Abstract
Allergic asthma is characterized by airway eosinophilia, increased mucin production and allergen-specific IgE. Fc gamma receptor IIb (FcγRIIb), an inhibitory IgG receptor, has recently emerged as a negative regulator of allergic diseases like anaphylaxis and allergic rhinitis. However, no studies to date have evaluated its role in allergic asthma. Our main objective was to study the role of FcγRIIb in allergic lung inflammation. We used a murine model of allergic airway inflammation. Inflammation was quantified by BAL inflammatory cells and airway mucin production. FcγRIIb expression was measured by qPCR and flow cytometry and the cytokines were quantified by ELISA. Compared to wild type animals, FcγRIIb deficient mice mount a vigorous allergic lung inflammation characterized by increased bronchoalveolar lavage fluid cellularity, eosinophilia and mucin content upon ragweed extract (RWE) challenge. RWE challenge in sensitized mice upregulated FcγRIIb in the lungs. Disruption of IFN-γ gene abrogated this upregulation. Treatment of naïve mice with the Th1-inducing agent CpG DNA increased FcγRIIb expression in the lungs. Furthermore, treatment of sensitized mice with CpG DNA prior to RWE challenge induced greater upregulation of FcγRIIb than RWE challenge alone. These observations indicated that RWE challenge upregulated FcγRIIb in the lungs by IFN-γ- and Th1-dependent mechanisms. RWE challenge upregulated FcγRIIb on pulmonary CD14+/MHC II+ mononuclear cells and CD11c+ cells. FcγRIIb deficient mice also exhibited an exaggerated RWE-specific IgE response upon sensitization when compared to wild type mice. We propose that FcγRIIb physiologically regulates allergic airway inflammation by two mechanisms: 1) allergen challenge mediates upregulation of FcγRIIb on pulmonary CD14+/MHC II+ mononuclear cells and CD11c+ cells by an IFN-γ dependent mechanism; and 2) by attenuating the allergen specific IgE response during sensitization. Thus, stimulating FcγRIIb may be a therapeutic strategy in allergic airway disorders.
Introduction
Allergic asthma is an airway inflammatory disease that is characterized by bronchial hyper-responsiveness, airway eosinophilia, goblet cell hyperplasia and production of allergen specific IgE. Cross-linking of the high affinity IgE receptor (FcεRI) on mast cells by IgE, in the presence of allergen activates Btk, PLC-gamma and PI3K [1]–[4]. This ultimately leads to production and release of pro-inflammatory substances like histamine, leukotrienes and cytokines that promote allergic inflammation. In addition, cytokines produced by allergen specific Th2 cells such as IL4, IL5, IL9, IL13 and IL25 also promote allergen-specific IgE production and allergic airway inflammation [5]–[14].
There is considerable amount of data on pro-inflammatory mediators that contribute to the development of allergic inflammation. However, relatively little is known about negative regulatory mechanisms that attenuate allergic inflammation. FcγRIIb is an inhibitory low affinity IgG receptor expressed on many inflammatory cells, including monocytes, macrophages, dendritic cells, B cells, mast cells and basophils[15]. It negatively regulates innate and adaptive immune responses, and has been shown to inhibit activation of mast cells, basophils, B cells and T cells [16]–[19]. It is composed of two Ig-like extra-cellular domains that bind the Fc region of IgG, one trans-membrane domain and an intra-cytoplasmic tail with an immuno-receptor phospho-tyrosine based inhibitory (ITIM) motif [15], [20]. Activation of FcγRIIb leads to recruitment of phosphatases to the ITIM motif that inhibits signal transduction from other activating receptors[21]. This block in the signaling cascade is the main reason for its potent inhibitory effects on BCR-mediated B-cell activation, TCR-mediated T-cell activation and FceRI-mediated mast cell activation [17], [22]–[24]. This inhibitory role is evident from studies of FcγRIIb deficient mice that are more susceptible to auto-immune diseases and IgE mediated anaphylaxis [25]–[32]. Only a few studies have shown a regulatory role of this receptor in animal models of allergic diseases. One study showed that IgG antibodies can prevent IgE mediated anaphylaxis in vivo through both antigen interception and FcγRIIb cross-linking [33]. Another study demonstrated a regulatory role of FcγRIIb in a murine model of allergic rhinitis[34]. However, the role of this receptor in allergic lung inflammation has not been elucidated.
We recently showed in a gene micro-array analysis (GEO accession number GSE18083) that allergen challenge upregulated 352 genes in the lungs four hours after the challenge [35]. Careful review of that list revealed FcγRIIb as one of the genes upregulated. Based on this observation, we hypothesized that FcγRIIb may play a regulatory role in allergic airway inflammation. Here we show that mice lacking FcγRIIb have exaggerated allergic airway inflammation, suggesting its negative regulatory role in asthma. We further show that allergen challenge upregulates FcγRIIb in the lungs in an IFN-γ dependent mechanism. Our results indicate that FcγRIIb upregulation physiologically reduces allergic airway inflammation.
Materials and Methods
Ethics Statement
All animal experiments were approved by the Institutional Animal Care and Use Committee of the University of Texas Medical Branch at Galveston.
Mice
Female BALB/c mice, 6–8 wk old, were purchased from the Harlan Laboratories (Indianapolis, IN). BALB/c IFN-γ KO, C57Bl6 FcγRIIb knock-out (KO) and C57Bl6 WT mice were purchased from Jackson laboratories (Bar Harbor, Maine). BALB/c FcγRIIb knock-out (KO) mice were purchased from Taconics (Albany, NY). All mice were maintained in a specific pathogen-free environment throughout the experiment.
Model of Allergic Sensitization and Challenge
WT Balb/c, IFN-γ KO or FcγRIIb KO mice were sensitized by two intraperitoneal (i.p.) injections of endotoxin-free RWE (150 µg) and alum on days 0 and 4. On day 11, allergen challenge was performed by intranasal (i.n.) instillation of RWE (200 µg) in anesthetized mice. Mice were sacrificed at various time points as indicated after the challenge and bronchoalveolar lavage (BAL) fluid, blood, lung and spleen specimens were collected. Mice sensitized but not challenged served as the zero time point. For the Th1/CpG experiments, 35 µg CpG or GpC oligonucleotides were administered intranasally in 50 µl of sterile PBS [36].
Ragweed Extract
We have previously shown that endotoxin contamination alters the inflammatory cell recruitment following allergen challenge [37]. To avoid this problem endotoxin-free ragweed (lot XP56-D10-1320) was purchased from Greer Laboratories (Lenoir, NC).
