Abstract
Objective
The unique needs of sero-discordant couples are largely missing from many current family planning efforts, which focus on the prevention of pregnancies in absence of the reduction of the risk of human immunodeficiency virus (HIV) and other sexually transmitted infections (STIs). Conversely, HIV testing and programs focus exclusively on condom use without discussion of more effective contraceptive methods. In order to provide information to inform the development of family planning services tailored to the unique needs of sero-discordant couples, this study examined the contraceptive knowledge, use, and concerns among sero-discordant couples in urban Rwanda and Zambia.
Methods
This article presents a comparison of family planning knowledge, use, and concerns about contraception among two cohorts of HIV sero-discordant study participants in Rwanda and Zambia.
Results
The results reveal an interesting profile of contraceptive knowledge and use among sero-discordant couples; in both settings, despite high levels of knowledge of contraception, use of contraceptive methods remains relatively low. There is a clear gender difference in both the reporting of knowledge and use of contraceptive methods, and there is evidence of clandestine contraceptive use by women.
Conclusions
Including information on family planning in voluntary counseling and testing (VCT) services in addition to tailoring the delivery of family planning information to meet to needs and concerns of HIV-positive women or those with HIV positive partners is an essential step in the delivery of services and prevention efforts to reduce the transmission of HIV. Family planning and HIV prevention programs should integrate counseling on “dual method use,” combining condoms for HIV/STI prevention with a long-acting contraceptive for added protection against unplanned pregnancy.
Introduction
Despite recent progress in some countries, sub-Saharan Africa continues to experience the most severe effects of the human immunodeficiency virus (HIV)/acquired immune deficiency syndrome (AIDS) pandemic.1 In 2005, there were more adults and children living with HIV, more new HIV infections, and more AIDS-related deaths in sub-Saharan Africa than in any other region of the world.1 Of the estimated 2.3 million children living with HIV worldwide at the end of 2005, 2 million (nearly 90%) were living in sub-Saharan Africa, along with more than 12 million orphans on the continent.1 These high levels of HIV prevalence exist in countries that also often have high levels of fertility and low contraceptive use. Sub-Saharan Africa has the lowest rate of contraceptive use in the world, due to a nexus of issues including difficulty in accessing contraceptive supplies, insufficient health care infrastructure, a large rural population, poor economic development and cultural values placed on fertility.2,3 As a result, two issues regarding children and the HIV/AIDS epidemic remain: firstly, the potential for maternal transmission of HIV from mother to child during pregnancy or labor, which leads to an increase in pediatric AIDS cases, and secondly, the growing numbers of children who are orphaned when their parents die from AIDS. Comprehensive HIV/AIDS prevention programs must also address the prevention of unplanned pregnancies among couples living with HIV, while also providing couples with services and support to manage their fertility desires.
There is a lack of systematic research on family size preferences and contraceptive use among HIV-positive women in Africa, and although many studies have examined the determinants of contraceptive adoption in African countries,4 few studies have examined the intersection between HIV and contraceptive use. Studies on the fertility preferences of HIV-positive women in the United States have shown poor family planning uptake; however, women in these cohorts were often intravenous drug users and are in many ways not comparable to African women.3 Acceptance of contraception among HIV-positive African women may well depend on a number of social, cultural and economic factors, and the mechanisms through which family planning and VCT services are integrated and delivered. Previous studies show that despite initial uptake of contraception after counseling, contraceptive use among HIV-positive women often declines with time, as pre-sero-conversion fertility desires return in the context of an environment of low contraceptive use and cultural constructs that support high fertility.5,6 Thus, although some attention has been paid to the contraceptive needs of HIV-positive women,7,8 and to the influence of knowledge of sero-status on contraceptive use,9 there is a lack of information on the knowledge and concerns surrounding family planning among those living with HIV.
In particular, little attention has been paid to the contraceptive needs of sero-discordant couples (in which one member is HIV-positive and one is HIV-negative). A focus on sero-discordant couples is warranted as these couples are faced with the dual burdens of high risk of HIV transmission and risk of pregnancy, and the resultant risk of mother-to-child transmission of HIV. The challenge is to provide sero-discordant couples with family planning services that can allow them to effectively manage both their risks of HIV transmission and their fertility desires.
In order to provide information to inform the development of family planning services tailored to the unique needs of sero-discordant couples, this article examines the contraceptive knowledge, use and concerns among two cohorts of sero-discordant couples in urban Rwanda and Zambia. Both Rwanda and Zambia have high levels of HIV prevalence and relatively low contraceptive use. Previous studies have demonstrated that the majority of new HIV infections in these contexts occur within married or cohabiting couples10; thus, these settings provide an opportunity to examine knowledge and concerns surrounding contraceptive use in populations that have high fertility and low contraceptive, use and in which married/cohabiting couples represent the greatest risk group for HIV infection. This article does not focus on issues of couple communication, fertility desires or the disclosure of sero-status and its effects on contraceptive use (the couples in the current data all receive their HIV test results together, thus negating the issue of sero-status disclosure). Although these issues are undoubtedly important in shaping a couple's decision to use contraception, with so little research conducted on the contraceptive behaviors of sero-discordant couples, this article focuses only on knowledge and concerns surrounding contraceptive use as a means of establishing whether there are unique knowledge and concern issues among sero-discordant couples that need to be addressed in family planning programming.
