Abstract
Aim:
To examine the hypothesis that circular labour migrants who become seriously ill while living away from home return to their rural homes to convalesce and possibly to die.
Methods:
Drawing on longitudinal data collected by the Agincourt health and demographic surveillance system in rural northeastern South Africa between 1995 and 2004, discrete time event history analysis is used to estimate the likelihood of dying for residents, short-term returning migrants, and long-term returning migrants controlling for sex, age, and historical period.
Results:
The annual odds of dying for short-term returning migrants are generally 1.1 to 1.9 times (depending on period, sex, and age) higher than those of residents and long-term returning migrants, and these differences are generally highly statistically significant. Further supporting the hypothesis is the fact that the proportion of HIV/TB deaths among short-term returning migrants increases dramatically as time progresses, and short-term returning migrants account for an increasing proportion of all HIV/TB deaths.
Conclusions:
This evidence strongly suggests that increasing numbers of circular labour migrants of prime working age are becoming ill in the urban areas where they work and coming home to be cared for and eventually to die in the rural areas where their families live. This shifts the burden of caring for them in their terminal illness to their families and the rural healthcare system with significant consequences for the distribution and allocation of health care resources.
Keywords: Agincourt, AIDS, HIV, labour, migration, mortality, South Africa
Background
Population settlement and mobility patterns in South Africa have been strongly influenced by the mining industry, and in particular the notorious migrant labour system that supplied black labour for the mines and industrial development from the 1940s to current times [1,2]. The supply of labour was tied to the apartheid political system through a range of state mechanisms such as Influx Control and the Group Areas Act, and consequently a deliberate impermanence was introduced into the urbanization process of black South Africans. People were forced to live in “homeland” areas based on assigned ethnic identity, and within homelands access to land was severely restricted by a process of “villagization” in which people were forcibly moved to peri-urban villages [3]. This created a shortage of land for villagers and resulted in a transition from an agrarian to a cash-based economy [4,5] that critically depended on migrant labour.
One result was rural poverty with vast numbers of separated families living in dense settlements largely without adult males. These features still characterize much of South Africa's rural interior although the patterns of migration have altered considerably over the last three decades. Migrant labour is tending to involve longer periods of circular migration but with more frequent returns home, enabled by transport and infrastructural development [2]. The general trend of high and increasing levels of temporary (or circular) migration is supported by data from the Agincourt field site (the locus of the present study) [6] although now the range of destinations and types of work involved are more diverse than mining alone.
There is a growing literature on the relationship between temporary migration and the HIV epidemic; for South Africa see Jochelson [7] and Lurie [2], and for other parts of sub-Saharan African see Nunn [8], Pison [9], Decosas [10], and Quinn [11]. A study of the sero-prevalence of HIV in rural KwaZulu-Natal found a threefold higher risk of HIV infection associated with a recent migration [12]. The mechanism underlying this risk is that migrants are more likely than non-migrants to practice unsafe sex with multiple sexual partners [13]. This risk can be increased by rural migrants experiencing emotional instability on exposure to the urban environment, which can lead to “temporary solutions in serial and potentially high-risk sexual relationships” [14]. However recent studies [13,15] show that the link between migration and HIV transmission may be more complex than first suggested, and that both sending communities and workplace communities are affected by the high levels of migration. While much existing literature focuses on the role of migration in the transmission of the HI virus, this paper examines the role of chronic, terminal illness in migration, specifically movement back to rural homes.
There are a number of important public health implications. Critical information for planning involves “place”: where people are getting sick and where people are dying. This is part of a more general challenge – little addressed – of how to develop health services that can adequately respond to the needs of circular labour migrants.
Aims
In large parts of rural South Africa, high levels of endemic circular labour migration resulting from apartheid-era labour policies ensure that large fractions of working-age men, and increasingly women, spend significant portions of the year living in urban areas and working away from their rural homes. With the advent of the HIV/AIDS epidemic in South Africa many of these regular labor migrants are at increased risk of exposure to infection with HIV while they are living alone in comparatively poor conditions in the urban centers far from their families and home communities.
This work examines the hypothesis that people who become seriously ill while living away from home return to their rural homes, where social networks and support systems may be stronger, to convalesce and possibly to die.