Measurement of Allergic Airway Inflammation
For BAL fluid analyses, mice were anesthetized with an i.p. injection of ketamine and xylazine, tracheotomy performed and the trachea was cannulated. BAL of both lungs was performed twice with 0.7 ml of sterile PBS (pH 7.3) through the tracheal cannula with a syringe. Total cell counts were performed on BAL samples and differential cell counts were done on cytocentrifuge preparations (Cytospin 3; Thermo Shandon) stained with Wright-Giemsa, counting 200 cells from each animal. Mucin was quantified using mucin-binding lectin Jacalin (Calbiochem, La jolla, CA) as described previously [38]. Aliquots of BAL fluid were diluted 1∶100, 1∶1000 and 1∶10000, added in triplicate to individual wells of microtiter ELISA plates and incubated for 2 h at room temperature. Plates were washed and blocked with 5% BSA and 0.02% biotinylated jacalin was added. After 1 h incubation at room temperature, plates were washed extensively, then developed with alkaline phosphatase-conjugated avidin (Sigma) and nitrophenylphosphate (Sigma) and quantified by comparison with a mucin (Sigma) standard curve. The morphometric method we described previously was used to quantify mucin in lung epithelium[39]. Briefly, coronal sections of the 4% paraformaldehyde-fixed lungs were stained with PAS stain. Morphometirc analysis was done using Metamorph™ software (Version 5, Universal Imaging, Downingtown, Pennsylvania). Several images from five different levels per lung (three animals per group) were obtained and reassembled using the montage stage stitching algorithm of the Metamorph™ software. The integrated morphometric analysis function was used to transform total pixel area of the signal to µm2 per mm of peribronchial diameter.
Measurement of Enhanced Pause Index (PENH Index)
PENH was assessed by a method previously described [40] using a dual chamber whole body plethysmograph obtained from Buxco (Troy, NY). Mice were exposed for 3 min to nebulized PBS and subsequently to 37.5 mg/ml nebulized methacholine (Sigma Chemicals) in PBS using the AeroSonic ultrasonic nebulizer. After each nebulization, recordings were taken for 4 min. The PENH values measured during each 4 min sequence were averaged and expressed as the percentage of baseline PENH values after PBS exposure.
Quantification of Serum RWE-Specific IgE
Serum was collected from RWE-sensitized WT and FcγRIIb KO mice 4 h after challenge with PBS (WT PBS and KO PBS) or RWE (WT RWE and KO RWE). RWE-specific IgE was quantified using standard sandwich ELISA technique and comparison with an IgE standard curve as described previously[41].
Antigen Recall Assay
Splenocytes were obtained from sensitized WT and FcγRIIb KO mice after crushing the spleens and making single cell suspensions. These were incubated with or without RWE for 3 d and Th2 cytokines (IL-4, IL-5, IL-9 and IL-13) were quantified in the supernatants using standard ELISA techniques as described previously [36], [41], [42].
Quantitative RT-PCR
Balb/c mice sensitized with RWE were challenged with either RWE or PBS. Mice were sacrificed and lungs collected at 1, 4, 24, 72 and 240 h post-challenge. RNA was extracted and quantitative PCR analyses were performed using the SYBR green real time PCR kit (Applied Biosystems) as described previously [35], [43]. Transcript copy numbers for FcγRIIb and beta-actin were quantified by comparing to a standard curve generated from serial log-dilutions of the target DNA [44], [45]. FcγRIIb signal was normalized to beta-actin. Table 1 shows the primers used.
Table 1. Primers used for quantitative PCR analyses.
| Gene | Forwad Primer | Reverse Primer |
| β-actin | ACACCTTCTACAATGAGCTG | GGATCTTCATGAGGTAGTCC |
| FcγRIIb | ATCTTGCTGCTGGGACTCAT | TGACTGTGGCCTTAAACGTG |
Flow Cytometry
Single cell suspensions of lung and spleen were analyzed by flow cytometry [46]. Cells were washed 3X with PBS and resuspended in FACS staining media containing 0.5% FBS in PBS. To study expression of FcγRIIb on dendritic cells, 1×106 cells were incubated with anti-CD11c PE (Pharmingen, Clone HL3) and anti-CD16/CD32-biotin (Pharmingen, Clone 2.4G2) for 30 min on ice protected from light. After three washes, cells were incubated with Streptavidin Cy-chrome (Pharmingen, #554062). Species and isotype matched antibodies were used as controls. FACS analysis was performed using analytical Flow cytometer (FACS Scan, Beckton Dickinson) with CellQuest software (San jose, CA). Further analyses were performed using FlowJo software (Tree Star Inc., Ashland, OR). Similarly, FcγRIIb expression on macrophages (anti-CD14; Clone rmC5-3, Pharmingen and anti-MHC class II-FITC; Miltenyi biotech, #130-081-601) and B cells (anti-B220, Clone RA3-6B2, Pharmingen) was studied.
Statistical Methods
There were 4–6 animals in each group and results are representative of at least two independent experiments. Statistical significance between groups was determined using Student's T test.
Results
Disruption of the FcγRIIb Gene Augments Allergic Airway Inflammation
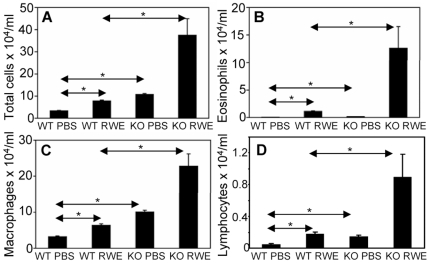
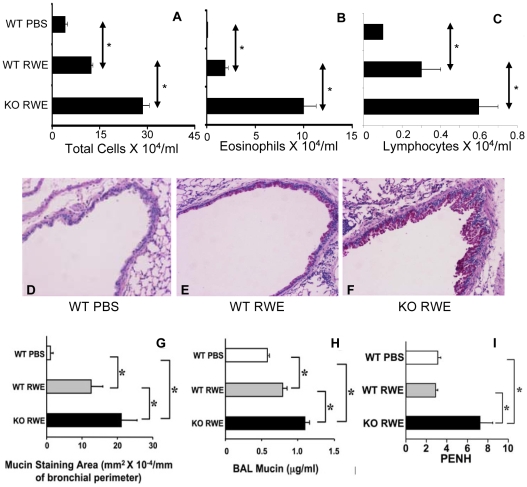
We assessed the biological role of FcγRIIb in a murine model of allergic asthma. C57Bl6 wild type (WT) and C57Bl6 FcγRIIb knock-out (KO) mice were sensitized and then challenged with RWE. RWE challenge in WT mice recruited 3-fold more total inflammatory cells, 10-fold more eosinophils, 2-fold more lymphocytes and macrophages ( Figure 1A, 1B, 1C and 1D ). Disrupting the FcγRIIb gene further increased total inflammatory cells (5-fold), eosinophils (12-fold), lymphocytes (5-fold) and macrophages (3.6-fold) in the BAL ( Figure 1A, 1B, 1C and 1D ). To determine the reproducibility of this result in a different strain of mouse, we repeated this experiment in Balb/c mice. RWE challenge in WT Balb/c mice recruited 3-fold more total inflammatory cells, 32-fold more eosinophils and 3-fold more lymphocytes in BAL as compared to PBS challenge ( Figure 2A, 2B and 2C ) at 72 h post-challenge. Similar to our observations in C57Bl6 mice, RWE challenge in Balb/c FcγRIIb KO mice further increased total cells (2.3-fold increase), eosinophils (5.2-fold increase) and lymphocytes (2-fold increase) in BAL fluid as compared to WT mice ( Figure 2A, 2B and 2C ). RWE challenge in WT mice increased mucin-containing cells in the airway ( Figures 2D, 2E and 2G ) and mucin levels in BAL fluid ( Figure 2H ). RWE challenge in mice that lacked FcγRIIb further increased mucin-containing cells in the airway ( Figures 2E, 2F and 2G ) and mucin levels in BAL fluid ( Figure 2H ) as compared to WT mice. RWE challenge in mice that lacked FcγRIIb induced greater increase in enhanced pause (PENH) index as compared to wild type mice ( Figure 2I ).
