Abstract
Adult bone marrow multipotential stromal cells (MSCs) hold great promise in regenerative medicine and tissue engineering. However, due to their low numbers upon harvesting, MSCs need to be expanded in vitro without biasing future differentiation for optimal utility. In this concept paper, we focus on the potential use of epidermal growth factor (EGF), prototypal growth factor for enhancing the harvesting and/or differentiation of MSCs. Soluble EGF was shown to augment MSC proliferation while preserving early progenitors within MSC population, and thus did not induce differentiation. However, tethered form of EGF was shown to promote osteogenic differentiation. Soluble EGF was also shown to increase paracrine secretions including VEGF and HGF from MSC. Thus, soluble EGF can be used not only to expand MSC in vitro, but also to enhance paracrine secretion through drug-releasing MSC-encapsulated scaffolds in vivo. Tethered EGF can also be utilized to direct MSC towards osteogenic lineage both in vitro and in vivo.
1. Multipotential Stromal Cells/Mesenchymal Stem Cells (MSCs)
1.1. MSC Overviews
Adult bone marrow multipotential stromal cells/mesenchymal stem cells (MSCs) are multipotent cells with strong paracrine activities of various growth factors [1–7]. These cells were originally isolated as colony forming adherent fibroblast-like cells or colony forming unit fibroblastic cells (CFU-Fs) from bone marrow suspension [8], but it was subsequently realized that these cells carry multipotency capable of differentiating into multiple cell lineages including osteoblasts, chondrocytes, adipocytes, smooth muscle cells, skeletal and cardiac myocytes, endothelial cells, and neurons [3–6, 9, 10].
Initially MSC differentiation and direct incorporation into local tissues undergoing wound healing and tissue regenerations were regarded as a primary mechanism of MSC action; however, the contribution of MSC differentiation and direct incorporation into regenerating tissues remains debated [11]. For example, some groups showed that MSCs were differentiated and incorporated as myocardiocytes or vascular cells (endothelial cell and vascular smooth muscle cells) in newly formed vessels in MSC-based cardioplasty models in rat (isogenic and allogenic MSC transplantation) and pig (allogenic transplantation) [11–14]. Human MSCs from adult bone marrow were engrafted and differentiated into cardiomyocytes within myocardium of SCID mice [15]. In contrast, another group showed that bone marrow-derived cells were not incorporated into newly formed blood vessels in hindlimb ischemia in mice allogenic bone marrow transplantation model [16]. Direct incorporation and differentiation of transplanted MSC into keratinocytes and vascular cells were also shown in mice dermal wound healing model (allogenic MSC transplantation) [17–19], whereas others showed that MSC differentiation of transplanted MSCs into keratinocytes and vascular cells was not observed in mice dermal wound healing model (allogenic MSC transplantation) and mice limb ischemia models (isogenic MSC transplantation) [20, 21]. Furthermore, even when there is an early incorporation noted into regenerating tissue, these cells are largely gone by one month[15]. The efficacy of engraftment of transplanted MSC was varied, suggesting the presence of other mechanisms of MSC-mediated promotion of tissue regeneration [7, 11].
One such mechanism is paracrine secretion of growth factors and cytokines. MSCs are known to have a strong paracrine capability of various growth factors and cytokines such as vascular endothelial growth factor (VEGF) or hepatocyte growth factor (HGF), which promote angiogenesis and wound healing [7, 22–24]. Indeed, conditioned medium of MSCs was also shown to promote angiogenesis or wound healing in animal models, suggesting the crucial role of MSC's paracrine action in promotion of angiogenesis and wound healing [21, 23, 25].
1.2. In Vitro Expansion of MSCs
A major thrust is to use MSCs pharmacologically. Even if the physiological involvement of MSCs is debatable, studies have shown injected MSCs to home to wounded tissues [1, 2, 4, 5]. However, the availability of sufficient number of MSCs that retain their multipotency and paracrine activity is prerequisite for successful MSC-based therapeutics and tissue engineering. MSCs are present only in low frequency in the bone marrow (one in 105-106 bone marrow mononuclear cells, lower frequency in aged hosts) [5, 26], thus, MSCs harvested from the bone marrow for pharmacological uses need to be expanded in vitro. These cells are expandable in vitro [3, 27] and that is one of the desirable characteristics about MSCs.
Current in vitro expansion strategies generally rely on the use of fetal bovine serum, but this practice not only carries inherent disease risks [28] but also hampers standardization that is critical to establishing a broad clinical adoption. Another issue about current MSC expansion is the loss of differentiation, proliferative, and therapeutic potentials of MSCs through in vitro expansion process [29, 30]. Thus, there is a strong motivation to identify factors that might be used in serum-free formulations to expand MSC in vitro without losing differentiation capacity and to preserve self-renewal and therapeutic potentials of undifferentiated MSCs [31].
A recent report found that a combination of transforming growth factor-β (TGF-β), platelet-derived growth factor (PDGF), and basic fibroblast growth factors (bFGF) could replace serum component in cell culture medium to expand human MSCs ex vivo without compromising differentiation potentials, at least up to 5 passages [32]. Subsequently, serum and animal component-free MSC culture media (STEMPRO MSC SFM, from Invitrogen, Carlsbad, CA) (MesenCult-ACF Culture Kit, from STEMCELL Technologies, Vancouver, Canada) became available on the market. The manufacturers claim that the culture media exert superior MSC proliferation potentials while maintaining differentiation potentials and colony formation potentials, as supported by at least one study [33]. Those chemically-defined media should be safer and thus better for clinical settings, although the proprietary composition of these culture media may hinder acceptance in preclinical and clinical usage.
1.3. Heterogenous Populations within MSC Preparations
Although MSCs possess vast proliferative potential, have the capacity for self-renewal, and give rise to differentiated progenies, all MSC populations analyzed by clonal assays were shown to be heterogeneous, with individual cells capable of various differentiation potential and expansion capacity [34]. Thus, the International Society for Cellular Therapy proposed MSCs to be named as multipotential mesenchymal stromal cells, which can also be abbreviated as MSCs [35]. MSC populations in vitro are known to include early progenitors or rapidly self-renewing (RS)-cells as well as large slow replicating mature/senescent cells. It is early progenitors or RS-cells which retain strong multipotentiality for differentiation. In contrast, mature/senescent cells have only limited differentiation potentials, and these cells predominate in multiple passaged MSCs [27, 29, 36].
One of the prominent characteristics about MSCs is their ability to produce colonies after being seeded at low density [8]. Generation of a single-cell derived colony relies on the presence of early progenitors or RS cells in MSC preparations. In other words, assessment of the colony formation unit (CFU) can be used to gauge the proportion of colony forming early progenitors in MSC population [29, 37, 38].
The number of MSC within bone marrow mononuclear cells was shown to decrease with age [26]. Moreover, both MSCs from old donors and high passaged MSCs were shown to have decreased paracrine activity and reduced organ protective effects upon transplantation [30, 39]. These reports clearly suggest the importance of preserving early progenitors or RS cells in MSC preparation to maintain therapeutic potentials of MSCs.
