Abstract
Background
African American women have more symptoms of depressed mood than white women. Adverse neighborhood conditions may contribute to these symptoms. Although reductions in depressive symptoms with physical activity have been demonstrated in white adults, little research has examined the mental health benefits of physical activity in African American women. Further, it is unknown whether physical activity can offset the effects of living in disadvantaged neighborhoods on depressive symptoms. The purpose of this study was to examine the relationships among neighborhood characteristics, adherence to a physical activity intervention, and change over time in depressive symptoms in midlife African American women.
Methods
Two hundred seventy-eight women participated in a home-based, 24-week moderate-intensity walking intervention. Either a minimal treatment (MT) or enhanced treatment (ET) version of the intervention was randomly assigned to one of the two community health centers. Walking adherence was measured as the percentage of prescribed walks completed. Objective and perceived measures of neighborhood deterioration and crime were included.
Results
Adjusting for demographics, body mass index (BMI), and depressive symptoms at baseline, walking adherence and objective neighborhood deterioration were associated with significantly lower depressive symptoms, whereas perceived neighborhood deterioration was associated with significantly higher depressive symptoms at 24 weeks.
Conclusions
Adherence to walking as well as aspects of the environment may influence depressive symptoms in African American women. In addition to supporting active lifestyles, improving neighborhood conditions may also promote mental health among African American women.
Introduction
Along with such associated symptoms as changes in appetite, sleep, and feelings of worthlessness, depression is characterized by a marked downturn in mood or loss of pleasure that interferes with daily life and normal functioning.1 Many people, however, have experienced symptoms that mimic or match one or more of these symptoms without having enough of them to have a diagnosable health problem of depression.2 Epidemiological data show that the prevalence of depressive symptoms is higher in African American women than in white women.3 Known individual characteristics that place women at risk for depressive symptoms are low income, not working, being unmarried, and low educational attainment.3,4 Further, there is some evidence from longitudinal studies to suggest that obesity is a stigmatizing attribute that promotes negative stereotyping and produces depressive symptoms.5
In recent years, attention has focused beyond individual characteristics to the effects of neighborhood characteristics (e.g., socioeconomic status [SES], built environment, social environment) on depressive symptoms. Neighborhood conditions may be particularly salient for African American women because they are more likely than white women, for example, to live in disadvantaged neighborhoods or neighborhoods with fewer economic or other resources and more hazards.6–8 In addition to cardiovascular benefits and reduction in obesity,9,10 a growing body of evidence from observational and intervention studies suggests that leisure time physical activity may decrease depressive symptoms.11 It is not yet known, however, if physical activity can offset the negative effects of living in disadvantaged neighborhoods on depressive symptoms among African American women. The purpose of this study was to examine relationships among neighborhood characteristics, adherence to a physical activity intervention, and change over time in depressive symptoms in midlife African American women.
Neighborhood characteristics and depressive symptoms
Two recent reviews of neighborhood characteristics and depressive symptoms or major depression found that most studies have focused on neighborhood SES, with the majority finding associations in the expected direction.12,13 Fewer studies have examined specific features of the social environment (e.g., social disorder, crime) and especially the physical environment (e.g., vacant lots, abandoned buildings) that may influence depressive symptoms, with most relying on respondents' perceptions (subjective appraisals or understandings) of their environment.12,13 For example, in a cross-sectional study of African Americans and whites residing in a racially integrated neighborhood, those who perceived more neighborhood problems (e.g., crime, drug, and gang activity; lack of access to healthcare, banking, grocery stores, and transportation; poor street lighting) had higher levels of anxiety, stress, and depression.14 Likewise, in a sample of African American women living in a low-income, predominantly African American neighborhood in Detroit, perceived neighborhood safety stress was directly and positively associated with depressive symptoms.15 A longitudinal analysis of persons residing in disadvantaged areas showed baseline perceptions of neighborhood problems, such as vacant housing, burglary, robbery, and vandalism, predicted higher rates of depression at follow-up,16 although others have found no association.17,18
Among the few studies using objective indicators (empirically observable measures derived from sources independent of respondents' perceptions or self-reports) of neighborhood physical and social environments, crime and deterioration have been among the most commonly studied neighborhood characteristics, with complex results. For example, one recent report found depressive/anxiety disorders were more likely among individuals who both lived in a high crime area and had violence exposure,19 whereas another suggested crime may indirectly impact depressive symptoms through perceptions of the neighborhood and personal experience with neighborhood violence.20 There are some conflicting reports related to objective neighborhood deterioration and depressive symptoms. Whereas one study found no association in an African American sample,17 another study in an African American and white urban sample found fear of crime and social capital mediated the association between residential building deterioration and depressive symptoms.21 Nonetheless, only a handful of the studies have included substantively equivalent objective and perceived measures of neighborhood characteristics, with even fewer comparing the relative effects of perceived and objectively measured neighborhood characteristics on depressive symptoms.
Physical activity and depressive symptoms
A recent review of physical activity and the likelihood of depression11 included 9 observational studies with nonclinical community samples22–30 and 16 interventions with healthy or mildly depressed individuals living in the United States.31–45 All but 123 of the 9 observational studies showed an inverse relationship between physical activity and depressive symptoms, and the positive effects of physical activity persisted after adjusting for differences in individual characteristics, including sociodemographics, selected health behaviors, self-reported physical disorders, and comorbid mental disorders.24,26,28,29 The only study with a large representative sample of African American women found that women who reported vigorous exercise in both high school and adulthood had the lowest odds of depressive symptoms.30 Despite evidence showing that perceived lack of neighborhood safety46–48 and unpleasant aesthetics49–53 (e.g., deterioration) are barriers to physical activity, only 1 of the 9 observational studies included these neighborhood problems. That study failed to examine the interaction between neighborhood problems and physical activity on depressive symptoms.29
Despite some inconsistencies in the intervention studies, the preponderance of evidence verifies observational findings by suggesting that physical activity can improve depressive symptoms.11 Nonetheless, the intervention studies have several limitations with respect to understanding relationships between physical activity and improvement of depressive symptoms in African American women. First, either they did not specify race or their participants were predominantly white. As noted by Wise et al.,30 physical activity may serve as a buffer for African American women against stressful life situations, such as those posed by disadvantaged neighborhoods. Second, only King et al.40 examined whether there were factors common to tested interventions that might be more sensitive predictors of psychological outcomes than intervention assignment; they found that regardless of intervention type, exercise participation level or adherence was associated with fewer depressive symptoms. Last, none of the intervention studies examined the joint influence of neighborhood characteristics and physical activity on depressive symptoms.