Beyond describing a further heartbreaking twist to the unfolding HIV/AIDS epidemic affecting South Africa, the answer to this question will be important in assessing which communities should receive special allocations and support aimed at caring for persons with AIDS. Moreover there may well be additional burdens placed on already strained rural health services; this warrants judicious monitoring and timely intervention where indicated.
Material and methods
Data
Data supporting this investigation come from the Agincourt health and demographic surveillance system (AHDSS) in rural northeastern South Africa [16,17]. From 1992 to the present the AHDSS has northwestern monitored approximately 70,000 individuals comprising roughly 11,500 households in 21 villages of Bushbuckridge District, Limpopo Province, South Africa. Annual visits are made to each household during which a range of individual and household-level demographic, socioeconomic, and health-related information is collected, and importantly all vital and migration events that occurred during the preceding year are recorded. A separate team follows up on each reported death and conducts an in depth verbal autopsy interview to assign a probable cause to each death [18-22]. Each verbal autopsy is read independently by two physicians who assign ICD-10-coded main, immediate, and contributing causes. When there is disagreement and consensus cannot be reached, a third physician, blind to prior findings, reviews the case. When this diagnosis is congruent with one of the others it is accepted as the probable cause of death. When all three disagree, the case is assigned to an undetermined category. During 2002 (the most recent full year for which all deaths have been assigned a cause) roughly one-third of both female and male adult deaths resulted from an AIDS-related cause. Finally during each annual update, the residence and migration status of each individual living in the surveillance site is ascertained. Circular labour migrants are identified as adults who spend six months or more working away from home during the year, but return regularly and continue to view their rural home as the center of their social and economic lives. The current residence location and most recent date of return are also recorded for each circular labour migrant. From the late 1990s to the present roughly 60% of men and 20% of women aged 20–60 years are considered regular circular labour migrants [23].
Analysis
The hypothesis predicts a differential in the likelihood of dying between residents of the study area and short-term returning circular labour migrants. Discrete time event history analysis [24-26] is used to estimate the likelihood of dying for residents, short-term returning migrants, and migrants who returned permanently some time in the past, controlling for sex, age, and historical period. This method provides the ability to take into account the duration-specific components of the likelihood of dying in addition to providing statistical tests of the differences in likelihoods of dying between different migrant status groups and through time.
A person-year file is constructed that contains one record for each year lived by each individual in the study population. The values of the following attributes are defined at the beginning of each person year: individual ID, sex, date of birth, date of death, age, calendar year, return date for circular migrants who have moved back home permanently, whether or not the person dies during the year, and – if there is a death – the ICD-10-coded causes (main, immediate, and contributing). This file contains 682,056 person years for both sexes and all ages over the period 1992–2004. Restricting this to working-age adults between 20 and 80 years of age leaves 317,510 person years with 3,689 deaths. Further restricting this to only those years for which deaths have been assigned a probable cause, 1992–2002, leaves 291,713 person years and 2,952 deaths (reading the verbal autopsies and assigning causes is a time-consuming task and consequently there is always a lag between the time deaths are recorded and probable causes are assigned). All of the analysis presented here is conducted using this person-year file.
Discrete time event history analysis is used to estimate the annual hazard of death of adults aged 20–80 years as a function of historical period, sex, age, and migrant status. Two historical periods are used in this analysis: the first, 1992–97, covers the initial phase of the HIV epidemic during which comparatively few HIV-related deaths occurred [27], and the second, 1998–2004, covers the remainder of the study period when AIDS is an increasingly important cause of death. Migrant status is assigned one of three values: (1) resident, (2) short-term returning migrants, and (3) long-term returning migrants. Short-term returning migrants have been back home on a permanent basis for less than five years while long-term returning migrants have been home for five years or more. The basic model relates the probability of dying during a person year (the annual hazard of death) to migrant status and historical period. This model is estimated separately for males and females in 20-year age groups 20–39, 40–59, and 60–79 using ordinary logistic regression. The resulting period, sex, age, migrant status-specific annual hazards of death are converted to life-table probabilities of dying 20q20, 20q40, and 20q60 (nqx: the probability of dying between ages x and x+n for those who survive to age x).