Figure 1. Role of FcγRIIb in allergic airway inflammation.
(A, B, C and D) Total inflammatory cells (A), eosinophils (B), macrophages (C) and lymphocytes (D) were quantified in BAL of C57Bl6 RWE-sensitized WT and FcγRIIb KO mice challenged with either PBS (WT PBS and KO PBS) or RWE (WT RWE and KO RWE). *, p<0.05.
Figure 2. Role of FcγRIIb in allergic airway inflammation.
(A, B and C) Total inflammatory cells (A), eosinophils (B) and lymphocytes (C) were quantified in BAL of Balb/c RWE-sensitized WT and FcγRIIb KO mice challenged with either PBS (WT PBS) or RWE (WT RWE and KO RWE). (D, E and F) Lung sections were obtained from RWE-sensitized WT and FcγRIIb KO mice challenged with either PBS (WT PBS) or RWE (WT RWE & KO RWE). These sections were stained with PAS to identify mucin containing cells. (G) Mucin containing cells in the lung sections were analyzed by morphometric analyses of PAS staining area. (H) Mucin was quantified in BAL samples by ELISA using biotinylated mucin binding lectin. (I) WT and FcγRIIb KO mice were sensitized with RWE and challenged with either PBS (WT PBS) or RWE (WT & KO RWE). PENH was measured by Buxco whole body plethysmography. *, p<0.05.
RWE Challenge Upregulates FcγRIIb in the Lungs by an IFN-γ-Dependent Mechanism
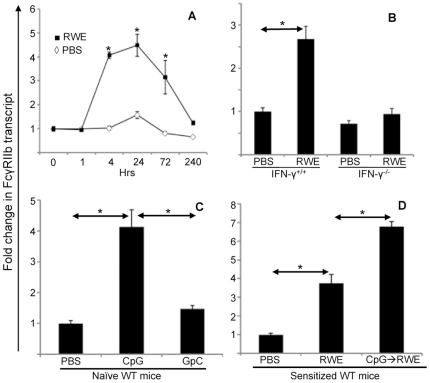
Since allergen challenge recruits inflammatory cells that express FcγRIIb to the lungs, and lack of FcγRIIb further increases this inflammation, we hypothesized that allergen challenge upregulates FcγRIIb on pulmonary inflammatory cells. Quantitative PCR of lung mRNA confirmed that RWE challenge upregulated FcγRIIb as early as 4 hours post-RWE challenge, and gene expression peaked at 24 h ( Figure 3A ). This upregulation was sustained till 10 d after challenge ( Figure 3A ). Prior studies have shown that IFN-γ and Th1 response can inhibit allergic inflammation [39], [47]–[50]. Since our studies suggested that FcγRIIb inhibited allergic airway inflammation, we sought to determine whether its upregulation was Th1 or IFN-γ dependent. RWE challenge upregulated FcγRIIb in wild type mice but not in IFN-γ KO mice ( Figure 3B ). IFN-γ KO mice also exhibited greater allergic airway inflammation when compared to WT mice (data not shown). Treatment of naïve wild type mice with the Th1-inducing CpG DNA significantly upregulated FcγRIIb; however, GpC control DNA (which does not induce IFN-γ) failed to do so ( Figure 3C ). Furthermore, intra-nasal administration of CpG DNA, but not GpC DNA, 48 h prior to RWE challenge in wild type mice enhanced RWE-induced FcγRIIb upregulation ( Figure 3D ). These findings indicated that RWE-challenge upregulated FcγRIIb by an IFN-γ and Th1-dependent mechanism.
Figure 3. Expression of FcγRIIb in the lungs after RWE challenge.
(A) Balb/c mice sensitized with RWE and challenged with either RWE (filled squares) or PBS (open diamond). Mice were sacrificed 1, 4, 24, 72 and 240 h after challenge, lungs were collected and RNA was extracted. Quantitative PCR (qPCR) analysis for FcγRIIb was performed on these RNA samples using SYBR green Real time PCR kit (Applied biosystems). (B) Wild-type and INF-γ deficient BALB/c mice were sensitized with RWE, and challenged with PBS or RWE. 4 h later, the lungs were collected and qPCR for FcγRIIb was performed. (C) Naïve wild-type mice were challenged with PBS, CpG DNA or GpC DNA. 4 hours post-challenge lungs were collected and FcγRIIb expression was quantified by qPCR. (D) Wild-type BALB/c mice were sensitized with RWE. The mice were pre-treated with PBS (PBS challenge or RWE challenge group) or 35 µg CpG oligonucleotide intranasally (CpG → RWE) 48 h prior to RWE challenge. 4 h post-challenge, lungs were collected and qPCR for FcγRIIb was performed. * = p<0.05.
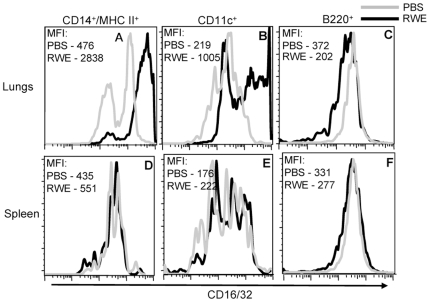
RWE Challenge Upregulates FcγRIIb in CD14+ MHC II+ Mononuclear Cells and CD11c+ Cells in the Lungs
We verified the upregulation of FcγRIIb in the lungs by flow cytometry measurements of single cell suspensions of whole lungs. RWE challenge upregulated FcγRIIb on pulmonary CD14+/MHC II+ cells ( Figure 4A ) and on CD11c+ cells ( Figure 4B ), but not on B220+ cells ( Figure 4C ). Furthermore, intrapulmonary RWE challenge failed to upregulate FcγRIIb expression on these cells in the spleen ( Figures 4D, 4E and 4F ). This suggested that RWE challenge upregulated FcγRIIb expression on CD14+/MHC II+ and CD11c+ cells in the challenged organ (lungs) with no detectable systemic upregulation.