1.4. MSC Expansion and Differentiation Potentials
To preserve early progenitors within MSC populations, self-renewal of these cells has to be maintained or even enhanced through in vitro MSC expansion process. Otherwise, early progenitors will be lost during in vitro expansion. Cell division is a central step of self-renewal and expansion of these cells. There are various growth factors and cytokines known to work as a mitogen, but the ideal growth factors for in vitro MSC expansion must reversibly suppress or at least not alter the subsequent differentiation process. In other words, these factors should not diminish differentiation potentials of MSCs. Growth factors or cytokines which promote differentiation of MSCs into certain lineages cannot be used for in vitro MSC expansion, as the differentiation process itself is antagonizing self-renewal of undifferentiated MSCs including early progenitors and the differentiation would compromise utilization of these cells.
Among those growth factors, we have focused on epidermal growth factor (EGF) as a candidate to utilize in vitro expansion of MSCs as EGF stimulates MSC proliferation without altering differentiation process and potentials [3].
2. EGF to Enhance Self-Renewal and Expansion of MSCs In Vitro
2.1. EGF and EGF Receptor
EGF was originally isolated from mouse salivary gland extract as a factor accelerating the corneal wound healing [40], but it was soon recognized that it is indeed a general growth factor exerting various actions including cell migration and proliferation on a wide variety of cells [41–43].
The EGF receptor (EGFR/ErbB-1 or human epidermal growth factor receptor 1(HER1)) is the prototypal growth factor receptor with intrinsic tyrosine kinase activity. It is widely expressed on many cell types, including epithelial and mesenchymal lineages [42]. Upon binding of at least five genetically distinct ligands (including EGF, transforming growth factor-α (TGF-α), and heparin-binding EGF (HB-EGF)), the intrinsic tyrosine kinase within EGFR/ErbB-1 is activated and phosphorylates the receptor itself (autophosphorylation) and numerous target downstream molecules. Intracellular signaling pathways downstream of EGFR/ErbB-1 include phosholipase Cγ (PLCγ) and its downstream calcium- and protein kinase C (PKC)-mediated cascades, ras activation leading to various mitogen activated protein kinases (MAPK), other small GTPases such as rho and rac, multiple signal transducer and activator of transcription (STAT) isoforms, and heterotrimeric G proteins, phosphatidylinositol 3'-OH kinase (PI3K) and phospholipase D (PLD) [3, 42, 43].
Upon ligand binding and activation, EGFR/ErbB-1 undergoes internalization from the cell surface via the clathrin-coated endocytic system. Within the acidic late endosomal compartment, both EGF and EGF-bound EGFR/ErbB-1 undergo degradation as EGF is a nondissociative ligand for EGF, whereas TGF-α-bound EGFR/ErbB-1 is recycled back to cell surface after dissociation of TGF-α from EGFR /ErbB-1 [42]. There is a growing evidence suggesting that preferential and prolonged activation of EGFR/ErbB-1 from cell surface exerts a distinct activity from internalized EGFR/ErbB-1, as surface-tethered EGF promotes cell spreading and survival of MSCs, whereas soluble EGF does not (See discussion below) [44].
2.2. EGF Enhances MSC Proliferation
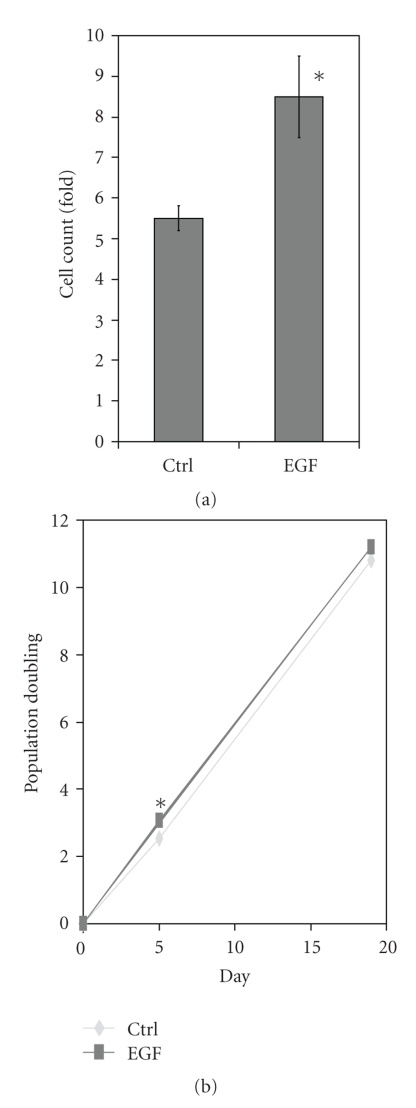
EGF is a prototypal mitogen for various types of cells. Human MSCs express EGFR/ErbB-1, and we and others demonstrated the mitogenic effect of EGF and HB-EGF on MSCs [3, 45]. Cell proliferation is an integral part of self-renewal and expansion of the cells, and thus these data supports our hypothesis that EGF can be used for in vitro MSC expansion, at least in short-term culture setting; however, additive effects of EGF treatment on human MSC proliferation become less clear in the long-term culture (Figure 1), presumably due to down-regulation of EGFR/ErbB1, as discussed below.
Figure 1.
Effect of EGF on primary human MSC proliferation (a) and accumulative population doubling (PD)(b). (a) The cell number of primary human MSCs increases about 5.5-fold in the diluent (Ctrl) in culture medium supplemented with 17% FBS in 120 hours (5 days) time period. The addition of EGF (10 nM) gives an extra increase of cell counts to 8.5-fold. Total of 10000 cells was seeded per each well in 12-well plate and the cell count of each well was measured by Coulter Cell Counter Z2 (Beckman Coulter, Inc. Fullerton, CA). Shown are mean ± s.e.m. of three experiments; each performed in triplicate. The differences in proliferation were compared between growth factor and diluent (Ctrl) exposed (*P < .05). (b) Accumulated PD of primary human MSCs in day 5 and 19 in the culture condition same as (a). After cell counting at day 5, equal number of cells (Total of 1000) was seeded per each well in 6-well plate and the cell count of each well was measured at day 19 by Coulter Cell Counter Z2 (Beckman Coulter, Inc. Fullerton, CA). Note that the PD is higher in EGF treated group (2.54 in Ctrl, 3.07 in EGF) for the initial 5 days (*P < .05), but this difference is reduced in the following 14-day period (10.79 in Ctrl, 11.19 in EGF)(No significant difference). Shown are representative data of three independent experiments; each performed in triplicate.
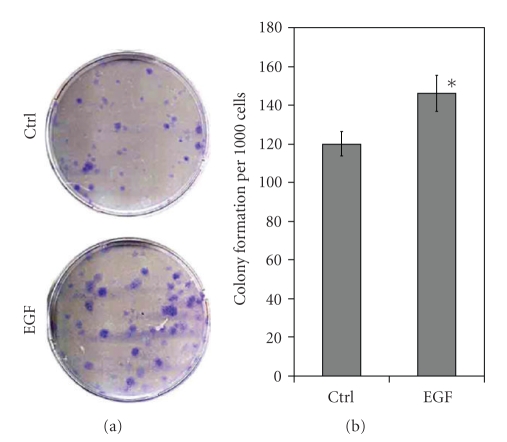
The second aspect of expansion is to maintain colony-forming units. In this aspect, EGF treatment is also successful. EGF leads to a statistically significant 25% increase in stainable colonies (Figure 2), suggesting that EGF treatment helps preserve early progenitors within human MSC populations.
