Abstract
Objective
This research sought to describe associations among parity, breastfeeding, and adult obesity in black and white women in the southeastern United States.
Methods
Cross-sectional data from 7,986 white women and 23,198 black women (age 40–79 years) living in the southeastern United States and enrolled in the Southern Community Cohort Study during 2002–2006 were used to examine self-reported body mass index (BMI) and weight change since age 21 in association with parity and breastfeeding. Multiple linear regression and logistic regression with adjustment for demographic and lifestyle factors were used.
Results
At all levels of parity and breastfeeding, black women had higher BMI and weight gain since age 21 than white women. Compared to nulliparity, five or more live births was associated with increased odds of obesity in white women (odds ratio [OR] = 1.37, 95% confidence interval [CI] = 1.08–1.74) and, to a lesser extent, in black women (OR = 1.22, 95% CI = 1.07–1.38). In white women, breastfeeding for more than 12 months compared to none was associated with decreased odds of obesity (OR = 0.68, 95% CI = 0.56–0.82), whereas in black women, no association between obesity and breastfeeding was seen.
Conclusions
The associations between childbearing factors and measures of adult obesity appear to be larger in white women compared to black women but relatively small overall. However, when considered as part of the constellation of factors that lead to obesity, even these small associations may be important in an overall obesity prevention strategy.
Introduction
The prevalence of obesity in the United States has rapidly increased in recent decades. According to the National Health and Nutrition Examination Survey (NHANES), the prevalence of obesity (defined as body mass index [BMI] ≥ 30 kg/m2) among U.S. women has more than doubled, growing from 16% in 1971–1974 to 33% in 2003–2004.1,2 The prevalence rates of obesity (BMI > 30 kg/m2) and overweight (BMI 25–29.9 kg/m2) vary by race, particularly among women. In 2003–2004, 54% of black women were obese compared to 30% of white women, and 82% of black women were overweight compared to 54% of white women.1
Overweight and obesity in women may be associated with parity and breastfeeding. Parity has generally been found to be positively associated with body size and other weight-related conditions such as metabolic syndrome, although study results vary regarding the parity threshold linked to weight gain, the magnitude of the association, and differences by race.3–16 Fewer studies have examined the relationship between childbearing and obesity among black women.10,12–14 The literature examining the effects of breastfeeding on obesity among mothers is inconclusive for both black and white women.17–19
Considerable evidence shows that obesity in women is associated with increased risk of several high burden diseases, including cancer of the breast (postmenopausal), endometrium, ovary and colon,20–22 as well as cardiovascular disease and stroke.23 Given the known racial differences in the prevalence of obesity, a better understanding of the role that childbearing plays in the development of obesity in both black and white women may provide valuable avenues for public health prevention strategies to reduce obesity and its negative health sequelae. Thus, the goal of the current analysis was to determine whether obesity was associated with parity or breastfeeding and whether these associations differed between black and white women.
Methods
The SCCS is an on-going prospective epidemiologic cohort study in the southeastern United States focused on racial disparities in cancer incidence and mortality.24 Participants have been enrolled primarily in-person at Community Health Centers (CHCs) in the states of Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Virginia, and West Virginia, as well as via mailed recruitment activities in the same geographical area. CHCs are government-funded health care facilities that provide basic health services primarily to low-income individuals.25 Participants were enrolled by approaching people entering the CHCs (patients, persons accompanying patients, etc.) and screening them for eligibility and interest in study participation. Participants were required to be between the ages of 40 and 79, to speak English, and to not have undergone treatment for cancer (excluding non-melanoma skin cancer) within the past year. For the present cross-sectional analysis, we considered all females who enrolled in-person at one of 48 CHCs between March 2002 and December 2006, and self-reported their race as either white or black (N = 31,502).
Trained interviewers conducted comprehensive, in-person, baseline interviews with all participants at the CHC at the time of study enrollment. The baseline interview included several aspects of health and behavior, including current height and weight, weight at age 21, personal and family medical history, reproductive history, diet, physical activity, tobacco use, health care utilization, and demographic characteristics. All women were asked for their age at their first menstrual period, whether they had ever been pregnant, and whether they had been through menopause or if their menstrual periods had stopped for at least 6 months. Women who reported ever being pregnant were asked how many times they had been pregnant, how many pregnancies resulted in a live birth, and the total number of months (counting all pregnancies) that they breastfed.
Women were excluded from this analysis if current height or weight (N = 318) was missing from the baseline SCCS interview, leaving 31,184 women for study. The primary outcome of interest was BMI calculated as self-reported weight in kilograms, divided by the square of self-reported height in meters and treated continuously. A dichotomous measure of obesity was calculated by categorizing women as obese (BMI ≥ 30 kg/m2) or non-obese (BMI < 30 kg/m2). Adult weight change was calculated as self-reported weight at the SCCS baseline interview, minus self-reported weight at age 21. BMI at age 21 was calculated using weight at age 21 and current height from the baseline SCCS interview. Primary exposures of interest included parity (treated both continuously and categorized as nulliparous, 1, 2, 3, 4, and 5+) and total months of breastfeeding (treated both continuously and categorized as none, 1–3, 4–6, 7–12, and >12).
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research. The study was approved by institutional review boards at Vanderbilt University and Meharry Medical College.
