Abstract
Older adults are more likely than young to fall upon a loss of balance, yet the factors responsible for this difference are not well understood. This study investigated whether age-related differences in movement stability, limb support, and reactive stepping contribute to the greater likelihood of falling among older adults. Sixty young and 41 older, safety-harnessed, healthy adults were exposed to a novel and unexpected forward slip during a sit-to-stand task. More older than young adults fell (76% vs. 30%). Falls in both age groups were related to lesser stability and lower hip height at first step touchdown, with 97.1% of slip outcomes correctly classified based on these variables. Decreases in hip height at touchdown had over 20 times greater effect on the odds of falling than equivalent decreases in stability. Three age-differences placed older adults at greater risk of falling: older adults had lower and more slowly rising hips at slip onset, they were less likely to respond to slipping with forceful limb extension, and they placed their stepping foot less posterior to their center of mass. The first two differences, each associated with deficient limb support, reduced hip ascent and increased hip descent. The third difference resulted in lesser stability at step touchdown. These results suggest that deficient limb support in normal movement patterns and in the reactive response to a perturbation is a major contributor to the high incidence of falls in older adults. Improving proactive and reactive limb support should be a focus of fall prevention efforts.
Keywords: older adults, slips, stability, limb collapse
Introduction
Falls are a serious and growing health concern for older adults (Kannus et al., 1999). Their consequences include fear-related restriction of activities, serious injury, and even death (National Safety Council, 2004; Stel et al., 2004; Tinetti et al., 1988). Increased fall risk in older adults has been attributed to a variety of sensory, motor, cognitive, environmental, and medical factors (Moreland et al., 2003; Myers et al., 1996; Northridge et al., 1995). In particular, many aging-related changes in the postural responses used to maintain and regain balance have been identified (Maki and McIlroy, 1996; McIlroy and Maki, 1996; Mille et al., 2003; Stelmach et al., 1989). However, the mechanisms whereby older adults actually fall following a loss of balance have been little investigated (Lockhart et al., 2003; Pavol et al., 2001; Pijnappels et al., 2005). Arguably, understanding these mechanisms will allow for more effective intervention against falls by older adults.
Factors that can play large roles in falling are movement stability, vertical hip motion related to the limbs’ support of body weight, and reactive stepping for balance recovery (Pavol et al., 2004a). Instability (i.e. balance loss) in the transverse plane will lead to a fall unless stability is reestablished through a change in the base of support, typically by stepping. By normal definition, however, falls result from vertical descent of the body. Such descent will result from instability and/or from insufficient limb support. Of particular concern is the potential, during stepping, for the single support limb to collapse under the body’s weight (Pai et al., in press). If excessive hip descent occurs prior to step touchdown, the stepping limb will likely contact the ground in a highly flexed position from which it may be unable to arrest the body’s descent; a fall could result despite improved stability. At present, the relative roles of movement stability and limb support in falls by older versus young adults are unknown.
Recent experiments confirmed the general belief that healthy older adults are more likely than young to fall upon experiencing a novel and unexpected perturbation during movement, specifically a slip during a sit-to-stand (Pavol et al., 2002b). For a similar perturbation, falls by young adults were attributable to lesser stability at slip onset followed by limb collapse during stepping (Pavol et al., 2004a). This study therefore investigated whether age-related differences in movement stability, in vertical hip motion related to limb support, and in reactive stepping explained the greater likelihood of falling among older adults.
Methods
The subjects and experimental protocol have been detailed previously (Pavol et al., 2002b). Forty-one healthy older adults (mean ± SD age: 73 ± 5 years [range: 65-85]; height: 1.69 ± 0.09 m; mass: 79 ± 14 kg; 21 women) and 60 healthy young adults (age: 25 ± 5 years; height: 1.69 ± 0.10 m; mass: 67 ± 14 kg; 44 women) gave written informed consent and were paid to participate. Older adults were ambulatory and community-dwelling. Subjects were screened for neurological, musculoskeletal, cardiopulmonary, and other systemic disorders. Older adults were further screened for cognitive impairment, poor mobility, orthostatic hypotension, and bone loss (i.e. osteopenia or osteoporosis). Institutional Review Board approval was obtained.
Experimental Protocol
Slips were induced during a sit-to-stand movement using a side-by-side pair of low-friction platforms (dimensions: 31 × 29 × 2.5 cm; friction coefficient: 0.02). These were free to slide 24 cm forward upon release of their locking mechanisms. Platforms slid independently and latched into place in their maximum forward positions. Subjects wore a full-body safety harness, attached from the shoulders to a ceiling-mounted support by a pair of shock-absorbing ropes. A load cell measured the force exerted on the ropes.
Trials began with subjects sitting on a stool in a standardized position. One shoe rested on each platform; ankles were dorsiflexed 10°; knees were flexed 80°; arms were at the sides with the elbows flexed 90°. Subjects were told that they would initially be performing sit-to-stand trials and that, “later on,” a slip would take place. No practice was given and the trial, timing, and mechanisms of the slip were not provided. When cued, subjects were to stand up “as quickly as possible,” without using their arms, then remain standing still. After four normal sit-to-stand trials, a slip was induced without warning.