Study settings
In 2005, HIV prevalence in Rwanda was estimated at 3% for persons aged 15–49 years, with higher rates among females than males (3.6% and 2.3%, respectively).1 In the capital city of Kigali, HIV infection levels were estimated to be two to three times higher than in the rest of the country.1 The total fertility rate (TFR) in Rwanda was estimated at 6.1 children per woman in 2005, slightly higher than the TFR in 2000 (5.8).11,12 Contraceptive use among married women was 17% for any method and 10% for modern methods (i.e., oral contraceptive pill and sterilization), with injectables being the most common form of modern contraceptive used (5%).11,12 Overall HIV prevalence in Zambia in 2005 was approximately 16% among persons 15–49 years, with higher infection levels among women (18%) than men (13%). In urban areas, HIV infection among pregnant women declined between 1994 and 2004, especially among young people aged 15–24 years from 30% in 1994 to 24% in 2004, yet rates in rural areas of Zambia increased slightly from 11% to 12%.1,13 Zambia's TFR was 5.9 births per woman, and the contraceptive prevalence rate was relatively low, with only 23% of women of reproductive age reporting use of a contraceptive method, and only 17% of these reporting use of a modern method. Among currently married women, the oral contraceptive pill (12%) and withdrawal (5%) were the most commonly used modern and traditional methods.13
Methods
Rwanda Zambia HIV Research Group
The Rwanda Zambia HIV Research Group (RZHRG) currently operates eight free-standing couples voluntary counseling and testing (CVCT) clinics and two clinical research centers in two countries in Africa: Project San Francisco (PSF) in Kigali, Rwanda, and the Zambia Emory HIV Research Project (ZEHRP) in Lusaka, Zambia. Couples receive joint, same-day HIV counseling and testing at the CVCT clinics, an intervention with proven efficacy in reducing HIV incidence among heterosexual couples in the African setting.14–18 Couples meeting eligibility criteria are invited to participate in ongoing clinical studies based at the two research centers. Couples that agree to be enrolled in studies return to the research centers every 3 months for follow-up visits, during which time behavioral and clinical data are collected, and health care, referrals, counseling, and free condoms are offered to study participants. More detailed information regarding CVCT recruitment strategy and procedures, HIV results and demographic characteristics of RZHRG study participants have been published elsewhere.14,15,19–23
Study participants
The data presented in this article are based on a cohort of couples enrolled in the Heterosexual Transmission of HIV in Africa study. Study participants were cohabiting HIV sero-discordant couples identified at RZHRG CVCT centers in Kigali, Rwanda and Lusaka, Zambia. Females were eligible for participation between the ages of 16 and 45, and for males between the ages of 16 and 65. Eligible couples were cohabiting for at least 12 months and planned to stay in Kigali or Lusaka for 1 year from the date of enrollment. Couples with incomplete or inconsistent demographic or family planning data were not included in the study population (less than 5%). In Zambia, individuals dually enrolled in a randomized factorial family planning trial designed to assess contraceptive knowledge, use and concerns were eliminated from this analysis because the informed consent for that study included information on contraceptive methods, which may have influenced their knowledge of family planning (a total of 2029 couples were enrolled in all activities in Zambia: of these, 111 dropped out after the consent process, 975 enrolled in the family planning trial, 471 enrolled in both the family planning and heterosexual transmission trial, leaving 472 couples who were enrolled in the heterosexual transmission study only). From February 2003 to October 2005, 990 couples were tested at RZHRG CVCT centers in Kigali, Rwanda, of which 961 were eligible for this study. In Lusaka, Zambia, from July 2002 to October 2005, 947 couples were tested, and 472 were eligible for this study. Approval for this study was granted by the Emory University Institutional Review Board, the National Ethics Committee of Rwanda, and the University of Zambia Research Ethics Committee.
Statistical analysis
Data for this analysis were collected by trained CVCT counselors and study staff during the clients' initial visit to the CVCT clinic and their subsequent enrollment visit at the research site. Data were entered on-site into Microsoft Access databases, and statistical analyses were performed using SAS software, version 9.1 (SAS Institute Inc., Cary, NC). Participants were asked if they had ever or were currently using a method of contraception, if they had heard of contraceptive methods (both spontaneous and prompted responses were recorded), and if they had any worries or concerns about the methods. These data were collected separately for men and women using a standard questionnaire.
