Abstract
Aims
The purpose of this randomized controlled clinical trial was to examine the effects of three couples-focused interventions and a control condition on women and men's resolution of depression and grief during the first year after miscarriage.
Methods
Three hundred forty-one couples were randomly assigned to nurse caring (NC) (three counseling sessions), self-caring (SC) (three video and workbook modules), combined caring (CC) (one counseling session plus three SC modules), or control (no treatment). Interventions, based on Swanson's Caring Theory and Meaning of Miscarriage Model, were offered 1, 5, and 11 weeks after enrollment. Outcomes included depression (CES-D) and grief, pure grief (PG) and grief-related emotions (GRE). Differences in rates of recovery were estimated via multilevel modeling conducted in a Bayesian framework.
Results
Bayesian odds (BO) ranging from 3.0 to 7.9 favored NC over all other conditions for accelerating women's resolution of depression. BO of 3.2–6.6 favored NC and no treatment over SC and CC for resolving men's depression. BO of 3.1–7.0 favored all three interventions over no treatment for accelerating women's PG resolution, and BO of 18.7–22.6 favored NC and CC over SC or no treatment for resolving men's PG. BO ranging from 2.4 to 6.1 favored NC and SC over CC or no treatment for hastening women's resolution of GRE. BO from 3.5 to 17.9 favored NC, CC, and control over SC for resolving men's GRE.
Conclusions
NC had the overall broadest positive impact on couples' resolution of grief and depression. In addition, grief resolution (PG and GRE) was accelerated by SC for women and CC for men.
Introduction
Approximately 15% of pregnancies end in miscarriage, the unexpected, unplanned loss of pregnancy prior to the expected point of fetal viability.1 Most women experience miscarriage as the loss of a baby to whom they already feel attached.2,3 In the days surrounding miscarriage, the majority of women experience grief or depression or both.4–7 As documented in a variety of cross-sectional and prospective studies, women's sadness may last up to 1 year after loss.4,7–15 Some women also experience guilt, anger, posttraumatic stress, and anxiety about future childbearing.16–19
Six months after miscarrying, women who are most depressed are least likely to have partners willing to talk about the miscarriage.5 Most women wish to discuss pregnancy loss and share it with their partners,20,21 yet 85% of couples share their feelings to a limited degree, if at all.22 Lack of partner support, both around the time of miscarriage5,23 and up to 2 years later, has been connected to women's increased emotional distress.24 Interpersonal and sexual distance 1 year after loss has been associated with male partners not engaging in caring acts and couples' failure to mutually share feelings about miscarriage.25,26 Partner support has also been linked to women's well-being during pregnancies after loss.27,28
Miscarriage also impacts men. In a new survey of 40 men, 59% reported a deepened awareness of the fragility of life, 45% mourned the loss of their family's hopes and dreams, 50% claimed they did not share feelings with their partner, and 40% experienced a strong sense of vulnerability and powerlessness to help their wife.29 Men's greatest concern after miscarriage tends to be the well-being of their partner;30–33 yet, fearing they might say the wrong thing, many resort to saying nothing.32
Men's initial responses to miscarriage may hamper their grief resolution. Eight weeks after miscarriage, Puddifoot and Johnson34 surveyed 323 men and discovered they had slightly lower active grief and somewhat higher difficulty coping, despair, and total grief scores than those reported for women at 6–8 weeks after loss. These findings warrant attention, given a prior prospective survey in which Lasker and Toedter35 demonstrated that elevations in difficulty coping and despair scores soon after miscarriage were significantly associated with higher grief scores 2 years after loss.
We found no published randomized controlled trials (RCTs) focused on emotional healing in men or couples after miscarriage. There were, however, six published clinical trials focused on women's emotional recovery: (1) Swanson randomized 185 women who were up to 5 weeks postmiscarriage to no treatment or to three nurse counseling sessions based on Swanson's Caring Theory (SCT)36,37 and Meaning of Miscarriage Model (MMM).38,39 Counseled women had significantly less depressed, angry, and overall disturbed moods during their first year after loss.39 (2) At 3 weeks after miscarriage, Adolfsson et al.40 randomized 88 Swedish women to either a traditional 30-minute midwife visit or an expanded 60-minute visit with a midwife whose care was based on the SCT and MMM. At 4 months, although there was a 30% greater reduction in grief scores in the treated group, the difference was not significant. (3) Lee et al.,41 using a trauma framework, randomized 39 women who miscarried for the first time to no treatment or to a home-delivered 1-hour counseling session based on a six-step debriefing process. At 4 months, there were no differences in anxiety, depression, intrusiveness, or avoidance. (4) At 5 weeks after loss, Nikcević et al.42 randomized 80 women to learning about medical cause (MC) or to MC plus 50 minutes of psychological counseling (MPC). Counseling focused on the trauma of miscarriage, self-blame, emotions, and worries about future childbearing. A comparison group of 61 women received no follow-up care. At 4, 7, and 16 weeks, there were greater decreases in grief and worry for the MPC group and in self-blame for the MPC and MC groups. (5) Neugebauer et al.43 enrolled 17 minimally depressed, recently miscarried, inner city women in a one group pretest and posttest pilot of a manualized, telephone-administered, interpersonal counseling (IPC) protocol. Women received one to six weekly phone calls focused on sustaining relationships and resolving miscarriage. At 9 weeks, treated women who completed outcome measures (n = 9) realized a clinically and statistically significant decline in their depression scores. For the noncompleters (n = 8), the investigators substituted baseline scores for their outcome scores, thus creating an intent-to-treat (ITT) sample of 17. There was a greater decrease in depressive symptoms for the 9 completers vs. the ITT total sample of 17, but the difference was not significant. (6) Neugebauer et al.44 also reported on a pilot randomized trial of their manualized IPC protocol vs. treatment as usual (TAU) with a sample of 19 mildly depressed English-speaking or Spanish-speaking women who were within 18 weeks of loss. Once again using ITT analysis, they compared depression and role functioning between the IPC (n = 10) and TAU (n = 9) groups and found a significantly greater within-subject average decline in depression scores in the IPC group. There were, however, no differences between the two groups in improved role functioning. Given the small sample size, it is possible that this study lacked sufficient power to detect a true treatment difference.
In summary, both women and men experience emotional upheaval after miscarriage. Although findings are mixed, the trend across studies indicates that women's emotional healing is enhanced by receipt of follow-up counseling interventions. There were no studies focused on ways to help men or couples resolve depression or grief after miscarriage. Hence, the purpose of the Couples Miscarriage Healing Project (CMHP) was to examine the effects of three theory-based couples-focused interventions (nurse, self, and combined caring) and a control condition (no treatment) on the rates at which women and men resolve depression and grief during the first year after miscarriage. All interventions were based on the SCT36,37,45 and MMM.38,39,46 We tested two hypotheses:
H1: During the first year after miscarriage, women and men randomized to nurse, self, or combined caring will exhibit faster rates of recovery from depression, pure grief (PG), and grief-related emotions (GRE) than those randomized to no treatment.
H2: During the first year after miscarriage, there will be no differences in rates of recovery from depression, PG, and GRE for women and men receiving nurse, self, or combined caring.
Materials and Methods
Design
This randomized controlled clinical trial was a repeated measures pretest–posttest experimental design (trial registration: clinicaltrials.gov/ Identifier: NCT00194844). The primary outcome was depression (CES-D47); the secondary outcome was grief (PG and GRE48).
Upon receipt of written consents and baseline data, using a card-pulling protocol, we randomly allocated couples to nurse caring (NC) (three counseling sessions), self-caring (SC) (three video and workbook modules), combined caring (CC) (one counseling session plus three video and workbook modules), or control (no treatment). To facilitate evenness across groups in size and historical context during the 2 1/2 years that we enrolled subjects, couples were randomized in blocks of 12.49 To assure integrity in randomization procedures and avoid potential errors due to physical randomization,50 a strict card-pulling protocol was followed. Randomization always involved two team members: one who shuffled the cards, vigorously shook the box, and lifted the box above the card puller's eye level, and the other who reached up and blindly pulled a card out of the box. After a card was drawn, both members recorded results.