A computer controlled the timing of the slip, simultaneously releasing both platforms when the stool supported less than 10% body weight and the forward velocity of the body center of mass (COM) exceeded 20 cm/s. The slip was thereby initiated 16 ± 11 ms after seat-off. Release data were computed in real time from three force plates (AMTI, Newton, MA) located beneath the stool and each platform.
The kinematics of 26 markers attached to the bilateral upper and lower extremities, torso, and platforms were recorded by a motion capture system at 60 Hz (Peak Performance, Centennial, CO). Force plate and safety harness data were collected at 600 Hz.
Data Analysis
Positions of joint centers, heels, and toes in 3-dimensional space were computed from the filtered marker paths using transformations derived from anthropometric measurements. The position of the body COM was computed using sex- and age-dependent inertial parameters (de Leva, 1996; Pavol et al., 2002a) in a 13-segment kinematic model that included separate pelvis, torso, and head segments.
Slip outcomes were classified as falls if the midpoint of the hips descended within 5% body height of its initial seated height (Pavol et al., 2002b). Recoveries occurred if the average force on the safety harness did not exceed 4.5% body weight over any one-second period. The remaining outcomes were considered harness-affected. The “time of fall” was defined as the earlier of (a) when the average safety harness force first exceeded 4.5% body weight over the preceding one-second period or (b) 66 ms before the end of the first descent of the hip midpoint below the fall criterion.
Movement stability, vertical hip motion, and relative timing were determined at or between six events of interest of each slip. Slip onset was 16 ms before the displacement of either platform from its initial position exceeded three SD of the measurement noise. Mid-slip occurred when the forward displacement of the more posterior platform reached 12 cm. The start of hip descent corresponded to the first downward motion of the midpoint of the hips. Step initiation corresponded to the start of a simultaneous decrease in vertical force beneath the stepping foot and increase in vertical force beneath the support foot that continued until step lift-off. Step lift-off and touchdown were determined from the absence or presence of vertical force on the underlying force plates.
Movement stability was computed from the COM’s state (i.e. instantaneous position and velocity). The COM anterior position and forward velocity were found relative to the heel and support surface, respectively, of the posterior foot in ground contact. They were normalized by foot length and , respectively, where g is the acceleration due to gravity and bh is body height (McMahon, 1984). A mathematical model has previously established threshold boundaries, within the COM state space, for backward balance loss while standing on a nonslip or a frictionless surface (Pai and Iqbal, 1999). Outside of a given boundary, balance recovery is theoretically impossible under the corresponding surface conditions without a change in base of support. Stability was quantified as the shortest inwardly-directed distance from the applicable boundary to the instantaneous COM state (Pai et al., 2003). From slip onset until step touchdown, the stability boundary for backward balance loss on a frictionless surface applied. At step touchdown, the boundary for a nonslip surface was used for the 87% of slips in which touchdown was on a stationary surface; otherwise, the boundary for a frictionless surface was used.
Vertical hip motion and limb support were quantified by the height of the hip midpoint relative to the support surface, its upward velocity, and the changes in these variables. Hip variables were normalized by body height.
Where protective stepping occurred, the length of the initial step was computed as the posterior-directed position of the stepping ankle relative to the support ankle at step touchdown. Steps where lift-off occurred after the time of fall were excluded.
Statistics
Fisher’s exact test identified age-differences in the distribution of falls and recoveries, in the distribution of falls with and without stepping, and in the distribution of recoveries with one and multiple backward steps. Four young adults were excluded from analysis because their data were lost or their slip did not occur as intended due to equipment malfunction.
Five recoveries and two falls were atypical and were not analyzed further. Of these, two young adults recovered by sliding one platform backward, whereas the step initiation time and/or slip duration during recoveries by one older and two young adults were four or more SD above average. The atypical fallers, one young and one older, completed three protective steps and “fell” more than 0.93 s after slip onset (0.65 ± 0.10 s for all other fallers). Also excluded from further analysis, due to their low incidence, were no-step falls by young adults.
Univariate logistic regressions determined the influence, across all subjects, of each kinematic variable on the odds of falling (versus recovery). Two-factor analyses of variance (ANOVA) identified kinematic differences between slip outcomes (Recover, Fall) and age groups (Young, Older) among those who stepped in response to slipping. Simple effects were analyzed upon a significant interaction between factors. ANOVA were also performed to identify kinematic differences between older adults who recovered, those who fell after a protective step, and those who fell without stepping. The Dunnett test was used for post hoc comparison of no-step fallers to the other groups.
A forward, stepwise logistic regression analysis determined the influence of stability at step touchdown, hip height at step touchdown, and age group on the likelihood of falling. The likelihood ratio test with a cutoff probability of .05 was used for variable entry and a threshold probability of .5 was used for classification.
A significance level of .05 was used throughout. Analyses were performed using SPSS 12.0 (Chicago, IL).
Results
A greater proportion of older than young adults fell upon the novel and unexpected slip (p < .001; Table 1). Excluding harness-affected outcomes, 76% of older adults fell versus 30% of the young. While all but one recovery included a protective step, 30% of fallers did not step, regardless of age group (p = .52).
Table 1.
