlier age at onset of alcohol dependence (p = .005), Caucasian race (p = .005), and higher number of ADHD symptoms (p = .017) were found to be significant predictors. Similar to the analysis for ever smoking, the OR associated with ADHD symptom total (OR = 1.11) suggested that, after controlling for covariates, each additional symptom of childhood inattention or hyperactivity/impulsivity corresponded with an 11% increase in the odds of becoming nicotine dependent.
Concentration difficulties secondary to nicotine withdrawal
The overall test of the model to predict concentration difficulties following smoking cessation or reduction was significant (χ2 = 30.60, p < .001, R2 = .22). A lifetime diagnosis of nicotine dependence (p = .001), younger age (p = .044), and a higher number of childhood ADHD symptoms (p = .046) predicted a greater likelihood of experiencing such concentration problems.
Successful quitting (i.e., former vs. current smoker)
In the regression analysis to predict successful quitting, five additional variables entered into a model containing the protocol variable (full model: χ2 = 54.88, p < .001, R2 = .39). Successful quitters were more likely to be female (p = .048), older (p = .003), and heavier smokers (i.e., more cigarettes per day, when smoking regularly; p = .001); have a higher income (p = .001); and not meet lifetime criteria for nicotine dependence (p = .001). Total ADHD symptoms did not predict successful quitting (p = .333).
Discussion
In this study, we found that a greater number of childhood ADHD symptoms predicted both ever smoking and nicotine dependence in these alcohol-dependent adults who did not meet lifetime criteria for ADHD. These results extend the findings of an association between childhood ADHD symptoms and regular smoking and nicotine dependence in the general population (Fuemmeler et al., 2007; Kollins et al., 2005). Our results in this clinical sample also expand findings from general population studies that indicate a generally linear relationship between the number of childhood ADHD symptoms and the risk of cigarette smoking. In the present study, each one-symptom increase in the number of ADHD symptoms was associated with a 12% increase in the odds of ever smoking and an 11% increase in the odds of developing nicotine dependence. These figures are comparable to estimates obtained in prior studies using general population samples, where one-unit increases in the number of ADHD symptoms have been linked to a 10%–20% increase in the odds of being a regular smoker (Kollins et al.; Upadhyaya & Carpenter, 2008).
We also found that, among ever-smokers, the total number of ADHD symptoms endorsed was associated with an increased likelihood of reporting concentration problems following cessation or reduction of smoking. These results extend the work of C. S. Pomerleau, Marks, and Pomerleau (2000), who found that a DSM-IV diagnosis of childhood ADHD predicted concentration difficulties following smoking cessation or reduction. The findings are thus consistent with the hypothesis that some smokers may be predisposed to developing particular withdrawal symptoms that are characteristic of their preexisting psychiatric condition, and our findings suggest that this effect also extends to individuals who do not meet full criteria for ADHD. Thus, even subthreshold symptoms of inattention and hyperactivity/impulsivity during childhood are associated with greater withdrawal-related concentration difficulties.
Contrary to the results of post-hoc analyses examining the relationship between ADHD symptoms and smoking cessation in clinical studies with treatment-seeking smokers (Covey et al., 2008; Humfleet et al., 2005), we did not find evidence to suggest a reduced likelihood of successful smoking cessation among these alcohol-dependent smokers based on the number of self-reported ADHD symptoms during childhood. Instead, demographic and smoking-related characteristics that have been linked to smoking cessation outcomes in general population samples were identified as significant predictors, including older age (Murray et al., 2000; Velicer, Redding, Sun, & Prochaska, 2007), higher income and/or socioeconomic status (Matheny & Weatherman, 1998), and not meeting criteria for nicotine dependence (Ferguson et al., 2003). In contrast to previous findings that men (Ferguson et al.; Murray et al.) and lighter smokers (Carlson, Taenzer, Koopmans, & Bultz, 2000) are more likely to quit than women and heavier smokers, respectively, the opposite was true in the present study.