Interventions were offered 1, 5, and 11 weeks after enrollment and took place in couples' homes. Data were gathered via mailed surveys at approximately 1 (baseline), 3, 5, and 13 months after miscarriage.
Recruitment
The study was approved for access to patients and protection of human subjects by Scientific Review Boards or Internal Review Boards at the University of Washington, Group Health Cooperative of Puget Sound, Evergreen Hospital and Medical Center, Madigan Army Medical Center, and St. Joseph Medical Center. Scientists from the University of Washington Center for Women's Health and Gender Research (5P30 NR 004001) comprised the Data Safety and Monitoring Board.
Volunteer couples from throughout the Puget Sound (Washington) area called the research project in response to recruitment posters, print and media ads, or pamphlets found in healthcare facilities. Couples were deemed eligible if both agreed to participate; they reported an unplanned, unexpected loss of pregnancy prior to 20 weeks gestation; they could speak and write in English; and they were in a self-proclaimed committed relationship, geographically accessible, and within 3 months of loss. Unmarried people aged <18 were not eligible. Couples were excluded if only one member returned the baseline survey. Enrollment began in January 2003. Data collection ended in June 2006. Couples were compensated up to $260.00.
The total sample for the CMHP was estimated to enable analysis from either a parametric or Bayesian framework.51 To detect a treatment effect on depression of 0.5 standard deviation (SD), two tailed, with alpha at 0.05 and power at 80%, we needed 54 women and 54 men per group.52 Aiming for 60 women and their male mates per group and anticipating a 30% attrition rate, recruitment goals were set at 85 couples per group.
Interventions
The content for all three interventions in the CMHP was based on the MMM. This model had been empirically developed through a phenomenological study with 20 women who were up to 4 months postmiscarriage when interviewed.38,46 The MMM consists of six emotionally challenging and meaning-laden experiences that commonly accompany miscarriage. For the CMHP, all interventions offered at 1 week focused on coming to know (the confusing painful process of balancing the mounting evidence of impending loss against hopes for a healthy pregnancy outcome) and losing and gaining (naming for oneself just what was lost or gained or both through miscarriage). Content at 5 weeks dealt with sharing the loss (identifying who was or was not available to acknowledge the loss, validate responses, and offer support) and going public (reentering the childbearing/rearing world and resuming life as a no longer expectant couple). Content at 11 weeks focused on getting through it (chronicling personal progress toward resolution) and trying again (facing the ongoing fears of future loss and planning for conception and pregnancy).
The process for all interventions was based on the SCT, which was derived through three phenomenological studies with individuals who had personally or professionally dealt with loss and stress related to childbearing.36,37,45 Caring is defined as “a nurturing way of relating to a valued other towards whom one feels a personal sense of commitment and responsibility.”36,p165 Caring is exhibited through five ways of relating to the one cared for: (1) knowing—striving to understand an event as it has meaning in the life of the other, (2) being with—offering an authentic and receptive emotional presence to the other, (3) doing for—doing for the other what they would do for themselves if it were at all possible, (4) enabling—facilitating the other's passage through an event or transition by offering information, support, and validation, and (5) maintaining belief—sustaining faith in the other's capacity to come through an event or transition and face a future with meaning.
Couples assigned to the NC condition received three 1-hour counseling sessions that took place in their homes or an alternate private location. Staying within the caring framework, process took precedence over content. If couples brought up a MMM topic out of order, their needs were addressed first. The primary goal of the two nurse counselors was to know, be with, do for, enable, and maintain belief in the couples and their capacity to come through the loss, care for each other, and face a future with meaning. Counselors were trained through role playing with actors, studying the SCT and MMM, and reviewing transcripts from Swanson's prior RCT, which was based on the same frameworks and involved women only.38,39 Counselors were coached by Swanson and had ongoing access to a social worker who offered support and generalized feedback on couples' confidential written evaluations of their sessions. One woman and five men attended none of their NC sessions.
The SC condition was included to determine if a lower cost, self-administered, mailed intervention would offer results comparable to those derived from counseling. Three videos of approximately 18 minutes each featured Swanson coaching couples on ways to practice self and partner caring. Also in the videos were clips of eight ethnically diverse actors scripted as four couples sharing stories of what it was like to go through the MMM experiences and care for each other. Videos were accompanied by two workbooks (his and hers). Workbooks had seven daily questions that elicited reflective writing about the MMM topics. Workbooks were considered private journals and not collected as data. Couples return-mailed a self-report checklist on use of the SC modules. If reports were not returned, couples were called to ascertain they had at least viewed their videos. Eight women and nine men reported never using their SC materials.
The CC condition was included because the Institute of Medicine reported that one of the greatest obstacles to establishing effectiveness of self-delivered interventions is getting people to actually use their prescribed protocol.53 At the end of their only counseling session, nurses gave CC couples their first SC module and encouraged its use. Their next two SC modules were mailed. Two women and one man did not participate in any aspect of their CC protocol.
Measures
All data were self-report. Demographics (including racial and ethnic identity), childbearing histories, and inquiries about prior treatment for depression, anxiety, or grief were gathered via investigator-developed checklists and for the purpose of sample description.
Depression was assessed using the Center for Epidemiological Studies-Depression scale (CES-D),47 a highly standardized 20-item indicator of depression in the general population. Scores of 16 are associated with higher risk for clinical depression and suggest the need for further assessment. Respondents are asked if they experienced symptoms during the prior 7 days on a 0 (rarely) to 3 (most of the time) scale. CMHP Cronbach's alpha reliability estimates for women ranged from 0.908 to 0.923 and for men from 0.884 to 0.902.
Grief was measured using two subscales from the Miscarriage Grief Inventory (MGI).48 The MGI was adapted from the Texas Grief Inventory.54 Respondents rate items as 1 (completely true) to 5 (completely false) indicators of their experience. The PG subscale (7 items) focuses on thinking about the miscarriage and crying inwardly and outwardly about the lost baby. GRE (6 items) focuses on feelings that indicate distance (numbness, avoiding thinking about it, can't cry) and distress (guilty, angry, unfair). CMHP Cronbach's alpha reliability estimates for women ranged from 0.876 to 0.897 for PG and from 0.761 to 0.853 for GRE and for men from 0.871 to 0.878 for PG and from 0.802 to 0.854 for GRE.
Analysis
Background data were described using measures of central tendency. Equivalency across treatment arms at baseline was examined using MANOVA with Bonferroni-corrected post hoc pairwise comparisons. Differences in baseline measures between partners were further examined using paired t tests. Hypothesized treatment effects on individual recovery were examined using multilevel modeling (MLM) conducted in a Bayesian framework. (See Lewis and Wears' description of the advantages of Bayesian approaches to evaluating relative effectiveness of clinical interventions.)51
Three covariates were included in the statistical model used to assess treatment effects: (1) difference between the person's and sample's average time since loss at baseline, (2) history of treatment for depression, anxiety, or grief (yes = 1, no = 0), and (3) baseline scores. Gender differences in treatment effects were addressed by inclusion of mutually exclusive statistical clauses, one activated if the person was female and the other if the person was male. MLM enables consideration of the fact that each person's slope of recovery is impacted by both the treatment he or she received and by his or her mate's recovery over time. The following equation was inspired by a similar approach used to study psychological change in married couples over time55:
 |
In this set of equations, yi is a person's estimated scale score at each postbaseline measurement occasion, α is the person-level intercept (which is set to baseline), b1 is the regression coefficient for the (centered) time of enrollment (enrollc), b2 is the regression coefficient for baseline history of treatment for depression, anxiety, or grief (blmtmt), b3 is the regression coefficient for the baseline score (representing whether initial scores predict later scores, having taken the actual baseline into account as the intercept), ɛi represents random error at the person-measure level, πF and πM are the effects of being in a particular couple for females or for males (respectively), (wave = 1) is the measurement-wave variable (centered at the first postbaseline measurement wave). γF and γM are the female and male regression coefficients representing average recovery trajectories attributable to membership in a particular group, and ɛFk and ɛMk represent random error for females and males, respectively, at the couple level.