Study hypotheses
We developed a 24-week, home-based, moderate-intensity walking intervention for midlife African American women residing throughout metropolitan Chicago. We compared an enhanced treatment (ET) that included behavioral strategies culturally targeted and tailored to African American women with a minimal treatment (MT) for effects on depressive symptoms. The limitations of prior studies of physical activity interventions and depressive symptoms were addressed by including a socioeconomically diverse sample of African American women and both objective and perceived measures of neighborhood characteristics (deterioration and crime) as predictors of depressive symptoms. In addition, rather than relying solely on treatment group, we examined the influence of adherence to physical activity on depressive symptoms. First, we hypothesized that at the end of 24 weeks, ET women compared with MT women would have greater improvement in their depressive symptoms. We also hypothesized that controlling for individual characteristics, walking adherence at 24 weeks would be associated with lower depressive symptoms, whereas neighborhood deterioration and crime would be associated with higher depressive symptoms. Our third hypothesis was that walking adherence would moderate the effects of neighborhood deterioration and crime on depressive symptoms at 24 weeks.
Materials and Methods
Design and setting
The Woman's Walking Program was a clinical trial that had a 24-week adoption phase.54 Using a quasi-experimental design, either the ET or MT was randomly assigned to one of two federally qualified Chicago community health centers serving communities with >25% of the population living below poverty level, >65% African American residents, and among the top 20% of 77 Chicago community areas with high heart disease mortality rates.55 Random assignment of treatments to noncontiguous communities avoided the problem of women having acquaintances assigned to the opposite condition choosing to walk together and causing treatment contamination. To make the study logistically feasible, women were staggered into the study over 3½ years (2001–2005); thus, it was not possible to randomly assign the intervention to the community health center site after all the subjects were recruited.
Subjects
Recruitment efforts were concentrated within a 3-mile radius of the health centers and included distribution of print materials, presentations at community sites, and newspaper announcements.56 Participants were also recruited through social networking. All recruitment materials had eligibility criteria and site-specific information, including telephone numbers and contact information. Women were recruited to one of two community health centers (ET or MT), and, thus, were not aware of the alternate treatment. To be eligible the women had to have no signs or symptoms of cardiovascular disease (CVD), have no participation in regular moderate or vigorous exercise (i.e., 30 minutes two or more times a week in the preceding 6 months), and be without any disabilities preventing activity. After initial screening over the telephone, women were scheduled for further screening at their respective community health center. Data collection included a health history and physical assessment, lipoprotein level, and height and weight with a nurse practitioner and a maximal aerobic fitness test with an exercise physiologist.
Of the 628 women screened, 281 women met the eligibility criteria and enrolled in the study56; 156 women were recruited at the ET site and 125 women at the MT site. For the purpose of the analysis presented here, 3 women whose neighborhoods extended into an adjacent state (Indiana) were excluded, for a total sample of 278 women.
Protocol and intervention
Following final eligibility screening at the community health center, women completed study questionnaires (including depressive symptoms) and were oriented to their treatment. Behavioral strategies based on Social Cognitive Theory (problem solving, role modeling, supportive feedback) and the Transtheoretical Model were applied systematically.57
Women in both treatment groups received a tailored walking prescription from the program's exercise physiologist to walk a minimum of three times a week within their target heart rate range determined by a baseline maximal aerobic test. Women were to walk two times per week for the first 4 weeks and to gradually progress to walk three or more times per week for 20–30 minutes within their moderate-intensity target heart rate. The frequency of walking was set at a minimum of 3 days a week based on the finding of King et al.58 that adherence in a home-based walking program dropped as a result of the increasing difficulty in maintaining the recommended minimum of five times a week. Healthy People 2010 indicates that if frequency falls below 3 days a week, however, people are less likely to adhere to a regular pattern of exercise.59 Thus, the overall expectation was 68 walks over 24 weeks.58 The women's walks were recorded on heart rate monitors and exercise logs.
The ET also had four weekly 1-hour motivational workshops designed to be culturally sensitive to African American women based on focus groups held with community women.46 Each workshop began with a 10-minute video featuring African American role models discussing the featured topic and were led by a staff member of the same ethnicity who was familiar with the community. Workshops were followed by tailored supportive staff telephone calls weekly for 3 weeks (weeks 5–7) and every other week for 14 weeks (weeks 10–22) during a 24-week adoption phase. Women were encouraged to add purposeful walking for leisure to their daily activity but were also encouraged, because of the known benefits of lifestyle physical activity on cardiovascular health9 and psychological health,60 to seek additional utilitarian walking. Women returned to the community health center between weeks 8 and 9 to have their heart rate monitor data downloaded and at the end of adoption (24 weeks) to download heart rate monitor data and to complete study questionnaires (including depressive symptoms).
Measures
Depressive symptoms
The 20-item Center for Epidemiological Studies-Depression (CES-D) scale was used to assess symptoms associated with depressed mood in the preceding week. Participants responded on a scale from 1 (rarely or none of the time) to 4 (most or all of the time), and responses were summed for a total score.61 A Cronbach's alpha of 0.88 in a large probability sample of African Americans has been demonstrated62; the Cronbach's alpha for this sample was 0.71.
Walking adherence
Adherence to walking frequency was calculated as the percentage of the prescribed minimum of 68 walks completed during the adoption phase of the intervention. Adherence was measured with heart rate monitors, a walking logbook, and an automated telephone response system.54 Briefly, women wore a Polar Accurex Plus Heart Rate Monitor (HRM) (Warminster, PA) during each walking session. The monitor was programmed with the woman's target heart rate range based on her baseline maximal aerobic fitness test. The wrist monitor can store individual data files for 67 hours of information. Women were encouraged to carry a small walking logbook with them and record the day, time, and duration of each walk. Women were to report their walking every week from their logs through an automated telephone response system that provided prompts for data entry. Staff tracked calls and made reminder telephone calls to women when no reports were registered for 3 weeks. The data from these three sources were compared, and duplicate data were eliminated. If no data were recorded in any of the three measures for a particular week, the participant was assumed to not have walked.