The outcomes of interest included self-reported knowledge of modern family planning methods (oral contraceptive pill, injection, implant [Norplant], IUD, emergency contraception, tubal ligation, and vasectomy). We do not include condoms in our list of modern contraceptives, as the focus of the present study is understanding the knowledge and concerns of sero-discordant couples surrounding methods used primarily to avoid pregnancy. Previous studies have shown that while condoms are effective in lowering rates of HIV transmission, they are associated with relatively high pregnancy rates.24 Our prevention efforts in these countries also promote condoms as a method of HIV prevention, and thus the majority of couples in the cohorts are already using condoms consistently. We also examine use of modern contraceptives, reasons for stopping use of modern contraceptives (side effects, desire pregnancy, not available, take a test or other), and worries or concerns about modern contraception (no worries, doesn't work, bad for health, side effects or no opinion). For knowledge of modern family planning methods, spontaneous and prompted responses were combined to create a binary variable coded “1” if the respondent reported knowledge of that type of contraception (the number of respondents reporting prompted knowledge was too small to allow a separate analysis of spontaneous and prompted knowledge). The analysis of contraceptive use was restricted to a subset of participants who reported knowledge of each particular contraceptive method; aside from condoms, no couples reported dual method use, so this restriction of the analysis sample did not omit couples using more than one method. Similarly, the analyses on reasons for stopping contraceptive use and worries/concerns about contraception were done on a subset of participants that indicated ever using that contraceptive method. Thus, these sample sizes vary by type. This analysis examines the distribution of knowledge, use and attitudes towards contraceptive methods, and compares these by gender and study site (Rwanda or Zambia), and then by study site for females and males separately. Chi-square tests of association and Fisher's exact test were used to assess the statistical significance of differences between the genders and the two study sites.
Results
The demographic profile of study participants is displayed in Tables 1 and 2. In total, 1,433 HIV sero-discordant couples are included in this study, 961 from Kigali, Rwanda, and 472 from Lusaka, Zambia. In Kigali, this includes 515 couples where the female partner is HIV-positive and 446 couples where the male partner is HIV-positive. In Lusaka, this includes 277 couples where the female partner is HIV-positive and 195 couples where the male partner is HIV-positive. The mean age of female study participants is 29 in Rwanda and 30 in Zambia (range, 16–45) years, while the mean age among males is 36 (range, 19–64) years in both Rwanda and Zambia.
Table 1.
Demographic Characteristics of Study Participants in Kigali, Rwanda (01 February 2003 to 01 October 2005) and Lusaka, Zambia (23 July 2002 to 01 October 2005)
| Total | Rwanda | Zambia | |
|---|---|---|---|
| Total number of participants | 2,866 | 1,922 | 944 |
| Total number of couples | 1,433 | 961 | 472 |
| Number of men | 1,433 | 961 | 472 |
| Number of women | 1,433 | 961 | 472 |
| Distribution of HIV status among couples | |||
| Discordant male positive, female negative | 641 | 446 | 195 |
| Discordant male negative, female positive | 792 | 515 | 277 |
| Age range in years (mean) | |||
| Women | 16–45 (29.55) | 16–45 (29.47) | 16–45 (29.70) |
| Men | 18–64 (36.03) | 18–63 (35.95) | 19–64 (36.21) |
| All | 16–64 (32.79) | 16–63 (32.71) | 16–64 (32.96) |
Table 2.
Literacy and Employment Characteristics of Female and Male Study Participants in Kigali, Rwanda (01 February 2003 to 01 October 2005) and Lusaka, Zambia (23 July 2002 to 01 October 2005)
| |
Rwanda |
Zambia |
||
|---|---|---|---|---|
| Women (n = 961) | Men (n = 961) | Women (n = 472) | Men (n = 472) | |
| Understand French (Rwanda) or English (Zambia) | ||||
| Easily | 33 (3%) | 88 (9%) | 112 (24%) | 300 (64%) |
| With difficulty | 86 (9%) | 165 (17%) | 194 (41%) | 155 (33%) |
| No | 842 (88%) | 708 (74%) | 166 (35%) | 17 (4%) |
| Read French (Rwanda) or English (Zambia) | ||||
| Easily | 27 (3%) | 87 (9%) | 93 (20%) | 288 (61%) |
| With difficulty | 89 (9%) | 154 (16%) | 160 (34%) | 145 (31%) |
| No | 845 (88%) | 720 (75%) | 219 (46%) | 39 (8%) |
| Employment | ||||
| All year | 241 (25%) | 509 (53%) | 141 (30%) | 254 (54%) |
| Part of the year | 78 (8%) | 105 (11%) | 68 (14%) | 117 (25%) |
| Once in a while | 100 (10%) | 231 (24%) | 20 (4%) | 27 (6%) |
| N/A | 542 (56%) | 116 (12%) | 243 (51%) | 74 (16%) |
In Rwanda, understanding the French language is relatively low, with only 12% of women and 25% of men reporting that they can understand or read French. Comparatively, English literacy is higher in Zambia, with 24% of women and 64% of men reporting that they can understand English easily. In both countries literacy is much higher among men than among women. Employment rates are similar in both countries, with more than 50% of men reporting to have year-round employment, compared to only 25% and 30% of women in Rwanda and Zambia, respectively.