Statistical analysis
Chi-square tests and t-tests were used to compare differences in categorical and continuous factors, respectively, between race groups. Multiple linear regression models were used to examine associations between predictors of interest (parity and breastfeeding) and continuous BMI and weight change since age 21. Logistic regression models were used to examine predictors of dichotomously categorized obesity. Models for parity included all 31,184 eligible women, while models for breastfeeding excluded nulliparous women. A list of a priori confounders was generated from the literature, and potential confounders were categorized as shown in Table 1. All models presented here contained the entire set of a priori confounders. Models containing only a subset of the covariates determined using backwards model selection and a >10% change-in-estimate criterion for the primary exposures produced very similar effect estimates and are not presented. The likelihood ratio test (LRT) was used to evaluate whether race was an effect modifier by comparing −2-log-likelihood values from models with and without interaction terms for race and the primary exposures (parity and breast-feeding). When race was found to be an important modifier (defined as an LRT p-value < 0.05 a priori), models were stratified by race.
Table 1.
Demographic and Lifestyle Characteristics among 31,184 White and Black Women Enrolled in the Southern Community Cohort Study
| |
White (N = 7,986) |
Black (N = 23,198) |
||
|---|---|---|---|---|
| Characteristic | N | % | N | % |
| Age at baseline interview (years) | ||||
| 40–44 | 1627 | 20.4 | 6039 | 26.0 |
| 45–49 | 1726 | 21.6 | 5465 | 23.6 |
| 50–54 | 1434 | 18.0 | 4502 | 19.4 |
| 55–59 | 1250 | 15.7 | 2956 | 12.7 |
| 60–64 | 956 | 12.0 | 1938 | 8.4 |
| 65–69 | 515 | 6.5 | 1185 | 5.1 |
| 70–74 | 298 | 3.7 | 722 | 3.1 |
| 75–79 | 180 | 2.3 | 391 | 1.7 |
| Menopausal status | ||||
| Pre | 2002 | 25.1 | 8608 | 37.1 |
| Post | 5954 | 74.6 | 14516 | 62.6 |
| Missing | 30 | 0.4 | 74 | 0.3 |
| Yearly household income | ||||
| <$15,000 | 4636 | 58.1 | 14144 | 61.0 |
| $15,000–24,999 | 1615 | 20.2 | 5435 | 23.4 |
| $25,000–49,999 | 1013 | 12.7 | 2551 | 11.0 |
| $50,000+ | 629 | 7.9 | 774 | 3.3 |
| Missing | 93 | 1.2 | 294 | 1.3 |
| Educational attainment | ||||
| <9 years | 746 | 9.3 | 1784 | 7.7 |
| 9–11 years | 1656 | 20.7 | 5624 | 24.2 |
| High school | 3230 | 40.5 | 9121 | 39.3 |
| Some college or junior college | 1518 | 19.0 | 4583 | 19.8 |
| College graduate and beyond | 833 | 10.4 | 2075 | 8.9 |
| Missing | 3 | 0.0 | 11 | 0.1 |
| Marital status | ||||
| Married/living as married | 3401 | 42.6 | 6099 | 26.3 |
| Separated/divorced | 2827 | 35.4 | 7951 | 34.3 |
| Widowed | 1088 | 13.6 | 3355 | 14.5 |
| Single, never been married | 661 | 8.3 | 5765 | 24.9 |
| Missing | 9 | 0.1 | 28 | 0.1 |
| Occupational status | ||||
| Currently working | 2546 | 31.9 | 8878 | 38.3 |
| Not currently working | 5292 | 66.3 | 13801 | 59.5 |
| Missing | 148 | 1.9 | 519 | 2.2 |
| Cigarette smoking | ||||
| Current | 3200 | 40.1 | 7948 | 34.3 |
| Former | 1947 | 24.4 | 4481 | 19.3 |
| Never | 2821 | 35.3 | 10721 | 46.2 |
| Missing | 18 | 0.2 | 48 | 0.2 |
| Alcohol consumption in past year (drinks per day) | ||||
| None | 4750 | 59.5 | 12493 | 53.9 |
| <1 | 2578 | 32.3 | 7347 | 31.7 |
| 1+ | 555 | 7.0 | 3062 | 13.2 |
| Missing | 103 | 1.3 | 296 | 1.3 |
| Fruit/vegetable servings (daily) | ||||
| None | 474 | 5.9 | 1300 | 5.6 |
| 1–2 | 3311 | 41.5 | 7798 | 33.6 |
| 3–5 | 3426 | 42.9 | 10647 | 45.9 |
| >5 | 704 | 8.8 | 3234 | 13.9 |
| Missing | 71 | 0.9 | 219 | 0.9 |
| Depression (based on CES-D)a | ||||
| Yes | 3858 | 48.3 | 9797 | 42.2 |
| No | 4073 | 51.0 | 13256 | 57.1 |
| Missing | 55 | 0.7 | 145 | 0.6 |
| Total physical activity (MET-hours/day)b | ||||
| 0–9.29 | 1985 | 24.9 | 5065 | 21.8 |
| 9.3–16.89 | 2188 | 27.4 | 6182 | 26.7 |
| 16.9–27.79 | 1882 | 23.6 | 5921 | 25.5 |
| 27.8+ | 1858 | 23.3 | 5760 | 24.8 |
| Missing | 73 | 0.9 | 270 | 1.2 |
| Oral contraceptive use | ||||
| None | 2425 | 30.4 | 7481 | 32.3 |
| <1 year | 954 | 12.0 | 2654 | 11.4 |
| 1–4 years | 1985 | 24.9 | 6160 | 26.6 |
| 5–9 years | 1157 | 14.5 | 3141 | 13.5 |
| 10+ years | 1369 | 17.1 | 3309 | 14.3 |
| Missing | 96 | 1.2 | 453 | 2.0 |
| Age at menarche (years) | ||||
| ≤11 | 1900 | 23.8 | 4619 | 19.9 |
| 12 | 2087 | 26.1 | 5691 | 24.5 |
| 13 | 1966 | 24.6 | 5214 | 22.5 |
| 14 | 909 | 11.4 | 2846 | 12.3 |
| 15+ | 1052 | 13.2 | 4551 | 19.6 |
| Missing | 72 | 0.9 | 277 | 1.2 |
| Age at first birthc (years) | ||||
| <20 | 3390 | 48.1 | 12387 | 59.0 |