Neighborhood characteristics
Using both objective and perceived measures, we assessed two neighborhood environmental characteristics: deterioration and crime. Home addresses for all participants were available and geocoded to StreetMap USA using ArcGIS 9.1 (ESRI, Redlands, CA). Based on the assumption of a 30-minute walk at a moderate pace (4 mph), women's neighborhoods were defined as, and environmental characteristics measured within, 1-mile radial buffers around their homes. Other neighborhood studies have also used 1-mile radii.63 However, we also tested the sensitivity of our findings to objective environmental measures derived based on ¼-mile radial buffers, considered an appropriate distance for utilitarian walking (e.g., walking to store), around their homes.64
Neighborhood deterioration
Objective neighborhood deterioration was measured as the mean of two standardized scores (Z-scores) for the percent vacant housing units and percent net land area with abandoned buildings or rubble lots in the neighborhood (α = 0.79). Drawn from the Census 2000 Summary File 1 (SF1), percent of housing units that were vacant was based on census blocks intersecting the participant's neighborhood. The percent net (minus water) land area in the neighborhood that was abandoned buildings or rubble lots was derived from the 2001 Land Use Inventory for Metropolitan Chicago (category 4220).65 Higher scores indicate greater neighborhood deterioration. Perceived deterioration was measured with a single item from the Neighborhood Problems Scale,66 which allows participants to rate their neighborhood. Participants rated how much of a problem abandoned houses or buildings were in their neighborhood on a 3-point scale: not a problem (0), somewhat of a problem (1), and big problem (2).66 Because of the skewed distribution, the measure was dichotomized to not a problem (0) and somewhat or a big problem (1).
Neighborhood crime
Objective neighborhood crime was measured as the annual number of police-reported incidents of violent person-to-person crimes (homicide, robbery, aggravated assault, criminal sexual assault) in the neighborhood. As described elsewhere,67 exact counts of neighborhood crime incidents were aggregated from police files for women living in neighborhoods entirely inside Chicago. However, outside Chicago, the smallest spatial scale at which violent crime incidents were available was by municipality from the Annual Illinois Uniform Crime Report Database (2002–2005).68 Thus, for neighborhoods completely outside Chicago, number of violent crime incidents was estimated based on crime densities (number of crimes per unit land area), according to the proportion of the neighborhood in each municipality. For neighborhoods that were partially inside and partially outside Chicago, exact crime counts for the Chicago portion were combined with weighted crime densities for the suburban portions. Crime data were applied to correspond to the majority year in which the woman participated in the intervention.
Perceived neighborhood crime was measured with seven items from the Neighborhood Problems Scale,66 which included problems with stealing, destroying property, guns and violence, disrespect for laws/rules/authority, rape or sexual assaults, getting attacked or robbed on the street, and illegal gambling. Participants rated the degree to which each item was a problem in their neighborhoods on a 3-point scale: not a problem (0), somewhat of a problem (1), and big problem (2). The seven items were summed for a score range from 0 to 14, where a higher score indicated greater perceived neighborhood crime. There was strong internal consistency (α = 0.90).
Covariates/individual characteristics
Demographic variables of age, marital status, education, and income as well as body mass index (BMI) were included as covariates in multivariate analyses. Age was measured in years. Marital status was designated as married or not married (reference category). Educational status was high school, GED, or less; some college or vocational school; and college or above (reference category). Annual household income was measured using 11 categories each with $10,000 increment from <$10,000 to ≥$100,000. BMI was calculated by dividing weight (converted to kilograms) by height (converted to meters) squared (kg/m2).69
Statistical analysis
Multiple attempts were made to schedule and reschedule missed assessments at 24 weeks.54 Overall, 69% of the ET group and 53% of the MT group participated in completing questionnaires at 24 weeks (total n = 107, 62%). The most common reason for nonparticipation in the 24-week questionnaire assessments was health problems (34%) followed by work demands (22%). Nine women dropped out of the study, 2 women moved out of state, and 4 women were lost to contact during the 24 weeks of adoption. When comparing those with missing questionnaires with those who completed questionnaires at 24 weeks, there were no differences on individual characteristics (age, marital status, education, income, BMI, baseline depressive symptoms) or neighborhood characteristics (deterioration, crime). Further, 26 women did not return walking adherence data during the 24 weeks (3% ET vs. 18% MT, p > 0.01). Women with adherence data did not differ from those without adherence data on individual characteristics or neighborhood characteristics. To be conservative, women without reported adherence data were treated as not walking.
Rubin70 has demonstrated that imputing missing values will almost always produce more valid results than dropping the missing observations. In this study, substantial information on individual characteristics was available to help predict what missing values might be for depressive symptoms. One method of using this information efficiently is to use Rubin's propensity score method.70 The propensity method combines the most informative predictors for depressive symptoms in the database and then uses this index to guide the imputation of missing scores. We employed the multiple imputation procedure using PROC MI (SAS Inc., Cary, NC) with the propensity score method to impute the missing values for depressive symptoms.71,72 This data imputation was conducted prior to the main analysis. Because of the 38% missing data for 24-week depressive symptoms scores, a sensitivity analysis was done to determine the overall impact of missing data on study results. Study results were unchanged across levels of 10% to 40% missing data.
Data were summarized using descriptive statistics (e.g., means and standard deviations [SDs] for continuous variables; frequencies and percentages for categorical variables). Site differences were estimated using intraclass correlations for baseline depressive symptoms, age, income, and neighborhood characteristics (perceived and objective neighborhood deterioration and crime). The mean intraclass correlation was <0, indicating no significant site effects. As a consequence, data were analyzed without including a nesting term in the regression models. Ordinary least squares regression was the primary multivariate analytic strategy. Hypothesis 1 was addressed first by assessing for change in depressive symptoms between baseline and 24 weeks for the ET and MT groups using paired samples t tests and then by regressing depressive symptoms at 24 weeks on group/treatment assignment controlling for neighborhood characteristics, baseline depressive symptoms, and individual covariates (demographics, BMI).
To address hypothesis 2, 24-week depressive symptoms were regressed on walking adherence and neighborhood characteristics (perceived and objective neighborhood deterioration and crime) as well as baseline depressive symptoms and individual covariates. Interaction terms were added to test whether walking adherence moderated the effect of the neighborhood characteristics on depressive symptoms (hypothesis 3). Statistical significance was established at an alpha level of 0.05. All statistical analyses were performed using SAS 9.1 statistical software. Regression assumptions, including those for multicollinearity, were assessed and met.