Outcomes of the slips induced in young and older adults.
| Slip Outcome |
Backward Steps |
Young (n = 56) |
Older (n = 41) |
|---|---|---|---|
| Recover | 0 | 1 | 0 |
| 1 | 22 | 1 | |
| ≥ 2 | 12 a | 8 | |
| Total | 35 | 9 | |
| Fall | 0 | 3 | 11 b |
| 1 | 9 | 14 | |
| ≥ 2 | 3 | 4 | |
| Total | 15 | 29 | |
| Harness- affected |
Total | 6 | 3 |
Occurrences are shown according to age group and the number of backward steps completed (i.e. stepping ankle posterior to the contralateral ankle at step touchdown) either during the recovery or prior to the time of the fall.
Includes 2 subjects whose first step was not backward.
Includes 1 subject who completed a forward step.
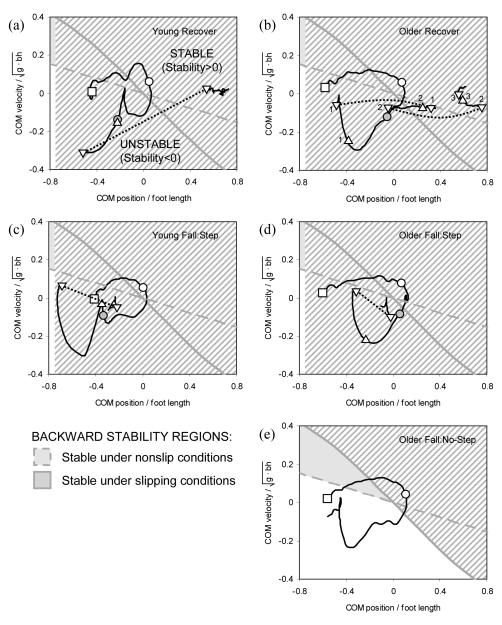
Slipping produced instability that necessitated a backward step for successful recovery; those who did not step fell (Figure 1; Table 2). While all individuals were classified as stable at slip onset, 98.5% were unstable by mid-slip. Overall, stability at or before mid-slip and step initiation was unrelated to slip outcome. Although young fallers were less stable than all others at slip onset, this difference disappeared by mid-slip.
Figure 1.
State-space diagram of the anteroposterior motion of the body center of mass (COM) relative to the base of support for representative (a) young and (b) older adults who recovered, (c) young and (d) older fallers who stepped, and (e) an older no-step faller. COM anterior position and forward velocity are expressed relative to the heel position and support surface velocity, respectively, of the posterior foot in ground contact. Positions and velocities are normalized to foot length and , respectively (g = acceleration due to gravity; bh = body height). The COM state trajectory is shown as a solid black line, with dotted lines indicating instantaneous changes in COM state at ground contact of the stepping foot. Also shown are the model-predicted threshold boundaries for backward balance loss while standing on a nonslip surface (dashed gray line) or on a frictionless surface (solid gray line; Pai and Iqbal, 1999). The shaded stability region inside each boundary comprises those COM states for which anteroposterior movement may be terminated under the indicated conditions without a backward step. Stability was quantified as the shortest inwardly-directed distance from the applicable boundary to the instantaneous COM state. Symbols correspond to the COM state at selected events: the start of motion (square), slip onset (open circle), first step initiation (filled circle), step lift-off (upward triangle), and step touchdown (downward triangle). The stepping sequence is numbered in (b). Trajectories for the fallers end at their time of “fall.”
Table 2.
Mean ± SD kinematics of anteroposterior stability as a function of age group, slip outcome, the presence or absence of a protective stepping response, and as related to the odds of falling.
| Variable | Young | Older | Odds Ratio | ||||
|---|---|---|---|---|---|---|---|
| Recover (n = 31) |
Fall:Step (n = 11) |
Recover (n = 8) |
Fall:Step (n = 18) |
Fall:No-Step (n = 10) |
For Falling a |
||
| At Slip Onset: | |||||||
| XCOM | (%ft len) | 0.5 ± 7.4 | −6.5 ± 7.7 d | 2.7 ± 8.6 | 6.9 ± 9.0 | 10.1 ± 10.4 | 0.81 |
| dXCOM/dt | (m/s ) | 0.10 ± 0.01 | 0.09 ± 0.02 | 0.09 ± 0.01 | 0.09 ± 0.01 | 0.09 ± 0.02 | 1.56 |
| Stability | (%) | 8.9 ± 4.1 | 4.5 ± 4.7 d | 9.4 ± 4.7 | 11.6 ± 4.5 | 13.0 ± 5.0 | 0.92 |
| At Mid-Slip:b | |||||||
| XCOM | (%ft len) | −10.6 ± 10.5 | −19.0 ± 5.5 | −15.3 ± 9.1 | −11.8 ± 12.9 | −9.0 ± 8.7 | 1.20 |
| dXCOM/dt | (m/s ) | −0.11 ± 0.08 | −0.12 ± 0.05 | −0.20 ± 0.07 f | −0.18 ± 0.06 f | −0.16 ± 0.06 | 1.45 |
| Stability | (%) | −14.6 ± 9.7 | −20.1 ± 6.1 | −25.3 ± 8.3 e | −21.4 ± 7.8 e | −18.9 ± 0.06 | 1.49 |
| At 1st Step Initiation: c | |||||||
| XCOM | (%ft len) | −15.8 ± 16.7 | −26.3 ± 16.2 | −22.4 ± 25.2 | −16.0 ± 25.9 | – | 1.23 |
| dXCOM/dt | (m/s ) | −0.06 ± 0.10 | −0.07 ± 0.07 | −0.14 ± 0.09 e | −0.10 ± 0.10 e | – | 1.11 |
| Stability | (%) | −13.2 ± 13.7 | −19.3 ± 10.0 | −23.2 ± 12.7 | −16.8 ± 13.8 | – | 1.27 |
| At 1st Step Touchdown: | |||||||
| XCOM | (%ft len) | 39.0 ± 23.8 | 6.5 ± 31.5 i | 20.7 ± 21.1 f | −15.3 ± 27.8 f,i | – | 6.67 j |
| dXCOM/dt | (m/s ) | −0.01 ± 0.06 | −0.01 ± 0.03 | −0.05 ± 0.04 | −0.02 ± 0.05 | – | 0.93 |
| Stability | (%) | 7.5 ± 8.6 | −0.8 ± 9.3 h | −0.6 ± 5.5 f | −4.7 ± 5.2 f,h | – | 4.55 j |
XCOM = center of mass (COM) anteriorly-directed position relative to heel of posterior foot in ground contact; dXCOM/dt = COM forward velocity relative to support surface of posterior foot in ground contact; Stability = distance of COM state from model-predicted boundary for backward balance loss (<0 indicates unstable); g = 9.81 m/s2; ft len = foot length; bh = body height.