Although the finding of no relationship between ADHD symptoms and smoking cessation was unexpected based on the results of prior research (e.g., Covey et al., 2008; Humfleet et al., 2005), one possible explanation is that, unlike the previous studies, the participants in the present study were not currently attempting to quit smoking, which may have obscured relationships between ADHD symptoms and successful smoking cessation treatment. An alternative explanation is that the prior studies used a categorical definition of ADHD rather than examining subthreshold symptoms, leaving open the possibility that clinically significant ADHD symptoms, but not subthreshold ADHD symptoms, predict smoking cessation treatment failure. Yet another possibility is that previous findings suggesting a link between ADHD symptoms and unsuccessful smoking cessation do not generalize to this special population of smokers with alcohol dependence. Very few studies have examined predictors of smoking cessation in an alcohol-dependent population, and results of the few extant studies in this area suggest that the length of abstinence from alcohol is the only robust predictor of successful smoking cessation (see review by Heffner, Winders-Barrett, & Anthenelli, 2007). Because we did not collect specific data regarding the length of alcohol abstinence at the time that former smokers quit, we were unable to evaluate this relationship using the retrospective data available in the present study. However, completion of the two studies from which we have utilized baseline data for these analyses will yield prospective data on the relationship between length of alcohol abstinence and unaided smoking cessation in these alcohol-dependent smokers.
There are several limitations of this secondary data analysis. Some research has suggested that retrospective self-report of ADHD symptomatology during childhood may be biased in the direction of overestimating the extent of symptoms (Mannuzza, Klein, Klien, Bessler, & Shrout, 2002). Because the assessment of ADHD was not a primary aim of the studies, we did not examine other sources of information (e.g., collateral informant interviews) to assess the reliability of participants’ retrospective self-report. However, it is not clear that findings demonstrating a high rate of false positives for the ADHD syndrome are applicable to assessment of specific ADHD symptoms that do not reach the diagnostic threshold. Additionally, there is other evidence to suggest that adults are able to accurately report on their experience of inattention and hyperactivity/impulsivity symptoms during childhood, at least to the extent that there is a strong correlation between self- and observer-reported symptoms (Murphy & Schachar, 2000; Zucker, Morris, Ingram, Morris, & Bakeman, 2002). Other limitations include the reliance on a clinical (treatment seeking) versus population sample of individuals with alcohol dependence and no current psychiatric comorbidity, which limits the generalizability of the results; the use of current smoking status (i.e., current vs. former smoker) as a proxy for smoking cessation rather than prospectively examining the link between ADHD symptoms and cessation among individuals who are trying to quit; the possibility that subthreshold ADHD symptoms recalled during childhood may tap into many different domains (e.g., personality/temperament, other psychopathology such as depression or anxiety) that are not easily distinguishable on the basis of retrospective self-report; and that our strict adherence to the age-of-onset criterion for an ADHD diagnosis (i.e., emergence of symptoms prior to age 7 years) might have influenced the results. Indeed, recent research has suggested that the age-at-onset criterion may be too rigorous a requirement and that individuals with an onset of symptoms at age 7 years or after demonstrate levels of impairment and patterns of comorbidity that strongly resemble those of their counterparts with onset of symptoms prior to age 7 years (Faraone et al., 2006).
Despite the limitations of this study, these results shed new light on the potential clinical significance of subthreshold ADHD symptoms among individuals with alcohol dependence as it relates to cigarette smoking. Utilizing well-validated diagnostic assessments of alcohol and other substance use disorders as well as psychiatric comorbidity in this relatively large sample of alcohol-dependent adults, we demonstrated that childhood symptoms of inattention and hyperactivity/impulsivity are associated with subsequent cigarette smoking and nicotine dependence in a continuous rather than a categorical manner and are prognostic of concentration difficulties among smokers who attempt to quit or significantly reduce their use of tobacco. These findings are not likely to have been confounded by psychiatric comorbidity as the prevalence of independent lifetime psychiatric disorders other than substance use disorders in this sample was extremely low and none of the participants met current criteria for an Axis I disorder other than alcohol, nicotine, or other drug dependence.