Figure 2.
Effects of EGF treatment (10 nM) on primary human MSC colony formation. Five hundred cells were seeded in 10 cm dish within culture medium supplemented with 17% FBS and the number of formed colonies (Diameter ≥1.5 mm) was counted manually in day 14. (a) Representative image of MSC colonies stained with crystal violet. (b) Colony count of MSC. The number of colony is given per 1000 cells seeded initially (*P < .05 to EGF treatment). Shown are representative data of two independent experiments; each performed in triplicate.
2.3. EGF and MSC Differentiation Potentials
Multidifferentiation potential is a key characteristic of MSCs, which attracts so much attention in the field of tissue engineering and regenerative medicine [4, 5]. Differentiation potential itself has to be preserved through the in vitro expansion of MSCs; however, ongoing differentiation process itself should be suppressed or not induced at least as it antagonizes self-renewal and expansion of undifferentiated MSCs and limits further use of these cells.
Kratchmarova and her colleagues showed that EGF stimulation enhances osteogenic differentiation of human MSCs in the presence of chemical cues, whereas PDGF does not [46]. Through mass spectrometry-based proteomics approach, they identified PI3K as a molecular switch to turn off pro-osteogenic signal from PDGFR.
This report is contradictory to reports by our group and others. Our data show that EGF alone does not induce differentiation in the absence of chemical or other cues, and does not alter human MSC differentiation processes into osteogenic, adipogenic, and chondrogenic lineages by chemical cues in vitro [3]. This discrepant finding might be attributable to a different intracellular signaling, as PI3K-protein kinase B/akt pathway is activated in the downstream of EGFR/ErbB-1 in our report [3], whereas this pathway is not activated in their report [46]. The apparent reason for this discrepancy is unclear, but one prominent difference is EGF concentration; 10 nM EGF was used in our report [3], whereas Kratchmarova and her colleagues used 83 nM of EGF in their report [46]. This speculation is supported by a recent report showing that 80 pM EGF inhibits osteogenic differentiation of human MSCs [47]. Krampera and his colleague also showed that HB-EGF (2.3 nM) inhibits osteogenic differentiation of MSC induced by chemical cues [45]. Human MSCs do not express ErbB-4, another receptor for HB-EGF; both EGF and HB-EGF bind only EGFR/ErbB-1 on MSC, and downstream signaling cascade is similar [3, 45].
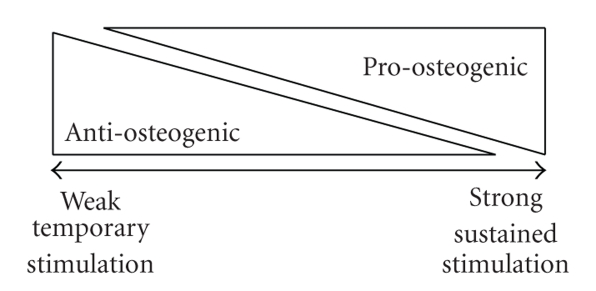
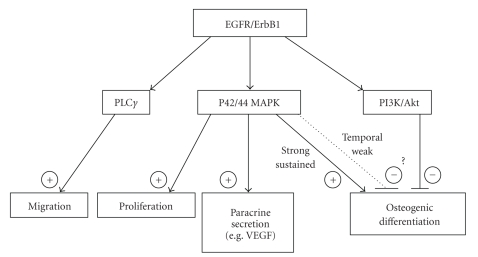
Do EGFR/ErbB1 agonists exert both positive and negative effects on osteogenic differentiation of MSC in a concentration-dependent manner? And if so, what is the underlying mechanism? This question is still unresolved, but we and our collaborators are utilizing immobilized tethered EGF surface in a manner that provides some important hints [44, 47]. Tethered EGF blocks EGFR/ErbB1 endocytic internalization and enhances osteogenic differentiation through providing sustained activation of downstream signaling through EGFR/ErbB1, whereas 80 pM of soluble EGF interferes with osteogenic differentiation through inducing receptor internalization and subsequent degradation [47], in agreement with Krampera's data [45]. Thus, we hypothesize that weak and temporal signaling from low concentration of soluble EGF exerts anti-osteogenic effects, whereas strong sustained signaling from tethered EGF exerts pro-osteogenic signaling on MSC (Figure 3). Previous reports have shown that the activation of ERK/MAPK pathway, one of the major signaling pathways in the downstream of EGFR/ErbB-1 [3, 42], promotes MSC osteogenic differentiation [48–50]. In agreement with these reports, strong and sustained activation of ERK/MAPK pathway has been observed in MSCs cultured on tethered EGF surface [44, 47], and thus, ERK/MAPK pathway might be one of the main pro-osteogenic signaling pathways in the downstream of EGFR/ErbB-1.
Figure 3.
Simplified model for the effects of EGFR/ErbB1 signaling on MSC osteogenic differentiation. Weak and temporal stimulation of EGFR/ErbB1 exerts anti-osteogenic effects, whereas strong and sustained stimulation of EGFR/ErbB1 exerts pro-osteogenic effects on MSC.
Other possible reasons for overall discrepancy about the effects of EGF on MSC differentiation include the heterogeneity of human MSC preparations including primary or immortalized. Kratchmarova and her colleagues used human MSCs immortalized by human telomerase reverse transcriptase (hTERT) [46], whereas Krampera and his colleague used primary human MSCs [45]. We and Griffith's group also used AOC (Adipogenic, Osteogenic, Chondrogenic) clone of human MSCs immortalized by hTERT [3, 47, 51]. As immortalized MSCs were derived from single clone, it is possible that discrepant results between Kratchmarova's group and our group might be due to clone selection bias. Heterogeneity exists even within primary preparation too. The expression levels of EGFR/ErbB-1 are highly variable in each clone of human MSC preparation, up to 77-fold difference among clones [52]. In this report, no significant correlation was observed between the levels EGFR/ErbB-1 and osteogenic differentiation capacity, although the levels of EGFR/ErbB-1 in average were higher in nonbone-forming colonies than bone-forming colonies. Patterns of protein tyrosine phosphorylation downstream of EGFR/ErbB-1 appeared heterogenous among colonies also. Thus, it is likely that heterogeneity does exist not only in EGFR/ErbB-1 expression levels, but also in the downstream signaling pathways from EGFR/ErbB-1 even within the same MSC preparation, which should also contribute to the overall discrepancy about the effects of EGF on MSC differentiation.
As we see above, reports about EGFR agonists and their effects on ongoing MSC differentiation still provide discrepant directives mainly due to different EGF conditions and external stimuli. Still, we need to emphasize that both our report and Krampera report agree that EGF or HB-EGF treatment does not diminish MSC differentiation potentials [3, 45]. There are no reports showing that EGF alone in the absence of osteogenic chemical cues promotes osteogenic differentiation of MSCs. In vitro MSC differentiation into adipogenic and chondrogenic lineages was not altered by soluble EGF [3]. Thus, soluble EGF can still be used to expand MSCs in vitro without inducing differentiation or sacrificing differentiation potentials.