| 20–24 | 2440 | 34.6 | 5974 | 28.5 |
| 25–29 | 797 | 11.3 | 1706 | 8.1 |
| 30–34 | 286 | 4.1 | 582 | 2.8 |
| 35–39 | 104 | 1.5 | 245 | 1.2 |
| 40+ | 27 | 0.4 | 48 | 0.2 |
| Missing | 6 | 0.1 | 47 | 0.2 |
| Age at last birthc (years) | ||||
| <20 | 516 | 7.3 | 1862 | 8.9 |
| 20–24 | 2043 | 29.0 | 4740 | 22.6 |
| 25–29 | 2123 | 0.1 | 5703 | 27.2 |
| 30–34 | 1402 | 19.9 | 4414 | 21.0 |
| 35–39 | 723 | 10.3 | 3139 | 15.0 |
| 40+ | 223 | 3.2 | 941 | 4.5 |
| Missing | 20 | 0.3 | 190 | 0.9 |
| Parity | ||||
| Nulliparous | 907 | 11.4 | 2144 | 9.2 |
| 1 | 1262 | 15.8 | 3127 | 13.5 |
| 2 | 2389 | 29.9 | 5121 | 22.1 |
| 3 | 1708 | 21.4 | 4896 | 21.1 |
| 4 | 891 | 11.2 | 3270 | 14.1 |
| 5+ | 800 | 10.0 | 4572 | 19.7 |
| Missing | 29 | 0.4 | 68 | 0.3 |
| Breastfeeding (months)c | ||||
| None | 4479 | 63.5 | 14416 | 68.7 |
| 1–3 | 856 | 12.1 | 1860 | 8.9 |
| 4–6 | 469 | 6.7 | 1225 | 5.8 |
| 7–12 | 515 | 7.3 | 1242 | 5.9 |
| >12 | 719 | 10.2 | 2100 | 10.0 |
| Missing | 12 | 0.2 | 146 | 0.7 |
| Body mass index at baseline interview (kg/m2) | ||||
| <18.5 | 155 | 1.9 | 245 | 1.1 |
| 18.5–24.9 | 1853 | 23.2 | 3742 | 16.1 |
| 25.0–29.9 | 2073 | 26.0 | 5915 | 25.5 |
| 30.0–34.9 | 1787 | 22.4 | 5798 | 25.0 |
| 35.0–39.9 | 1058 | 13.3 | 3798 | 16.4 |
| 40.0+ | 1060 | 13.3 | 3700 | 16.0 |
| Body mass index at age 21 (kg/m2) | ||||
| <18.5 | 1263 | 15.8 | 3119 | 13.5 |
| 18.5–24.9 | 4945 | 61.9 | 13626 | 58.7 |
| 25.0–29.9 | 901 | 11.3 | 3469 | 15.0 |
| 30.0–34.9 | 435 | 5.5 | 1256 | 5.4 |
| 35.0–39.9 | 171 | 2.1 | 413 | 1.8 |
| 40.0+ | 153 | 1.9 | 320 | 1.4 |
| Missing | 118 | 1.5 | 995 | 4.3 |
| Weight change since age 21 (kg) | ||||
| <0 | 804 | 10.1 | 1883 | 8.1 |
| 0–9.9 | 1245 | 15.6 | 2566 | 11.1 |
| 10–19.9 | 1858 | 23.3 | 4835 | 20.8 |
| 20–29.9 | 1723 | 21.6 | 5058 | 21.8 |
| 30–39.9 | 1034 | 13.0 | 3395 | 14.6 |
| 40+ | 1204 | 15.1 | 4466 | 19.3 |
| Missing | 118 | 1.5 | 995 | 4.3 |
Based on the 10-question Center for Epidemiologic Studies Depression scale (scale 0–30, depression categorized as No if score <10 and Yes if score ≥10).
Sum of household and occupational work plus moderate and vigorous sports.
Among women with one or more live births.
To assess the potential for bias due to clustering of participants who enrolled in the SCCS at the same CHC compared to participants who enrolled at different CHCs, models that used generalized estimating equations (GEE) to produce standard errors and test statistics were compared to models that did not use GEE. In the models that used GEE, an exchangeable working correlation structure was assumed, meaning that a common covariance was assumed among all participants enrolled in a single CHC. The standard errors produced in the models using GEE were negligibly different from those produced in models without the use of GEE. Thus, the results presented here are from models that do not use GEE.
SAS/STAT software, Version 9.1 of the SAS System for Windows (SAS Institute Inc., Cary, NC), was used for all analyses.
Results
Demographic and lifestyle factors obtained from the baseline SCCS interview in this study of low-income black and white women from the southeast are presented in Table 1. Women were on average in their early 50s when they enrolled in the SCCS (range, 40–79 years). More than half of the women had a household income less than $15,000 in the past year (58% for white and 61% for black women). Education levels were low, with 71% each of white and black women having a high school education or less. Black women were significantly more likely to be obese (BMI ≥ 30 kg/m2) than white women at the baseline SCCS interview (57% vs. 49%, χ2 p-value < 0.0001). There was, however, little difference in the prevalence of obesity at age 21 between black and white women (9% vs. 10%, respectively). Mean weight gain between age 21 and the baseline SCCS interview was higher among black women than white women even after adjustment for age (age-adjusted mean weight gain for black women= 25.1 kg vs. 21.6 kg for white women, p < 0.0001). Black women had on average 3.1 live births compared to 2.4 for white women and were twice as likely to have five or more live births (20% vs. 10.0%). Overall, approximately 11% of the white women and 9% of the black women included in this analysis were nulliparous. Among women with at least one live birth, black women were more likely to have never breastfed than white women (69% vs. 64%), but among the women who did breastfeed, the average number of months spent breastfeeding per birth was similar in white women (1.6 months) compared to black women (1.4 months).