Several implications of our findings are worth highlighting. First, our results provide additional evidence for a clustering of tobacco use, alcohol misuse, and subthreshold ADHD symptoms within individuals, suggesting that further investigation into the causes and consequences of their co-occurrence is warranted. Second, the knowledge that children and adolescents who display even low-severity difficulties with inattention and hyperactivity/impulsivity, in addition to those who meet full criteria for ADHD, are at heightened risk for cigarette smoking and nicotine dependence suggests that prevention programs for youth who are considered at risk for tobacco and other substance use should include this group. Finally, it is possible that targeted behavioral interventions to assist smokers who are particularly vulnerable to developing postcessation concentration problems (i.e., those who endorse ADHD symptoms during childhood, even at levels below the diagnostic threshold) could potentially improve smoking cessation outcomes for both alcohol- and nonalcohol-dependent smokers. To our knowledge, the efficacy of this type of treatment strategy has not yet been reported, and further research exploring the association between ADHD symptoms and difficulty initiating or maintaining smoking abstinence is still needed.
Funding
This work was supported by the National Institutes of Health (AA013307, AA013307-05S1, AA013957, and AA013957-03S1 to RMA). JLH, CSJ, and RMA and TJB were also supported, in part, by National Institute on Drug Abuse/Department of Veterans Affairs Cooperative Studies Program 1022 and by the Department of Veterans Affairs. The Tri-State Tobacco and Alcohol Research Center receives research support from Lilly and Pfizer.
Declaration of interests
None declared.
Acknowledgments
The authors would like to thank Anne Autry, M.D., Reene Cantwell, Kerri Dawson-Earles, B.S., Julie Jansen, B.A., Rebecca Kramer, B.A., Stephanie Nolting, M.Ed., Patricia Shay, and Deonna Suggs, B.A. for their assistance on this project. RMA provides consultancy, advisory, and/or speakers’ bureau services to Sanofi-Aventis and Pfizer.
References
- Anthenelli RM, Blom TJ, Johnson CS, Heffner JL, Wand GS. Sex differences in the stress response to the combined dexamethasone-CRH stimulation test in non-depressed, abstinent alcoholics and controls. 2009 Manuscript submitted for publication. [Google Scholar]
- Arias AJ, Gelernter J, Chan G, Weiss RD, Brady KT, Farrer L, et al. Correlates of co-occurring ADHD in drug-dependent subjects: Prevalence and features of substance dependence and psychiatric disorders. Addictive Behaviors. 2008;33:1199–1207. doi: 10.1016/j.addbeh.2008.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J, Monuteaux MC, Mick E, Spencer T, Wilens TE, Silva JM, et al. Young adult outcome of attention deficit hyperactivity disorder: A controlled 10-year follow-up study. Psychological Medicine. 2006;36:167–179. doi: 10.1017/S0033291705006410. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI, et al. A new, semi-structured psychiatric interview for use in genetic linkage studies: A report on the reliability of the SSAGA. Journal of Studies on Alcohol. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- Buka SL, Shenassa ED, Niaura R. Elevated risk of tobacco dependence among offspring of mothers who smoked during pregnancy: A 30-year prospective study. American Journal of Psychiatry. 2003;160:1978–1984. doi: 10.1176/appi.ajp.160.11.1978. [DOI] [PubMed] [Google Scholar]