Figure 4. Identification of cells in the lungs that upregulate FcγRIIb after RWE challenge.
Single cell lung and spleen suspensions were prepared from RWE-sensitized BALB/c mice that were challenged with PBS or RWE. A multi-color FACS analysis for FcγRIIb and cell specific markers (CD14/MHC II for macrophages, CD11c for dendritic cells and B220 for B cells) was performed on these cells. FcγRIIb expression is shown for PBS challenged (grey histogram) and RWE challenged (black histogram) mice. FcγRIIb expression is increased on CD14+/MHC II+ and CD11c+ gated cells. Data from one representative animal in each group. MFI, Mean fluorescence intensity.
Disruption of the FcγRIIb Gene Augments Serum RWE-Specific IgE Levels after Antigen Sensitization, but Does Not Affect Th2 Cytokine Production in Antigen Recall Assay
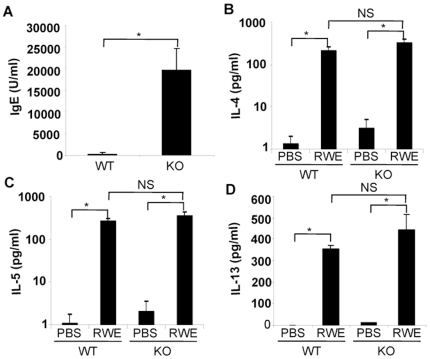
Building on the observation that FcγRIIb regulated RWE challenge induced allergic lung inflammation, we examined its role in the sensitization process and antigen-driven Th2 cytokine production. As shown in Figure 5A , sensitized FcγRIIb KO mice had significantly higher RWE-specific IgE levels when compared to WT mice. We hypothesized that this enhanced IgE response in FcγRIIb KO mice was due to an exaggerated Th2 response. To test this hypothesis we performed an antigen recall assay using splenocytes from sensitized WT and FcγRIIb KO mice. Importantly, IL-4, IL-5 and IL-13 production in response to RWE was similar in WT and FcγRIIb KO mice ( Figures 5B, 5C and 5D ). Thus, disruption of FcγRIIb increased antigen-specific IgE levels in vivo without increasing antigen-induced Th2 cytokine production.
Figure 5. Role of FcγRIIb on serum IgE levels and antigen-induced Th2 cytokine production.
(A) RWE-specific IgE levels in serum were quantified in sensitized WT and FcγRIIb KO mice. (B, C and D) Splenocytes from sensitized wild-type and FcγRIIb KO mice were cultured with PBS or RWE for four days, and the cell supernatants were analyzed for IL-4, IL-5 and IL-13 levels by ELISA. *, P<0.05; NS, not significant.
Discussion
FcγRIIb is an inhibitory IgG receptor that can prevent BCR-, TCR- and FcεRI-mediated activation of B-, T- and mast cells by recruitment of SHIP to its ITIM motif [17], [51]–[54]. Multiple studies have looked at the role of FcγRIIb in down regulating specific allergic inflammatory cells in vitro. However, only a few studies have demonstrated its regulatory role in animal models of allergic disease. One study showed that disruption of FcγRIIb increased nasal eosinophilia in mice sensitized and challenged with Schistosoma egg antigen (SEA)[34]. Another study suggested a role of upregulated FcγRIIb in the inhibition of anaphylaxis[55]. In this study we demonstrated the role of FcγRIIb in regulating allergen-induced eosinophilic inflammation in the lungs. We further showed for the first time that allergen challenge upregulated FcγRIIb in the lungs.
The genes that regulate FcγRIIb expression in the lungs have not been described. Here we demonstrate that IFNγ plays a critical role in mediating allergen-induced FcγRIIb upregulation. We recently showed that IFNγ plays an important role in upregulating Th1-associated genes such as p47 and p65 GTPases, Socs1, Cxcl9 and Cxcl10 after allergen challenge [35]. Our observations in the current manuscript indicate that FcγRIIb is another allergen-induced IFNγ-dependent, CpG DNA inducible gene. Other reports have demonstrated upregulation of FcγRIIb on naïve human blood-derived monocytes and dendritic cells by IL-4[56], [57]. This apparent disparity between mice and humans in regulation of FcγRIIb by Th1 and Th2 cytokines could be due to tissue-specific differences in the regulation of FcγRIIb, or may reflect divergence in regulation of the gene in the two species.
RWE challenge upregulated FcγRIIb on pulmonary CD14+/MHC II+ macrophages in this study. Alveolar macrophages have been shown to play a regulatory role in airway inflammation. Monocytes/macrophages account for a large number of cells in the airway in quiescent asthma. Removal of macrophages from the airways of patients with asthma by BAL enhances eosinophilic inflammation[58]. There could be several mechanisms by which alveolar macrophages contribute to this regulatory function. Macrophages express functional FcεRI and cross-linking leads to activation and secretion of pro-inflammatory cytokines[59], [60]. It is possible that the balance of expression of FcγRIIb and FcεRI by alveolar macrophages determines a pro-inflammatory versus anti-inflammatory role of these cells. In the present study, RWE challenge also upregulated CXCL9 and CXCL10 (data not shown), which are Th1-associated chemokines that have been shown to inhibit allergic airway inflammation[61], [62]. It is possible that airway monocytes secrete these anti-inflammatory cytokines upon FcγRIIb ligation, and mediate attenuation of allergic inflammation. Another possibility is that RWE challenge induces the anti-inflammatory PGE2 by macrophages in an FcγRIIb dependent fashion[63].
Allergen challenge also upregulated FcγRIIb on pulmonary CD11c+ cells, most likely dendritic cells. Myeloid dendritic cells have been shown to regulate allergic airway inflammation by inducing a Th2 immune response[64], [65]. FcγRIIb on DCs can potentially inhibit the induction of the Th2 cytokine response. However in the present study, the antigen recall assay failed to show an increase in IL-4 and IL-5 production in FcγRIIb knockout mice. These observations suggested that FcγRIIb does not affect the antigen presenting and Th2 skewing properties of DCs.