Deaths are classified and counted by historical period, sex, age, migrant status, and cause category. Because assigned causes are not available for all deaths occurring in 2003–04, the historical periods are 1992–97 and 1998–2002. The cause categories are HIV/TB (using the verbal autopsy method it can be difficult to distinguish AIDS and TB as causes of death at ages younger than 60, and because HIV and TB so often occur together in patients the two causes are pooled under the assumption that most TB deaths have AIDS as a contributing cause [27]), non-communicable diseases (NCD), external causes (including both intentional and unintentional injury), and all other causes (the “other” category includes a small number of deaths that do not have a verbal autopsy and deaths for which a probable cause could not be determined based on the verbal autopsy). We are primarily interested in the deaths due to HIV/AIDS and TB, but it is instructive to compare trends in HIV/TB deaths with trends in the NCD deaths that should be less affected by the HIV epidemic or the mechanisms contributing to the transmission of HIV (there are exceptions to this, for example some stroke, some cancer of the cervix, and some other malignancies can be associated with HIV).
Results
To test the hypothesis that short-term returning migrants face a greater risk of dying compared with similar people who are permanent residents or long-term returning migrants, life-table probabilities of dying (nqx) are calculated and plotted by sex, period, migrant status, and age (Figure 1). Since there is no statistical difference in the risk of dying experienced by permanent residents and long-term returning migrants, these two groups have been merged and treated as one. Table I displays the odds ratios, p-values, and confidence intervals for the logistic regressions of death during a year on migrant status and period at the beginning of the year. These regressions are performed separately for each sex–age group and therefore relate the risk of dying of recent returning migrants to residents and long-term returning migrants within a specific sex-age category. The nqx values in Figure 1 are calculated from the annual hazards of death predicted by these regression results.
Figure 1.
Life table probability of dying by sex, period, migrant status and age. The life table probability of dying (nqx) is greater for short-term (recently) returned migrants in all sex–period–age categories. There are large increases in the risk of dying with age and in the second period for both sexes.
Table I.
Logistic regression of death on migrant status and period: 1992–2004, Agincourt.
| Migrant status/period | OR | p-value | CI |
|---|---|---|---|
| Female: 20–39 | |||
| resident | reference | ||
| short-term returning | 1.869 | <0.001 | [1.495–2.336] |
| long-term returning | 2.089 | 0.015 | [1.151–3.791] |
| first period: 1992–1997 | reference | ||
| second period: 1998–2004 | 3.464 | <0.001 | [2.840–4.226] |
| Female: 40–59 | |||
| resident & long-term returning | reference | ||
| short-term returning | 1.633 | 0.001 | [1.230–2.166] |
| first period: 1992–1997 | reference | ||
| second period: 1998–2004 | 2.432 | <0.001 | [1.944–3.042] |
| Female: 60–79 | |||
| resident & long-term returning | reference | ||
| short-term returning | 1.125 | 0.581 | [0.740–1.711] |
| first period: 1992–1997 | reference | ||
| second period: 1998–2004 | 1.165 | 0.067 | [0.990–1.372] |
| Male: 20–39 | |||
| resident & long-term returning | reference | ||
| short-term returning | 1.570 | <0.001 | [1.273–1.937] |
| first period: 1992–1997 | reference | ||
| second period: 1998–2004 | 1.953 | <0.001 | [1.647–2.317] |
| Male: 40–59 | |||
| resident & long-term returning | reference | ||
| short-term returning | 1.333 | 0.006 | [1.086–1.635] |
| first period: 1992–1997 | reference | ||
| second period: 1998–2004 | 1.535 | <0.001 | [1.300–1.811] |
| Male: 60–79 | |||
| resident & long-term returning | reference | ||
| short-term returning | 0.720 | 0.008 | [0.565–0.918] |
| first period: 1992–1997 | reference | ||
| second period: 1998–2004 | 1.343 | <0.001 | [1.139–1.584] |
The unit of analysis for these regressions is ‘person-year’. The regressions predict the annual hazard of death as a function of migrant status and period within each sex–age group. OR=odds ratio; p-value=testing the null hypothesis that (1 – odds ratio)=0; CI=95% confidence interval around the odds ratio.
Females aged 60–79 is the only group without a statistically significant difference between short-term returning migrants and residents/long-term returning migrants. This is a group that contains very few short-term returning migrants and would not be expected to contain very many because the recent upswing in female circular labour migration relates to younger women. The remaining differences in nqx values between short-term returning migrants and residents/long-term returning migrants are statistically significant within sex-age categories. The only sex-age group to demonstrate a statistically significant difference between short-term and long-term returning migrants is females aged 20–39.