After running the initial tests of H1 and H2, we controlled for individual CES-D scores at each measurement wave and reran all equations pertaining to the effects of treatment on PG and GRE. These analyses enabled consideration of whether treatment had a unique impact on grief (adjustment to miscarriage) separate from its impact on depression (reduction of depressive symptoms that may or may not have been a response to miscarriage).
Treatment effects, the difference in estimated recovery trajectories between any two groups, are represented via three summary statistics. The probability value (p) indicates the proportion of times (based on 20,000 iterations) the estimated slope of recovery due to treatment A was steeper (faster) than that due to treatment B. Bayesian odds (BO), the ratio of pA/pB, characterizes the strength of evidence favoring treatment A over B (also described as the posterior probability that the theory undergirding treatment A vs. its rival is true). The median estimate of the difference in slopes (Mdn) indicates the size of the effect on outcome scores at each measurement wave. A negative Mdn indicates the rate of recovery (slope) due to A was faster (steeper) than that due to B.
Bayesian factors simply summarize the evidence found in a dataset that favors one hypothesis over its rival hypothesis. As Bayesian approaches do not assume a normal distribution, placing confidence intervals around a BO ratio is not appropriate. Jeffreys56 offered rough guidelines for interpreting BO ratios and suggested that a BO ratio > 3.2 be interpreted as “substantial” evidence favoring one treatment over its rival and that a BO > 10 be interpreted as “strong” evidence. Kass and Raftery state: “Jeffreys was concerned with the comparison of predictions made by two competing scientific theories. In his approach, statistical models are introduced to represent the probability of the data according to each of two theories, and Bayes theorem is used to compute the posterior probability that one of those two competing theories is correct.”57,p773
Results
Recruitment and retention
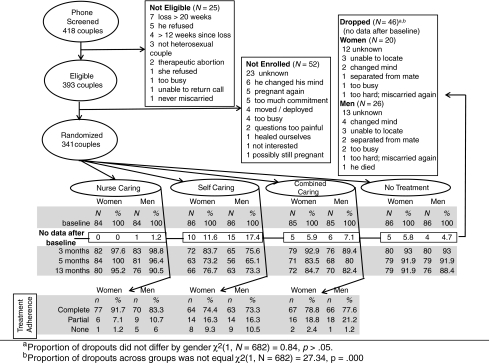
As depicted in Figure 1, 418 couples were screened, 393 met eligibility criteria, and 341 were enrolled and randomized. Seventeen couples plus an additional 3 women and 9 men returned no data after baseline. As MLM requires at least two data points to estimate a slope of recovery, those 46 (6.7% of 682) individuals were considered dropouts and eliminated from all further analysis. Thus, the sample size for the final analysis was 636 (93.26% of 682). There were no known adverse events or side effects for any of the intervention groups.
Fig. 1.
Subject flow: Recruitment, eligibility, randomization, data completion, and treatment adherence.
Sample characteristics
Couples had been together from 3 months to 24 years (mean = 6.9 years, SD = 4.5, Mdn = 6). They had up to 6 children, with 181 couples (53.1%) having none and 107 (31.4%) having 1. Pregnancies were planned by 246 couples (72.1%) and wanted by 333 (97.7%). Women had from 1 to 6 miscarriages, with the current loss being the first for 232 (68%) women. Gestational age at loss ranged from 2.7 to 21 weeks (mean = 9.8, SD = 3.1, Mdn = 9.6). Most (n = 324; 95%) miscarried before 16 weeks gestation. (At screening, one couple reported miscarrying prior to 20 weeks. When we calculated gestational age based on onset of last menses (as per her baseline data), the gestational age was closer to 21 weeks.)
As displayed in Table 1, compared with women, men were older and more likely to be employed. Men (25.2%) were significantly less likely than women (48.7%) to have ever been treated for depression, anxiety, or grief: chi-square (1, n = 682) = 40.3, p = 0.000. There were no significant differences in baseline characteristics due to randomization.
Table 1.
Sample Characteristics
| |
Number (%) of Individualsa |
|
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| |
NC |
SC |
CC |
Control |
|
|
||||
| |
Women |
Men |
Women |
Men |
Women |
Men |
Women |
Men |
p valueb,c |
|
| Characteristic | (n = 84) | (n = 84) | (n = 86) | (n = 86) | (n = 85) | (n = 85) | (n = 86) | (n = 86) | Group | Sex |
| Employed | 57 (67.9) | 73 (86.9) | 60 (70.6) | 81 (94.2) | 59 (69.4) | 69 (82.1) | 60 (69.8) | 73 (84.9) | 0.464 | 0.001 |
| History of depression, anxiety, or grief | 45 (53.6) | 22 (26.2) | 42 (48.8) | 22 (25.6) | 42 (49.4) | 20 (23.5) | 38 (44.2) | 23 (26.7) | 0.855 | 0.001 |
| Education | 0.763 | 0.223 | ||||||||
| ≤12 years | 12 (14.3) | 7 (8.3) | 7 (8.1) | 12 (14) | 7 (8.2) | 12 (15.3) | 6 (7.0) | 12 (14) | ||
| Some college | 12 (14.3) | 23 (27.4) | 25 (29.1) | 24 (27.9) | 22 (25.9) | 20 (23.5) | 26 (30.2) | 26 (30.2) | ||
| College graduate | 28 (33.3) | 36 (42.9) | 29 (33.7) | 29 (33.7) | 34 (40) | 23 (27.1) | 29 (33.7) | 32 (37.2) | ||
| Graduate degree | 32 (38.1) | 18 (21.4) | 25 (29.1) | 21 (24.4) | 22 (25.9) | 29 (34.1) | 25 (29.1) | 16 (18.6) | ||
| Ethnicity/race | 0.463 | 0.520 | ||||||||
| Native American | 3 (3.6) | 1 (1.2) | 0 (0) | 0 (0) | 0 (0) | 1 (1.2) | 4 (4.7) | 0 (0) | ||
| Black | 2 (2.4) | 5 (6) | 3 (3.5) | 2 (2.4) | 5 (6) | 4 (4.7) | 3 (3.5) | 5 (5.8) | ||
| Asian/Pacific Islander | 5 (6) | 2 (2.4) | 6 (7.1) | 5 (5.9) | 6 (7.1) | 8 (9.4) | 4 (4.7) | 4 (4.7) | ||
| Hispanic | 3 (3.6) | 5 (6) | 3 (3.5) | 2 (2.4) | 3 (3.6) | 1 (1.2) | 2 (2.3) | 3 (3.5) | ||
| White | 71 (84.5) | 71 (84.5) | 73 (85.9) | 76 (89.4) | 70 (83.3) | 71 (83.5) | 73 (84.9) | 74 (86) | ||
| Missing | 0 (0) | 0 (0) | 1 (1.2) | 1 (1.2) | 1 (1.2) | 0 (0) | 0 (0) | 0 (0) | ||
| Income | 0.086 | 0.773 | ||||||||
| 0–20 K | 12 (14.3) | 8 (9.6) | 7 (8.2) | 6 (7.1) | 11 (12.9) | 12 (14.1) | 9 (10.5) | 12 (14) | ||
| 21–50 K | 18 (21.4) | 21 (25.3) | 18 (21.2) | 19 (22.4) | 18 (21.2) | 15 (17.6) | 22 (25.6) | 23 (26.7) | ||
| 51–90 K | 24 (28.6) | 24 (28.9) | 37 (43.5) | 35 (41.2) | 37 (43.5) | 35 (41.2) | 32 (37.2) | 24 (27.9) | ||
| 91 K plus | 30 (35.7) | 30 (36.1) | 23 (27.1) | 25 (29.4) | 19 (22.4) | 23 (27.1) | 23 (26.7) | 27 (31.4) | ||
| Missing | 0 (0) | 1 (1.2) | 1 (1.2) | 1 (1.2) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | ||
| Age, mean (SD) | 32.7 (6.4) | 33.8 (6.8) | 32.0 (5.3) | 33.8 (6.3) | 32.5 (5.8) | 34.1 (6.2) | 32.5 (6.5) | 34.0 (7.7) | 0.938 | 0.002 |
| Days since loss at baseline, mean (SD) | 29.1 (22.7) | 30.8 (23.1) | 30.7 (24.2) | 32.7 (25.5) | 28.3 (19.5) | 30.5 (20.9) | 32.7 (22.8) | 34.5 (25.4) | 0.330 | 0.277 |
Unless otherwise indicated.
p value from chi-square if categorical or binary data; from F test if interval data.