Factor by which the odds of falling change for a decrease of 1 SD in the variable across all subjects.
Excludes 9 Young Recover, 4 Young Fall:Step, and 1 Older Recover subject who stepped before the posterior foot reached the slip midpoint.
Step initiation could not be identified in 1 Young Recover, 1 Young Fall:Step, and 3 Older Fall:Step subjects.
p < .05 vs. Young Recover and Older Fall:Step (interaction of age group and slip outcome).
p < .05
p < .01 vs. Young (main effect of age group).
p < .01
p < .001 vs. Recover (main effect of slip outcome).
p < .001 for Odds Ratio ≠ 1.
Among those who stepped, falls were in part related to lesser stability at step touchdown (Table 2). Fallers, regardless of age, took a shorter backward step and placed their stepping foot less posterior to their COM than those who recovered (Tables 2 and 3). Older adults, regardless of outcome, placed their stepping foot less posterior to their COM than did the young, resulting in lesser stability at step touchdown. Consistent with this difference, older adults were more likely to employ a second backward step for successful recovery (p = .006; Table 1).
Table 3.
Mean ± SD kinematics of the first protective step as a function of age group, slip outcome, and as related to the odds of falling.
| Variable | Young | Older | Odds Ratio | |||
|---|---|---|---|---|---|---|
| Recover (n = 31) |
Fall:Step (n = 11) |
Recover (n = 8) |
Fall:Step (n = 18) |
For Falling a |
||
| Onset to Step Init b | (ms) | 287 ±122 | 314 ± 94 | 291 ± 62 | 320 ± 87 | 0.70 |
| Descent to Step Init b | (ms) | 2 ± 77 | 70 ± 82 d | −56 ± 107 c | −13 ± 94 c,d | 0.65 |
| Step Duration | (ms) | 104 ± 36 | 117 ± 38 | 122 ± 28 | 97 ± 39 | 1.09 |
| Step Length | (%bh) | 12.5 ± 6.5 | 10.6 ± 6.6 d | 11.9 ± 4.8 | 5.6 ± 4.0 d | 2.36 e |
Onset = slip onset; Descent = start of hip descent; Step Init= step initiation; bh = body height.
Factor by which the odds of falling change for a decrease of 1 SD in the variable across all subjects.
Step initiation could not be identified in 1 Young Recover, 1 Young Fall:Step,and 3 Older Fall:Step subjects.
p < .01 vs. Young (main effect of age group).
p < .05 vs. Recover (main effect of slip outcome).
p < .01 for Odds Ratio ≠ 1.
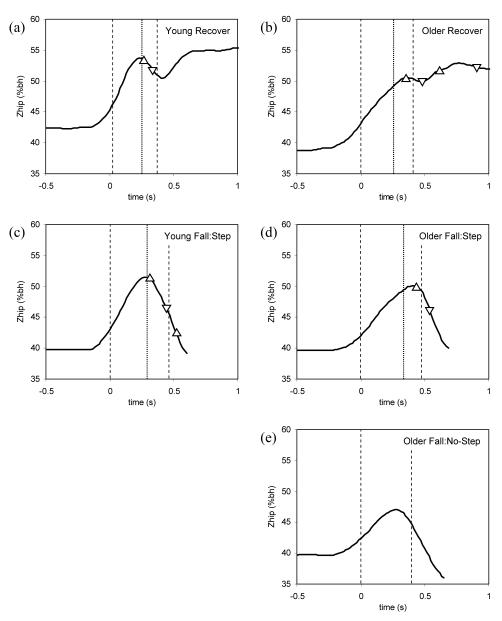
In both young and older adults, falls were most strongly related to deficient limb support (Figure 2; Table 4). To start, falls were related to lower hip heights and slower upward hip velocities at slip onset. These characteristics were exhibited by older adults regardless of outcome. After slip onset, everyone experienced hip descent. Falls were related to lower hip heights at the start of descent. In particular, the hips of older fallers started to descend from a lower height than in all others. Regardless of age, fallers then exhibited greater hip descent between step initiation and touchdown and greater corresponding increases in the speed of descent. Because older adults initiated stepping while their hips were still ascending (Table 3), they exhibited less hip descent over this period than did the young. The net result was that hip height at step touchdown did not differ between age groups for either outcome. Hip height at step touchdown was the strongest predictor of slip outcome; a decrease of one SD (3.6% body height) increased the odds of falling by a factor of 102.