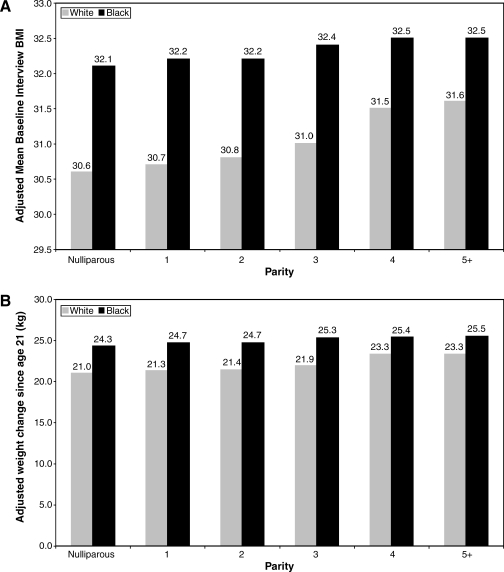
As shown in Table 2, an increase in parity of one live birth was associated with a small but statistically significant increase in BMI among white women (β = 0.20, p < 0.001). The effect of parity on BMI was negligible for black women, with an increase of one live birth associated with an increase in BMI of only 0.06 kg/m2. These associations translated to a 1 kg/m2 difference in the adjusted mean BMI values between nulliparous women and women with five or more births (30.6 vs. 31.6 kg/m2) for white women and a 0.4 kg/m2 difference in the adjusted means for black women (32.1 vs. 32.5 kg/m2) at these extremes of parity (Fig. 1A). An increase of one in parity was associated with a 0.45 kg increase in weight gain since age 21 for white women but only 0.17 kg for black women (Table 2). Among white women, the difference in the adjusted mean weight change between nulliparous women and women with five or more live births was 2.3 kg, while for black women the difference was just 1.2 kg (Fig. 1B). Both higher BMI values and greater weight change since age 21 were observed among black women at all levels of parity. For example, the adjusted mean weight gain since age 21 among nulliparous white women was 21.0 kg compared to 24.3 kg among nulliparous black women (Fig. 1B).
Table 2.
Associations between Current Body Mass Index (BMI) (kg/m2) and Weight Change since Age 21 (kg) and Parity and Breastfeeding from Race-Stratified Multivariate Linear Regression Models of Women in the Southern Community Cohort Study
| |
All women |
White women |
Black women |
|||
|---|---|---|---|---|---|---|
| Exposure | Beta ± SE | p-value | Beta ± SE | p-value | Beta ± SE | p-value |
| Parity (live births)a | ||||||
| Outcome: BMI (kg/m2) | 0.12 ± 0.02 | <0.0001 | 0.20 ± 0.05 | 0.0001 | 0.06 ± 0.02 | 0.02 |
| Outcome: Weight change since age 21 (kg) | 0.32 ± 0.06 | <0.0001 | 0.45 ± 0.14 | 0.0008 | 0.17 ± 0.06 | 0.008 |
| Breastfeeding (total months)a,b | ||||||
| Outcome: BMI (kg/m2) | −0.003 ± 0.003 | 0.26 | −0.02 ± 0.007 | 0.008 | 0.0002 ± 0.003 | 0.94 |
| Outcome: Weight change since age 21 (kg) | 0.009 ± 0.09 | 0.92 | −0.22 ± 0.17 | 0.20 | 0.17 ± 0.10 | 0.11 |
All models adjusted for age, BMI at age 21, education, household income, menopausal status, marital status, current occupational status, smoking status, alcohol consumption, fruit and vegetable consumption, total MET-hrs/day of physical activity, depression based on CESD, use of oral contraceptives, and age of menarche in categories as shown in Table 1.
Models with breastfeeding as the outcome are additionally adjusted for number of live births.
FIG. 1.
Multivariate adjusted means for current body mass index (BMI; A) and weight change since age 21 (B) by categories of parity among white and black women, including adjustment for factors listed in Table 3.
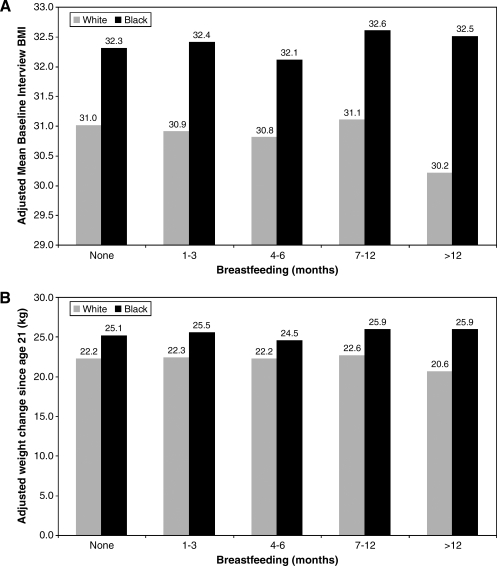
Breastfeeding was found to be significantly associated with BMI but not weight change since age 21 in white women only (Table 2). The magnitude of the association, however, was small; for each month of breastfeeding, BMI decreased by 0.02 kg/m2 (p = 0.008), resulting in a tangible decrease in BMI only for women who breastfed for a total of more than 12 months compared to no breastfeeding (change of 0.8 kg/m2; Fig. 2A).