3. EGF Treatment to Enhance Therapeutic Potentials of MSC
3.1. EGF Enhances Motility of MSC
Numerous cellular, hormonal, matrix and enzymatic activities are involved in wound repair and tissue regeneration processes. EGF is one of the pivotal growth factors present in the wound bed, accelerating wound repair along with other growth factors such as PDGF. Topical application of recombinant EGF was shown to accelerate epithelialization of wound healing process including diabetic foot ulcer [53, 54].
EGF is secreted from platelets and macrophages in wounded tissues [55]. HB-EGF is abundant in ECM [56]. Both EGF and HB-EGF stimulate proliferation and migration of fibroblasts and keratinocytes. Similarly, MSCs transplanted in the wounded tissues need to proliferate and repopulate themselves to promote wound healing and tissue regeneration processes in the MSC-based therapeutics. We and others showed that both EGF and HB-EGF elicit mitogenic and motogenic response of MSCs in vitro [3, 45, 52]. Thus, it is speculated that EGF-induced mitogenic and motogenic responses of MSCs play a role in regulating proliferation and repopulation of MSCs in the wounded tissues.
EGFR/ErbB1 ligands exist not only in soluble form, but also within multiple EGF-like repeats of extracellular matrix molecules such as tenascin and laminin in vivo [57]. We have previously shown that these EGF-like repeats within tenascin C bind to EGFR/ErbB1 and produce intracellular signaling promoting cell motility and adhesion, similar to tethered EGF [58, 59]. Tenacin C is produced by keratinocytes and fibroblasts during wound healing process, and thus it might serve as endogenous tethered EGF-like ligands and produce promigratory tracks for fibroblasts or implanted MSCs within the wound healing edges [57, 60].
Although motility enables MSC to reposition themselves in wounded tissues, it might make precise control of in vivo cell distribution difficult. One possible approach is to create concentration gradients or patterns of tethered EGF within MSC-embedded scaffolds. Motogenic activity of EGF is preserved in the tethered form, as human keratinocytes on tethered EGF gradients were reported to migrate in the direction of higher tethered EGF concentration [61]. Tethered form of EGF allows more precise control of EGF concentration and patterning within tissue microenvironments and one that lasts over a longer duration. This connecting of motogenic ligand to the space-forming matrix should be a strong tool in the field of tissue engineering.
3.2. EGF Enhances Paracrine Activities of MSC
MSC-based therapeutics heavily relies on the strong capability to secrete various growth factors and cytokines to promote angiogenesis, wound repair, and tissue regeneration [7, 21–25]. MSCs are required to be transplanted into the wounded tissues, which fail to heal otherwise. In vivo microenvironments of these nonhealing wounds are characterized by lack of oxygen and nutrients due to compromised blood flow and by exuberant proinflammatory mediators [62–64]. MSCs are needed to produce bioactive molecules even in those harsh environments to exert tissue regenerative effects. Indeed, the proinflammatory mediator tumor necrosis factor-alpha (TNF-α) or lipopolysacharide (LPS) was shown to enhance paracrine and autocrine functions of MSCs [65]. Also, TGF-α, another EGFR/ErbB1 ligand, was shown to further increase VEGF secretion from MSCs already up-regulated by TNF-α stimulation in a p42/44 MAPK dependent manner [66, 67].
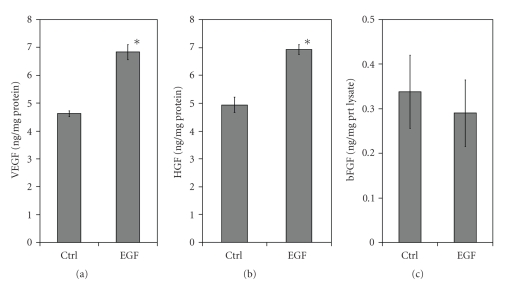
Our in vitro data showed that EGF treatment of MSCs further promotes secretion of VEGF and HGF, but not bFGF (Figure 4), in agreement with a previous study [65]. Both VEGF and HGF play a pivotal role in MSC-mediated accelerated wound healing through inducing angiogenesis and improving oxygen supplies to the ischemic tissues [7, 21, 68–70].
Figure 4.
Effects of EGF treatment (10 nM) on paracrine activities of human primary MSCs. MSCs were cultured in serum-free culture medium with and without EGF (10 nM) for 24 hours. Concentrations of VEGF (a), HGF (b), and bFGF (c) within conditioned media were measured by ELISA and standardized to the total amount of cellular protein contents (*P < .05 to EGF treatment). Shown are average data of three independent experiments; each performed in triplicate.
Thus, it is likely that soluble EGFR/ErbB1 ligands (TGF-α, EGF and HB-EGF) enhance paracrine and autocrine functions of MSCs not only in vitro, but also in vivo, even in the inflammatory microenvironments within nonhealing wounded tissues. It is also likely that tethered EGF enhances paracrine and autocrine functions of MSCs in vitro as well as in vivo through strong and sustained activation of p42/44 MAPK pathway in the downstream of EGFR/ErbB1 [44]. Both soluble and tethered EGFR/ErbB1 ligands are speculated to promote wound healing and tissue regeneration process through stimulating the secretion of angiogenic growth factors from transplanted MSCs in vivo. Further studies are warranted to elucidate the role of soluble EGFR/ErbB1 ligands and tethered EGF on the paracrine and autocrine effects of MSCs in vitro as well as in vivo.
3.3. Does EGF Enhance Therapeutic Potentials of MSC?
EGF stimulates cell proliferation and enhances self-renewal of MSCs, especially undifferentiated early progenitors within the MSC preparations in vitro. The presence of early progenitors is critical for MSC-based therapeutics, as MSCs from old donors and high passaged MSCs have decreased paracrine activity and reduced organ protective effects upon transplantation, presumably through loss of early progenitors [27, 29, 30, 36, 39]. EGF treatment also enhances cell motility, which is required for repopulation of MSCs within the wound bed. EGF treatment further increases paracrine secretion of VEGF and HGF, both of which enhance angiogenesis and promote wound healing and tissue regeneration also being stimulatory for the adherent cells resident within the wound bed. Taken together, it is reasonable to hypothesize that in vitro MSC treatment with EGFR/ErbB1 ligands enhances therapeutic potentials of MSCs. This could be tested by in vivo study.
It is also reasonable to hypothesize that EGFR/ErbB1 stimulation on MSC enhances therapeutic potentials of MSCs in vivo, presumably through augmenting paracrine activity and exerting both mitogenic and motogenic activities of MSCs. Biodegradable scaffolds are a promising approach to support cell delivery, guide proliferation and differentiation of the cells [71]. Drug delivery scaffolds or growth factor release scaffolds are also available, which enables the controlled release of growth factor [72]. Availability of EGF is less predictable in vivo setting; however, EGF slow releasing scaffolds allow for better prediction of EGF concentration within microenvironments in vivo, thus, in vitro findings should be better translated to the in vivo settings and the role of EGF in MSC-based therapeutics could be better evaluated.