Figure 2.
Hip height (ZHIP) kinematics for representative (a) young and (b) older adults who recovered, (c) young and (d) older fallers who stepped, and (e) an older no-step faller. Subjects are the same as in Figure 1. Dashed vertical lines indicate the onset and end of the slip. A dotted vertical line indicates the time of first step initiation. Step lift-offs and touchdowns are indicated by upward and downward triangles, respectively. Trajectories for the fallers end at their time of “fall.” bh = body height.
Table 4.
Mean ± SD kinematics of limb collapse as a function of age group, slip outcome, the presence or absence of a protective stepping response, and as related to the odds of falling.
| Variable | Young | Older | Odds Ratio | ||||
|---|---|---|---|---|---|---|---|
| Recover (n = 31) |
Fall:Step (n = 11) |
Recover (n = 8) |
Fall:Step (n = 18) |
Fall:No-Step (n = 10) |
For Falling a |
||
| At Slip Onset: | |||||||
| ZHIP | (%bh) | 43.9 ± 1.5 | 43.6 ± 1.7 | 42.8 ± 0.8 e | 41.8 ± 1.7 e | 42.4 ± 1.6 | 2.17 j |
| dZHIP/dt | (%bh/s) | 37.1 ± 8.2 | 38.0 ± 8.3 | 28.4 ± 6.0 e | 23.1 ± 5.3 e | 23.2 ± 4.8 | 2.27 j |
| At Start of Hip Descent: | |||||||
| From Onset | (ms) | 284 ± 110 | 245 ± 38 | 347 ± 95 d | 321 ± 74 d | 268 ± 35 | 1.16 |
| ZHIP | (%bh/s) | 52.1 ± 1.4 | 51.1 ± 1.8 | 51.3 ± 1.0 | 47.9 ± 2.2 c | 47.9 ± 2.2 i | 7.14 k |
| From Step Initiation to Touchdown:b | |||||||
| ΔZHIP | (%bh) | −1.2 ± 1.6 | −5.8 ± 2.6 h | −0.3 ± 1.7 e | −3.1 ± 1.9 e,h | – | 7.69 j |
| ΔdZHIP/dt | (%bh/s) | −17.5 ± 17.6 | −31.7 ± 22.8 f | −19.5 ± 16.3 | −38.4 ± 28.2 f | – | 2.56 j |
| At 1st Step Touchdown: | |||||||
| ZHIP | (%bh) | 50.7 ± 1.6 | 45.0 ± 2.3 h | 50.4 ± 1.1 | 44.1 ± 2.6 h | – | 101.95 k |
ZHIP = height of hip midpoint; dZHIP/dt = vertical velocity of hip midpoint; bh = body height; Δ = change
Factor by which the odds of falling change for a decrease of 1 SD in the variable across all subjects.
Step initiation could not be identified in 1 Young Recover, 1 Young Fall:Step, and 3 Older Fall:Step subjects.
p < .001 vs. Young Fall:Step and Older Recover (interaction of age group and slip outcome).
p < .01 vs. Young
p ≤ .001 vs. Young (main effect of age group).
p < .01 vs. Recover
p < .001 vs. Recover (main effect of slip outcome).
p < .01 vs. Older Recover.
p < .01
p < .001 for Odds Ratio ≠ 1.
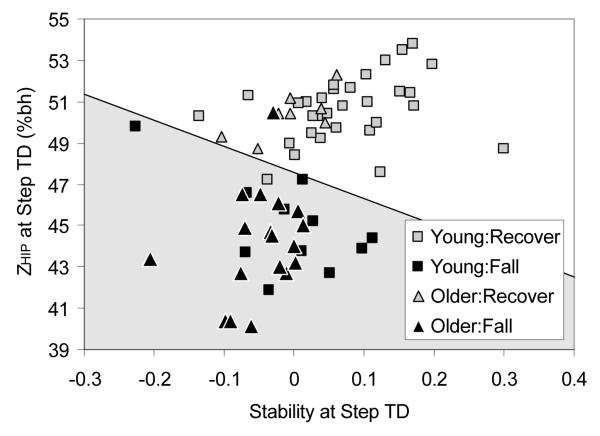
Lesser stability at step touchdown also increased the likelihood of falling due to a lower hip height at touchdown. A logistic model with these two variables correctly classified 97.1% of slip outcomes after a protective step (Figure 3). Age group did not enter into the model. Fallers were classified with both a sensitivity and a specificity of 97%.
Figure 3.
Relationship between anteroposterior stability at touchdown of the first protective step, the corresponding height of the hip midpoint (ZHIP, in %bh; bh = body height) at step touchdown, and the outcome of the induced slip in young and older adults. Individuals within the shaded region would be classified as likely to fall by the derived logistic regression model: p(fall) = 1/[1 + exp(−69.18 + 18.36 Stability + 1.454 ZHIP)] (p < .05 for all model coefficients). The logistic model correctly classified 97% of slip outcomes.