Results
Participants
Of the study participants, 66.5% resided within the Chicago city limits. On average, the women were 48.5 years of age (SD 6.0), 41% were married, and 39% had a college education or above (Table 1). Mean annual household income was between $40,000 and $49,999 with 39.2% of the women having an annual household income of <$40,000. Overall, 45% of the women described their incomes as low and 52% as medium. The percent of land in the women's neighborhoods that was abandoned buildings or rubble lots ranged from 0 to 28.4% (M = 3.1%). The percent of homes that were vacant ranged from 0 to 24.9% (M = 7.8%). The mean baseline BMI for the entire sample was in the class 1 obesity category (30.0–34.4).73 The mean depressive symptom score at baseline was 11.3. Twenty-six percent of the women perceived abandoned houses or buildings to be either somewhat or a big problem in their neighborhood. The annual number of violent crime incidents in their neighborhoods ranged from 4 to >2000 (M = 703). This included from 0–37 homicides. The mean score on perceived neighborhood crimes was relatively low at 3.2, with a possible low of 0 and high of 14. There were no significant differences between the treatment groups (ET and MT) on any of the baseline individual or neighborhood characteristics. Thus, baseline equivalence was established. Across both treatment groups, the participants completed 38% of the prescribed walks, but adherence was higher in the ET group (45%) than in the MT group (29%).
Table 1.
Descriptive Statistics for Individual Characteristics, Neighborhood Characteristics, Baseline Depressive Symptoms, and Adherence to Walking
| Sample characteristics | Total sample (n = 278) |
|---|---|
| Individual characteristics | |
| Age, mean (SD) | 48.5 (6.0) |
| Marital status, % | |
| Married | 41 |
| Not married | 59 |
| Education, % | |
| High school/GED or less | 17 |
| Some college/vocational | 44 |
| College or above | 39 |
| Annual household income, mean (SD)a | 4.6 (2.7) |
| BMI, kg/m2, mean (SD) | 34.4 (7.2) |
| Baseline depressive symptoms | |
| CES-D, mean (SD) | 11.3 (7.9) |
| CES-D >16, % | 25 |
| Neighborhood characteristics | |
| Neighborhood deterioration | |
| Objective deteriorationb | |
| Percent abandoned buildings or rubble lots,b mean (SD) | 3.1 (3.7) |
| Percent vacant housing,b mean (SD) | 7.8 (4.5) |
| Perceived deterioration, % | |
| Somewhat or a big problem | 26 |
| Not a problem | 74 |
| Neighborhood crime | |
| Objective, total annual violent crime, mean (SD)b | 703 (559) |
| Perceived crime,c mean (SD) | 3.2 (3.4) |
| Walking adherence, mean (SD) | 38.0 (35.0) |
Annual household income was measured on an 11-point scale in $10,000 increments, ranging from <$10,000 (0) to >$100,000 (10).
Based on 1-mile radial buffers.
Score ranged from 0 to 14, with higher score indicating more perceived crime.
Study hypotheses
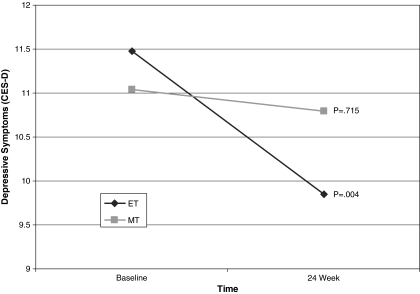
Paired samples t tests revealed a significant reduction in depressive symptoms from baseline to 24 weeks for the ET group, but not for the MT group (Fig. 1). When controlling in regression analysis for baseline depressive symptoms, however, individual characteristics, including baseline depressive symptoms, age, marital status, education, income and BMI group, and neighborhood characteristics, treatment was no longer significant.
FIG. 1.
Depressive symptoms by treatment group over time.
Table 2 shows regression of 24-week depressive symptoms on adherence to walking, baseline depressive symptoms, individual characteristics, and neighborhood characteristics. As expected, baseline depressive symptoms were positively associated with depressive symptoms at 24 weeks. No relationship was found between depressive symptoms and marital status or years of education. However, higher annual household income was predictive of lower depressive symptoms at 24 weeks. Consistent with our hypothesis, perceived neighborhood deterioration was positively associated with depressive symptoms, but, unexpectedly, objective neighborhood deterioration was negatively associated with depressive symptoms at 24 weeks. That is, women who perceived more neighborhood deterioration at baseline had higher depressive symptoms at 24 weeks, whereas higher objectively measured neighborhood deterioration was associated with lower depressive symptoms. Neither objective nor perceived neighborhood crime was associated with depressive symptoms. Consistent with our hypothesis, walking adherence had a significant negative association with depressive symptoms, indicating higher walking adherence was predictive of lower depressive symptoms at 24 weeks. The model accounted for 42% of the variance in depressive symptoms at 24 weeks (adjusted R2 = 40%). In a separate regression model testing interaction effects between the neighborhood environment characteristics and adherence to walking, none of the interaction terms were significant (data not shown), thus providing no evidence that walking adherence moderated the effect of the neighborhood characteristics on depressive symptoms. Regression results were consistent in models that tested deterioration and crime separately and that included objective neighborhood environmental measures (deterioration, crime) for ¼-mile radial buffers.
Table 2.
Regression of Depressive Symptoms at 24 Weeks on Baseline Depressive Symptoms, Individual Demographic Characteristics, Neighborhood Characteristics, and Walking Adherencea
| Predictor | Coefficient | SE | p value |
|---|---|---|---|
| Intercept | −1.976 | 4.088 | 0.629 |
| Baseline depressive symptoms | 0.520 | 0.051 | 0.000 |
| Demographics | |||
| Age | 0.043 | 0.064 | 0.503 |
| Marital status (married) | 0.328 | 0.916 | 0.721 |
| Education (reference: college degree) | |||
| High school or less | −0.455 | 1.216 | 0.708 |
| Technical school or some college | −1.020 | 0.854 | 0.233 |
| Income | −0.354 | 0.171 | 0.040 |
| Baseline BMI | 0.050 | 0.052 | 0.341 |
| Neighborhood deterioration | |||
| Objective deteriorationb | −1.543 | 0.565 | 0.007 |
| Perceived deterioration | 2.657 | 0.737 | 0.000 |
| Neighborhood crime | |||
| Objective crimeb | 0.000 | 0.001 | 0.973 |
| Perceived crime | 0.189 | 0.134 | 0.153 |
| Adherence to walking | −0.023 | 0.011 | 0.036 |
R2 = 0.42; adjusted R2 = 0.40.
Based on 1-mile radial buffers.