Controlling for period, short-term returning migrants have odds of dying that are between 1.1 and 1.9 times greater than residents and long-term returning migrants, depending on period, sex, and age (except for men in the 60–79 age group who are discussed below). Figure 1 clearly reveals that short-term returning migrants of both sexes in both periods and of all ages face a substantially higher risk of dying. Furthermore, the risk of dying increases dramatically over time in all categories, but the difference in the risk of dying between short-term returning migrants and everyone else is even more pronounced in the second period when AIDS mortality is more significant (Figure 2). Note that the greatest difference between short-term returning migrants and residents is for younger (20–59) women in the most recent period 1998–2004. This may reflect the rapid increase in HIV prevalence among young women, and also their greater susceptibility to infection while living away from home in urban areas. These findings confirm that circular labour migrants who have moved back home within the past five years are more likely to die than either permanent residents or circular migrants who returned home more than five years ago, regardless of their sex or age; and, furthermore, that this additional risk is greater in the more recent historical period (1998–2004).
Figure 2.
Difference between life table probabilities of dying by sex, period and age: Short-term returning migrants / residents and long-term returning migrants. The absolute difference between the life table probabilities of dying of short-term returning migrants and all other people is large and positive in all sex–age categories except for males 60–79 years. The largest differences are for females 20-59 in the second period 1998–2004.
There is one puzzling exception to this pattern: older men 60–79 who are long-term returning migrants actually have an important and significant lower likelihood of dying compared with residents. This is probably due to a sustained, strong selection process that eliminated less healthy male migrant laborers over the past 40 years or so, and additionally men in this age group are less likely to have become infected with HIV before returning home (remember that they returned some time earlier than five years into the past). However, additional investigation is necessary to explain this finding with confidence.
We explain the general finding that short-term returning migrants experience a higher likelihood of dying by hypothesizing that the increase in the prevalence of HIV is leading to increasing numbers of circular migrants who become ill with AIDS while in urban settings and then return to their rural homes to be cared for before they eventually die. This hypothesis would predict that a disproportionately large number of the deaths occurring in short-term returning migrants are in the HIV/TB category, and further that this imbalance is particularly pronounced in the second period (1998–2002) when many more people were becoming sick with AIDS. Table II lists the number of deaths by sex, period, age, and cause category, and Figure 3 summarizes the counts presented in Table II to display the percentage of total deaths within each sex, period, and age group that are HIV related according to migrant status category. The fraction of HIV-related deaths in the short-term returning migrants category goes from nearly zero during the first period to between 10% and 25% in the second period, with the largest increase in the 40–59 year age group. Figure 4 presents the percentage of total deaths in each sex, period, age, migrant-status group that are attributable to HIV/TB. This clearly reveals that HIV/TB is growing rapidly as a cause in all sex, period, age, migrant-status groups, and that the migrant-status group with the greatest growth in the fraction of deaths attributable to HIV/TB is short-term returning migrants.