In addition to soluble EGFR/ErbB1 ligands, tethered EGF might bestow even stronger therapeutic potential on MSCs. First, tethered EGF exerts proliferative and cytoprotective effects on MSCs [44, 73]. Therapeutic effects of MSC largely depend on the number of injected MSC [19]; however, low viability of postimplant MSCs limits the overall effectiveness of MSC-based therapeutics due to harsh microenvironments [15, 74]. Thus, improvement of postimplant MSC survival should increase the efficacy of MSC-based therapeutics. Second, tethered EGF provides pro-osteogenic cues for MSCs, thus it could be utilized in both in vitro and in vivo osteogenic differentiation of MSCs. This mechanism might play a significant role in vivo, as laminin 5, which contains EGF-like repeats, was shown to stimulate osteogenic differentiation of human MSCs through activation of ERK within bone tissue [75]. Thus, MSC-embedded scaffold with tethered EGF could be potentially applicable to current human studies such as osteogenic imperfecta [76–78].
The challenge of translating theoretical findings to bedsides always resides in moving from in vitro to in vivo studies and then into people. While we cannot foresee all the obstacles, the main challenge in this translation involves the inflammatory situation and immunological issues. In the case of the latter, this is moot if the MSCs are autologous, but allogenic MSCs are also useful, especially for aged patients, as MSC harvest and subsequent ex vivo expansion might be limited for those populations [26, 39]. The immunosuppressive nature of MSC makes allogenic transplantation feasible [26]. Nonspecific inflammation due to any foreign body is something not avoidable. Actually we propose that the tethered EGF confer resistance to death signals on MSCs [44]. Still the complex mixture of inflammatory cytokines and chemokines may alter the response to EGFR/ErbB1 ligands in unpredictable ways. Lastly, if the inflammatory response runs towards fibrosis, MSCs risk being walled-off from the site of injury. Another potential challenge of the translation into people is underlying disease conditions, as nutrient delivery, oxygen supplies, and removal of toxic metabolites are often severely compromised in these populations [62–64]; in diabetes the hyperglycemia also impacts EGFR signaling pathways [79, 80]. These harsh microenvironments, with alter extracellular pH, will impinge on the MSC behavior in an unpredictable manner. That is why we are quickly moving to test these models in increasingly challenged animal models.
4. Epilogue
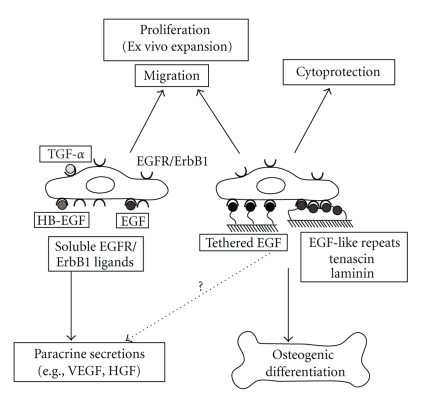
Previous studies suggest that EGF facilitates expansion of colony forming early progenitors in MSC population without inducing differentiation or compromising differentiation potentials. EGF treatment also promotes paracrine activity of MSC, at least the production of VEGF and HGF, both of which are pivotal for wound healing and tissue regeneration. EGF can be utilized to promote expansion and paracrine activities of MSCs in vitro, at least with short-term treatment with EGF. For in vivo settings, EGF can be incorporated in growth factor-releasing scaffolds encapsulating MSCs to augment MSC proliferation and paracrine action. Tethered form of EGF can also be incorporated in the scaffold to control osteogenic differentiation of MSCs or MSC distributions in vivo. The roles of EGFR/ErbB1 ligands and downstream signaling from EGFR/ErbB1 on MSC physiology are summarized in Figures 5 and 6. Overall, it should be reasonable to utilize EGF for MSC expansion in vitro, enhancement of MSC therapeutic potentials in vivo, and regulation of MSC differentiation both in vitro and in vivo.
Figure 5.
Simplified diagram of EGFR/ErbB1 signaling pathways in MSC physiology. EGFR/ErbB1 ligands activate PLCγ pathway, p42/44 MAPK pathway, and PI3K/Akt pathways in MSCs [3]. PLCγ pathway plays a pivotal role in motogenic activity, whereas p42/44 MAPK pathway plays a key role in mitogenic activity and paracrine activities of certain factors such as VEGF [42, 43, 66, 67]. Sustained and strong activation of p42/44 MAPK pathway exerts cytoprotective and pro-osteogenic effects [44, 47], whereas PI3K/Akt pathway might exert anti-osteogenic effects [46].
Figure 6.
The roles of soluble and tethered EGFR/ErbB1 ligands on MSC physiology. Soluble EGFR/ErbB1 ligands (EGF, HB-EGF, TGF-α) enhance paracrine secretions, proliferation, and migration of MSCs. Tethered EGF or EGF-like repeats within tenascin or laminin augment osteogenic differentiation of MSCs, in addition to cytoprotective, motogenic, and mitogenic effects on MSCs.
Acknowledgments
Preparation of this article was supported by Grants from AHA Beginner-Grant-in-aid (09BGIA2050227) and start-up fund from Department of Pathology, OSU (K.T.) and from NIH (R01GM063569 and R01GM069668) (A.W.). We would like to thank Dr. J. Van Brooklyn (OSU, Columbus, OH) for his generous instrumental support.
References
- 1.Barry FP, Murphy JM. Mesenchymal stem cells: clinical applications and biological characterization. International Journal of Biochemistry and Cell Biology. 2004;36(4):568–584. doi: 10.1016/j.biocel.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Phinney DG, Prockop DJ. Concise review: mesenchymal stem/multipotent stromal cells: the state of transdifferentiation and modes of tissue repair—current views. Stem Cells. 2007;25(11):2896–2902. doi: 10.1634/stemcells.2007-0637. [DOI] [PubMed] [Google Scholar]
- 3.Tamama K, Fan VH, Griffith LG, Blair HC, Wells A. Epidermal growth factor as a candidate for ex vivo expansion of bone marrow-derived mesenchymal stem cells. Stem Cells. 2006;24(3):686–695. doi: 10.1634/stemcells.2005-0176. [DOI] [PubMed] [Google Scholar]
- 4.Prockop DJ. Marrow stromal cells as stem cells for nonhematopoietic tissues. Science. 1997;276(5309):71–74. doi: 10.1126/science.276.5309.71. [DOI] [PubMed] [Google Scholar]
- 5.Pittenger MF, Mackay AM, Beck SC, et al. Multilineage potential of adult human mesenchymal stem cells. Science. 1999;284(5411):143–147. doi: 10.1126/science.284.5411.143. [DOI] [PubMed] [Google Scholar]
- 6.Owen M, Friedenstein AJ. Stromal stem cells: marrow-derived osteogenic precursors. Ciba Foundation Symposium. 1988;136:42–60. doi: 10.1002/9780470513637.ch4. [DOI] [PubMed] [Google Scholar]
- 7.Kinnaird T, Stabile E, Burnett MS, Epstein SE. Bone marrow-derived cells for enhancing collateral development: mechanisms, animal data, and initial clinical experiences. Circulation Research. 2004;95(4):354–363. doi: 10.1161/01.RES.0000137878.26174.66. [DOI] [PubMed] [Google Scholar]