Knowledge of any modern contraceptive method is high across the board, with a range of 90–99.8%, indicating that they know at least one type of modern contraception (Table 3). In general, women report greater knowledge of contraceptive methods than men, with the exception of emergency contraception and vasectomy in Rwanda for which men report higher levels of knowledge (although the difference is not statistically significant). In Rwanda, knowledge of all other types of contraception is significantly higher among women than among men, with the oral contraceptive pill as the most commonly known contraceptive for both women and men (97% and 86%, respectively; p < 0.0001). In Zambia, emergency contraception is the only method for which levels of knowledge are statistically different for women and men, with 11% of women and 7% of men reporting knowledge of the method (p = 0.0532).
Table 3.
Distribution of Knowledge of Family Planning Method (“Yes” or “No”) among Study Participants in Kigali, Rwanda (01 February 2003 to 01 October 2005) and Lusaka, Zambia (23 July 2002 to 01 October 2005) by Country and Gender
| |
Stratified by country |
|||||
|---|---|---|---|---|---|---|
| |
Rwanda |
Zambia |
||||
| Women (n = 961) | Men (n = 961) | p-value | Women (n = 472) | Men (n = 472) | p-value | |
| Contraceptive method | ||||||
| Any methoda | 940 (98%) | 866 (90%) | <0.0001 | 471 (99.8%) | 464 (98%) | 0.0382b |
| OCP | 929 (97%) | 827 (86%) | <0.0001 | 469 (99%) | 458 (97%) | 0.0120b |
| Injectable | 926 (96%) | 809 (84%) | <0.0001 | 454 (96%) | 401 (85%) | <0.0001 |
| Implant (Norplant) | 674 (70%) | 379 (39%) | <0.0001 | 335 (71%) | 134 (28%) | <0.0001 |
| IUD | 453 (47%) | 283 (29%) | <0.0001 | 325 (69%) | 179 (38%) | <0.0001 |
| Emergency contraceptive | 71 (7%) | 84 (9%) | 0.2761 | 51 (11%) | 34 (7%) | 0.0532 |
| Tubal ligation | 726 (76%) | 640 (67%) | <0.0001 | 357 (76%) | 202 (43%) | <0.0001 |
| Vasectomy | 178 (19%) | 215 (22%) | 0.0364 | 153 (32%) | 123 (26%) | 0.0318 |
| |
Stratified by gender |
|||||
|---|---|---|---|---|---|---|
| |
Women |
Men |
||||
| Rwanda (n = 961) | Zambia (n = 472) | p-value | Rwanda (n = 961) | Zambia (n = 472) | p-value | |
| Contraceptive method | ||||||
| Any methoda | 940 (98%) | 471 (99.8%) | 0.0024b | 866 (90%) | 464 (98%) | <0.0001 |
| OCP | 929 (97%) | 469 (99%) | 0.0015b | 827 (86%) | 458 (97%) | <0.0001 |
| Injectable | 926 (96%) | 454 (96%) | 0.8715 | 809 (84%) | 401 (85%) | 0.7039 |
| Implant (Norplant) | 674 (70%) | 335 (71%) | 0.7436 | 379 (39%) | 134 (28%) | <0.0001 |
| IUD | 453 (47%) | 325 (69%) | <0.0001 | 283 (29%) | 179 (38%) | 0.0013 |
| Emergency contraceptive | 71 (7%) | 51 (11%) | 0.0294 | 84 (9%) | 34 (7%) | 0.3197 |
| Tubal ligation | 726 (76%) | 357 (76%) | 0.9705 | 640 (67%) | 202 (43%) | <0.0001 |
| Vasectomy | 178 (19%) | 153 (32%) | <0.0001 | 215 (22%) | 123 (26%) | 0.1223 |
Any method = indicated 1 (spontaneous) or 2 (prompted) to knowledge of at least one contraceptive method.
Two-sided Fishers exact used, because less than 5 in at least one cell.
Among women, levels of contraceptive knowledge are generally higher in Zambia, though three out of the eight possible methods do not reveal statistically significant differences between women in the two countries (injectables, Norplant, and tubal ligation). In both countries, women report the highest levels of knowledge for the oral contraceptive pill (97% and 99% in Rwanda and Zambia, respectively; p = 0.0015), with the lowest levels of knowledge about emergency contraception (7% and 11%, respectively; p = 0.0294). Overall, men in Zambia report higher knowledge of any method than men in Rwanda (98% and 90%, respectively; p < 0.0001); however, knowledge of Norplant, emergency contraception, and tubal ligation are greater among men in Rwanda than Zambia. The levels of knowledge among men in Rwanda and Zambia are not different for injectables, and vasectomy (p = 0.7039, p = 0.3197, respectively).