A previous study showed a critical role of Fc receptor gamma chain in the sensitization phase of allergic airway inflammation [66]. In the present study, absence of FcγRIIb increased levels of allergen specific IgE after sensitization. This indicated that FcγRIIb can specifically attenuate IgE humoral responses, suggesting its specific regulatory role in allergic lung inflammation. IgE production by the differentiating B cell requires class switch recombination (CSR) to Cε that is CD40 and IL-4 dependent[67], [68]. FcγRIIb deficient splenocytes made similar amount of IL-4 as wild type splenocytes in allergen recall assay. Thus, T cell-secreted IL-4 might not be involved in the FcγRIIb-mediated suppression of Cε class switch. One possibility is that FcγRIIb suppresses CD40L expression on T cells thus reducing the stimulus for IgE class switch. Another mechanism might involve regulation of IgE production by DCs. CSR in B cells is regulated by the expression of BAFF (BLyS) and APRIL on DCs[69]–[71]. One report showed inhibition of B cell IgE production by DCs via direct cell-cell interaction as well as by soluble factors including TGF-β and IFN-γ[72]. It is possible that FcγRIIb expression affects the ability of DCs to regulate IgE production by B cells. Yet another possibility is that the enhanced IgE response in FcγRIIb deficient mice is independent of the Th2 T cell response.
Upregulation of FcγRIIb on mast cells after exposure to allergen can lead to co-ligation of FcγRIIb and FcεRI by allergen and inhibit activation/degranulation of the mast cell. This concept was exploited in recent studies using two novel bio-engineered fusion proteins, one that consists of human Fc regions of IgG1 and IgE linked together and another a fusion protein made by linking an allergen to human IgG1 Fc region[73]. These proteins block pro-inflammatory mediator and cytokine release from allergic cells and prevent skin, lung and systemic allergic reactivity in a murine model[16], [73]–[77]. Our study demonstrates that FcγRIIb-dependent regulatory mechanism(s) control allergic airway inflammation, making this inhibitory receptor a physiologically relevant therapeutic target in allergic asthma. FcγRIIb appears to inhibit both allergic sensitization (possibly by attenuating the IgE response) as well as allergic inflammation from allergen exposure (possibly by upregulating FcγRIIb expression on inflammatory cells in the target organ). Stimulating the inhibitory FcγRIIb receptor is an elegant strategy because it is naturally upregulated by allergen exposure, and has the potential of controlling allergic inflammation by inhibiting multiple cells and mediators. In this manner it is likely to alter airway remodeling and disease progression.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work was supported by grants from National Institutes of Health (NIH) RO1HL071163 (S.S.), National Institute of Allergy and Infectious Disease (NIAID), PO1AI062885-01 (I.B., S.S.), National Heart, Lung, and Blood Institute (NHLBI) Proteomics Initiative, NO1HV-28184 (S.S.) and National Institute of Environmental Health Sciences (NIEHS) Center Grant, EOS 006677 (I.B., S.S.). The funders had no role in study design, data collection and analysis, decision to publish or preparation of manuscript.
References
- 1.Kalesnikoff J, Galli SJ. New developments in mast cell biology. Nat Immunol. 2008;9:1215–1223. doi: 10.1038/ni.f.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Laffargue M, Calvez R, Finan P, Trifilieff A, Barbier M, et al. Phosphoinositide 3-kinase gamma is an essential amplifier of mast cell function. Immunity. 2002;16:441–451. doi: 10.1016/s1074-7613(02)00282-0. [DOI] [PubMed] [Google Scholar]
- 3.Kawakami Y, Kitaura J, Satterthwaite AB, Kato RM, Asai K, et al. Redundant and opposing functions of two tyrosine kinases, Btk and Lyn, in mast cell activation. J Immunol. 2000;165:1210–1219. doi: 10.4049/jimmunol.165.3.1210. [DOI] [PubMed] [Google Scholar]
- 4.Manetz TS, Gonzalez-Espinosa C, Arudchandran R, Xirasagar S, Tybulewicz V, et al. Vav1 regulates phospholipase cgamma activation and calcium responses in mast cells. Mol Cell Biol. 2001;21:3763–3774. doi: 10.1128/MCB.21.11.3763-3774.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohn L, Homer RJ, Marinov A, Rankin J, Bottomly K. Induction of airway mucus production By T helper 2 (Th2) cells: a critical role for interleukin 4 in cell recruitment but not mucus production. J Exp Med. 1997;186:1737–1747. doi: 10.1084/jem.186.10.1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Corry DB, Folkesson HG, Warnock ML, Erle DJ, Matthay MA, et al. Interleukin 4, but not interleukin 5 or eosinophils, is required in a murine model of acute airway hyperreactivity. J Exp Med. 1996;183:109–117. doi: 10.1084/jem.183.1.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grunig G, Warnock M, Wakil AE, Venkayya R, Brombacher F, et al. Requirement for IL-13 independently of IL-4 in experimental asthma. Science. 1998;282:2261–2263. doi: 10.1126/science.282.5397.2261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhu Z, Homer RJ, Wang Z, Chen Q, Geba GP, et al. Pulmonary expression of interleukin-13 causes inflammation, mucus hypersecretion, subepithelial fibrosis, physiologic abnormalities, and eotaxin production. J Clin Invest. 1999;103:779–788. doi: 10.1172/JCI5909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Foster PS, Hogan SP, Ramsay AJ, Matthaei KI, Young IG. Interleukin 5 deficiency abolishes eosinophilia, airways hyperreactivity, and lung damage in a mouse asthma model. J Exp Med. 1996;183:195–201. doi: 10.1084/jem.183.1.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robinson DS, Hamid Q, Ying S, Tsicopoulos A, Barkans J, et al. Predominant TH2-like bronchoalveolar T-lymphocyte population in atopic asthma. N Engl J Med. 1992;326:298–304. doi: 10.1056/NEJM199201303260504. [DOI] [PubMed] [Google Scholar]