No significant interactions between group and sex.
As displayed in Figure 1, the proportion of dropouts did not differ by gender: chi-square (1, n = 682) = 0.84, p > 0.05. The proportion of dropouts across groups was not equal: chi-square (1, n = 682) = 27.34, p = 0.000. SC had the highest proportion of individuals (25 of 172, 14.5%) who never returned data after baseline, and NC had the least (1 of 168, 0.6%).
Baseline equivalency
As depicted in Table 2, although there were no significant differences in baseline scores attributable to randomization, there were some differences attributable to dropout status and gender. Those who dropped out (mean = 17.57, SD = 5.64) had a significantly higher average baseline GRE (p = 0.011) than those who continued (mean = 15.75, SD = 5.14). Women had significantly higher PG and CES-D scores than men. Upon further examination using paired t tests for related samples, women's PG (mean = 25.8, SD = 6.1), GRE (mean =17.0, SD = 5.1), and CES-D (mean = 21.7, SD = 11.9) scores were all significantly higher (p = 0.000) than that of their mates [men: PG (mean = 19.1, SD = 6.2), GRE (mean = 14.8, SD = 5.0), and CES-D (mean = 13.8, SD = 9.3)].
Table 2.
Baseline Differences due to Randomization (Group), Dropout Status, and Gender
| |
Mean (SD)a |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |
NCb |
SC |
CC |
NT |
||||||||||||
| |
Dropc,f |
Stay |
Drop |
Stay |
Drop |
Stay |
Drop |
Stay |
||||||||
| Women(n = 0) | Mend(n = 1) | Women(n = 84) | Men(n = 83) | Women(n = 10) | Men(n = 15) | Women(n = 76) | Men(n = 71) | Women(n = 5) | Men(n = 6) | Women(n = 80) | Men(n = 79) | Women(n = 5) | Men(n = 4) | Women(n = 81) | Men(n = 82) | |
| CES-De | 0 (0) | 26 (0) | 21.4 (10.8) | 12.5 (8.5) | 27.6 (15) | 15.1 (7.9) | 16.5 (5.1) | 13.7 (4.8) | 23 (7.1) | 10.2 (7.9) | 22 (13.2) | 12.8 (8.7) | 16.4 (8.3) | 12 (8.8) | 21.7 (12.5) | 15.5 (10.3) |
| PG | 0 (0) | 27 (0) | 25.9 (6) | 18.9 (6) | 27.7 (4.6) | 18.47 (6) | 25.6 (5.7) | 17.9 (5.6) | 26.8 (6.1) | 19.7 (5.4) | 26.2 (6.1) | 19.7 (6.2) | 22.8 (10.9) | 22.5 (11) | 25.4 (6.4) | 19.7 (6.7) |
| GRE | 0 (0) | 22 (0) | 17.2 (5.1) | 14.7 (4.4) | 18.9 (4.1) | 16.2 (5.3) | 21.5 (10.9) | 14.4 (9.8) | 20.6 (6.9) | 15.2 (6.7) | 17 (5.2) | 14.7 (5) | 17.4 (6.3) | 18.3 (6.6) | 16.7 (5.1) | 15.3 (5.4) |
| CES-D | PG | GRE | ||||||||||||||
| df | F | p | F | p | F | p | ||||||||||
| 3, 667 | 1.06 | ns | 0.241 | ns | .365 | ns | ||||||||||
| 1, 667 | 0.168 | ns | 0.841 | ns | 6.45 | 0.011 | ||||||||||
| 1, 667 | 12.69 | <0.001 | 21.03 | <0.001 | 2.54g | ns |
Main effects based on MANOVA are as follows; there were no significant interactions effects.
Group
Drop
Gender
Women's CES-D (mean = 21.7, SD = 11.9) ranged from 1 to 60, with 66.9% (n = 228) ≥16.
Men's CES-D (mean = 13.8, SD = 9.3) ranged from 0 to 51 with 37.2% (n = 127) ≥16.
Drops (mean = 17.57, SD = 5.64) had higher GRE than nondrops (mean = 15.75; SD = 5.14).
When reexamined using paired t tests, women's GRE were higher than men's (p = 0.000).
There were no significant two-way or three-way interactions resulting from dropout status, gender, and randomization on any of the baseline measures. Thus, we assumed variability in PG, GRE, and CES-D scores attributable to gender and dropout status was equivalent across groups at baseline.
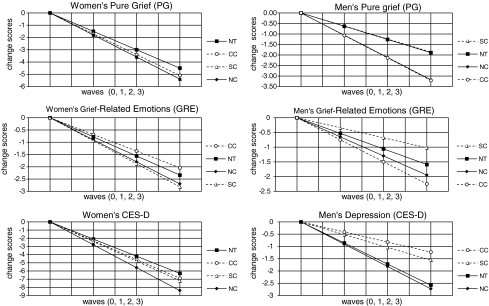
Treatment effects
As depicted in Table 3 and Figure 2, compared with no treatment, there was mixed evidence in favor of H1 that NC, SC, and CC accelerated resolution of depression, PG, and GRE. Women in all three treated groups exhibited a faster rate of recovery from depression compared with women receiving no treatment. However, it was only NC (BONC v control = 7.9, p = 0.89, Mdn = −0.7) that met Jeffrey's criterion for “substantial evidence.”56 Relative to no treatment, there was substantial evidence that all three interventions hastened women's resolution of PG [(BOCC v control = 3.1, p = 0.76, Mdn = −0.2), (BONC v control = 5.5, p = 0.85, Mdn = −0.3) and SC (BOSC v control = 7.0, p = 0.87, Mdn = −0.4)]. The evidence weakly favored NC's impact on GRE but substantially favored SC's effectiveness in hastening women's resolution of GRE (BOSC v control = 3.2, p = 0.76, Mdn = −0.2). In no circumstance was there substantial evidence that the control condition was preferable to SC, CC, or NC in accelerating women's resolution of PG, GRE, or depression.
Table 3.