Despite the fact that these data were obtained from a sample of cohabiting couples, the reported figures for contraceptive use differ for women and men in both Rwanda and Zambia (Table 4). In general, women report more use of contraceptive methods than men in both countries. Reported use is significantly greater for any contraceptive method (p < 0.0001 in both Rwanda and Zambia), oral contraceptive pill (p = 0.0006 in Rwanda, p < 0.0001 in Zambia), and injectables (p < 0.0001 in both Rwanda and Zambia).
Table 4.
Distribution of Ever Use of Family Planning Method (“Yes” or “No”) among Study Participants who Know about the Type of Contraception in Kigali, Rwanda (01 February 2003 to 01 October 2005) and Lusaka, Zambia (23 July 2002 to 01 October 2005) by Country and Gender
| |
Stratified by country |
|||||
|---|---|---|---|---|---|---|
| |
Rwanda |
Zambia |
||||
| Women | Men | p-value | Women | Men | p-value | |
| Contraceptive method | ||||||
| Any methoda | 281/938d (30%) | 153/866 (18%) | <0.0001 | 278/471 (59%) | 191/463 (41%) | <0.0001 |
| OCP | 142/929 (15%) | 81/827 (10%) | 0.0006 | 244/469 (52%) | 172/458 (38%) | <0.0001 |
| Injectable | 220/926 (24%) | 98/809 (12%) | <0.0001 | 112/454 (25%) | 52/401 (13%) | <0.0001 |
| Implant (Norplant) | 14/674 (2%) | 8/379 (2%) | 0.9708 | 3/335 (1%) | 2/134 (1%) | 0.6269c |
| IUD | 7/453 (2%) | 5/283 (2%) | 0.8174 | 13/325 (4%) | 3/179 (2%) | 0.1909c |
| Emergency contraceptive | 0/71 (0%) | 1/84 (1%) | 1.0b | 3/51 (6%) | 0/34 (0%) | 0.2714b |
| |
Stratified by gender |
|||||
|---|---|---|---|---|---|---|
| |
Women |
Men |
||||
| Rwanda | Zambia | p-value | Rwanda | Zambia | p-value | |
| Contraceptive method | ||||||
| Any methoda | 281/938d (30%) | 278/471 (59%) | <0.0001 | 153/866 (18%) | 191/463 (41%) | <0.0001 |
| OCP | 142/929 (15%) | 244/469 (52%) | <0.0001 | 81/827 (10%) | 172/458 (38%) | <0.0001 |
| Injectable | 220/926 (24%) | 112/454 (25%) | 0.7097 | 98/809 (12%) | 52/401 (13%) | 0.6714 |
| Implant (Norplant) | 14/674 (2%) | 3/335 (1%) | 0.1696 | 8/379 (2%) | 2/134 (1%) | 1.0c |
| IUD | 7/453 (2%) | 13/325 (4%) | 0.0329 | 5/283 (2%) | 3/179 (2%) | 1.0c |
| Emergency contraceptive | 0/71 (0%) | 3/51 (6%) | 0.0705b | 1/84 (1%) | 0/34 (0%) | 1.0c |
Any method = indicated 1 (past, not now) or 2 (now) for use of any of the contraceptive methods.
Two-sided Fishers exact test used, because 0 observations in one cell.
Two-sided Fishers exact test used, because less than five in cell(s).
Denominator is 938—not 940—because two individuals had tubal ligation or vasectomy. This was not an option for this variable, so these values are missing for ever use of any method.
Contraceptive use is higher among women in Zambia than women in Rwanda (59% Zambia, 30% Rwanda [p < 0.0001]). Interestingly, 52% of women in Zambia report using oral contraceptive pills, compared to only 15% in Rwanda (p < 0.0001). The percentage of women reporting use of injectables in Rwanda was 24%, which is greater than the percentage of women using oral contraceptive pills in the same country (15%). This is a reversal of the pattern observed in Zambia, where 25% of women reported using injectables and 52% report using oral contraceptive pills. Among men, the only statistically significant differences between the two countries were among those using any method (at least one) and those using oral contraceptive pills (both p < 0.0001). Less than 6% of women and men in both countries reported using Norplant, IUD, or emergency contraception.
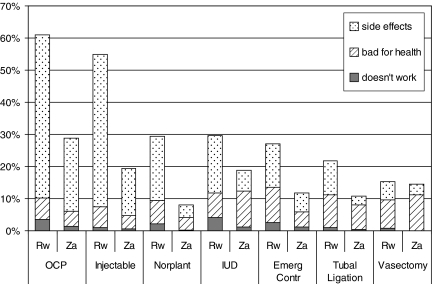
The distribution of worries or concerns about contraceptive types is displayed in Figure 1. Among persons reporting knowledge of a contraceptive method, a higher percentage of respondents report worries or concerns in Rwanda than in Zambia. The most common concerns are side effects, with 51% of the study population in Rwanda reporting concerns about side effects for oral contraceptive pills, compared with 23% of the study population in Zambia. Similarly, 47% of persons in Rwanda reported concerns about side effects for injectables, compared with 15% in Zambia. In Zambia, there was more concern that contraception was bad for one's health for the specific methods of IUD, tubal ligation, and vasectomy. In Rwanda, this was true only for vasectomy, though 11% and 10% of persons were concerned that emergency contraception and tubal ligation were also bad for one's health. In both Rwanda and Zambia, the percentage of women and men reporting concerns about the efficacy of a contraceptive method was not higher than 4%.