- 11.Ray A, Cohn L. Th2 cells and GATA-3 in asthma: new insights into the regulation of airway inflammation. J Clin Invest. 1999;104:985–993. doi: 10.1172/JCI8204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Herrick CA, Bottomly K. To respond or not to respond: T cells in allergic asthma. Nat Rev Immunol. 2003;3:405–412. doi: 10.1038/nri1084. [DOI] [PubMed] [Google Scholar]
- 13.Passalacqua G, Ciprandi G. Allergy and the lung. Clin Exp Immunol. 2008;153(Suppl 1):12–16. doi: 10.1111/j.1365-2249.2008.03715.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goswami S, Angkasekwinai P, Shan M, Greenlee KJ, Barranco WT, et al. Divergent functions for airway epithelial matrix metalloproteinase 7 and retinoic acid in experimental asthma. Nat Immunol. 2009 doi: 10.1038/ni.1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ravetch JV, Bolland S. IgG Fc receptors. Annu Rev Immunol. 2001;19:275–290. doi: 10.1146/annurev.immunol.19.1.275. [DOI] [PubMed] [Google Scholar]
- 16.Zhang K, Kepley CL, Terada T, Zhu D, Perez H, et al. Inhibition of allergen-specific IgE reactivity by a human Ig Fcgamma-Fcepsilon bifunctional fusion protein. J Allergy Clin Immunol. 2004;114:321–327. doi: 10.1016/j.jaci.2004.03.058. [DOI] [PubMed] [Google Scholar]
- 17.Daeron M, Malbec O, Latour S, Arock M, Fridman WH. Regulation of high-affinity IgE receptor-mediated mast cell activation by murine low-affinity IgG receptors. J Clin Invest. 1995;95:577–585. doi: 10.1172/JCI117701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kepley CL, Cambier JC, Morel PA, Lujan D, Ortega E, et al. Negative regulation of FcepsilonRI signaling by FcgammaRII costimulation in human blood basophils. J Allergy Clin Immunol. 2000;106:337–348. doi: 10.1067/mai.2000.107931. [DOI] [PubMed] [Google Scholar]
- 19.Rabinovitch N, Gelfand EW. Expression of functional activating and inhibitory Fcgamma receptors on human B cells. Int Arch Allergy Immunol. 2004;133:285–294. doi: 10.1159/000076836. [DOI] [PubMed] [Google Scholar]
- 20.Muta T, Kurosaki T, Misulovin Z, Sanchez M, Nussenzweig MC, et al. A 13-amino-acid motif in the cytoplasmic domain of Fc gamma RIIB modulates B-cell receptor signalling. Nature. 1994;368:70–73. doi: 10.1038/368070a0. [DOI] [PubMed] [Google Scholar]
- 21.Bruhns P, Vely F, Malbec O, Fridman WH, Vivier E, et al. Molecular basis of the recruitment of the SH2 domain-containing inositol 5-phosphatases SHIP1 and SHIP2 by fcgamma RIIB. J Biol Chem. 2000;275:37357–37364. doi: 10.1074/jbc.M003518200. [DOI] [PubMed] [Google Scholar]
- 22.Jensen WA, Marschner S, Ott VL, Cambier JC. FcgammaRIIB-mediated inhibition of T-cell receptor signal transduction involves the phosphorylation of SH2-containing inositol 5-phosphatase (SHIP), dephosphorylation of the linker of activated T-cells (LAT) and inhibition of calcium mobilization. Biochem Soc Trans. 2001;29:840–846. doi: 10.1042/0300-5127:0290840. [DOI] [PubMed] [Google Scholar]
- 23.Qin D, Wu J, Vora KA, Ravetch JV, Szakal AK, et al. Fc gamma receptor IIB on follicular dendritic cells regulates the B cell recall response. J Immunol. 2000;164:6268–6275. doi: 10.4049/jimmunol.164.12.6268. [DOI] [PubMed] [Google Scholar]
- 24.Phillips NE, Parker DC. Fc-dependent inhibition of mouse B cell activation by whole anti-mu antibodies. J Immunol. 1983;130:602–606. [PubMed] [Google Scholar]
- 25.Nakamura A, Yuasa T, Ujike A, Ono M, Nukiwa T, et al. Fcgamma receptor IIB-deficient mice develop Goodpasture's syndrome upon immunization with type IV collagen: a novel murine model for autoimmune glomerular basement membrane disease. J Exp Med. 2000;191:899–906. doi: 10.1084/jem.191.5.899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yuasa T, Kubo S, Yoshino T, Ujike A, Matsumura K, et al. Deletion of fcgamma receptor IIB renders H-2(b) mice susceptible to collagen-induced arthritis. J Exp Med. 1999;189:187–194. doi: 10.1084/jem.189.1.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bolland S, Yim YS, Tus K, Wakeland EK, Ravetch JV. Genetic modifiers of systemic lupus erythematosus in FcgammaRIIB(-/-) mice. J Exp Med. 2002;195:1167–1174. doi: 10.1084/jem.20020165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ujike A, Ishikawa Y, Ono M, Yuasa T, Yoshino T, et al. Modulation of immunoglobulin (Ig)E-mediated systemic anaphylaxis by low-affinity Fc receptors for IgG. J Exp Med. 1999;189:1573–1579. doi: 10.1084/jem.189.10.1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pritchard NR, Cutler AJ, Uribe S, Chadban SJ, Morley BJ, et al. Autoimmune-prone mice share a promoter haplotype associated with reduced expression and function of the Fc receptor FcgammaRII. Curr Biol. 2000;10:227–230. doi: 10.1016/s0960-9822(00)00344-4. [DOI] [PubMed] [Google Scholar]
- 30.Stefanescu RN, Olferiev M, Liu Y, Pricop L. Inhibitory Fc gamma receptors: from gene to disease. J Clin Immunol. 2004;24:315–326. doi: 10.1023/B:JOCI.0000029105.47772.04. [DOI] [PubMed] [Google Scholar]
- 31.Suzuki Y, Shirato I, Okumura K, Ravetch JV, Takai T, et al. Distinct contribution of Fc receptors and angiotensin II-dependent pathways in anti-GBM glomerulonephritis. Kidney Int. 1998;54:1166–1174. doi: 10.1046/j.1523-1755.1998.00108.x. [DOI] [PubMed] [Google Scholar]
- 32.Takai T, Ono M, Hikida M, Ohmori H, Ravetch JV. Augmented humoral and anaphylactic responses in Fc gamma RII-deficient mice. Nature. 1996;379:346–349. doi: 10.1038/379346a0. [DOI] [PubMed] [Google Scholar]
- 33.Strait RT, Morris SC, Finkelman FD. IgG-blocking antibodies inhibit IgE-mediated anaphylaxis in vivo through both antigen interception and Fc gamma RIIb cross-linking. J Clin Invest. 2006;116:833–841. doi: 10.1172/JCI25575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Watanabe T, Okano M, Hattori H, Yoshino T, Ohno N, et al. Roles of FcgammaRIIB in nasal eosinophilia and IgE production in murine allergic rhinitis. Am J Respir Crit Care Med. 2004;169:105–112. doi: 10.1164/rccm.200302-239OC. [DOI] [PubMed] [Google Scholar]