Finally, older fallers who did not step differed from those who did only in their lack of a stepping response (Tables 2 and 4). No measure of stability or hip height from slip onset through mid-slip and the start of descent differed between older fallers who did and did not step.
Discussion
While it has been reported that older adults are more likely than young to fall upon a loss of balance (Pavol et al., 2002b), the factors responsible for this difference are not well understood. This study therefore focused on the roles of movement stability and limb support in falls by young and older adults following a novel and unexpected slip during a sit-to-stand task.
In both young and older adults, recovery from a backward loss of balance depended on executing a stepping response that provided adequate stability and hip height at step touchdown. Slipping induced instability, and individuals who did not respond by stepping fell. Among those who stepped, fallers took a shorter step that placed the foot less posterior to the COM, resulting in lesser stability at step touchdown. Simultaneously, fallers exhibited greater collapse of the support limb due to deficient limb support while stepping. This was evidenced by greater and faster hip descent that resulted in a lower hip height at step touchdown.
Jointly, stability and hip height at step touchdown were highly predictive of falling, explaining 97% of slip outcomes. The logistic model indicated that the lesser the stability at step touchdown, the greater the hip height needed to avoid falling (Figure 3). In actuality, however, stability and hip height at step touchdown were directly related (r = 0.49; p < .001), with hip height being the primary determinant of slip outcome. A decrease in hip height increased the odds of falling over 20 times more than an equivalent decrease in stability. Avoiding a fall was thus vitally dependent on providing sufficient limb support to limit hip descent, thereby facilitating an effective step to reestablish stability. This supports previous assertions that the support limb plays a critical role in reactive stepping (Pai, 1999; Pavol et al., 2001; Pavol et al., 2004a; Pijnappels et al., 2004). Stability at step touchdown was less critical. In fact, five of eight older adults who recovered were unstable at step touchdown. But because these individuals limited their hip descent, their instability could be resolved by stepping again; all five took a second step backward. Such multiple stepping by older adults during balance recovery, more frequently than among the young, has often been observed (Luchies et al., 1994; McIlroy and Maki, 1996).
Older adults were 2.5 times more likely than young to fall upon the novel and unexpected slip, and this age-difference appeared to result from three factors. First, older and young adults differed in their execution of the sit-to-stand task, such that the hips of older adults were lower and rising more slowly at slip onset. Second, older adults were less likely than young to respond to the slip with the forceful knee and/or hip extensor moments needed, first to achieve adequate hip height and then to limit the collapse of the support limb during stepping (Pai et al., in press). As a result of these first two factors, the 76% of older adults who fell achieved lesser hip height than the young before starting to descend, and those who stepped experienced substantial support limb collapse upon withdrawal of the stepping limb. These led to low hip heights at step touchdown. Third and finally, older adults placed their stepping foot less posterior to their COM, resulting in lesser stability at step touchdown (or they failed to step entirely). Together, the low hip height and instability made it impossible to recover without stepping again and impossible to take such a step.
Notably, 28% of older adults failed to step, versus only 6% of young adults. Older fallers who did not step differed from those who did only in their absence of a stepping response. Thus, had they stepped, the no-step fallers likely still would have fallen due to their low hip height at the start of descent. In the case of a certain backward fall, a “squat response” with eccentric contraction of the hip and knee extensors is an effective strategy for reducing the body’s energy at landing impact (Robinovitch et al., 2004; Sandler and Robinovitch, 2001), and this is what the no-step fallers did. Arguably, the no-step fallers’ deficient limb support led them to suppress stepping, under the prediction that it would fail, and attempt to land safely instead.
The factors that placed older adults at greater risk of falling could arguably reflect differences in muscle strength, neuromuscular control, or both. Slower ascent during a sit-to-stand is characteristic of older adults (Pai et al., 1994) and has been associated with decreased strength (Corrigan and Bohannon, 2001; Schot et al., 2003). However, the deficient limb support after slip onset in the fallers was likely not due to a lack of strength. Firstly, hip ascent at slip onset did not differ between older adults who recovered and who fell, implying that these groups were similar in strength and that differences in neuromuscular control after slip onset played a key role in determining slip outcome. Secondly, the incidence of falls among these subjects decreased by a factor of three with each repeated exposure to the slipping perturbation (Pavol et al., 2002b), even though their strength almost certainly remained the same.
Rather than reflecting a lack of strength, the deficient limb support of the fallers after slip onset is likely attributable to their reactive responses. Slipping may lead to initially weakened limb support, as the slip-induced knee extension may induce short-latency stretch reflex responses by the knee flexors. Recovery therefore most likely relies on medium- and long-latency triggered responses. A spectrum of these exists within and across limbs and their selection is influenced by the “postural set” inherent to supraspinal control (Horak et al., 1989). The deficient limb support of the fallers may reflect a “postural set” that was biased, from lack of experience and/or readiness, towards an ineffective reactive response. More specifically, since simultaneous knee and hip extension are destabilizing during a backward loss of balance, the responses of the fallers may have been to limit their knee and hip extension moments in a failed initial attempt to maintain stability. If true, this would argue that when the objectives of resisting balance loss and providing limb support conflict, the latter is of priority in avoiding a fall.