- Burling AS, Burling TA. A comparison of self-report measures of nicotine dependence among male drug/alcohol-dependent cigarette smokers. Nicotine & Tobacco Research. 2003;5:625–633. doi: 10.1080/1462220031000158708. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Taenzer P, Koopmans J, Bultz BD. Eight-year follow-up of a community-based large group behavioral smoking cessation intervention. Addictive Behaviors. 2000;25:725–741. doi: 10.1016/s0306-4603(00)00081-2. [DOI] [PubMed] [Google Scholar]
- Covey LS, Manubay J, Jiang H, Nortick M, Palumbo D. Smoking cessation and inattention or hyperactivity/impulsivity: A post hoc analysis. Nicotine & Tobacco Research. 2008;10:1717–1725. doi: 10.1080/14622200802443536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daeppen J.-B., Smith TL, Danko GP, Gordon L, Landi NA, Nurnberger JI, Jr., et al. Clinical correlates of cigarette smoking and nicotine dependence in alcohol-dependent men and women. Alcohol & Alcoholism. 2000;35:171–175. doi: 10.1093/alcalc/35.2.171. [DOI] [PubMed] [Google Scholar]
- Elkins IJ, McGue M, Iacono WG. Prospective effects of attention-deficit/hyperactivity disorder, conduct disorder, and sex on adolescent substance use and abuse. Archives of General Psychiatry. 2007;64:1145–1152. doi: 10.1001/archpsyc.64.10.1145. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Spencer T, Mick E, Murray K, Petty C, et al. Diagnosing adult attention deficit hyperactivity disorder: Are late onset and subthreshold diagnoses valid? American Journal of Psychiatry. 2006;163:1720–1729. doi: 10.1176/ajp.2006.163.10.1720. [DOI] [PubMed] [Google Scholar]
- Ferguson JA, Patten CA, Schroeder DR, Offord KP, Eberman KM, Hurt RD. Predictors of 6-month tobacco abstinence among 1224 cigarette smokers treated for nicotine dependence. Addictive Behaviors. 2003;28:1203–1218. doi: 10.1016/s0306-4603(02)00260-5. [DOI] [PubMed] [Google Scholar]
- Fuemmeler BF, Kollins SH, McClernon FJ. Attention deficit hyperactivity disorder symptoms predict nicotine dependence and progression to regular smoking from adolescence to young adulthood. Journal of Pediatric Psychology. 2007;32:1203–1213. doi: 10.1093/jpepsy/jsm051. [DOI] [PubMed] [Google Scholar]
- Gehricke J-G, Loughlin SE, Whalen CK, Potkin SG, Fallon JH, Jammer JH, et al. Smoking to self-medicate attentional and emotional dysfunctions. Nicotine & Tobacco Research. 2007;9:S523–S536. doi: 10.1080/14622200701685039. [DOI] [PubMed] [Google Scholar]
- Grant BF. Age at smoking onset and its association with alcohol consumption and DSM-IV alcohol abuse and dependence: Results from the National Longitudinal Alcohol Epidemiologic Survey. Journal of Substance Abuse. 1998;10:59–73. doi: 10.1016/s0899-3289(99)80141-2. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström test for nicotine dependence: A revision of the Fagerström tolerance questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Heffner JL, Tran GQ, Johnson CS, Winders-Barrett S, Blom TJ, Thompson RD, et al. Combining Motivational Interviewing with Compliance Enhancement Therapy (MI-CET): Development and preliminary evaluation of a new, manual-guided psychosocial adjunct to alcohol dependence pharmacotherapy. Journal of Studies on Alcohol and Drugs. doi: 10.15288/jsad.2010.71.61. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heffner JL, Winders-Barrett S, Anthenelli RM. Predicting alcohol misusers’ readiness and ability to quit smoking: A critical review. Alcohol and Alcoholism. 2007;42:186–195. doi: 10.1093/alcalc/agm021. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied logistic regression. New York: Wiley; 1989. [Google Scholar]