- 8.Friedenstein AJ, Gorskaja JF, Kulagina NN. Fibroblast precursors in normal and irradiated mouse hematopoietic organs. Experimental Hematology. 1976;4(5):267–274. [PubMed] [Google Scholar]
- 9.Oswald J, Boxberger S, Jørgensen B, et al. Mesenchymal stem cells can be differentiated into endothelial cells in vitro. Stem Cells. 2004;22(3):377–384. doi: 10.1634/stemcells.22-3-377. [DOI] [PubMed] [Google Scholar]
- 10.Tamama K, Sen CK, Wells A. Differentiation of bone marrow mesenchymal stem cells into the smooth muscle lineage by blocking ERK/MAPK signaling pathway. Stem Cells and Development. 2008;17(5):897–908. doi: 10.1089/scd.2007.0155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pittenger MF, Martin BJ. Mesenchymal stem cells and their potential as cardiac therapeutics. Circulation Research. 2004;95(1):9–20. doi: 10.1161/01.RES.0000135902.99383.6f. [DOI] [PubMed] [Google Scholar]
- 12.Davani S, Marandin A, Mersin N, et al. Mesenchymal progenitor cells differentiate into an endothelial phenotype, enhance vascular density, and improve heart function in a rat cellular cardiomyoplasty model. Circulation. 2003;108(10, supplement):II253–II258. doi: 10.1161/01.cir.0000089186.09692.fa. [DOI] [PubMed] [Google Scholar]
- 13.Amado LC, Saliaris AP, Schuleri KH, et al. Cardiac repair with intramyocardial injection of allogeneic mesenchymal stem cells after myocardial infarction. Proceedings of the National Academy of Sciences of the United States of America. 2005;102(32):11474–11479. doi: 10.1073/pnas.0504388102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dai W, Hale SL, Martin BJ, et al. Allogeneic mesenchymal stem cell transplantation in postinfarcted rat myocardium: short- and long-term effects. Circulation. 2005;112(2):214–223. doi: 10.1161/CIRCULATIONAHA.104.527937. [DOI] [PubMed] [Google Scholar]
- 15.Toma C, Pittenger MF, Cahill KS, Byrne BJ, Kessler PD. Human mesenchymal stem cells differentiate to a cardiomyocyte phenotype in the adult murine heart. Circulation. 2002;105(1):93–98. doi: 10.1161/hc0102.101442. [DOI] [PubMed] [Google Scholar]
- 16.Ziegelhoeffer T, Fernandez B, Kostin S, et al. Bone marrow-derived cells do not incorporate into the adult growing vasculature. Circulation Research. 2004;94(2):230–238. doi: 10.1161/01.RES.0000110419.50982.1C. [DOI] [PubMed] [Google Scholar]
- 17.Wu Y, Chen L, Scott PG, Tredget EE. Mesenchymal stem cells enhance wound healing through differentiation and angiogenesis. Stem Cells. 2007;25(10):2648–2659. doi: 10.1634/stemcells.2007-0226. [DOI] [PubMed] [Google Scholar]
- 18.Sasaki M, Abe R, Fujita Y, Ando S, Inokuma D, Shimizu H. Mesenchymal stem cells are recruited into wounded skin and contribute to wound repair by transdifferentiation into multiple skin cell type. Journal of Immunology. 2008;180(4):2581–2587. doi: 10.4049/jimmunol.180.4.2581. [DOI] [PubMed] [Google Scholar]
- 19.Falanga V, Iwamoto S, Chartier M, et al. Autologous bone marrow-derived cultured mesenchymal stem cells delivered in a fibrin spray accelerate healing in murine and human cutaneous wounds. Tissue Engineering. 2007;13(6):1299–1312. doi: 10.1089/ten.2006.0278. [DOI] [PubMed] [Google Scholar]
- 20.Javazon EH, Keswani SG, Badillo AT, et al. Enhanced epithelial gap closure and increased angiogenesis in wounds of diabetic mice treated with adult murine bone marrow stromal progenitor cells. Wound Repair and Regeneration. 2007;15(3):350–359. doi: 10.1111/j.1524-475X.2007.00237.x. [DOI] [PubMed] [Google Scholar]
- 21.Kinnaird T, Stabile E, Burnett MS, et al. Local delivery of marrow-derived stromal cells augments collateral perfusion through paracrine mechanisms. Circulation. 2004;109(12):1543–1549. doi: 10.1161/01.CIR.0000124062.31102.57. [DOI] [PubMed] [Google Scholar]
- 22.Kilroy GE, Foster SJ, Wu X, et al. Cytokine profile of human adipose-derived stem cells: expression of angiogenic, hematopoietic, and pro-inflammatory factors. Journal of Cellular Physiology. 2007;212(3):702–709. doi: 10.1002/jcp.21068. [DOI] [PubMed] [Google Scholar]
- 23.Chen L, Tredget EE, Wu PYG, Wu Y, Wu Y. Paracrine factors of mesenchymal stem cells recruit macrophages and endothelial lineage cells and enhance wound healing. PLoS ONE. 2008;3(4, article e1886) doi: 10.1371/journal.pone.0001886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schinkothe T, Bloch W, Schmidt A. In vitro secreting profile of human mesenchymal stem cells. Stem Cells and Development. 2008;17(1):199–205. doi: 10.1089/scd.2007.0175. [DOI] [PubMed] [Google Scholar]
- 25.Gnecchi M, He H, Noiseux N, et al. Evidence supporting paracrine hypothesis for Akt-modified mesenchymal stem cell-mediated cardiac protection and functional improvement. FASEB Journal. 2006;20(6):661–669. doi: 10.1096/fj.05-5211com. [DOI] [PubMed] [Google Scholar]
- 26.Caplan AI. Why are MSCs therapeutic? New data: new insight. Journal of Pathology. 2009;217(2):318–324. doi: 10.1002/path.2469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sekiya I, Larson BL, Smith JR, Pochampally R, Cui J-G, Prockop DJ. Expansion of human adult stem cells from bone marrow stroma: conditions that maximize the yields of early progenitors and evaluate their quality. Stem Cells. 2002;20(6):530–541. doi: 10.1634/stemcells.20-6-530. [DOI] [PubMed] [Google Scholar]
- 28.Stute N, Holtz K, Bubenheim M, Lange C, Blake F, Zander AR. Autologous serum for isolation and expansion of human mesenchymal stem cells for clinical use. Experimental Hematology. 2004;32(12):1212–1225. doi: 10.1016/j.exphem.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 29.Colter DC, Class R, DiGirolamo CM, Prockop DJ. Rapid expansion of recycling stem cells in cultures of plastic-adherent cells from human bone marrow. Proceedings of the National Academy of Sciences of the United States of America. 2000;97(7):3213–3218. doi: 10.1073/pnas.070034097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Crisostomo PR, Wang M, Wairiuko GM, et al. High passage number of stem cells adversely affects stem cell activation and myocardial protection. Shock. 2006;26(6):575–580. doi: 10.1097/01.shk.0000235087.45798.93. [DOI] [PubMed] [Google Scholar]
- 31.Sotiropoulou PA, Perez SA, Salagianni M, Baxevanis CN, Papamichail M. Cell culture medium composition and translational adult bone marrow-derived stem cell research. Stem Cells. 2006;24(5):1409–1410. doi: 10.1634/stemcells.2005-0654. [DOI] [PubMed] [Google Scholar]