FIG. 2.
Multivariate adjusted means for current body mass index (BMI; A) and weight change since age 21 (B) by categories of breastfeeding among parous white and black women, including adjustment for factors listed in Table 3.
When body size was examined dichotomously (Table 3), increasing parity was associated with increased odds of obesity among both black and white women. The effect was somewhat stronger for the highest levels of parity among white compared to black women (parity 5+: odds ratio [OR] = 1.37, 95% confidence interval [CI] 1.08–1.74 for white women vs. OR = 1.22, 95% CI 1.07–1.38 for black women). To assess the potential for cohort effects, models were stratified by 10-year age categories. Increasing parity was generally associated with increased odds of obesity within each age category (data not shown). Similarly, when the data were stratified by BMI at age 21, increasing parity was again generally associated with increasing odds of obesity (data not shown).
Table 3.
Odds Ratios from Multivariatea Logistic Regression Models for the Effects of Parity and Breastfeeding on Obesity (BMI ≥30 kg/m2) among women in the Southern Community Cohort Study
| |
Multivariate |
|||||
|---|---|---|---|---|---|---|
| |
All women |
White women |
Black women |
|||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Parity | ||||||
| Nulliparous | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference |
| 1 | 1.12 | 1.00–1.25 | 1.06 | 0.86–1.31 | 1.12 | 0.98–1.27 |
| 2 | 1.09 | 0.99–1.21 | 1.10 | 0.90–1.33 | 1.08 | 0.96–1.22 |
| 3 | 1.16 | 1.05–1.29 | 1.10 | 0.90–1.35 | 1.16 | 1.03–1.31 |
| 4 | 1.31 | 1.17–1.46 | 1.35 | 1.07–1.70 | 1.23 | 1.08–1.41 |
| 5+ | 1.34 | 1.20–1.50 | 1.37 | 1.08–1.74 | 1.22 | 1.07–1.38 |
| LRT p-valueb | <0.0001 | |||||
| Breastfeedingc | ||||||
| None | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference |
| 1–3 months | 1.02 | 0.93–1.12 | 0.95 | 0.80–1.13 | 1.07 | 0.96–1.20 |
| 4–6 months | 0.97 | 0.86–1.09 | 1.05 | 0.84–1.31 | 0.95 | 0.83–1.09 |
| 7–12 months | 1.05 | 0.94–1.18 | 1.07 | 0.86–1.32 | 1.07 | 0.93–1.23 |
| >12 months | 0.91 | 0.82–1.00 | 0.68 | 0.56–0.82 | 1.04 | 0.93–1.17 |
| LRT p-valueb | <0.0001 | |||||
Models adjusted for parity (breastfeeding model only), age, BMI at age 21, education, household income, menopausal status, marital status, current occupational status, smoking status, alcohol consumption, fruit and vegetable consumption, total MET-hrs/day of physical activity, depression based on CESD, use of oral contraceptives, and age of menarche in categories as shown in Table 1.
LRT p-value = p-value from LRT evaluating models with and without inclusion of interaction term for race and breastfeeding categories.
Breastfeeding model excludes nulliparous women.
BMI, Body Mass Index; OR, odds ratio; CI, confidence interval; LRT, likelihood ratio test.
White women who breastfed for more than 12 months were 30% less likely to be obese than parous white women who did not breastfeed (OR = 0.68, 95% CI 0.56–0.82), while no effect was seen for any duration of breastfeeding among black women after multivariate adjustment (OR = 1.04, 95% CI 0.93–1.17 for 12+ months of breastfeeding compared to none; Table 3). In order to evaluate whether the effects seen for white women were due to residual confounding by socioeconomic status (SES), we examined education- and income-stratified logistic regression models. We found that the odds of obesity were reduced among white women who breastfed for more than 12 months compared to those who did not breastfeed in all categories of education and income (data not shown). To examine the potential for cohort effects which might reflect changes in breastfeeding practices over time in the United States, the models were stratified by 10-year age categories. OR and 95% CI for obesity among white women who breastfed more than 12 months compared to none was 0.58 (0.42–0.79) for women of ages 40–49; 0.58 (0.41–0.82) for ages 50–59; 0.99 (0.63–1.56) for ages 60–69; and 0.51 (0.33–1.32) for ages 70–79.
Discussion
In this large population-based study of low-income black and white women from the southeastern United States, we observed small but significant positive associations between parity and BMI in women of both races, with the magnitude of effect being larger in white women. At all levels of parity, BMI values as well as weight change since age 21 were higher among black women compared to white women. In addition, breastfeeding for a total of 12 months or more compared to none was associated with 30% decrease in the odds of obesity among white women. The overall contribution of parity and breastfeeding to BMI and weight change since age 21 was small. White women gained, on average, nearly 22 kg from age 21 until the SCCS baseline interview, and black women gained 25 kg, yet the largest differential in weight gain observed between any of the most extreme categories of parity and breastfeeding was 2.3 kg.