- Hu M, Davies M, Kandel DB. Epidemiology and correlates of daily smoking and nicotine dependence among young adults in the United States. American Journal of Public Health. 2006;96:299–308. doi: 10.2105/AJPH.2004.057232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humfleet GL, Prochaska JJ, Mengis M, Cullen J, Muñoz R, Reus V, et al. Preliminary evidence of the association between the history of childhood attention-deficit/hyperactivity disorder and smoking treatment failure. Nicotine & Tobacco Research. 2005;7:453–460. doi: 10.1080/14622200500125310. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Novak SP. Onset and persistence of daily smoking: The interplay of socioeconomic status, gender, and psychiatric disorders. Drug and Alcohol Dependence. 2009;104S:S50–S57. doi: 10.1016/j.drugalcdep.2009.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kollins SH, McClernon FJ, Fuemmeler BF. Association between smoking and attention-deficit/hyperactivity disorder symptoms in a population-based sample of young adults. Archives of General Psychiatry. 2005;62:1142–1147. doi: 10.1001/archpsyc.62.10.1142. [DOI] [PubMed] [Google Scholar]
- Lambert NM, Hartsough CS. Prospective study of tobacco smoking and substance dependencies among samples of ADHD and non-ADHD participants. Journal of Learning Disabilities. 1998;31:533–544. doi: 10.1177/002221949803100603. [DOI] [PubMed] [Google Scholar]
- Laucht M, Hohm E, Esser G, Schmidt MH, Becker K. Association between ADHD and smoking in adolescence: Shared genetic, environmental and psychopathological factors. Journal of Neural Transmission. 2007;114:1097–1104. doi: 10.1007/s00702-007-0703-y. [DOI] [PubMed] [Google Scholar]
- Lerman C, Audrain J, Tercyak K, Hawk LW, Bush A, Crystal-Mansour S, et al. Attention-deficit hyperactivity disorder (ADHD) symptoms and smoking patterns among participants in a smoking cessation program. Nicotine & Tobacco Research. 2001;3:353–359. doi: 10.1080/14622200110072156. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Klein DF, Bessler A, Shrout P. Accuracy of adult recall of childhood attention deficit hyperactivity disorder. American Journal of Psychiatry. 2002;159:1882–1888. doi: 10.1176/appi.ajp.159.11.1882. [DOI] [PubMed] [Google Scholar]
- Matheny KB, Weatherman KE. Predictors of smoking cessation and maintenance. Journal of Clinical Psychology. 1998;54:223–235. doi: 10.1002/(sici)1097-4679(199802)54:2<223::aid-jclp12>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- McClernon FJ, Kollins SH. ADHD and smoking: From genes to brain to behavior. Annals of the New York Academy of Sciences. 2008;1141:131–147. doi: 10.1196/annals.1441.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClernon FJ, Kollins SH, Lutz AM, Fitzgerald DP, Murray DW, Redman C, et al. Effects of smoking abstinence on adult smokers with and without attention deficit hyperactivity disorder: Results of a preliminary study. Psychopharmacology. 2008;197:95–105. doi: 10.1007/s00213-007-1009-3. [DOI] [PubMed] [Google Scholar]
- Mick E, Biederman J, Faraone SV, Sayer J, Kleinman S. Case-control study of attention-deficit hyperactivity disorder and maternal smoking, alcohol use, and drug use during pregnancy. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:378–385. doi: 10.1097/00004583-200204000-00009. [DOI] [PubMed] [Google Scholar]
- Murphy P, Schachar R. Use of self-ratings in the assessment of symptoms of attention deficit hyperactivity disorder. American Journal of Psychiatry. 2000;157:1156–1159. doi: 10.1176/appi.ajp.157.7.1156. [DOI] [PubMed] [Google Scholar]
- Murray RP, Gerald LB, Lindgren PG, Connett JE, Rand CS, Anthonisen NR. Characteristics of participants who stop smoking and sustain abstinence for 1 and 5 years in the Lung Health Study. Preventive Medicine. 2000;30:392–400. doi: 10.1006/pmed.2000.0642. [DOI] [PubMed] [Google Scholar]