Evidence in Favor of the Hypothesis that Treatment A Is More Effective than Treatment B in Accelerating Emotional Healing
| |
Treatment A |
|||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |
Women |
Men |
||||||||||||||||||||||
| |
Control |
SC |
CC |
NC |
Control |
SC |
CC |
NC |
||||||||||||||||
| Mdna | BOb | pc | Mdn | BO | p | Mdn | BO | p | Mdn | BO | p | Mdn | BO | p | Mdn | BO | p | Mdn | BO | p | Mdn | BO | p | |
| Treatment B | ||||||||||||||||||||||||
| Control | ||||||||||||||||||||||||
| PG | −0.4 | 7.0 | 0.87 | −0.2 | 3.1 | 0.76 | −0.3 | 5.5 | .85 | 0.005 | 0.97 | 0.49 | −0.4 | 22.6 | 0.96 | −0.4 | 20.2 | 0.95 | ||||||
| GRE | −0.2 | 3.2 | 0.76 | 0.09 | 0.55 | 0.35 | −0.1 | 2.4 | 0.70 | 0.2 | 0.27 | 0.22 | −0.2 | 4.3 | 0.81 | −0.1 | 2.3 | 0.69 | ||||||
| CESD | −0.3 | 2.3 | 0.70 | −0.1 | 1.5 | 0.60 | −0.7 | 7.9 | 0.89 | 0.3 | 0.31 | 0.24 | 0.4 | 0.18 | 0.16 | −0.05 | 1.2 | 0.54 | ||||||
| SC | ||||||||||||||||||||||||
| PG | 0.4 | 0.15 | 0.13 | 0.1 | 0.54 | 0.35 | 0.05 | 0.79 | 0.44 | −0.005 | 1.0 | 0.51 | −0.4 | 18.7 | 0.95 | −0.4 | 19.2 | 0.95 | ||||||
| GRE | 0.2 | 0.32 | 0.24 | 0.3 | 0.16 | 0.14 | 0.05 | 0.74 | 0.43 | −0.2 | 3.5 | 0.78 | −0.4 | 17.9 | 0.95 | −0.3 | 8.0 | 0.89 | ||||||
| CESD | 0.3 | 0.43 | 0.30 | 0.1 | 0.69 | 0.41 | −0.4 | 3.0 | 0.75 | −0.3 | 3.2 | 0.76 | 0.1 | 0.67 | 0.40 | −0.4 | 3.9 | 0.80 | ||||||
| CC | ||||||||||||||||||||||||
| PG | 0.2 | 0.32 | 0.24 | −0.1 | 1.9 | 0.65 | −0.08 | 1.5 | 0.61 | 0.4 | 0.04 | 0.04 | 0.4 | 0.05 | 0.05 | 0.008 | 0.95 | 0.49 | ||||||
| GRE | 0.09 | 0.54 | 0.65 | −0.3 | 6.1 | 0.86 | −0.2 | 4.3 | 0.81 | 0.2 | 0.23 | 0.19 | 0.4 | 0.05 | 0.05 | 0.1 | 0.50 | 0.33 | ||||||
| CESD | 0.1 | 0.66 | 0.40 | −0.1 | 1.4 | 0.59 | −0.5 | 4.8 | 0.83 | −0.4 | 5.3 | 0.84 | −0.1 | 1.5 | 0.60 | −0.5 | 6.6 | 0.87 | ||||||
| NC | ||||||||||||||||||||||||
| PG | 0.3 | 0.18 | 0.15 | −0.05 | 1.3 | 0.56 | 0.08 | 0.64 | 0.39 | 0.4 | 0.05 | 0.05 | 0.4 | 0.05 | 0.05 | −0.008 | 1.0 | 0.51 | ||||||
| GRE | 0.1 | 0.43 | 0.30 | −0.05 | 1.3 | 0.57 | 0.2 | 0.23 | 0.19 | 0.1 | 0.45 | 0.31 | 0.3 | 0.14 | 0.11 | −0.1 | 2.0 | 0.67 | ||||||
| CESD | 0.7 | 0.14 | 0.11 | 0.4 | 0.33 | 0.25 | 0.5 | 0.20 | 0.17 | 0.05 | 0.85 | 0.46 | 0.4 | 0.25 | 0.20 | 0.5 | 0.15 | 0.13 | ||||||
Mdn, median estimate of the difference in recovery slopes across the postbaseline measurement waves (effect size).
BO, Bayesian odds ratio. Using Jeffreys criterion,56 evidence is substantial if BO ≥ 3.2 and strong if BO ≥ 10.
p, Probability that the slope of recovery due to treatment A is steeper (faster) than the slope of recovery to treatment B.
Fig. 2.
Estimated slopes of recovery for women and men by group.
For men, relative to no treatment, none of the interventions provided substantial evidence of accelerating resolution of depression. In fact, the evidence was substantial that men's depression resolved more rapidly for those randomized to control vs. SC (BOcontrol v SC = 3.2, p = 0.76, Mdn = −0.3) or CC (BOcontrol v CC = 5.3, p = 0.84, Mdn = −0.4). Both CC (BOCC v control = 22.6, p = 0.96, Mdn = −0.4) and NC (BONC v control = 20.2, p = 0.95, Mdn = −0.4) provided strong evidence of hastening men's resolution of PG. Whereas the evidence weakly favored NC's effectiveness relative to no treatment for hastening men's resolution of GRE, it substantially favored CC (BOCC v control = 4.3, p = 0.81, Mdn = −0.2). Finally, men randomized to no treatment resolved GRE faster than men in SC (BOcontrol v SC = 3.5, p = 0.78, Mdn = −0.2).
Under no circumstance did covarying on CES-D scores make a meaningful difference in interpretation of the impact of treatment on men or women's resolution of PG or GRE. The change in probability that treatment A (NC, SC, or CC) was more or less effective than treatment B (no treatment) ranged from p = 0.00 to p = 0.02. For example, controlling for CES-D and comparing NC to control for women, there was no difference in the median effect size (in both cases Mdn = −0.3), a minimal increase in BO (BO = 6.5 vs. BO = 5.5), and a miniscule increase in the likelihood that NC was more effective than no treatment (p = 0.87 vs. (p = 0.85).
Treatment comparisons
As depicted in Table 3 and Figure 2, there was mixed evidence refuting H2 that there would be no difference in treatment impact of SC, CC, and NC on the rates at which women and men resolved PG, GRE, and depression during the first year after miscarriage.
For women, the evidence favored NC over SC and CC for accelerating resolution of depression (BONC v SC = 3.0, p = 0.75, Mdn = −0.4 and BONC v CC = 4.8, p = 0.83, Mdn = −0.5). For men, compared with SC and CC, there was substantial evidence that NC hastened resolution of depression (BONC v SC = 3.9, p = 0.80, Mdn = −0.4 and BONC v CC = 6.6, p = 0.87, Mdn = −0.5).
For women, compared with CC, both NC and SC provided weak evidence of hastening PG resolution and substantial evidence of accelerating resolution of GRE (BONC v CC = 4.3, p = 0.81, Mdn = −0.2 and BOSC v CC = 6.1, p = 0.86, Mdn =−0.3). For men, compared with SC, both CC and NC offered strong evidence of accelerating resolution of PG (BONC v SC = 19.2, p = 0.95, Mdn = −0.4 and BOCC v SC = 18.7, p = 0.95, Mdn = −0.4) and substantial (BONC v SC = 8.0, p =0.89, Mdn = −0.3) to strong (BOCC v SC = 17.9, p = 0.95, Mdn = −0.4) evidence of hastening men's resolution of GRE.
There was no evidence to suggest that SC, CC, or control was more effective than NC in hastening women or men's resolution of PG, GRE, or depression. Furthermore, under no circumstance did covarying on CES-D scores at each measurement wave make a meaningful difference in interpretation of the relative effectiveness of NC, SC, and CC on women or men's resolution of PG or GRE.
Discussion
Treatment impact on resolution of depression
Women who received three nurse counseling sessions resolved depression faster than women in the control, CC, or SC conditions. For men, although NC offered no benefit over the control condition for resolving depression, both NC and no treatment were substantially more effective than SC or CC. In fact, men exposed to the SC modules, whether in isolation or in combination with one counseling session, took substantially longer to resolve their symptoms of depression. Conceivably, men appraised the SC modules as unacceptable (as evidenced by lower treatment adherence rates), irrelevant (one treatment did not fit all), or too narrow (as if miscarriage were the only salient issue impacting their lives).