Understanding the determinants of obesity is important because the prevalence of obesity continues to increase in the United States. Factors related to childbearing are thought to be related to obesity although the epidemiologic literature assessing these relationships is sometimes conflicting. Several studies have reported positive associations between parity and body size;3–11,13 however, the magnitude and form of the associations varies greatly across studies. Early studies of the parity-obesity relationship generally enrolled women at the time of pregnancy in order to assess the short-term effects of pregnancy on body size and often did not include a comparison group of nulliparous women. However, the results of studies with and without a comparison group of nulliparous women are generally in agreement that increased parity, particularly the first birth, is associated with weight gain.5,6,14,26
Cross-sectional data collected among women past the childbearing years have also been used to examine the weight-parity association using current measures of body size and recalled parity. In the Iowa Women's Health Study (in which 99% of the participants were white), parity values of three to eight were associated with a steady increase in BMI compared to nulliparity. The difference in the adjusted total weight gain from age 18 to 50 was 3.1 kg for women with nine or more children and 2.4 kg for women with five children, both compared to nulliparous women3. These differences in weight change were similar to those observed in the present study in which we found a difference in weight gain since age 21 of 2.7 kg for white women with five or more children compared to nulliparous women. Additional cross-sectional studies have found similarly modest positive associations between parity and obesity or adult weight change in white women in Sweden,7 Poland,8 Utah,9 and among Chinese women.11
Fewer studies have examined parity and breastfeeding in relation to obesity in black women. In a 5-year follow-up of young black and white women, Smith et al.14 reported that nulliparous, primiparous, and multiparous black women gained more weight than white women at each level of parity, an observation that was confirmed over a much longer time period in the present study. Rosenberg and colleagues examined BMI change in relation to childbearing over a 4-year period in more than 1200 black women enrolled in the Black Women's Health Study.10 They reported that women who had a child during this follow-up period gained more weight than women who remained nulliparous which was also seen among black women in the present study. Regarding racial differences in the effect of childbearing on body weight, Wolfe et al. found no significant differences in the regression coefficients for parity in relation to BMI between black and white women using data from NHANES II.12 Using NHANES III data to examine the parity-obesity relationship in models stratified by race and residential location (metropolitan vs. non-metropolitan, categorized as population above or below 1,000,000), Lee et al. found that black women in metropolitan areas had higher BMI with increasing parity although the relationship was non-linear and that there was no association between parity and BMI in black women residing in non-metropolitan areas.13
In the current study, breastfeeding was inversely associated with current BMI only among white women who breastfed for 12 months or more. Although there was no evidence of a trend as shorter durations of breastfeeding were not associated with lower odds of obesity, it is possible that the relationship is non-linear and there is a threshold effect evident after 12 or more months of breastfeeding. We found little evidence that breastfeeding was associated with adult weight change or BMI in black women. The literature examining the relationship between breastfeeding and obesity is inconclusive and few studies have examined long-term weight change in relation to breast-feeding. Breastfeeding for more than 12 weeks was associated with a lower BMI after a 10-year follow-up among a group of Wisconsin women compared to no breast-feeding or breastfeeding for less than 12 weeks.18 This overall pattern is consistent with our findings, although the duration of breast-feeding associated with benefit was longer in our study. Other authors have also found weak negative associations between breastfeeding and body size,17,27,28 while others found no association.19,29 The inconsistencies in the reports regarding breastfeeding and body size may be related to poor measurement of the duration and intensity of breastfeeding as well as inadequate length of follow-up.15 The design of our study did not allow for careful examination of duration and intensity of breastfeeding but did provide an examination of the breastfeeding-obesity relationship many years after childbearing was completed. It is important to note that women who are obese prior to pregnancy or those who gain excessive weight during pregnancy may breastfeed less and have more difficulty with lactation30,31. Thus, prepregnancy body size or pregnancy weight gain may be important confounders of the relationship between obesity later in life and breastfeeding behavior. By adjusting for BMI at age 21, we have attempted to control for this confounding effect, but it may be that this adjustment is not sufficient because a majority of the women in our study had a first child before age 21.
Our study has several strengths. It should be noted that the SCCS population does not reflect the general population of the United States due to the recruitment of participants within the Community Health Center system and the resulting over-representation of people of low SES and African-American race. However, this is indeed a strength of the SCCS, making it a unique cohort in which to study health effects in different racial groups because of the large number of African-Americans and the comparability of SES across racial groups. Within-population comparisons, such as those described in this analysis, are valid regardless of the generalizability to the general population. Therefore, a major strength of this study is that a large number of black women as well white women from similar SES and geographic locales were included, allowing for comparisons across race groups that were likely less affected by uncontrolled SES confounding than many other studies. This is particularly important given that some studies of the parity-obesity relationship have found that SES is an important confounder.4,8 Our study also had a wide range of parity including large numbers of nulliparous women as well as women with five or more births.
Study limitations should also be noted. First, we used self-reported measures of weight and height both at the time of the baseline study interview and recalled from age 21. While older literature has indicated a high concordance for measured and self-reported values of height and weight,32 a more recent review indicates that height tends to be overreported while weight tends to be underreported.33 This phenomenon may even be exaggerated in overweight women34 leading to underestimates in BMI. However, the self-reported height and weight data in the SCCS baseline interview are believed to be generally of high quality. First, it is expected that the in-person nature of the interview is a deterrent for gross under- or over-reporting of weight by the participants. In addition, for approximately 25% of the SCCS population, weight and height are measured in the CHC as part of the medical visit on the day of the baseline interview, and this information is abstracted from the medical record by the study interviewer. The correlation is extremely high overall for the BMI values calculated from self-reported height and weight data compared to BMI calculated from the medical record data (Pearson correlation coefficient >0.95). In addition, when the women are stratified by BMI category (based on self-reported values), the differences between self-reported and measured weights show no indication that overweight or obese women are under-reporting weight more so than healthy weight women; the mean difference was 3.0 lbs among women with BMI 18.5–24.9 kg/m2, 2.2 lbs for BMI 25–29.9 kg/m2, 2.1 lbs for BMI 30–35 kg/m2, 1.8 lbs for BMI 35–39.9 kg/m2, and 0.1 lbs for BMI > 40 kg/m2. Differences between self-reported and measured weights did not differ by race, education, or income categories. Our measure of weight at age 21 is also based on self-report which is a further limitation of this analysis. Reports in the literature, however, indicate that, among middle-aged women, recall of weight in early adulthood is highly correlated with measured values.35–37 Recall is also a limitation with our self-reported measure of breastfeeding. At least one report in the literature shows that, even after 15–20 years, breastfeeding duration is recalled within 2–5 weeks of a validation standard.38 Differences of this magnitude would not likely cause a meaningful change in the broad categorization of breastfeeding duration used in this study.