FIG. 1. .
Distribution of worries or concerns about contraception among those who know about contraceptive type in Kigali, Rwanda (01 February 2003 to 01 October 2005) and Lusaka, Zambia (23 July 2002 to 01 October 2005).
Discussion
The results reveal an interesting profile of contraceptive knowledge and use among sero-discordant couples in two African countries experiencing the dual burden of high levels of HIV and fertility. In both settings, despite high levels of knowledge of contraception, use of contraceptive methods remains relatively low. Interestingly, the levels of reported knowledge of contraceptive methods were as high as those reported by women of reproductive age in the demographic and health surveys of each country. The disconnect between knowledge and use may reflect the influence of a myriad of social, cultural and economic factors that inhibit access to and adoption of contraceptive methods. Knowledge of a contraceptive method clearly does not always translate into method adoption, and common factors influencing the non-use of contraception are a lack of female decision-making power,25 poor economic resources,26 low-quality care at family planning services,27 and desires for large families.28 As in many sub-Saharan African countries, the need clearly exists to make contraceptive services more socially and economically accessible to couples, and this need is particularly pressing for sero-discordant couples, who face issues associated with achieving fertility desires while also managing the risk of HIV infection.
There is a clear gender difference in both the reporting of knowledge and use of contraceptive methods. Women reported higher levels of knowledge of contraception in both study settings pointing to the need to improve men's knowledge of contraception. Previous studies have highlighted the inhibiting effect that men's lack of knowledge of, or negative attitudes towards contraception, have on a woman's ability to adopt a method of contraception.28–31 Involving men in family planning education, providing family planning services tailored to the needs of men, and delivering family planning education directly to men are some of the mechanisms through which the role of men as barriers to contraceptive use may be reduced. This is particularly important in an environment in which male desires for large numbers of children and high HIV prevalence may co-exist; the involvement of men in family planning programming may act to reduce both fertility and the heterosexual and mother-to-child transmission of HIV.
Interestingly, women were more likely to report contraceptive use than their partners, and this was particularly true for contraceptive methods that did not require male involvement. This points to potential clandestine contraceptive use, in which women are disecretly using contraception without the knowledge of their partners, behavior that has been reported in other African nations.32 This behavior may allow women who have differing fertility desires to their husbands to avoid further pregnancies. More attention is needed to counseling sero-discordant couples on the risks of unprotected sex and providing them with information to allow them to safely manage their fertility intentions.
Fears of side effects were the dominant concern reported from both men and women for almost all contraceptive methods. Although the reporting of fears of side effects was greater in Rwanda, a sizeable proportion of respondents in Zambia also reported this concern. Previous studies have demonstrated that fears of side effects are often a barrier to the adoption of contraceptive methods, and such concerns often result in a reliance on traditional forms of contraception (e.g., withdrawal).33,34 Many of these concerns are often ill-founded and are the consequence of misinformation on contraception.35 These results again point to the need for targeted family planning education that can dispel many of the myths that surround the use of modern contraceptive methods. Although such information is required by all reproductive age adults in high fertility settings such as Rwanda and Zambia, family planning programs must recognize the unique needs of sero-discordant couples, in terms of the need to reduce the risk of HIV infection. Fear of side effects of contraception may be exacerbated in HIV-positive women who are particularly sensitive about maintaining their health status6; family planning programs must recognize this and make the discussion of the relationship between contraceptive use and HIV disease central to HIV and family planning counseling.
The cohorts of couples analyzed here are not representative of the general adult population; they represent couples who opted to attend for HIV testing and to enroll in research studies. This potential lack of representation is the main limitation of this study. However, there are currently no nationally representative data sets that are both couple-based and include the sero-status for each partner; the data presented here is a unique opportunity to understand the contraceptive, attitudes and behaviors of couples at high risk of HIV transmission.
Conclusions
Despite high levels of contraceptive knowledge, use of methods to prevent pregnancy remained low among sero-discordant couples. Although the levels of knowledge among sero-discordant couples largely reflect those seen in the reproductive age population of each country, the unique needs of sero-discordant couples in terms of balancing fertility desires and HIV risk, mark them out as a key target group for the prevention of heterosexual and mother-to-child HIV transmission. These needs are, however, largely missing from many current family planning efforts, which focus on the prevention of pregnancies in absence of the reduction of the risk of HIV transmission.36 Both existing family planning and HIV services need to recognize these dual needs, and there is clearly a need to further integrate the two types of service. Including information on family planning in VCT services in addition to tailoring the delivery of family planning information to meet to needs and concerns of HIV-positive women or those with HIV-positive partners is an essential step in the delivery of services and prevention efforts to reduce the transmission of HIV. However, such efforts must also recognize the social and cultural environments in which couples exist, and include efforts to reduce these barriers to contraceptive adoption through the promotion of couple-based counseling and the involvement of men in family planning programs.