The present findings correspond to novel and unexpected slips by healthy older adults during a sit-to-stand; the extent to which they apply to other perturbations, populations, or tasks is unknown. Experience and expectation have been shown to alter the reactive responses to a perturbation in a manner that would reduce the likelihood of falling (Horak et al., 1989; Pavol et al., 2004b). Thus, older adults may be less likely to respond poorly to a perturbation that is familiar. If true, training older adults’ reactive responses through exposure to a variety of perturbations might be a means of reducing fall incidence. However, there likely exist other aging-related differences that increase the likelihood that older adults will fall following a perturbation. For example, severe impairments in strength or balance may alter the mechanisms of falling among frailer older adults or those with certain medical conditions (e.g. Parkinson’s disease). The relative importance of the factors found to affect falling may also vary between tasks, particularly if hip height at perturbation onset varies.
In summary, the present results provide important insight into the greater incidence of falls among older adults. Falls by both young and older adults were most strongly associated with deficient limb support. This was primarily in the form of a deficient, ineffective reactive response that did not adequately maintain hip height after slip onset, thereby impeding the restoration of stability by protective stepping. Older adults were far more likely than young to exhibit such a response. In addition, older adults exhibited deficient limb support even before slip onset, with their slower ascent during the sit-to-stand task. The results thus suggest that deficient limb support, both in normal movement patterns and in the reactive response to a novel and unexpected perturbation, is a major contributor to the high incidence of falls in older adults. Improving proactive and reactive limb support should therefore be a focus of fall prevention efforts.
Acknowledgements
This work was funded by NIH R01-AG16727 (YCP) and the Whitaker Foundation (YCP). The experiments were conducted in the Department of Physical Therapy and Human Movement Science at Northwestern University Medical School. The authors thank the Buehler Center on Aging, Dr. Beatrice Edwards, and Dr. Folasade Ojo for assisting in subject recruitment and screening, Thang Bui for fabricating the platforms, Eileen Runtz, Genevieve Gagnon, Jason Wening, Steven Iannaccone, Kent Irwin, and Michelle Tyrrell for assisting in data collection and processing, and Dr. Feng Yang for assisting with the stability analysis.
References
- Corrigan D, Bohannon RW. Relationship between knee extension force and stand-up performance in community-dwelling elderly women. Archives of Physical Medicine and Rehabilitation. 2001;82:1666–1672. doi: 10.1053/apmr.2001.26811. [DOI] [PubMed] [Google Scholar]
- de Leva P. Adjustments to Zatsiorsky-Seluyanov’s segment inertia parameters. Journal of Biomechanics. 1996;29:1223–1230. doi: 10.1016/0021-9290(95)00178-6. [DOI] [PubMed] [Google Scholar]
- Horak FB, Diener HC, Nashner LM. Influence of central set on human postural responses. Journal of Neurophysiology. 1989;62:841–853. doi: 10.1152/jn.1989.62.4.841. [DOI] [PubMed] [Google Scholar]
- Kannus P, Parkkari J, Koskinen S, Niemi S, Palvanen M, Järvinen M, Vuori I. Fall-induced injuries and deaths among older adults. Journal of the American Medical Association. 1999;281:1895–1899. doi: 10.1001/jama.281.20.1895. [DOI] [PubMed] [Google Scholar]
- Lockhart TE, Woldstad JC, Smith JL. Effects of age-related gait changes on the biomechanics of slips and falls. Ergonomics. 2003;46:1136–1160. doi: 10.1080/0014013031000139491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchies CW, Alexander NB, Schultz AB, Ashton-Miller JA. Stepping responses of young and old adults to postural disturbances: kinematics. Journal of the American Geriatrics Society. 1994;42:506–512. doi: 10.1111/j.1532-5415.1994.tb04972.x. [DOI] [PubMed] [Google Scholar]
- Maki BE, McIlroy WE. Postural control in the older adult. Clinics in Geriatric Medicine. 1996;12:635–658. [PubMed] [Google Scholar]
- McIlroy WE, Maki BE. Age-related changes in compensatory stepping in response to unpredictable perturbations. Journal of Gerontology: Medical Sciences. 1996;51A:M289–M296. doi: 10.1093/gerona/51a.6.m289. [DOI] [PubMed] [Google Scholar]
- McMahon TA. Muscles, Reflexes, and Locomotion. Princeton University Press; Princeton, NJ: 1984. [Google Scholar]
- Mille M-L, Rogers MW, Martinez K, Hedman LD, Johnson ME, Lord SR, Fitzpatrick RC. Thresholds for inducing protective stepping responses to external perturbations of human standing. Journal of Neurophysiology. 2003;90:666–674. doi: 10.1152/jn.00974.2002. [DOI] [PubMed] [Google Scholar]