A further limitation of this study is the cross-sectional nature of the data which precludes the examination of age or cohort effects or our ability to differentiate between the effects of child-bearing versus child-rearing on body size. In addition, these cross-sectional data make it difficult to assess whether factors related to health consciousness might confound associations between current body size and decisions made in the past related to breastfeeding and perhaps parity.
Conclusions
In this large population-based study of low-income black and white women from the southeastern United States, we observed small but significant positive associations between parity and BMI in women of both races with the magnitude of effect being larger in white women. In addition, breastfeeding for >12 months compared to none was associated with a 30% decrease in the odds of obesity among white women. The overall contribution of parity and breastfeeding to BMI and weight change since age 21 was small. However, child-bearing brings about a period of time in which women are frequently in contact with the health care system and may be more receptive to messages regarding weight control. Because the source of the obesity epidemic is likely multifaceted, parity and breastfeeding may be contributing components in a larger obesity prevention strategy.
Acknowledgments
We would like to thank Heather Munro for her statistical review. This project was supported by Susan G. Komen for the Cure (grant OP05-0927-DR1). The Southern Community Cohort Study is supported by the National Cancer Institute (grant R01 CA92447). Support was also provided by NCI (training grant T32 CA09330-26 to S.S.C.).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Ogden CL. Carroll MD. Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM. Carroll MD. Ogden CL, et al. Prevalence and trends in obesity among U.S. adults, 1999–2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 3.Brown JE. Kaye SA. Folsom AR. Parity-related weight change in women. Int J Obes Relat Metab Disord. 1992;16:627–631. [PubMed] [Google Scholar]
- 4.Wamala SP. Wolk A. Orth-Gomer K. Determinants of obesity in relation to socioeconomic status among middle-aged Swedish women. Prev Med. 1997;26:734–744. doi: 10.1006/pmed.1997.0199. [DOI] [PubMed] [Google Scholar]
- 5.Williamson DF. Madans J. Pamuk E, et al. A prospective study of childbearing and 10-year weight gain in US white women 25 to 45 years of age. Int J Obes Relat Metab Disord. 1994;18:561–569. [PubMed] [Google Scholar]
- 6.Harris HE. Ellison GT. Holliday M. Is there an independent association between parity and maternal weight gain? Ann Hum Biol. 1997;24:507–519. doi: 10.1080/03014469700005272. [DOI] [PubMed] [Google Scholar]
- 7.Lahmann PH. Lissner L. Gullberg B, et al. Sociodemographic factors associated with long-term weight gain, current body fatness and central adiposity in Swedish women. Int J Obes Relat Metab Disord. 2000;24:685–694. doi: 10.1038/sj.ijo.0801219. [DOI] [PubMed] [Google Scholar]
- 8.Szklarska A. Jankowska EA. Independent effects of social position and parity on body mass index among Polish adult women. J Biosoc Sci. 2003;35:575–583. doi: 10.1017/s002193200300600x. [DOI] [PubMed] [Google Scholar]
- 9.Bastian LA. West NA. Corcoran C, et al. Number of children and the risk of obesity in older women. Prev Med. 2005;40:99–104. doi: 10.1016/j.ypmed.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 10.Rosenberg L. Palmer JR. Wise LA, et al. A prospective study of the effect of childbearing on weight gain in African-American women. Obes Res. 2003;11:1526–1535. doi: 10.1038/oby.2003.204. [DOI] [PubMed] [Google Scholar]
- 11.Wen W. Gao YT. Shu XO, et al. Sociodemographic, behavioral, and reproductive factors associated with weight gain in Chinese women. Int J Obes Relat Metab Disord. 2003;27:933–940. doi: 10.1038/sj.ijo.0802318. [DOI] [PubMed] [Google Scholar]
- 12.Wolfe WS. Sobal J. Olson CM, et al. Parity-associated body weight: modification by sociodemographic and behavioral factors. Obes Res. 1997;5:131–141. doi: 10.1002/j.1550-8528.1997.tb00653.x. [DOI] [PubMed] [Google Scholar]
- 13.Lee SK. Sobal J. Frongillo EA, et al. Parity and body weight in the United States: differences by race and size of place of residence. Obes Res. 2005;13:1263–1269. doi: 10.1038/oby.2005.150. [DOI] [PubMed] [Google Scholar]
- 14.Smith DE. Lewis CE. Caveny JL, et al. Longitudinal changes in adiposity associated with pregnancy. The CARDIA Study. Coronary Artery Risk Development in Young Adults Study. JAMA. 1994;271:1747–1751. [PubMed] [Google Scholar]
- 15.Gunderson EP. Abrams B. Epidemiology of gestational weight gain and body weight changes after pregnancy. Epidemiol Rev. 2000;22:261–274. doi: 10.1093/oxfordjournals.epirev.a018038. [DOI] [PubMed] [Google Scholar]