- 35.Dharajiya N, Vaidya S, Sinha M, Luxon B, Boldogh I, et al. Allergen challenge induces Ifng dependent GTPases in the lungs as part of a Th1 transcriptome response in a murine model of allergic asthma. PLoS One. 2009;4:e8172. doi: 10.1371/journal.pone.0008172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sur S, Wild JS, Choudhury BK, Sur N, Alam R, et al. Long term prevention of allergic lung inflammation in a mouse model of asthma by CpG oligodeoxynucleotides. J Immunol. 1999;162:6284–6293. [PubMed] [Google Scholar]
- 37.Hunt LW, Gleich GJ, Ohnishi T, Weiler DA, Mansfield ES, et al. Endotoxin contamination causes neutrophilia following pulmonary allergen challenge. Am J Respir Crit Care Med. 1994;149:1471–1475. doi: 10.1164/ajrccm.149.6.8004300. [DOI] [PubMed] [Google Scholar]
- 38.Lee SH, Kiss A, Xu J, Qian Y, Bashoura L, et al. Airway glycoprotein secretion parallels production and predicts airway obstruction in pulmonary allergy. J Allergy Clin Immunol. 2004;113:72–78. doi: 10.1016/j.jaci.2003.09.039. [DOI] [PubMed] [Google Scholar]
- 39.Boldogh I, Bacsi A, Choudhury BK, Dharajiya N, Alam R, et al. ROS generated by pollen NADPH oxidase provide a signal that augments antigen-induced allergic airway inflammation. J Clin Invest. 2005;115:2169–2179. doi: 10.1172/JCI24422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Justice JP, Shibata Y, Sur S, Mustafa J, Fan M, et al. IL-10 gene knockout attenuates allergen-induced airway hyperresponsiveness in C57BL/6 mice. Am J Physiol Lung Cell Mol Physiol. 2001;280:L363–L368. doi: 10.1152/ajplung.2001.280.2.L363. [DOI] [PubMed] [Google Scholar]
- 41.Wild JS, Sigounas A, Sur N, Siddiqui MS, Alam R, et al. IFN-gamma-inducing factor (IL-18) increases allergic sensitization, serum IgE, Th2 cytokines, and airway eosinophilia in a mouse model of allergic asthma. J Immunol. 2000;164:2701–2710. doi: 10.4049/jimmunol.164.5.2701. [DOI] [PubMed] [Google Scholar]
- 42.Choudhury BK, Wild JS, Alam R, Klinman DM, Boldogh I, et al. In vivo role of p38 mitogen-activated protein kinase in mediating the anti-inflammatory effects of CpG oligodeoxynucleotide in murine asthma. J Immunol. 2002;169:5955–5961. doi: 10.4049/jimmunol.169.10.5955. [DOI] [PubMed] [Google Scholar]
- 43.Dharajiya N, Choudhury BK, Bacsi A, Boldogh I, Alam R, et al. Inhibiting pollen reduced nicotinamide adenine dinucleotide phosphate oxidase-induced signal by intrapulmonary administration of antioxidants blocks allergic airway inflammation. J Allergy Clin Immunol. 2007;119:646–653. doi: 10.1016/j.jaci.2006.11.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rohr UP, Wulf MA, Stahn S, Steidl U, Haas R, et al. Fast and reliable titration of recombinant adeno-associated virus type-2 using quantitative real-time PCR. J Virol Methods. 2002;106:81–88. doi: 10.1016/s0166-0934(02)00138-6. [DOI] [PubMed] [Google Scholar]
- 45.Scheurer ME, Dillon LM, Chen Z, Follen M, dler-Storthz K. Absolute quantitative real-time polymerase chain reaction for the measurement of human papillomavirus E7 mRNA in cervical cytobrush specimens. Infect Agent Cancer. 2007;2:8. doi: 10.1186/1750-9378-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hoffmann PR, Gurary A, Hoffmann FW, Jourdan-Le SC, Teeters K, et al. A new approach for analyzing cellular infiltration during allergic airway inflammation. J Immunol Methods. 2007;328:21–33. doi: 10.1016/j.jim.2007.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Flaishon L, Topilski I, Shoseyov D, Hershkoviz R, Fireman E, et al. Cutting edge: anti-inflammatory properties of low levels of IFN-gamma. J Immunol. 2002;168:3707–3711. doi: 10.4049/jimmunol.168.8.3707. [DOI] [PubMed] [Google Scholar]
- 48.Fulkerson PC, Zimmermann N, Brandt EB, Muntel EE, Doepker MP, et al. Negative regulation of eosinophil recruitment to the lung by the chemokine monokine induced by IFN-gamma (Mig, CXCL9). Proc Natl Acad Sci U S A. 2004;101:1987–1992. doi: 10.1073/pnas.0308544100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gavett SH, O'Hearn DJ, Li X, Huang SK, Finkelman FD, et al. Interleukin 12 inhibits antigen-induced airway hyperresponsiveness, inflammation, and Th2 cytokine expression in mice. J Exp Med. 1995;182:1527–1536. doi: 10.1084/jem.182.5.1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Huang TJ, MacAry PA, Eynott P, Moussavi A, Daniel KC, et al. Allergen-specific Th1 cells counteract efferent Th2 cell-dependent bronchial hyperresponsiveness and eosinophilic inflammation partly via IFN-gamma. J Immunol. 2001;166:207–217. doi: 10.4049/jimmunol.166.1.207. [DOI] [PubMed] [Google Scholar]
- 51.Bruhns P, Vely F, Malbec O, Fridman WH, Vivier E, et al. Molecular basis of the recruitment of the SH2 domain-containing inositol 5-phosphatases SHIP1 and SHIP2 by fcgamma RIIB. J Biol Chem. 2000;275:37357–37364. doi: 10.1074/jbc.M003518200. [DOI] [PubMed] [Google Scholar]
- 52.Jensen WA, Marschner S, Ott VL, Cambier JC. FcgammaRIIB-mediated inhibition of T-cell receptor signal transduction involves the phosphorylation of SH2-containing inositol 5-phosphatase (SHIP), dephosphorylation of the linker of activated T-cells (LAT) and inhibition of calcium mobilization. Biochem Soc Trans. 2001;29:840–846. doi: 10.1042/0300-5127:0290840. [DOI] [PubMed] [Google Scholar]
- 53.Phillips NE, Parker DC. Fc-dependent inhibition of mouse B cell activation by whole anti-mu antibodies. J Immunol. 1983;130:602–606. [PubMed] [Google Scholar]
- 54.Qin D, Wu J, Vora KA, Ravetch JV, Szakal AK, et al. Fc gamma receptor IIB on follicular dendritic cells regulates the B cell recall response. J Immunol. 2000;164:6268–6275. doi: 10.4049/jimmunol.164.12.6268. [DOI] [PubMed] [Google Scholar]