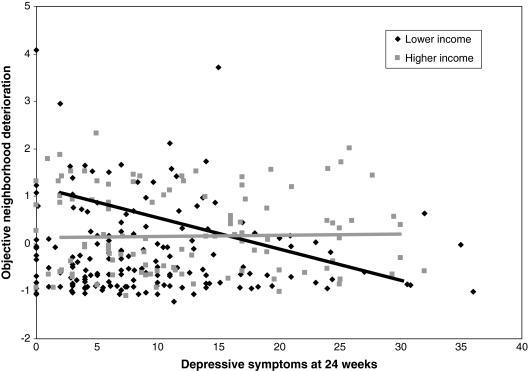
Secondary analyses
To further explore the unexpected negative association between objective neighborhood deterioration and depressive symptoms at 24 weeks, we conducted a stratified analysis by income level (Fig. 2). Using a mean split for income, we found a significant negative relationship between objective neighborhood deterioration and depressive symptoms in the low-income group (<$40,000). In the high-income group (>$40,000), however, there was no relationship between objective neighborhood deterioration and depressive symptoms.
FIG. 2.
Relationship between depressive symptoms and objective neighborhood deterioration stratified by income group.
Discussion
We believe we are among the first to examine the influence of adherence to physical activity and neighborhood characteristics on depressive symptoms within the context of a behavioral physical activity intervention. Further, it is among the first studies to look at a behavioral physical activity intervention and its impact on depressive symptoms in African American women. As expected, walking adherence was associated with lower levels of depressive symptoms at 24 weeks. We found that group assignment was significant in the bivariate analyses, with a significant decrease in depressive symptoms from baseline to 24 weeks for women in the ET group but not for women in the MT group. However, in regression analyses, group assignment was not associated with lower depressive symptoms at 24 weeks. Thus, like the findings of King et al.,40 our results suggest that staff support may not be the critical factor in the relationship between physical activity participation or adherence and positive psychological outcomes. Further, our study lends additional support to the only identified extant longitudinal observational study of African American women that found prior physical activity was associated with reduced odds of depressive symptoms.30
Controlling for the effects of baseline depressive symptoms, our results suggest that higher adherence to a walking intervention had independent effects on depressive symptoms. Adherence to walking, however, did not appear to buffer the deleterious effects of perceived neighborhood deterioration, as demonstrated by the lack of interaction between adherence and neighborhood characteristics. The stresses of living in neighborhoods perceived to be deteriorated may be so encompassing that physical activity does not distract the overall impact. Unexpectedly, objective neighborhood deterioration had a significant negative effect on depressive symptoms at 24 weeks: as objective neighborhood deterioration increased, there was a decrease in depressive symptoms. When we examined these results by income level, the negative association was found only in the lower-income women. This suggests that when compared with women with lower incomes living in more deteriorated neighborhoods (who seemed to be protected against depressive symptoms), those with comparable incomes living in less deteriorated neighborhoods seemed to be vulnerable. It is possible that lower-income women living in less deteriorated neighborhoods experience more stress in meeting daily needs, feel more isolated, or experience discrimination or relative deprivation. Another potential explanation is related to widespread housing relocations. Prior to and during the course of the study, sweeping changes in low-income housing availability were taking place in the neighborhoods where participants lived. Throughout Chicago's near west side, where one of the study sites was located, whole neighborhoods were transitioning to middle-income and high-income row housing, forcing out some lower-income residents. Elsewhere in the city, large high-rise housing projects were being demolished to make way for mixed low-income and middle-income low-rise housing. This neighborhood change also caused the relocation of large numbers of lower-income families, often to outlying suburban areas. In both cases, long-standing neighborhoods were irrevocably changed. To the extent that these housing changes affected our study participants, the low-income women who were forced to relocate may have experienced isolation and been exposed to discrimination, which has been associated with depressive symptoms in African American women.74 This finding warrants additional research.
Interestingly, the relationships between perceived and objective crime and depressive symptoms were nonsignificant. Unlike neighborhood deterioration, which is imminently present, problems with crime are dependent on occurrence. In follow-up focus groups, women indicated they were aware of high crime areas and times of the day and sought to avoid them. Although we did not examine experiences with crime, a possible explanation is that it is crime victimization or exposure to violence rather than crime per se that impacts depressive symptoms. In fact, a recent study found depressive/anxiety disorders were more likely among individuals who both lived in a high crime area and had witnessed violence in the past 12 months.19
Prior studies have predominantly used census administrative units (e.g., census tracts) to define neighborhood for objective measures.13 A strength of this study was the use of two different-sized radial buffers (1 mile and ¼ mile) around their homes to define participants' neighborhoods. Not only did this provide a more precise description of the area immediately surrounding the participants' homes, but it also allowed us to test the sensitivity of our results to alternative neighborhood definitions. Nonetheless, findings here suggest that crime within ¼ mile and 1 mile had similar effects on depressive symptoms.
Limitations
Despite the strengths of this study, there are limitations to the neighborhood measures that we identified earlier.67 They include the following: neighborhoods were not sampled to assure maximum variation in neighborhood characteristics, temporal inconsistency in the years for which data were available for the objective deterioration measure and the study period, and comparable data were lacking for objective crime for women residing in the urban vs. the suburban areas. With respect to the latter, the crime results were consistent when the sample was restricted to Chicago residents only.
Further, treatments were randomly assigned to sites rather than the accepted random assignment of women to conditions. In community-based research, we are sensitive to women who want to participate with their friends/family. We successfully established that the treatment groups were equivalent on key individual and neighborhood characteristics. With respect to the intervention, although we found that it was adherence to walking that had an influence on depressive symptoms, both the ET and MT included physical activity; thus, it is not possible to determine with certainty whether the reduction in depressive symptoms was due to physical activity alone or the social support provided in the ET. Further, we conservatively assumed women were not walking if no data were reported in any particular week. Some women who walked indicated that they did not record their walks or wear their HRM. As noted earlier, there is no reason to assume they differed by treatment group in this dynamic.54 Lastly, the percentage of women who participated in the 24-week measures (62%), although modest, was comparable to that reported in an earlier community-based studies (56%, 61.8%) with African American women of similar socioeconomic status.75,76
Conclusions
Despite limitations, although adherence to walking did not offset the adverse effect of perceptions of living in more deteriorated neighborhoods on depressive symptoms, our results suggest that physical activity interventions may have positive mental health benefits for midlife African American women. Special attention may need to be given to women with less financial means who reside in less deprived neighborhoods. Although these women may benefit from physical activity, future studies should address the mediating factors, such as social isolation and increased stress, that may place them at risk for depressive symptoms.