- Moreland J, Richardson J, Chan DH, O’Neill J, Bellissimo A, Grum RM, Shanks L. Evidence-based guidelines for the secondary prevention of falls in older adults. Gerontology. 2003;49:93–116. doi: 10.1159/000067948. [DOI] [PubMed] [Google Scholar]
- Myers AH, Young Y, Langlois JA. Prevention of falls in the elderly. Bone. 1996;18:87S–101S. doi: 10.1016/8756-3282(95)00384-3. [DOI] [PubMed] [Google Scholar]
- National Safety Council . Injury Facts. National Safety Council; Itasca, IL: 2004. [Google Scholar]
- Northridge ME, Nevitt MC, Kelsey JL, Link B. Home hazards and falls in the elderly: the role of health and functional status. American Journal of Public Health. 1995;85:509–515. doi: 10.2105/ajph.85.4.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai Y-C. Induced limb collapse in a sudden slip during termination of sit-to-stand. Journal of Biomechanics. 1999;32:1377–1382. doi: 10.1016/s0021-9290(99)00126-8. [DOI] [PubMed] [Google Scholar]
- Pai Y-C, Iqbal K. Simulated movement termination for balance recovery: can movement strategies be sought to maintain stability in the presence of slipping or forced sliding? Journal of Biomechanics. 1999;32:779–786. doi: 10.1016/s0021-9290(99)00074-3. [DOI] [PubMed] [Google Scholar]
- Pai Y-C, Naughton BJ, Chang RW, Rogers MW. Control of body centre of mass momentum during sit-to-stand among young and elderly adults. Gait and Posture. 1994;2:109–116. [Google Scholar]
- Pai Y-C, Wening JD, Runtz EF, Iqbal K, Pavol MJ. Role of feedforward control of movement stability in reducing slip-related balance loss and falls among older adults. Journal of Neurophysiology. 2003;90:755–762. doi: 10.1152/jn.01118.2002. [DOI] [PubMed] [Google Scholar]
- Pai Y-C, Yang F, Wening JD, Pavol MJ. Mechanisms of limb collapse following a slip among young and older adults. Journal of Biomechanics. doi: 10.1016/j.jbiomech.2005.07.004. in press. [DOI] [PubMed] [Google Scholar]
- Pavol MJ, Owings TM, Foley KT, Grabiner MD. Mechanisms leading to a fall from an induced trip in healthy older adults. Journal of Gerontology: Medical Sciences. 2001;56A:M428–M437. doi: 10.1093/gerona/56.7.m428. [DOI] [PubMed] [Google Scholar]
- Pavol MJ, Owings TM, Grabiner MD. Body segment inertial parameter estimation for the general population of older adults. Journal of Biomechanics. 2002a;35:707–712. doi: 10.1016/s0021-9290(01)00250-0. [DOI] [PubMed] [Google Scholar]
- Pavol MJ, Runtz EF, Edwards BJ, Pai Y-C. Age influences the outcome of a slipping perturbation during initial but not repeated exposures. Journal of Gerontology: Medical Sciences. 2002b;57A:M496–M503. doi: 10.1093/gerona/57.8.m496. [DOI] [PubMed] [Google Scholar]
- Pavol MJ, Runtz EF, Pai Y-C. Diminished stepping responses lead to a fall following a novel slip induced during a sit-to-stand. Gait and Posture. 2004a;20:154–162. doi: 10.1016/j.gaitpost.2003.08.004. [DOI] [PubMed] [Google Scholar]
- Pavol MJ, Runtz EF, Pai Y-C. Young and older adults exhibit proactive and reactive adaptations to repeated slip exposure. Journal of Gerontology: Medical Sciences. 2004b;59A:494–502. doi: 10.1093/gerona/59.5.m494. [DOI] [PubMed] [Google Scholar]
- Pijnappels M, Bobbert MF, van Dieen JH. Contribution of the support limb in control of angular momentum after tripping. Journal of Biomechanics. 2004;37:1811–1818. doi: 10.1016/j.jbiomech.2004.02.038. [DOI] [PubMed] [Google Scholar]
- Pijnappels M, Bobbert MF, van Dieen JH. Push-off reactions in recovery after tripping discriminate young subjects, older non-fallers, and older fallers. Gait and Posture. 2005;21:388–394. doi: 10.1016/j.gaitpost.2004.04.009. [DOI] [PubMed] [Google Scholar]
- Robinovitch SN, Brumer R, Maurer J. Effect of the “squat protective response” on impact velocity during backward falls. Journal of Biomechanics. 2004;37:1329–1337. doi: 10.1016/j.jbiomech.2003.12.015. [DOI] [PubMed] [Google Scholar]
- Sandler R, Robinovitch S. An analysis of the effect of lower extremity strength on impact severity during a backward fall. Journal of Biomechanical Engineering. 2001;123:590–598. doi: 10.1115/1.1408940. [DOI] [PubMed] [Google Scholar]
- Schot PK, Knutzen KM, Poole SM, Mrotek LA. Sit-to-stand performance of older adults following strength training. Research Quarterly for Exercise and Sport. 2003;74:1–8. doi: 10.1080/02701367.2003.10609058. [DOI] [PubMed] [Google Scholar]
- Stel VS, Smit JH, Pluijm SM, Lips P. Consequences of falling in older men and women and risk factors for health service use and functional decline. Age and Ageing. 2004;33:58–65. doi: 10.1093/ageing/afh028. [DOI] [PubMed] [Google Scholar]
- Stelmach GE, Teasdale N, Di Fabio RP, Phillips J. Age related decline in postural control mechanisms. International Journal of Aging and Human Development. 1989;29:205–223. doi: 10.2190/KKP0-W3Q5-6RDN-RXYT. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. New England Journal of Medicine. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]