- 55.Strait RT, Morris SC, Finkelman FD. IgG-blocking antibodies inhibit IgE-mediated anaphylaxis in vivo through both antigen interception and Fc gamma RIIb cross-linking. J Clin Invest. 2006;116:833–841. doi: 10.1172/JCI25575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tridandapani S, Siefker K, Teillaud JL, Carter JE, Wewers MD, et al. Regulated expression and inhibitory function of Fcgamma RIIb in human monocytic cells. J Biol Chem. 2002;277:5082–5089. doi: 10.1074/jbc.M110277200. [DOI] [PubMed] [Google Scholar]
- 57.Pricop L, Redecha P, Teillaud JL, Frey J, Fridman WH, et al. Differential modulation of stimulatory and inhibitory Fc gamma receptors on human monocytes by Th1 and Th2 cytokines. J Immunol. 2001;166:531–537. doi: 10.4049/jimmunol.166.1.531. [DOI] [PubMed] [Google Scholar]
- 58.Hunt LW, Gleich GJ, Kita H, Weiler DA, Schroeder DR, et al. Removal of bronchoalveolar cells augments the late eosinophilic response to segmental allergen challenge. Clin Exp Allergy. 2002;32:210–216. doi: 10.1046/j.1365-2222.2002.01228.x. [DOI] [PubMed] [Google Scholar]
- 59.Williams J, Johnson S, Mascali JJ, Smith H, Rosenwasser LJ, et al. Regulation of low affinity IgE receptor (CD23) expression on mononuclear phagocytes in normal and asthmatic subjects. J Immunol. 1992;149:2823–2829. [PubMed] [Google Scholar]
- 60.Joseph M, Tonnel AB, Torpier G, Capron A, Arnoux B, et al. Involvement of immunoglobulin E in the secretory processes of alveolar macrophages from asthmatic patients. J Clin Invest. 1983;71:221–230. doi: 10.1172/JCI110762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gangur V, Simons FE, HayGlass KT. IP-10 mediated reinforcement of human type 1 cytokine synthesis to environmental allergens among non-atopic subjects. Int Arch Allergy Immunol. 1999;118:387–390. doi: 10.1159/000024144. [DOI] [PubMed] [Google Scholar]
- 62.Fulkerson PC, Zimmermann N, Brandt EB, Muntel EE, Doepker MP, et al. Negative regulation of eosinophil recruitment to the lung by the chemokine monokine induced by IFN-gamma (Mig, CXCL9). Proc Natl Acad Sci U S A. 2004;101:1987–1992. doi: 10.1073/pnas.0308544100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhang Y, Liu S, Liu J, Zhang T, Shen Q, et al. Immune Complex/Ig Negatively Regulate TLR4-Triggered Inflammatory Response in Macrophages through Fc{gamma}RIIb-Dependent PGE2 Production. J Immunol. 2009;182:554–562. doi: 10.4049/jimmunol.182.1.554. [DOI] [PubMed] [Google Scholar]
- 64.Caron G, Delneste Y, Roelandts E, Duez C, Bonnefoy JY, et al. Histamine polarizes human dendritic cells into Th2 cell-promoting effector dendritic cells. J Immunol. 2001;167:3682–3686. doi: 10.4049/jimmunol.167.7.3682. [DOI] [PubMed] [Google Scholar]
- 65.Li Y, Chu N, Rostami A, Zhang GX. Dendritic cells transduced with SOCS-3 exhibit a tolerogenic/DC2 phenotype that directs type 2 Th cell differentiation in vitro and in vivo. J Immunol. 2006;177:1679–1688. doi: 10.4049/jimmunol.177.3.1679. [DOI] [PubMed] [Google Scholar]
- 66.Kitamura K, Takeda K, Koya T, Miyahara N, Kodama T, et al. Critical role of the Fc receptor gamma-chain on APCs in the development of allergen-induced airway hyperresponsiveness and inflammation. J Immunol. 2007;178:480–488. doi: 10.4049/jimmunol.178.1.480. [DOI] [PubMed] [Google Scholar]
- 67.Geha RS, Jabara HH, Brodeur SR. The regulation of immunoglobulin E class-switch recombination. Nat Rev Immunol. 2003;3:721–732. doi: 10.1038/nri1181. [DOI] [PubMed] [Google Scholar]
- 68.Poulsen LK, Hummelshoj L. Triggers of IgE class switching and allergy development. Ann Med. 2007;39:440–456. doi: 10.1080/07853890701449354. [DOI] [PubMed] [Google Scholar]
- 69.Bossen C, Schneider P. BAFF, APRIL and their receptors: structure, function and signaling. Semin Immunol. 2006;18:263–275. doi: 10.1016/j.smim.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 70.He B, Raab-Traub N, Casali P, Cerutti A. EBV-encoded latent membrane protein 1 cooperates with BAFF/BLyS and APRIL to induce T cell-independent Ig heavy chain class switching. J Immunol. 2003;171:5215–5224. doi: 10.4049/jimmunol.171.10.5215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Litinskiy MB, Nardelli B, Hilbert DM, He B, Schaffer A, et al. DCs induce CD40-independent immunoglobulin class switching through BLyS and APRIL. Nat Immunol. 2002;3:822–829. doi: 10.1038/ni829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Obayashi K, Doi T, Koyasu S. Dendritic cells suppress IgE production in B cells. Int Immunol. 2007;19:217–226. doi: 10.1093/intimm/dxl138. [DOI] [PubMed] [Google Scholar]
- 73.Saxon A, Kepley C, Zhang K. “Accentuate the negative, eliminate the positive”: engineering allergy therapeutics to block allergic reactivity through negative signaling. J Allergy Clin Immunol. 2008;121:320–325. doi: 10.1016/j.jaci.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 74.Zhu D, Kepley CL, Zhang K, Terada T, Yamada T, et al. A chimeric human-cat fusion protein blocks cat-induced allergy. Nat Med. 2005;11:446–449. doi: 10.1038/nm1219. [DOI] [PubMed] [Google Scholar]
- 75.Zhu D, Kepley CL, Zhang M, Zhang K, Saxon A. A novel human immunoglobulin Fc gamma Fc epsilon bifunctional fusion protein inhibits Fc epsilon RI-mediated degranulation. Nat Med. 2002;8:518–521. doi: 10.1038/nm0502-518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mertsching E, Bafetti L, Hess H, Perper S, Giza K, et al. A mouse Fcgamma-Fcepsilon protein that inhibits mast cells through activation of FcgammaRIIB, SH2 domain-containing inositol phosphatase 1, and SH2 domain-containing protein tyrosine phosphatases. J Allergy Clin Immunol. 2008;121:441–447. doi: 10.1016/j.jaci.2007.08.051. [DOI] [PubMed] [Google Scholar]
- 77.Yamada T, Zhu D, Zhang K, Saxon A. Inhibition of interleukin-4-induced class switch recombination by a human immunoglobulin Fc gamma-Fc epsilon chimeric protein. J Biol Chem. 2003;278:32818–32824. doi: 10.1074/jbc.M304590200. [DOI] [PubMed] [Google Scholar]