Our findings provided evidence that one fairly rushed counseling session (as in CC) was not enough to positively influence women's depression and may have played a part in hindering men's resolution of depression. Three sessions, however, hastened women's resolution of depression and, at the very least, did no harm to men's. The three counseling sessions were conducted from a patient-centered framework where the nurses' goals were to know, be with, do for, enable, and maintain belief in the couple. Conceivably, three sessions offered more time for each nurse and couple to connect, negotiate the pacing and content of their discussions, and jointly address the meaning of miscarriage in the overall context of each couple's lives.
Treatment impact on resolution of grief
Men's grief resolved most expeditiously through receipt of CC, suggesting that one nurse counseling session followed up with the videos and workbooks may have provided sufficient coaching to help men come to terms with their own transitional responses to miscarriage. The one counseling session also provided men with an opportunity to witness how the nurse responded to their mate's distress. This, in turn, might have helped men to experience a sense of adequacy in bearing witness to and responding to their mate's ongoing sadness.30–33
Although CC had a somewhat positive impact in hastening women's PG relative to NT, it did not substantially accelerate women's resolution of GRE. Perhaps, having observed their mates' healing subsequent to receipt of CC, women felt distressed by their inability to recover at the same rate. It is also possible that women, having enjoyed their one counseling session, felt disappointed or abandoned when they received no more. In contrast, women in the SC condition, having never been exposed to an NC session, were not aware of what they were missing. In fact, their PG and GRE resolved most expeditiously, suggesting that SC was particularly helpful to women as they dealt with their transitional grief. They had the option of using the SC modules as often as they desired, with or without their partners, and with whomever else they might wish to share the videos or discuss their workbook entries. In contrast, the evidence was substantial that SC alone did not accelerate men's resolution of PG and that use of the SC modules hindered their resolution of GRE. As men randomized to no treatment, NC, and CC all resolved GRE faster than men assigned to SC, perhaps men's need to move past the miscarriage was challenged by their partner's revisiting the experience each time she used the SC materials.
Grief, depression, and historical context
We found it particularly illuminating that when we controlled for CES-D scores at each measurement wave, conclusions drawn about treatment effectiveness on PG or GRE did not change. Miscarriage does not happen in isolation. We believe our findings of the impact of differential treatment on grief and depression may well reflect differences in the underlying sources of sadness that impacted the lives of the women and men we studied. Not surprisingly, because the PG scale contains items most closely reflecting expected transitory responses to miscarriage (e.g., I cry when I think about the miscarriage.), it was most responsive to our interventions. In contrast, the CES-D has indicators of sadness and melancholy that could be related to any number of issues ranging from a short-lived version of postmiscarriage adjustment to an underlying and possibly unrelated clinical depression.
As depicted in Table 2, approximately 1 month after miscarriage and prior to randomization, the average CES-D for women in this sample was almost 22. Two thirds (n = 228) of the women and 37.2% (n = 127) of the men scored ≥16 (a score suggestive of depression and warranting clinical evaluation).47 This proportion of individuals being at risk for clinical depression is considerably higher than previously reported rates of 10%–54% for women and 4%–10% for men at 2–12 weeks after miscarriage.5,58–60 For our sample, we believe responses to miscarriage were compounded by the study's historical context. Within weeks of enrolling the first couple in the CMHP, the United States went to war and remained at war for the duration of data collection. In addition, many individuals throughout the region lost jobs because of related downturns in the airline and internet/computer industries. It is noteworthy that almost one half of the women and one quarter of the men in our sample reported having been previously treated for depression, anxiety, or grief. These rates are somewhat higher than those found in a recently miscarried U.K. sample (n = 273 women and 133 men), where self-reported rates of prior treatment for depression or anxiety, respectively, were 30.8% and 28.6% for women and 14.3% and 18.9% for men.59 These differences between the U.S. and U.K. samples could be due to variations in how questions related to prior treatment were posed or interpreted, cultural differences in attitudes toward seeking support for emotional unrest, or indications of historical differences in experienced negative life events or perceived vulnerability between these two samples of women and men in their childbearing years.
Strengths and limitations
Critique could be offered that if the couple served as the unit of randomization and intervention, outcomes could also have been examined at the level of the couple. We contend, however, that although it may be possible to create an aggregate variable (e.g., the mean or sum of the couples' CES-D scores), the construct “couple depression” remains clinically problematic because the experience of feeling depressed still occurs at the level of the person. For this reason, we specifically chose MLM, as it allowed consideration of individualness (influence of personal background and baseline scores) and coupleness (influence of mate score at each measurement point) and treatment (influence of being treated together) on each individual's slope of recovery. (See Raudenbush et al.55 for an example of how MLM is an effective model for taking into account an individual's feelings over time as influenced by living in the context of a given couple relationship over time.)
Critique could also be levied against our use of physical randomization methods vs. reliance on a table of randomly generated numbers.50 Yet our findings of no significant group differences at baseline on any of the demographic or outcome variables measured indicate that the randomization strategy employed was effective in assuring that all subjects had an equal chance of being assigned to any of the four treatment arms.
There are limits to the generalizability of these findings. Our predominantly Caucasian sample comprised volunteer couples in self-proclaimed heterosexual committed relationships, who were also literate in English and responsive to advertisements or pamphlets. Furthermore, as demonstrated by jointly returning their consents and baseline measures, couples were able to come to agreement about enrolling. Because those who dropped out had higher GRE scores than those who remained, caution should be exercised when applying findings to individuals whose initial reactions suggest high distress (guilt, anger, feelings of unfairness) or an inability to deal with the loss (numbness, avoiding thinking about it, can't cry).
In those circumstances where we found substantial to strong evidence favoring one treatment over its comparator for hastening recovery, the associated median estimates of differences in effect sizes between group scores at each measurement wave were as low as Mdn = −0.2 points to as high as Mdn = −0.7 points. As effects were additive, by 1 year, point differences ranged from −0.6 to −2.1. Although these effect sizes were not dramatic, they may, nonetheless, be of consequence, especially if the differences in trajectories continued over time.
Strengths of this study are (1) including both genders, (2) basing intervention content and process on prior phenomenological research, (3) using design control for potential childbearing and demographic differences across treatment arms, (4) accruing sufficient evidence (e.g., an adequate sample) to demonstrate credible differences between nurse-delivered vs. self-delivered interventions, (5) examining whether the impact of treatment on grief was separate from its impact on depression, and (6) evaluating the impact of treatment on each individual while taking into account the reality that treatment and healing occurred in the context of his or her couple relationship.
It is not known if couples had been offered a menu of treatment options how study outcomes might have differed. Future couples-focused research needs to take into consideration couples' and individuals' preferences, costs, and consideration of which couples would benefit most strongly from which type of intervention.
Conclusions
Sadness after miscarriage can be approached as a transitory grief response warranting supportive care,39–44 a trigger of clinical depression or posttraumatic stress disorder necessitating treatment,4,5,9,60 or a situational crisis warranting careful consideration of both responses.25 Our study and the research of others61,62 suggest that couples desire validation of the meaningfulness of their experience, guidance on strategies to deal with their loss, and information on ways to care for each other.
Consistent with prior reports,5,21,29,63 we found that men and women responded differently to miscarriage. Likewise, their experiences of grief and depression were differently impacted by our three couples-focused caring-based interventions. We found substantial to strong evidence that relative to no treatment, NC accelerated women and men's resolution of PG, modest evidence that it accelerated their resolution of GRE, and substantial evidence that it enhanced women's resolution of depression. Although we found no evidence that NC offered any benefit over control with regard to men's depression relative to SC and CC, it substantially accelerated their resolution of depression. We, therefore, conclude that whereas SC was quite effective in hastening women's grief resolution and CC positively accelerated men's grief resolution, it took three theory-based couples-focused nurse counseling sessions to most adequately support couples' emotional healing after miscarriage.