- Ohlmeier MD, Peters K, Kordon A, Seifert J, te Wildt B, Wiese B, et al. Nicotine and alcohol dependence in patients with comorbid attention-deficit/hyperactivity disorder (ADHD) Alcohol & Alcoholism. 2007;42:539–543. doi: 10.1093/alcalc/agm069. [DOI] [PubMed] [Google Scholar]
- Piasecki TM, Jorenby DE, Smith SS, Fiore MC, Baker TB. Smoking withdrawal dynamics: III. Correlates of withdrawal heterogeneity. Experimental and Clinical Psychopharmacology. 2003;11:276–285. doi: 10.1037/1064-1297.11.4.276. [DOI] [PubMed] [Google Scholar]
- Pomerleau CS, Downey KK, Snedecor SM, Mehringer AM, Marks JL, Pomerleau OF. Smoking patterns and abstinence effects in smokers with no ADHD, childhood ADHD, and adult ADHD symptomatology. Addictive Behaviors. 2003;28:1149–1157. doi: 10.1016/s0306-4603(02)00223-x. [DOI] [PubMed] [Google Scholar]
- Pomerleau CS, Marks JL, Pomerleau OF. Who gets what symptom? Effects of psychiatric cofactors and nicotine dependence on patterns of nicotine withdrawal symptomatology. Nicotine & Tobacco Research. 2000;2:275–280. doi: 10.1080/14622200050147547. [DOI] [PubMed] [Google Scholar]
- Pomerleau OF, Downey KK, Stelson FW, Pomerleau CS. Cigarette smoking in adult patients diagnosed with attention deficit hyperactivity disorder. Journal of Substance Abuse. 1995;7:373–378. doi: 10.1016/0899-3289(95)90030-6. [DOI] [PubMed] [Google Scholar]
- Potter AS, Newhouse PA. Acute nicotine improves cognitive deficits in young adults with attention-deficit/hyperactivity disorder. Pharmacology, Biochemistry, and Behavior. 2008;88:407–417. doi: 10.1016/j.pbb.2007.09.014. [DOI] [PubMed] [Google Scholar]
- Rice JP, Reich T, Bucholz KK, Neuman RJ, Fishman R, Rochberg N, et al. Comparison of direct interview and family history diagnosis of alcohol dependence. Alcoholism: Clinical and Experimental Research. 1995;19:1018–1023. doi: 10.1111/j.1530-0277.1995.tb00983.x. [DOI] [PubMed] [Google Scholar]
- Upadhyaya HP, Carpenter MJ. Is attention deficit hyperactivity disorder symptom (ADHD) severity associated with tobacco use? American Journal on Addictions. 2008;17:195–198. doi: 10.1080/10550490802021937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velicer WF, Redding CA, Sun X, Prochaska JO. Demographic variables, smoking variables, and outcome across five studies. Health Psychology. 2007;26:278–287. doi: 10.1037/0278-6133.26.3.278. [DOI] [PubMed] [Google Scholar]
- Whalen CK, Jamner LD, Henker B, Delfino RJ, Lozano JM. The ADHD spectrum and everyday life: Experience sampling of adolescent moods, activities, smoking, and drinking. Child Development. 2002;73:209–227. doi: 10.1111/1467-8624.00401. [DOI] [PubMed] [Google Scholar]
- Wilens TE, Vitulano M, Upadhyaya H, Adamson J, Sawtelle R, Utzinger L, et al. Cigarette smoking associated with attention deficit hyperactivity disorder. Journal of Pediatrics. 2008;153:414–419. doi: 10.1016/j.jpeds.2008.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young SE, Friedman NP, Miyake A, Wilcutt EG, Corley RP, Haberstick BC, et al. Behavioral disinhibition: Liability for externalizing spectrum disorders and its genetic and environmental relation to response inhibition across adolescence. Journal of Abnormal Psychology. 2009;118:117–130. doi: 10.1037/a0014657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker M, Morris MK, Ingram SM, Morris RD, Bakeman R. Corcordance of self- and informant ratings of adults’ current and childhood attention-deficit/hyperactivity disorder symptoms. Psychological Assessment. 2002;14:379–389. doi: 10.1037//1040-3590.14.4.379. [DOI] [PubMed] [Google Scholar]