Acknowledgments
This work was supported by the National Institute of Nursing Research, National Institutes of Health (RO1 NRO4234), and Robert Wood Johnson Foundation Active Living Research. We thank the Multiethnic Advisory Board of Center for Reducing Risks in Vulnerable Populations NIH/NINR P30 NR09014. We also thank Dr. Louis Fogg, Rush University, for assistance in the statistical analyses.
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.Amercian Psychiatric Association. Diagnostic and statistical manual of mental disorders. DSM-IV-TR. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 2.U.S. Department of Health and Human Services. Mental health: A report of the Surgeon General. Rockville: U.S. Department of Health and Human Services; 1999. [Google Scholar]
- 3.Bromberger JT. Harlow S. Avis N. Kravitz HM. Cordal A. Racial/ethnic differences in the prevalence of depressive symptoms among middle-aged women: The Study of Women's Health Across the Nation (SWAN) Am J Public Health. 2004;94:1378–1385. doi: 10.2105/ajph.94.8.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scarinci IC. Robinson LA. Alfano CM. Zbikowski SM. Klesges RC. The relationship between socioeconomic status, ethnicity, and cigarette smoking in urban adolescents. Prev Med. 2002;34:171–178. doi: 10.1006/pmed.2001.0967. [DOI] [PubMed] [Google Scholar]
- 5.Blaine B. Does depression cause obesity? A meta-analysis of longitudinal studies of depression and weight control. J Health Psychol. 2008;13:1190–1197. doi: 10.1177/1359105308095977. [DOI] [PubMed] [Google Scholar]
- 6.Jargowsky PA. Poverty and place: Ghettos, barrios, and the American city. New York: Russell Sage Foundation; 1997. [Google Scholar]
- 7.Schulz A. Williams B. Isreal BA. Lempert LB. Racial and spatial relations as fundamental determinants of health in Detroit. Milbank Q. 2002;80:677–707. doi: 10.1111/1468-0009.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams DR. Collins C. Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Rep. 2001;116:404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dunn AL. Marcus BH. Kampert JB. Garcia ME. Kohl HW. Blair SN. Reduction in cardiovascular disease risk factors: 6-month results from Project Active. Prev Med. 1997;26:883–892. doi: 10.1006/pmed.1997.0218. [DOI] [PubMed] [Google Scholar]
- 10.Dunn AL. Marcus BH. Kampert JB. Garcia ME. Kohl HW. Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: A randomized trial. JAMA. 1999;281:327–334. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- 11.Teychenne M. Ball K. Salmon J. Physical activity and likelihood of depression in adults: A review. Prev Med. 2008;46:397–411. doi: 10.1016/j.ypmed.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 12.Kim D. Blues from the neighborhood? Neighborhood characteristics and depression. Epidemiol Rev. 2008;30:101–117. doi: 10.1093/epirev/mxn009. [DOI] [PubMed] [Google Scholar]
- 13.Mair C. Roux AV. Galea S. Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. J Epidemiol Community Health. 2008;62:940–946. doi: 10.1136/jech.2007.066605. [DOI] [PubMed] [Google Scholar]
- 14.Gary TL. Stark SA. LaVeist TA. Neighborhood characteristics and mental health among African Americans and whites living in a racially integrated urban community. Health Place. 2007;13:569–575. doi: 10.1016/j.healthplace.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 15.Schulz AJ. Israel BA. Zenk SN, et al. Psychosocial stress and social support as mediators of relationships between income, length of residence and depressive symptoms among African American women on Detroit's eastside. Soc Sci Med. 2006;62:510–522. doi: 10.1016/j.socscimed.2005.06.028. [DOI] [PubMed] [Google Scholar]
- 16.Latkin CA. Curry AD. Stressful neighborhoods and depression: A prospective study of the impact of neighborhood disorder. J Health Soc Behav. 2003;44:34–44. [PubMed] [Google Scholar]
- 17.Schootman M. Andresen EM. Wolinsky FD. Malmstrom TK. Miller JP. Miller DK. Neighborhood environment and the incidence of depressive symptoms among middle-aged African Americans. J Epidemiol Community Health. 2007;61:527–532. doi: 10.1136/jech.2006.050088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yen YC. Rebok GW. Yang MJ. Lung FW. A multilevel analysis of the influence of apolipoprotein E genotypes on depressive symptoms in late-life moderated by the environment. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32:479–486. doi: 10.1016/j.pnpbp.2007.09.023. [DOI] [PubMed] [Google Scholar]
- 19.Stockdale SE. Wells KB. Tang L. Belin TR. Zhang L. Sherbourne CD. The importance of social context: Neighborhood stressors, stress-buffering mechanisms, and alcohol, drug, and mental health disorders. Soc Sci Med. 2007;65:1867–1881. doi: 10.1016/j.socscimed.2007.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Curry AL. Latkin C. Davey-Rothwell M. Pathways to depression: The impact of neighborhood violent crime on inner-city residents in Baltimore, Marylalnd, USA. Soc Sci Med. 2008;67:23–30. doi: 10.1016/j.socscimed.2008.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kruger DJ. Reischl TM. Gee GC. Neighborhood social conditions mediate the accociation between physcial deterioration and mental health. Am J Community Psychol. 2007;40:261–271. doi: 10.1007/s10464-007-9139-7. [DOI] [PubMed] [Google Scholar]
- 22.Camacho TC. Roberts RE. Lazarus NB. Kaplan GA. Cohen RD. Physical activity and depression: Evidence from the Alameda County Study. Am J Epidemiol. 1991;134:220–231. doi: 10.1093/oxfordjournals.aje.a116074. [DOI] [PubMed] [Google Scholar]
- 23.Cooper-Patrick L. Ford DE. Mead LA. Chang PP. Klag MJ. Exercise and depression in midlife: A prospective study. Am J Public Health. 1997;87:670–673. doi: 10.2105/ajph.87.4.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Farmer ME. Locke BZ. Moscicki EK. Dannenberg AL. Larson DB. Radloff LS. Physical activity and depressive symptoms: The NHANES I epidemiologic follow-up study. Am J Epidemiol. 1988;128:1340–1351. doi: 10.1093/oxfordjournals.aje.a115087. [DOI] [PubMed] [Google Scholar]