Acknowledgments
We thank the study participants, staff, interns, and co-investigators of the Rwanda Zambia HIV Research Group. This study has been funded primarily by federal funds from the U.S. National Institute of Mental Health (grant R01 MH 66767) and the National Institute of Child Health and Human Development (grant R01 HD 40125), with contributions from the Fogarty AIDS International Training and Research Program (FIC 2D43 TW001042), the Social & Behavioral Core of the Emory Center for AIDS Research (P30 AI050409), and the International AIDS Vaccine Initiative.
Disclosure Statement
No competing financial interests exist.
References
- 1.Joint United Nations Program on HIV/AIDS (UNAIDS) Report on the global AIDS epidemic: a UNAIDS 10th anniversary special edition. Geneva: UNAIDS; 2006. [Google Scholar]
- 2.CDC. Family Planning Methods and Practice, Africa. Washington, DC: Centers for Disease Control and Prevention (CDC); 2000. [Google Scholar]
- 3.Preble E. Huber D. Piwoz E. Family planning and the prevention of mother-to-child transmission of HIV: technical and promgrammatic issues. Adv Africa. 2003:1–38. [Google Scholar]
- 4.Stephenson R. Bascheri A. Clements S, et al. Contextual influences on modern contraceptive use in sub-Saharan Africa. Am J Public Health. 2007;97:1233–1240. doi: 10.2105/AJPH.2005.071522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baylies C. The impact of HIV on family size preference in Zimbabwe. Reprod Health Matters. 2000;8:77–86. doi: 10.1016/s0968-8080(00)90008-9. [DOI] [PubMed] [Google Scholar]
- 6.King R. Estey J. Allen S, et al. A family planning intervention to reduce vertical transmission of HIV in Rwanda. AIDS. 1995;(Suppl 1):S45–S51. [PubMed] [Google Scholar]
- 7.Rutneberg N. Baek C. Field experiences integrating family planning into programs to prevent mother-to-child transmission of HIV. Studies Fam Plann. 2005;36:235–245. doi: 10.1111/j.1728-4465.2005.00064.x. [DOI] [PubMed] [Google Scholar]
- 8.Duerr D. Hurst S. Kourtis AP, et al. Integrating family planning and prevention of mother-to-child HIV transmission in resource poor settings. Lancet. 2005;366:261–263. doi: 10.1016/S0140-6736(05)66917-6. [DOI] [PubMed] [Google Scholar]
- 9.Hoffman IF. Martinson FEA. Powers KA, et al. The year-long effect of HIV-positive test results on pregnancy intentions, contraceptive use and pregnancy incidence among Malawi women. J Acquir Immune Defic Syndr. 2008;47:477–483. doi: 10.1097/QAI.0b013e318165dc52. [DOI] [PubMed] [Google Scholar]
- 10.Dunkle K. Stephenson R. Karita E, et al. Estimating the proportion of new heterosexually transmitted HIV infections that occur within married/cohabiting couples in urban Zambia and Rwanda. Lancet. 2008;371:2183–2191. doi: 10.1016/S0140-6736(08)60953-8. [DOI] [PubMed] [Google Scholar]
- 11.Institut National de la Statistique du Rwanda (INSR) and ORC Macro. Rwanda Demographic and Health Survey 2005. Calverton, MD: INSR and ORC Macro; 2006. [Google Scholar]
- 12.ORC Macro. www.measuredhs.com. [Mar 17;2007 ]. www.measuredhs.com
- 13.Central Statistical Office [Zambia], Central Board of Health [Zambia], ORC Macro. Zambia Demographic and Health Survey 2001–2002. Calverton, MD: Central Statistical Office, Central Board of Health, and ORC Macro; 2003. [Google Scholar]
- 14.Allen S. Meinzen-Derr J. Kautzman M, et al. Sexual behavior of HIV discordant couples after HIV counseling and testing. AIDS. 2003;17:733–740. doi: 10.1097/00002030-200303280-00012. [DOI] [PubMed] [Google Scholar]
- 15.Allen S. Tice J. Van de Perre P, et al. Effect of serotesting with counselling on condom use and seroconversion among HIV discordant couples in Africa. BMJ. 1992;304:1605–1609. doi: 10.1136/bmj.304.6842.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chu HY. Crump JA. Ostermann J, et al. Sociodemographic and clinical characteristics of clients presenting for HIV voluntary counselling and testing in Moshi, Tanzania. Int J STD AIDS. 2005;16:691–696. doi: 10.1258/095646205774357307. [DOI] [PubMed] [Google Scholar]