Acknowledgments
Funding was provided by the NIH, National Institute of Nursing Research, 5 R01 NR005343, to K.M.S. We express our deep gratitude to the couples who shared their experiences of miscarriage and healing so that others may learn from their experiences. Contributions of the following are acknowledged: Helga Sif Fridjonsdottir, R.N., Ph.D. (University of Iceland) and Alyson Shapiro, Ph.D. (Arizona State University) for data analysis and management; Rosalie Houston, R.N., M.N. (University of Washington Medical Center) and Susan Sandblom, A.R.N.P., M.N., (Virginia Mason Medical Center) for their roles as Nurse Counselors; and Appalachia Martine, B.S.N. (University of Washington) and Susan Lee-Pullen (University of Washington) for their administrative support.
K.M.S., J.C.G., and H.-T.C. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the analysis.
Disclosure Statement
K.M.S., developer of the SCT, consults internationally on its use in clinical, research, and academic settings and is compensated for consulting and receives honoraria for invited presentations. No competing financial interests exist for H.-T.C., J.C.G., D.M.W., and A.P.
References
- 1.Ventura SJ. Mosher WD. Curtin SC. Abma JC. Henshaw S. National Vital Statistics Reports. 29. Vol. 47. Hyattsville, MD: National Center for Health Statistics; 1999. Highlights of trends in pregnancies and pregnancy rates by outcome: Estimates for the United States, 1976–96. [PubMed] [Google Scholar]
- 2.Hutti MH. dePacheco MA. A study of miscarriage: Development and validation of the Perinatal Grief Intensity Scale. JOGN Nurs. 1998;27:547–555. doi: 10.1111/j.1552-6909.1998.tb02621.x. [DOI] [PubMed] [Google Scholar]
- 3.Neugebauer R. Ritsher J. Depression and grief following early pregnancy loss. Int J Childbirth Educ. 2005;20:21–24. [Google Scholar]
- 4.Beutel M. Deckardt R. vonRad M. Weiner H. Grief and depression after miscarriage: Their separation, antecedents, and course. Psychosom Med. 1995;57:517–526. doi: 10.1097/00006842-199511000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Beutel M. Willner H. Deckardt R. vonRad M. Weiner H. Similarities and differences in couples' grief reactions following a miscarriage: Results from a longitudinal study. J Psychosom Res. 1996;40:245–253. doi: 10.1016/0022-3999(95)00520-x. [DOI] [PubMed] [Google Scholar]
- 6.Prettyman RJ. Cordle CJ. Cook GD. A three month follow-up of psychological morbidity after early miscarriage. Br J Med Psychol. 1993;66:363–372. doi: 10.1111/j.2044-8341.1993.tb01762.x. [DOI] [PubMed] [Google Scholar]
- 7.Thapar AK. Thapar A. Psychological sequelae of miscarriage: A controlled study using the general health questionnaire and hospital anxiety and depression scale. Br J Gen Pract. 1992;42:94–96. [PMC free article] [PubMed] [Google Scholar]
- 8.Neugebauer R. Kline J. O'Connor P, et al. Determinants of depressive symptoms in the early weeks after miscarriage. Am J Public Health. 1992;82:1332–1339. doi: 10.2105/ajph.82.10.1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neugebauer R. Kline J. O'Connor P, et al. Depressive symptoms in women in the six months after miscarriage. Am J Obstet Gynecol. 1992;166:104–109. doi: 10.1016/0002-9378(92)91839-3. [DOI] [PubMed] [Google Scholar]
- 10.Garel M. Blondel B. LeLong N. Kaminski M. Depressive disorders after a spontaneous abortion. Am J Obstet Gynecol. 1993;168:1005–1006. doi: 10.1016/s0002-9378(12)90868-6. [DOI] [PubMed] [Google Scholar]
- 11.Garel M. Blondel B. LeLong N. Bonenfant S. Kaminski M. Long-term consequences of miscarriage: The depressive disorders and the following pregnancy. J Reprod Infant Psychol. 1994;12:233–240. [Google Scholar]
- 12.Robinson GE. Stirtzinger R. Stewart DE. Ralevski E. Psychological reactions in women followed for 1 year after miscarriage. J Reprod Infant Psychol. 1994;12:31–36. [Google Scholar]
- 13.Lee DT. Wong CK. Cheung LP. Leung HC. Haines CJ. Chung TK. Psychiatric morbidity following miscarriage: A prevalence study of Chinese women in Hong Kong. J Affect Disord. 1997;43:63–68. doi: 10.1016/s0165-0327(96)01418-8. [DOI] [PubMed] [Google Scholar]
- 14.Tunaley JR. Slade P. Duncan SB. Cognitive processes in psychological adaptation to miscarriage: A preliminary report. Psychol Health. 1993;8:369–381. [Google Scholar]
- 15.Swanson KM. Predicting depressive symptoms after miscarriage: A path analysis based on Lazarus' paradigm. J Womens Health Gend Based Med. 2000;9:191–206. doi: 10.1089/152460900318696. [DOI] [PubMed] [Google Scholar]
- 16.Klier CM. Geller PA. Ritsher JB. Affective disorders in the aftermath of miscarriage: A comprehensive review. Arch Womens Ment Health. 2002;5:129–149. doi: 10.1007/s00737-002-0146-2. [DOI] [PubMed] [Google Scholar]
- 17.Lee C. Slade P. Miscarriage as a traumatic event: A review of the literature and new implications for intervention. J Psychosom Res. 1996;40:235–244. doi: 10.1016/0022-3999(95)00579-x. [DOI] [PubMed] [Google Scholar]
- 18.Armstrong D. Hutti M. Pregnancy after perinatal loss: The relationship between anxiety and prenatal attachment. JOGN Nurs. 1998;27:183–189. doi: 10.1111/j.1552-6909.1998.tb02609.x. [DOI] [PubMed] [Google Scholar]
- 19.Côté-Arsenault D. Threat appraisal, coping, and emotions across pregnancy subsequent to perinatal loss. Nurs Res. 2007;56:108–116. doi: 10.1097/01.NNR.0000263970.08878.87. [DOI] [PubMed] [Google Scholar]
- 20.Black RB. Women's voices after pregnancy loss: Couples' patterns of communication and support. Soc Work Health Care. 1991;16:19–36. doi: 10.1300/j010v16n02_03. [DOI] [PubMed] [Google Scholar]
- 21.Conway K. Russell G. Couples' grief and experience of support in the aftermath of miscarriage. Br J Med Psychol. 2000;73:531–545. doi: 10.1348/000711200160714. [DOI] [PubMed] [Google Scholar]
- 22.Speraw SR. The relationship between marital adjustment, self-disclosure and intimacy and the accuracy of couples' perceptions of each other's grieving following a miscarriage [Dissertation] Los Angeles, CA: California School of Professional Psychology; 1991. [Google Scholar]
- 23.Toedter LJ. Lasker JN. Alhadeff JM. The Perinatal Grief Scale: Development and initial validation. Am J Orthopsychiatry. 1988;58:435–449. doi: 10.1111/j.1939-0025.1988.tb01604.x. [DOI] [PubMed] [Google Scholar]
- 24.Cordle CJ. Prettyman RJ. A 2-year follow-up of women who have experienced early miscarriage. J Reprod Infant Psychol. 1994;12:37–43. [Google Scholar]
- 25.Swanson KM. Jolley S. Pettinato M. Wang TY. Connor S. The context and evolution of women's responses to miscarriage over the first year after loss. Res Nurs Health. 2007;30:2–16. doi: 10.1002/nur.20175. [DOI] [PubMed] [Google Scholar]
- 26.Swanson KM. Karmali Z. Powell S. Pulvermahker F. Miscarriage effects on interpersonal and sexual relationships during the first year after loss: Women's perceptions. Psychosom Med. 2003;65:902–910. doi: 10.1097/01.psy.0000079381.58810.84. [DOI] [PubMed] [Google Scholar]