- 25.Galper DI. Trivedi MH. Barlow CE. Dunn AL. Mampert JB. Inverse association between physical inactivity and mental health in men and women. Med Sci Sports Exerc. 2006;38:173–178. doi: 10.1249/01.mss.0000180883.32116.28. [DOI] [PubMed] [Google Scholar]
- 26.Goodwin RD. Association between physical activity and mental disorder among adults in the United States. Prev Med. 2003;36:698–703. doi: 10.1016/s0091-7435(03)00042-2. [DOI] [PubMed] [Google Scholar]
- 27.Mobily KE. Smit E. Rubenstein LM. Lemke JH. O'Hara MW. Wallace RB. Walking and depression in a cohort of older adults: The Iowa 65+ Rural Health Study. J Aging Phys Act. 1996;4:119–135. [Google Scholar]
- 28.Kritz-Silverstein D. Barrett-Connor E. Corbeau C. Cross-sectional and prospective study of exercise and depressed mood in the elderly. Am J Epidemiol. 2001;153:596–603. doi: 10.1093/aje/153.6.596. [DOI] [PubMed] [Google Scholar]
- 29.Strawbridge WJ. Deleger S. Roberts RE. Kaplan G. Physical activity reduces the risk of subsequent depression for older adults. Am J Epidemiol. 2002;156:328–334. doi: 10.1093/aje/kwf047. [DOI] [PubMed] [Google Scholar]
- 30.Wise LA. Adams-Campbell LL. Palmer JR. Rosenberg L. Leisure time physical activity in relation to depressive symptoms in the Black Women's Health Study. Ann Behav Med. 2006;32:68–76. doi: 10.1207/s15324796abm3201_8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Andersen R. Wadden TA. Bartlett SJ. Zemel B. Verde TJ. Franckowaiak SC. Effects of lifestyle activity vs structured aerobic exercise in obese women: A randomized trial. JAMA. 1999;281:335–340. doi: 10.1001/jama.281.4.335. [DOI] [PubMed] [Google Scholar]
- 32.Blumenthal JA. Emery CF. Madden DJ, et al. Cardiovascular and behavioral effects of aerobic exercise training in healthy older men and women. J Gerontol. 1989;44:M147–157. doi: 10.1093/geronj/44.5.m147. [DOI] [PubMed] [Google Scholar]
- 33.Brown DR. Wang Y. Ward A, et al. Chronic psychological effects of exercise and exercise plus cognitive strategies. Med Sci Sports Exerc. 1995;27:765–775. [PubMed] [Google Scholar]
- 34.Cramer SR. Nieman DC. Lee JW. The effects of moderate exercise training on psychological well-being and mood state in women. J Psychosom Res. 1991;35:437–449. doi: 10.1016/0022-3999(91)90039-q. [DOI] [PubMed] [Google Scholar]
- 35.DiLorenzo TM. Bargman EP. Stucky-Ropp R. Brassington GS. Frensch PA. LaFontaine T. Long-term effects of aerobic exercise on psychological outcomes. Prev Med. 1999;28:75–85. doi: 10.1006/pmed.1998.0385. [DOI] [PubMed] [Google Scholar]
- 36.Dunn AL. Trivedi MH. Kampert JB. Clark CG. Chambliss HO. Exercise treatment for depression: Efficacy and dose response. Am J Prev Med. 2005;28:1–8. doi: 10.1016/j.amepre.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 37.Gitlin L. Lawton MP. Windsor-Landsberg LA. Kleban MH. Sands LP. Posner JG. In search of psychological benefits exercise in healthy older adults. J Aging Health. 1992;4:174–192. [Google Scholar]
- 38.Fremont J. Craighead L. Aerobic exercise and cognitive therapy in the treatment of dysphoric moods. Cognitive Ther Res. 1987;11:241–251. [Google Scholar]
- 39.King AC. Taylor CB. Haskell WL. DeBusk RF. Influence of regular aerobic exercise on psychological health: A randomized, controlled trial of healthy middle-aged adults. Health Psychol. 1989;8:305–324. doi: 10.1037//0278-6133.8.3.305. [DOI] [PubMed] [Google Scholar]
- 40.King AC. Taylor CB. Haskell WL. Effects of differing intensities and formats of 12 months of exercise training on psychological outcomes in older adults. Health Psychol. 1993;12:292–300. doi: 10.1037//0278-6133.12.4.292. [DOI] [PubMed] [Google Scholar]
- 41.Motl RW. Konopack JF. McAuley E. Elavsky S. Jerome GJ. Marquez DX. Depressive symptoms among older adults: Long-term reduction after a physical activity intervention. J Behav Med. 2005;28:385–394. doi: 10.1007/s10865-005-9005-5. [DOI] [PubMed] [Google Scholar]
- 42.Nieman DC. Custer WF. Butterworth DE. Utter AC. Henson DA. Psychological response to exercise training and/or energy restriction in obese women. J Psychosom Res. 2000;48:23–29. doi: 10.1016/s0022-3999(99)00066-5. [DOI] [PubMed] [Google Scholar]
- 43.Norvell N. Martin D. Salamon A. Psychological and physiological benefits of passive and aerobic exercise in sedentary middle-aged women. J Nerv Ment Dis. 1991;179:573–574. doi: 10.1097/00005053-199109000-00011. [DOI] [PubMed] [Google Scholar]
- 44.Roth DL. Holmes DS. Influence of aerobic exercise training and relaxation training on physical and psychologic health following stressful life events. Psychosom Med. 1987;49:355–365. doi: 10.1097/00006842-198707000-00004. [DOI] [PubMed] [Google Scholar]
- 45.West J. Otte C. Geher K. Johnson J. Mohr DC. Effects of Hatha yoga and African dance on perceived stress, affect, and salivary cortisol. Ann Behav Med. 2004;28:114–118. doi: 10.1207/s15324796abm2802_6. [DOI] [PubMed] [Google Scholar]
- 46.Wilbur J. Chandler P. Dancy B. Choi J. Plonczynski D. Environmental, policy and cultural factors related to physical activity in urban, African American Women. Women Health. 2002;36:17–28. doi: 10.1300/J013v36n02_02. [DOI] [PubMed] [Google Scholar]
- 47.Wilcox S. Bopp M. Oberrecht L. Kammermann SK. McElmurray CT. Psychosocial and perceived environmental correlates of physical activity in rural and older African American and white women. J Gerontol B Psychol Sci Soc Sci. 2003;58B:P329–P337. doi: 10.1093/geronb/58.6.p329. [DOI] [PubMed] [Google Scholar]
- 48.Taylor WC. Sallis JF. Lees E, et al. Changing social and built environments to promote physical activity: Recommendations from low income, urban women. J Phys Act Health. 2007;4:54–65. doi: 10.1123/jpah.4.1.54. [DOI] [PubMed] [Google Scholar]