- 17.Kawichai S. Celentano DD. Chaifongsri R, et al. (2002). Profiles of HIV voluntary counseling and testing of clients at a district hospital, Chiang Mai province, Northern Thailand, from 1995 to 1999. J Acquir Immune Defic Syndr. 2002;30:493–502. doi: 10.1097/00126334-200208150-00005. [DOI] [PubMed] [Google Scholar]
- 18.Sangiwa MG. Grinstead OA. Hogan M, et al. Characteristics of individuals and couples seeking HIV-1 prevention services in Dar es Salaam, Tanzania: The Voluntary HIV-1 Counseling and Testing Efficacy Study. AIDS Behav. 2000;4:25–33. [Google Scholar]
- 19.Kempf MC Rwanda/Zambia HIV Research Group. Predictors of enrollment and retention for HIV discordant couples in Lusaka, Zambia. Antivir Ther. 2003;8:S223. [Google Scholar]
- 20.McKenna SL. Muyinda GK. Roth D, et al. Rapid HIV testing and counseling for voluntary testing centers in Africa. AIDS. 1997;11:S103–S110. [PubMed] [Google Scholar]
- 21.Modjarrad K. Zulu I. Karita E, et al. Predictors of HIV serostatus among HIV discordant couples in Lusaka, Zambia and female antenatal clinic attendants in Kigali, Rwanda. AIDS Res Hum Retroviruses. 2005;21:5–12. doi: 10.1089/aid.2005.21.5. [DOI] [PubMed] [Google Scholar]
- 22.Nyblade LC. Menken J. Wawer MJ, et al. Population-based HIV testing and counseling in rural Uganda: participation and risk characteristics. J Acquir Immune Defic Syndr. 2001;28:463–470. doi: 10.1097/00042560-200112150-00010. [DOI] [PubMed] [Google Scholar]
- 23.Allen S. Lindan C. Serufilira A, et al. Human immunodeficiency virus infection in urban Rwanda: demographic and behavioral correlates in a representative sample of childbearing women. JAMA. 1991;266:1657–1663. [PubMed] [Google Scholar]
- 24.Cates W. Steiner MJ. Dual protection against unintended pregnancy and sexually transmitted infections: what is the best contraceptive approach? Sexually Transm Dis. 2002;29:168–174. doi: 10.1097/00007435-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Chapagain M. Masculine interest behind high prevalence of female contraceptive methods in rural Nepal. Aust J Rural Health. 2005;13:35–42. doi: 10.1111/j.1440-1854.2004.00643.x. [DOI] [PubMed] [Google Scholar]
- 26.Stephenson RB. Tsui AO. Community influences on reproductive health service utilisation in Uttar Pradesh, India. Stud Fam Plann. 2002;33:309–320. doi: 10.1111/j.1728-4465.2002.00309.x. [DOI] [PubMed] [Google Scholar]
- 27.Hamid S. Stephenson R. Provider and health facility influences on contraceptive adoption in urban Pakistan. Int Fam Plann Perspect. 2006;32:71–78. doi: 10.1363/3207106. [DOI] [PubMed] [Google Scholar]
- 28.Bankole A. Singh S. Couple's fertility and contraceptive decision making in developing countries; hearing the man's voice. Int Fam Plann Perspect. 1998;24:15–24. [Google Scholar]
- 29.Mbizvo M. Adamchak DJ. Family planning knowledge, attitudes and practices of men in Zimbabwe. Stud Fam Plann. 1991;22:31–38. [PubMed] [Google Scholar]
- 30.Agadjaian V. Men's talk about “women's matters”: gender, communication and contraception in urban Mozambique. Gender Society. 2002;16:194–215. [Google Scholar]
- 31.Agha S. Sexual activity and condom use in Lusaka, Zambia. Int Fam Plann Perspect. 1998;24:32–37. [Google Scholar]
- 32.Castle S. Konate MK. Ulin PR, et al. A qualitative study of clandestine contraceptive use in urban Mali. Stud Fam Plann. 1999;30:231–248. doi: 10.1111/j.1728-4465.1999.00231.x. [DOI] [PubMed] [Google Scholar]
- 33.Ali M. Clel J. Contraceptive discontinuation in six developing countries: a cause specific analysis. Int Fam Plann Perspect. 1995;21:92–97. [Google Scholar]
- 34.Tolley E. Loza S. Kafafi L, et al. The impact of menstrual side effects on contraceptive discontinuation: findings from a longitudinal study in Cairo, Egypt. Int Fam Plann Perspect. 2005;31:15–23. doi: 10.1363/3101505. [DOI] [PubMed] [Google Scholar]
- 35.Mistik S. Nacar M. Mazicioglu M, et al. Married men's opinions and involvement regarding family planning in rural areas. Contraception. 2003;67:133–137. doi: 10.1016/s0010-7824(02)00459-6. [DOI] [PubMed] [Google Scholar]
- 36.Foreit KGF. Hardee K. Agarwal K. When does it make sense to consider integrating STI and HIV services with Family Planning Services. Int Fam Plann Perspect. 2002;28:106–107. [Google Scholar]