- 32.Ng F, Boucher S, Koh S, et al. PDGF, TGF-β, and FGF signaling is important for differentiation and growth of mesenchymal stem cells (MSCs): transcriptional profiling can identify markers and signaling pathways important in differentiation of MSCs into adipogenic, chondrogenic, and osteogenic lineages. Blood. 2008;112(2):295–307. doi: 10.1182/blood-2007-07-103697. [DOI] [PubMed] [Google Scholar]
- 33.Agata H, Watanabe N, Ishii Y, et al. Feasibility and efficacy of bone tissue engineering using human bone marrow stromal cells cultivated in serum-free conditions. Biochemical and Biophysical Research Communications. 2009;382(2):353–358. doi: 10.1016/j.bbrc.2009.03.023. [DOI] [PubMed] [Google Scholar]
- 34.Javazon EH, Beggs KJ, Flake AW. Mesenchymal stem cells: paradoxes of passaging. Experimental Hematology. 2004;32(5):414–425. doi: 10.1016/j.exphem.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 35.Horwitz EM, Le Blanc K, Dominici M, et al. Clarification of the nomenclature for MSC: the International Society for Cellular Therapy position statement. Cytotherapy. 2005;7(5):393–395. doi: 10.1080/14653240500319234. [DOI] [PubMed] [Google Scholar]
- 36.Colter DC, Sekiya I, Prockop DJ. Identification of a subpopulation of rapidly self-renewing and multipotential adult stem cells in colonies of human marrow stromal cells. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(14):7841–7845. doi: 10.1073/pnas.141221698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Smith JR, Pochampally R, Perry A, Hsu S-C, Prockop DJ. Isolation of a highly clonogenic and multipotential subfraction of adult stem cells from bone marrow stroma. Stem Cells. 2004;22(5):823–831. doi: 10.1634/stemcells.22-5-823. [DOI] [PubMed] [Google Scholar]
- 38.Pochampally R. Colony forming unit assays for MSCs. Methods in Molecular Biology. 2008;449:83–91. doi: 10.1007/978-1-60327-169-1_6. [DOI] [PubMed] [Google Scholar]
- 39.Jiang S, Haider HKh, Ahmed RPH, Idris NM, Salim A, Ashraf M. Transcriptional profiling of young and old mesenchymal stem cells in response to oxygen deprivation and reparability of the infarcted myocardium. Journal of Molecular and Cellular Cardiology. 2008;44(3):582–596. doi: 10.1016/j.yjmcc.2007.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cohen S, Elliott GA. The stimulation of epidermal keratinization by a protein isolated from the submaxillary gland of the mouse. Journal of Investigative Dermatology. 1963;40:1–5. doi: 10.1038/jid.1963.1. [DOI] [PubMed] [Google Scholar]
- 41.Carpenter G, Cohen S. Epidermal growth factor. Journal of Biological Chemistry. 1990;265(14):7709–7712. [PubMed] [Google Scholar]
- 42.Wells A. EGF receptor. International Journal of Biochemistry and Cell Biology. 1999;31(6):637–643. doi: 10.1016/s1357-2725(99)00015-1. [DOI] [PubMed] [Google Scholar]
- 43.Wells A, Ware MF, Allen FD, Lauffenburger DA. Shaping up for shipping out: PLCγ signaling of morphology changes in EGF-stimulated fibroblast migration. Cell Motility and the Cytoskeleton. 1999;44(4):227–233. doi: 10.1002/(SICI)1097-0169(199912)44:4<227::AID-CM1>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 44.Fan VH, Tamama K, Au A, et al. Tethered epidermal growth factor provides a survival advantage to mesenchymal stem cells. Stem Cells. 2007;25(5):1241–1251. doi: 10.1634/stemcells.2006-0320. [DOI] [PubMed] [Google Scholar]
- 45.Krampera M, Pasini A, Rigo A, et al. HB-EGF/HER-1 signaling in bone marrow mesenchymal stem cells: inducing cell expansion and reversibly preventing multilineage differentiation. Blood. 2005;106(1):59–66. doi: 10.1182/blood-2004-09-3645. [DOI] [PubMed] [Google Scholar]
- 46.Kratchmarova I, Blagoev B, Haack-Sorensen M, Kassem M, Mann M. Mechanism of divergent growth factor effects in mesenchymal stem cell differentiation. Science. 2005;308(5727):1472–1477. doi: 10.1126/science.1107627. [DOI] [PubMed] [Google Scholar]
- 47.Platt MO, Roman AJ, Wells A, Lauffenburger DA, Griffith LG. Sustained epidermal growth factor receptor levels and activation by tethered ligand binding enhances osteogenic differentiation of multi-potent marrow stromal cells. Journal of Cellular Physiology. 2009;221(2):306–317. doi: 10.1002/jcp.21854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jaiswal RK, Jaiswal N, Bruder SP, Mbalaviele G, Marshak DR, Pittenger MF. Adult human mesenchymal stem cell differentiation to the osteogenic or adipogenic lineage is regulated by mitogen-activated protein kinase. Journal of Biological Chemistry. 2000;275(13):9645–9652. doi: 10.1074/jbc.275.13.9645. [DOI] [PubMed] [Google Scholar]
- 49.Salasznyk RM, Klees RF, Hughlock MK, Plopper GE. ERK signaling pathways regulate the osteogenic differentiation of human mesenchymal stem cells on collagen I and vitronectin. Cell Communication and Adhesion. 2004;11(5-6):137–153. doi: 10.1080/15419060500242836. [DOI] [PubMed] [Google Scholar]
- 50.Ward DF, Jr., Salasznyk RM, Klees RF, et al. Mechanical strain enhances extracellular matrix-induced gene focusing and promotes osteogenic differentiation of human mesenchymal stem cells through an extracellular-related kinase-dependent pathway. Stem Cells and Development. 2007;16(3):467–479. doi: 10.1089/scd.2007.0034. [DOI] [PubMed] [Google Scholar]
- 51.Okamoto T, Aoyama T, Nakayama T, et al. Clonal heterogeneity in differentiation potential of immortalized human mesenchymal stem cells. Biochemical and Biophysical Research Communications. 2002;295(2):354–361. doi: 10.1016/s0006-291x(02)00661-7. [DOI] [PubMed] [Google Scholar]
- 52.Satomura K, Derubeis AR, Fedarko NS, et al. Receptor tyrosine kinase expression in human bone marrow stromal cells. Journal of Cellular Physiology. 1998;177(3):426–438. doi: 10.1002/(SICI)1097-4652(199812)177:3<426::AID-JCP6>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 53.Brown GL, Nanney LB, Griffen J, et al. Enhancement of wound healing by topical treatment with epidermal growth factor. The New England Journal of Medicine. 1989;321(2):76–79. doi: 10.1056/NEJM198907133210203. [DOI] [PubMed] [Google Scholar]
- 54.Hong JP, Jung HD, Kim YW. Recombinant human epidermal growth factor (EGF) to enhance healing for diabetic foot ulcers. Annals of Plastic Surgery. 2006;56(4):394–398. doi: 10.1097/01.sap.0000198731.12407.0c. [DOI] [PubMed] [Google Scholar]
- 55.Schultz G, Rotatori DS, Clark W. EGF and TGF-α in wound healing and repair. Journal of Cellular Biochemistry. 1991;45(4):346–352. doi: 10.1002/jcb.240450407. [DOI] [PubMed] [Google Scholar]