- 27.Ney PG. Fung T. Wickett AR. Beaman-Dodd C. The effects of pregnancy loss on women's health. Soc Sci Med. 1994;38:1193–1200. doi: 10.1016/0277-9536(94)90184-8. [DOI] [PubMed] [Google Scholar]
- 28.Rajan L. Oakley A. No pills for heartache: The importance of social support for women who suffer pregnancy loss. J Reprod Infant Psychol. 1993;11:75–87. [Google Scholar]
- 29.Speraw SR. The experience of miscarriage: How couples define quality in health care delivery. J Perinatol. 1994;14:208–215. [PubMed] [Google Scholar]
- 30.Miron J. Chapman JS. Supporting men's experiences with the event of their partners' miscarriage. Can J Nurs Res. 1994;26:61–72. [PubMed] [Google Scholar]
- 31.Murphy FA. The experience of early miscarriage from a male perspective. J Clin Nurs. 1998;7:325–332. doi: 10.1046/j.1365-2702.1998.00153.x. [DOI] [PubMed] [Google Scholar]
- 32.Puddifoot JE. Johnson MP. The legitimacy of grieving: The partner's experience at miscarriage. Soc Sci Med. 1997;45:837–845. doi: 10.1016/s0277-9536(96)00424-8. [DOI] [PubMed] [Google Scholar]
- 33.Fisher KA. Miscarriage: A phenomenological approach to the father's experience [Dissertation] Charlottesville, VA: University of Virginia; 2001. [Google Scholar]
- 34.Puddifoot JE. Johnson MP. Active grief, despair, and difficulty coping: Some measured characteristics of male response following their partner's miscarriage. J Reprod Infant Psychol. 1999;17:89–93. [Google Scholar]
- 35.Lasker JN. Toedter LJ. Acute versus chronic grief: The case of pregnancy loss. Am J Orthopsychiatry. 1991;61:510–522. doi: 10.1037/h0079288. [DOI] [PubMed] [Google Scholar]
- 36.Swanson KM. Empirical development of a middle range theory of caring. Nurs Res. 1991;40:161–166. [PubMed] [Google Scholar]
- 37.Swanson KM. Nursing as informed caring for the well-being of others. Image J Nurs Sch. 1993;25:352–357. doi: 10.1111/j.1547-5069.1993.tb00271.x. [DOI] [PubMed] [Google Scholar]
- 38.Swanson KM. Research-based practice with women who have had miscarriages. Image J Nurs Sch. 1999;31:339–345. doi: 10.1111/j.1547-5069.1999.tb00514.x. [DOI] [PubMed] [Google Scholar]
- 39.Swanson KM. The effects of caring, measurement, and time on miscarriage impact and women's well-being in the first year subsequent to loss. Nurs Res. 1999;48:288–298. doi: 10.1097/00006199-199911000-00004. [DOI] [PubMed] [Google Scholar]
- 40.Adolfsson A. Berterö C. Larsson PG. Effect of a structured follow-up visit to a midwife on women with early miscarriage: A randomized study. Obstet Gynecol. 2006;85:330–335. doi: 10.1080/00016340500539376. [DOI] [PubMed] [Google Scholar]
- 41.Lee C. Slade P. Lygo V. The influence of psychological debriefing on emotional adaptation in women following miscarriage: A preliminary study. Br J Med Psychol. 1996;69:47–58. doi: 10.1111/j.2044-8341.1996.tb01849.x. [DOI] [PubMed] [Google Scholar]
- 42.Nikcević AV. Kuczmierczyk AR. Nicolaides KH. The influence of medical and psychological interventions on women's distress after miscarriage. J Psychosom Res. 2007;63:283–290. doi: 10.1016/j.jpsychores.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 43.Neugebauer R. Kline J. Bleiberg K, et al. Preliminary open trial of interpersonal counseling for subsyndromal depression following miscarriage. Depress Anxiety. 2007;24:219–222. doi: 10.1002/da.20150. [DOI] [PubMed] [Google Scholar]
- 44.Neugebauer R. Kline J. Markowitz J, et al. Pilot randomized controlled trial of interpersonal counseling for subsyndromal depression following miscarriage. J Clin Psychiatry. 2006;67:1299–1304. doi: 10.4088/jcp.v67n0819. [DOI] [PubMed] [Google Scholar]
- 45.Swanson KM. What's known about caring in nursing: A literary meta-analysis. In: Hinshaw AS, editor; Shaver J, editor; Feetham S, editor. Handbook of clinical nursing research. Thousand Oaks, CA: Sage; 1999. pp. 31–60. [Google Scholar]
- 46.Swanson-Kauffman KM. The unborn one: A profile of the human experience of miscarriage [Dissertation] Denver, CO: University of Colorado; 1983. [Google Scholar]
- 47.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 48.Nikcević AV. Snijders R. Nicolaides KH. Kupek E. Some psychometric properties of the Texas Grief Inventory adjusted for miscarriage. Br J Med Psychol. 1999;72:171–178. doi: 10.1348/000711299159925. [DOI] [PubMed] [Google Scholar]
- 49.Altman DG. Practical statistics for medical research. Boca Raton, FL: Chapman & Hall; 1991. [Google Scholar]
- 50.Bland M. An introduction to medical statistics. New York: Oxford University Press; 2000. [Google Scholar]
- 51.Lewis RJ. Wears RL. An introduction to the Bayesian analysis of clinical trials. Ann Emerg Med. 1993;22:1328–1336. doi: 10.1016/s0196-0644(05)80119-2. [DOI] [PubMed] [Google Scholar]
- 52.Cohen J. Statistical power analysis for the behavioral sciences. New York: Academic Press; 1977. [Google Scholar]
- 53.Margie NG, editor; Phillips DA, editor. Institute of Medicine. Revisiting home visiting: Summary of a workshop. Washington, DC: National Academy Press; 1999. pp. 7–10. [PubMed] [Google Scholar]
- 54.Zisook S. Devaul RA. Click MA., Jr. Measuring symptoms of grief and bereavement. Am J Psychiatry. 1982;139:1590–1593. doi: 10.1176/ajp.139.12.1590. [DOI] [PubMed] [Google Scholar]
- 55.Raudenbush SW. Brennan RT. Barnett RC. A multivariate hierarchical model for studying psychological change with married couples. J Fam Psychol. 1995;9:161–174. [Google Scholar]
- 56.Jeffreys H. Theory of probability. 3rd ed. Oxford, U.K.: Oxford University Press; 1961. [Google Scholar]
- 57.Kass R. Raftery A. Bayes factors. J Am Stat Assoc. 1995;90:773–795. [Google Scholar]
- 58.Lok IH. Neugebauer R. Psychological morbidity following miscarriage. Best Pract Res Clin Obstet Gynaecol. 2007;21:229–247. doi: 10.1016/j.bpobgyn.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 59.Cumming GP. Klein S. Bolsover D, et al. The emotional burden of miscarriage for women and their partners: Trajectories of anxiety and depression over 13 months. Br J Obstet Gynaecol. 2007;114:1138–1145. doi: 10.1111/j.1471-0528.2007.01452.x. [DOI] [PubMed] [Google Scholar]
- 60.Neugebauer R. Kline J. Shrout P, et al. Major depressive disorder in the 6 months after miscarriage. JAMA. 1997;277:383–388. [PubMed] [Google Scholar]
- 61.Wong MK. Crawford TJ. Gask L. Grinyer A. A qualitative investigation into women's experiences after a miscarriage: Implications for the primary healthcare team. Br J Gen Pract. 2003;53:697–702. [PMC free article] [PubMed] [Google Scholar]
- 62.Simmons RK. Singh G. Maconochie N. Doyle P. Green J. Experience of miscarriage in the UK: Qualitative findings from the National Women's Health Study. Soc Sci Med. 2006;63:1934–1946. doi: 10.1016/j.socscimed.2006.04.024. [DOI] [PubMed] [Google Scholar]
- 63.Stinson KM. Lasker J. Lohmann J. Toedter LJ. Parents' grief following pregnancy loss: A comparison of mothers and fathers. Fam Relat. 1992;41:218–223. [Google Scholar]