- 49.Ball K. Bauman A. Leslie E. Owen N. Perceived environmental aesthetics and convenience and company are associated with walking for exercise among Australian adults. Prev Med. 2001;33:434–440. doi: 10.1006/pmed.2001.0912. [DOI] [PubMed] [Google Scholar]
- 50.Brownson RC. Baker EA. Housemann RA. Brennan LK. Bacak SJ. Environmental and policy determinants of physical activity in the United States. Am J Public Health. 2001;91:1995–2003. doi: 10.2105/ajph.91.12.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Giles-Corti B. Donovan RJ. The relative influence of individual, social, and physical environment determinants of physical activity. Soc Sci Med. 2002;54:1793–1812. doi: 10.1016/s0277-9536(01)00150-2. [DOI] [PubMed] [Google Scholar]
- 52.Owen N. Humpel N. Leslie E. Bauman A. Sallis JF. Understanding environmental influences on walking: Review and research agenda. Am J Prev Med. 2004;27:67–76. doi: 10.1016/j.amepre.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 53.Brownson RC. Chang JC. Eyler AA, et al. Measuring the environment for friendliness toward physical activity: A comparison of the reliability of 3 questionnaires. Am J Public Health. 2004;94:473–483. doi: 10.2105/ajph.94.3.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wilbur J. McDevitt J. Wang E, et al. Outcomes of a home-based walking program for African-American women. Am J Health Promot. 2008;22:307–317. doi: 10.4278/ajhp.22.5.307. [DOI] [PubMed] [Google Scholar]
- 55.Kouvelis A. Harper D. Thomas S. Community Area Health Inventory 1992–2002. Chicago, IL: Chicago Department of Public Health Epidemiology. 2004:Program. [Google Scholar]
- 56.Wilbur J. McDevitt J. Wang E, et al. Recruitment of African American women to a walking program: Eligibility, ineligibility and attrition during screening. Res Nurs Health. 2006;29:176–189. doi: 10.1002/nur.20136. [DOI] [PubMed] [Google Scholar]
- 57.Glanz B. Rimer B. Lewis FM. Health behavior and health education: Theory, research, and practice. 3rd. Jossey-Bass; San Francisco, CA: 2002. [Google Scholar]
- 58.King AC. Haskell WL. Young DR. Oka RK. Stefanick ML. Long-term effects of varying intensities and formats of physical activity on participation rates, fitness, and lipoproteins in men and women aged 50 to 65 years. Circulation. 1995;91:2596–2604. doi: 10.1161/01.cir.91.10.2596. [DOI] [PubMed] [Google Scholar]
- 59.U.S. Department of Health and Human Services. Healthy people 2010 objectives. Washington, DC: Office of Disease Prevention and Health Promotion. 2000.
- 60.Ruuskanen JM. Ruopilla I. Physical activity and psychological well-being among people aged 65 to 84 years. Age Ageing. 1995;24:292–296. doi: 10.1093/ageing/24.4.292. [DOI] [PubMed] [Google Scholar]
- 61.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 62.Jones-Webb RJ. Snowden LR. Symptoms of depression among blacks and whites. Am J Public Health. 1993;83:240–244. doi: 10.2105/ajph.83.2.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Auchincloss AH. Roux AV. Brown DG. Erdmann CA. Bertoni AG. Neighborhood resources for physical activity and health foods and their association with insulin resistance. Epidemiology. 2008;19:146–157. doi: 10.1097/EDE.0b013e31815c480. [DOI] [PubMed] [Google Scholar]
- 64.Transportation Research Board. Does the built environment influence physical activity? Examining the evidence (Special Report 282) Washington, DC: Institute of Medicine; 2005. [Google Scholar]
- 65.Northeastern Illinois Planning Commission/Chicago Metropolitan Agency for Planning (NIPC/CMAP) 2001 land use inventory for Northeastern Illinois v 0.9 [electronic GIS shapefile] Chicago IL: 2005. [Google Scholar]
- 66.Elder G. Eccles J. Ardelt M. Lord S. Inner-city parents under economic pressure: Perspective on strategies of parenting. J Marriage Fam. 1995;57:771–784. [Google Scholar]
- 67.Zenk S. Wilbur J. Wang E, et al. Neighborhood environment and adherence to a walking intervention in African American women. Health Educ Behav. 2009;36:167–181. doi: 10.1177/1090198108321249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Illinois State Police. Crime in Illinois: Illinois uniform crime reports. www.isp.state.il.us/crime/ucrhome.cfm. www.isp.state.il.us/crime/ucrhome.cfm August 2006.
- 69.American College of Sports Medicine. ACSM's guidelines for exercise testing and prescription. 7th. Philadelphia: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 70.Rubin DB. Multiple imputation for nonresponse in survey research. New York: John Wiley & Sons; 1987. [Google Scholar]
- 71.Schafer JL. Analysis of incomplete multivariate data. New York: Chapman and Hall; 1997. [Google Scholar]
- 72.King A. Ahn D. Rejeski W. Marcus B. Dunn A. Sallis J. Identifying subgroups that succeed or fail with three levels of physical activity intervention: The Activity Counseling Trial. Health Psychol. 2006;24:336–347. doi: 10.1037/0278-6133.25.3.336. [DOI] [PubMed] [Google Scholar]
- 73.National Heart, Lung, Blood Institute. Clinical guidelines on the identification, evaluation and treatment of overweight and obesity in adults: The evidence report. Bethesda, MD: National Heart, Lung and Blood Institute; 1998. [Google Scholar]
- 74.Schulz AJ. Gravlee CC. Williams DR. Israel BA. Mentz G. Rowe Z. Discrimination, symptoms of depression, and self-rated health among African American women in Detroit: Results from a longitudinal analysis. Am J Public Health. 2006;96:1265–1270. doi: 10.2105/AJPH.2005.064543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yancey A. McCarthy W. Harrison G. Wong W. Siegel J. Leslie J. Challenges in improving fitness: Results of a community-based, randomized, controlled lifestyle change intervention. J Womens Health. 2006;15:412–428. doi: 10.1089/jwh.2006.15.412. [DOI] [PubMed] [Google Scholar]
- 76.Yanke L. Becker DM. Moy T. Gittelsohn J. Koffman DM. Project Joy: Faith-based cardiovascular health promotion for African American women. Public Health Rep. 2001;116:68–81. doi: 10.1093/phr/116.S1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]