- 56.Marikovsky M, Breuing K, Liu PY, et al. Appearance of heparin-binding EGF-like growth factor in wound fluid as a response to injury. Proceedings of the National Academy of Sciences of the United States of America. 1993;90(9):3889–3893. doi: 10.1073/pnas.90.9.3889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tran KT, Griffith L, Wells A. Extracellular matrix signaling through growth factor receptors during wound healing. Wound Repair and Regeneration. 2004;12(3):262–268. doi: 10.1111/j.1067-1927.2004.012302.x. [DOI] [PubMed] [Google Scholar]
- 58.Iyer AKV, Tran KT, Griffith L, Wells A. Cell surface restriction of EGFR by a tenascin cytotactin-encoded EGF-like repeat is preferential for motility-related signaling. Journal of Cellular Physiology. 2008;214(2):504–512. doi: 10.1002/jcp.21232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Swindle CS, Tran KT, Johnson TD, et al. Epidermal growth factor (EGF)-like repeats of human tenascin-C as ligands for EGF receptor. Journal of Cell Biology. 2001;154(2):459–468. doi: 10.1083/jcb.200103103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mackie EJ, Halfter W, Liverani D. Induction of tenascin in healing wounds. Journal of Cell Biology. 1988;107(6, part 2):2757–2767. doi: 10.1083/jcb.107.6.2757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stefonek TJ, Masters KS. Immobilized gradients of epidermal growth factor promote accelerated and directed keratinocyte migration. Wound Repair and Regeneration. 2007;15(6):847–855. doi: 10.1111/j.1524-475X.2007.00288.x. [DOI] [PubMed] [Google Scholar]
- 62.Gurtner GC, Werner S, Barrandon Y, Longaker MT. Wound repair and regeneration. Nature. 2008;453(7193):314–321. doi: 10.1038/nature07039. [DOI] [PubMed] [Google Scholar]
- 63.Henry G, Garner WL. Inflammatory mediators in wound healing. Surgical Clinics of North America. 2003;83(3):483–507. doi: 10.1016/S0039-6109(02)00200-1. [DOI] [PubMed] [Google Scholar]
- 64.Sen CK. Wound healing essentials: let there be oxygen. Wound Repair and Regeneration. 2009;17(1):1–18. doi: 10.1111/j.1524-475X.2008.00436.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Crisostomo PR, Wang Y, Markel TA, Wang M, Lahm T, Meldrum DR. Human mesenchymal stem cells stimulated by TNF-α, LPS, or hypoxia produce growth factors by an NFκB- but not JNK-dependent mechanism. American Journal of Physiology. 2008;294(3):C675–C682. doi: 10.1152/ajpcell.00437.2007. [DOI] [PubMed] [Google Scholar]
- 66.Wang Y, Crisostomo PR, Wang M, Markel TA, Novotny NM, Meldrum DR. TGF-α increases human mesenchymal stem cell-secreted VEGF by MEK- and PI3-K- but not JNK- or ERK-dependent mechanisms. American Journal of Physiology. 2008;295(4):R1115–R1123. doi: 10.1152/ajpregu.90383.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang Y, Wang M, Abarbanell AM, et al. MEK mediates the novel cross talk between TNFR2 and TGF-EGFR in enhancing vascular endothelial growth factor (VEGF) secretion from human mesenchymal stem cells. Surgery. 2009;146(2):198–205. doi: 10.1016/j.surg.2009.04.013. [DOI] [PubMed] [Google Scholar]
- 68.Duan H-F, Wu C-T, Wu D-L, et al. Treatment of myocardial ischemia with bone marrow-derived mesenchymal stem cells overexpressing hepatocyte growth factor. Molecular Therapy. 2003;8(3):467–474. doi: 10.1016/s1525-0016(03)00186-2. [DOI] [PubMed] [Google Scholar]
- 69.Kinnaird T, Stabile E, Burnett MS, et al. Marrow-derived stromal cells express genes encoding a broad spectrum of arteriogenic cytokines and promote in vitro and in vivo arteriogenesis through paracrine mechanisms. Circulation Research. 2004;94(5):678–685. doi: 10.1161/01.RES.0000118601.37875.AC. [DOI] [PubMed] [Google Scholar]
- 70.Rosová I, Dao M, Capoccia B, Link D, Nolta JA. Hypoxic preconditioning results in increased motility and improved therapeutic potential of human mesenchymal stem cells. Stem Cells. 2008;26(8):2173–2182. doi: 10.1634/stemcells.2007-1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Guan J, Fujimoto KL, Sacks MS, Wagner WR. Preparation and characterization of highly porous, biodegradable polyurethane scaffolds for soft tissue applications. Biomaterials. 2005;26(18):3961–3971. doi: 10.1016/j.biomaterials.2004.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Guan J, Stankus JJ, Wagner WR. Biodegradable elastomeric scaffolds with basic fibroblast growth factor release. Journal of Controlled Release. 2007;120(1-2):70–78. doi: 10.1016/j.jconrel.2007.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Platt MO, Wilder CL, Wells A, Griffith LG, Lauffenburger DA. Multipathway kinase signatures of multipotent stromal cells are predictive for osteogenic differentiation: tissue-specific stem cells. Stem Cells. 2009;27(11):2804–2814. doi: 10.1002/stem.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mangi AA, Noiseux N, Kong D, et al. Mesenchymal stem cells modified with Akt prevent remodeling and restore performance of infarcted hearts. Nature Medicine. 2003;9(9):1195–1201. doi: 10.1038/nm912. [DOI] [PubMed] [Google Scholar]
- 75.Klees RF, Salasznyk RM, Kingsley K, Williams WA, Boskey A, Plopper GE. Laminin-5 induces osteogenic gene expression in human mesenchymal stem cells through an ERK-dependent pathway. Molecular Biology of the Cell. 2005;16(2):881–890. doi: 10.1091/mbc.E04-08-0695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Horwitz EM, Gordon PL, Koo WKK, et al. Isolated allogeneic bone marrow-derived mesenchymal cells engraft and stimulate growth in children with osteogenesis imperfecta: implications for cell therapy of bone. Proceedings of the National Academy of Sciences of the United States of America. 2002;99(13):8932–8937. doi: 10.1073/pnas.132252399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Horwitz EM, Prockop DJ, Fitzpatrick LA, et al. Transplantability and therapeutic effects of bone marrow-derived mesenchymal cells in children with osteogenesis imperfecta. Nature Medicine. 1999;5(3):309–313. doi: 10.1038/6529. [DOI] [PubMed] [Google Scholar]
- 78.Horwitz EM, Prockop DJ, Gordon PL, et al. Clinical responses to bone marrow transplantation in children with severe osteogenesis imperfecta. Blood. 2001;97(5):1227–1231. doi: 10.1182/blood.v97.5.1227. [DOI] [PubMed] [Google Scholar]
- 79.Portero-Otin M, Pamplona R, Bellmunt MJ, et al. Advanced glycation end product precursors impair epidermal growth factor receptor signaling. Diabetes. 2002;51(5):1535–1542. doi: 10.2337/diabetes.51.5.1535. [DOI] [PubMed] [Google Scholar]
- 80.Prada PO, Ropelle ER, Mourao RH, et al. An EGFR tyrosine-kinase inhibitor (PD153035) improves glucose tolerance and insulin action in high-fat diet-fed mice. Diabetes. 2009;58(12):2910–2919. doi: 10.2337/db08-0506. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]