- 16.Cohen A. Pieper CF. Brown AJ, et al. Number of children and risk of metabolic syndrome in women. J Womens Health. 2006;15:763–773. doi: 10.1089/jwh.2006.15.763. [DOI] [PubMed] [Google Scholar]
- 17.Ohlin A. Rossner S. Factors related to body weight changes during and after pregnancy: the Stockholm Pregnancy and Weight Development Study. Obes Res. 1996;4:271–276. doi: 10.1002/j.1550-8528.1996.tb00545.x. [DOI] [PubMed] [Google Scholar]
- 18.Rooney BL. Schauberger CW. Excess pregnancy weight gain and long-term obesity: one decade later. Obstet Gynecol. 2002;100:245–252. doi: 10.1016/s0029-7844(02)02125-7. [DOI] [PubMed] [Google Scholar]
- 19.Sichieri R. Field AE. Rich-Edwards J, et al. Prospective assessment of exclusive breastfeeding in relation to weight change in women. Int J Obes Relat Metab Disord. 2003;27:815–820. doi: 10.1038/sj.ijo.0802285. [DOI] [PubMed] [Google Scholar]
- 20.Calle EE. Rodriguez C. Walker-Thurmond K, et al. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 21.Bianchini F. Kaaks R. Vainio H. Overweight, obesity, and cancer risk. Lancet Oncol. 2002;3:565–574. doi: 10.1016/s1470-2045(02)00849-5. [DOI] [PubMed] [Google Scholar]
- 22.Key TJ. Allen NE. Verkasalo PK, et al. Energy balance and cancer: the role of sex hormones. Proc Nutr Soc. 2001;60:81–89. doi: 10.1079/pns200068. [DOI] [PubMed] [Google Scholar]
- 23.Eckel RH. York DA. Rossner S, et al. Prevention Conference VII: Obesity, a worldwide epidemic related to heart disease and stroke: executive summary. Circulation. 2004;110:2968–2975. doi: 10.1161/01.CIR.0000140086.88453.9A. [DOI] [PubMed] [Google Scholar]
- 24.Signorello LB. Hargreaves MK. Steinwandel MD, et al. Southern community cohort study: establishing a cohort to investigate health disparities. J Natl Med Assoc. 2005;97:972–979. [PMC free article] [PubMed] [Google Scholar]
- 25.Hargreaves MK. Arnold C. Blot WJ. Community health centers: Their role in the treatment of minorities and in health disparities research. In: Satcher D, editor; Pamies R, editor. Multicultural medicine and health disparities. New York: McGraw-Hill; 2006. pp. 485–494. [Google Scholar]
- 26.Coitinho DC. Sichieri R. D'Aquino Benicio MH. Obesity and weight change related to parity and breast-feeding among parous women in Brazil. Public Health Nutr. 2001;4:865–870. doi: 10.1079/phn2001125. [DOI] [PubMed] [Google Scholar]
- 27.Janney CA. Zhang D. Sowers M. Lactation and weight retention. Am J Clin Nutr. 1997;66:1116–1124. doi: 10.1093/ajcn/66.5.1116. [DOI] [PubMed] [Google Scholar]
- 28.Dewey KG. Heinig MJ. Nommsen LA. Maternal weight-loss patterns during prolonged lactation. Am J Clin Nutr. 1993;58:162–166. doi: 10.1093/ajcn/58.2.162. [DOI] [PubMed] [Google Scholar]
- 29.Potter S. Hannum S. McFarlin B, et al. Does infant feeding method influence maternal postpartum weight loss? J Am Diet Assoc. 1991;91:441–446. [PubMed] [Google Scholar]
- 30.Linne Y. Dye L. Barkeling B, et al. Weight development over time in parous women—the SPAWN study, 15-years follow-up. Int J Obes Relat Metab Disord. 2003;27:1516–1522. doi: 10.1038/sj.ijo.0802441. [DOI] [PubMed] [Google Scholar]
- 31.Li R. Jewell S. Grummer-Strawn L. Maternal obesity and breast-feeding practices. Am J Clin Nutr. 2003;77:931–936. doi: 10.1093/ajcn/77.4.931. [DOI] [PubMed] [Google Scholar]
- 32.Stewart AL. The reliability and validity of self-reported weight and height. J Chronic Dis. 1982;35:295–309. doi: 10.1016/0021-9681(82)90085-6. [DOI] [PubMed] [Google Scholar]
- 33.Gorber SC. Tremblay M. Moher D, et al. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev. 2007;8:307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- 34.Rowl ML. Self-reported weight and height. Am J Clin Nutr. 1990;52:1125–1133. doi: 10.1093/ajcn/52.6.1125. [DOI] [PubMed] [Google Scholar]
- 35.Casey VA. Dwyer JT. Berkey CS, et al. Long-term memory of body weight and past weight satisfaction: a longitudinal follow-up study. Am J Clin Nutr. 1991;53:1493–1498. doi: 10.1093/ajcn/53.6.1493. [DOI] [PubMed] [Google Scholar]
- 36.Must A. Willett WC. Dietz WH. Remote recall of childhood height, weight, and body build by elderly subjects. Am J Epidemiol. 1993;138:56–64. doi: 10.1093/oxfordjournals.aje.a116777. [DOI] [PubMed] [Google Scholar]
- 37.Stevens J. Keil JE. Waid LR, et al. Accuracy of current, 4-year, and 28-year self-reported body weight in an elderly population. Am J Epidemiol. 1990;132:1156–1163. doi: 10.1093/oxfordjournals.aje.a115758. [DOI] [PubMed] [Google Scholar]
- 38.Li R. Scanlon KS. Serdula MK. The validity and reliability of maternal recall of breastfeeding practice. Nutr Rev. 2005;63:103–110. doi: 10.1111/j.1753-4887.2005.tb00128.x. [DOI] [PubMed] [Google Scholar]