Table II.
Deaths by sex, period, age, cause and migration status: 1992–2002.
| Returning migrants |
|||||||
|---|---|---|---|---|---|---|---|
| Cause | Residents | Short | Long | Total | |||
| Female | Early period, 1992–97 | Ages 20–39 | HIV/TB | 28 | 1 | 0 | 29 |
| NCD | 13 | 2 | 0 | 15 | |||
| External | 4 | 0 | 0 | 4 | |||
| Other | 75 | 0 | 0 | 75 | |||
| Total | 120 | 3 | 0 | 123 | |||
| Ages 40–59 | HIV/TB | 9 | 0 | 0 | 9 | ||
| NCD | 33 | 0 | 0 | 33 | |||
| External | 10 | 0 | 0 | 10 | |||
| Other | 50 | 2 | 0 | 52 | |||
| Total | 102 | 2 | 0 | 104 | |||
| Ages 60–79 | HIV/TB | 9 | 0 | 0 | 9 | ||
| NCD | 97 | 2 | 0 | 99 | |||
| External | 3 | 0 | 0 | 3 | |||
| Other | 148 | 5 | 0 | 153 | |||
| Total | 257 | 7 | 0 | 264 | |||
| Late period, 1998–2002 | Ages 20–39 | HIV/TB | 148 | 27 | 3 | 178 | |
| NCD | 16 | 1 | 1 | 18 | |||
| External | 4 | 0 | 0 | 4 | |||
| Other | 117 | 19 | 4 | 140 | |||
| Total | 285 | 47 | 8 | 340 | |||
| Ages 40–59 | HIV/TB | 47 | 14 | 0 | 61 | ||
| NCD | 43 | 5 | 0 | 48 | |||
| External | 3 | 1 | 0 | 4 | |||
| Other | 112 | 10 | 1 | 123 | |||
| Total | 205 | 30 | 1 | 236 | |||
| Ages 60–79 | HIV/TB | 6 | 1 | 1 | 8 | ||
| NCD | 93 | 4 | 0 | 97 | |||
| External | 2 | 0 | 0 | 2 | |||
| Other | 155 | 6 | 3 | 164 | |||
| Total | 256 | 11 | 4 | 271 | |||
|
| |||||||
| Male | Early period, 1992–97 | Ages 20–39 | HIV/TB | 33 | 1 | 0 | 34 |
| NCD | 6 | 0 | 0 | 6 | |||
| External | 37 | 0 | 0 | 37 | |||
| Other | 110 | 4 | 0 | 114 | |||
| Total | 186 | 5 | 0 | 191 | |||
| Ages 40–59 | HIV/TB | 44 | 2 | 0 | 46 | ||
| NCD | 47 | 0 | 0 | 47 | |||
| External | 22 | 0 | 0 | 22 | |||
| Other | 109 | 8 | 0 | 117 | |||
| Total | 222 | 10 | 0 | 232 | |||
| Ages 60–79 | HIV/TB | 39 | 1 | 0 | 40 | ||
| NCD | 62 | 2 | 0 | 64 | |||
| External | 14 | 0 | 0 | 14 | |||
| Other | 151 | 5 | 0 | 156 | |||
| Total | 266 | 8 | 0 | 274 | |||
| Late period, 1998–2002 | Ages 20–39 | HIV/TB | 110 | 33 | 0 | 143 | |
| NCD | 6 | 0 | 0 | 6 | |||
| External | 32 | 2 | 0 | 34 | |||
| Other | 124 | 21 | 4 | 149 | |||
| Total | 272 | 56 | 4 | 332 | |||
| Ages 40–59 | HIV/TB | 81 | 29 | 1 | 111 | ||
| NCD | 23 | 4 | 1 | 28 | |||
| External | 14 | 3 | 1 | 18 | |||
| Other | 116 | 30 | 2 | 148 | |||
| Total | 234 | 66 | 5 | 305 | |||
| Ages 60–79 | HIV/TB | 27 | 4 | 1 | 32 | ||
| NCD | 62 | 15 | 4 | 81 | |||
| External | 1 | 1 | 0 | 2 | |||
| Other | 130 | 28 | 7 | 165 | |||
| Total | 220 | 48 | 12 | 280 | |||
In total, 12.0% of all deaths aged 20–79 in 1992–2002 do not have a coded cause. These deaths (354 of 2,952) are classified in the Other category. There are an additional 664 deaths for which it was not possible to assign a cause, making up 22.5% of the total 2,952. These deaths are also in the Other category.
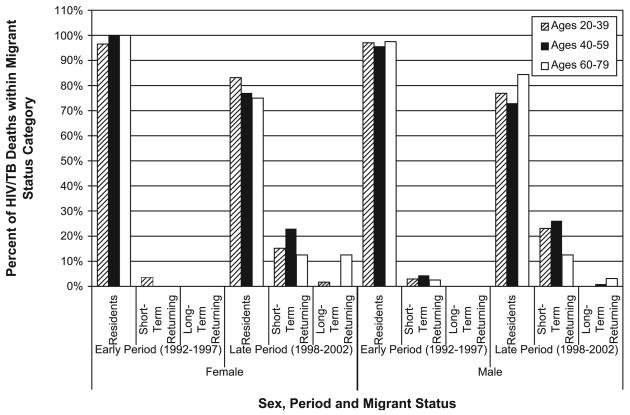
Figure 3.
Percentage of HIV/TB deaths by sex, period, migrant status and age (sums to 100% across resident statuses within each period). The distribution of HIV/TB deaths among migrant status categories within each sex–period category is displayed. Comparing the second to the first period clearly reveals a shift in the distribution of HIV/TB deaths across migrant status categories with a much larger fraction of HIV/TB deaths among short-term returning migrants in the second period 1998–2004 for both sexes and all ages, but most notably for ages 40–59.
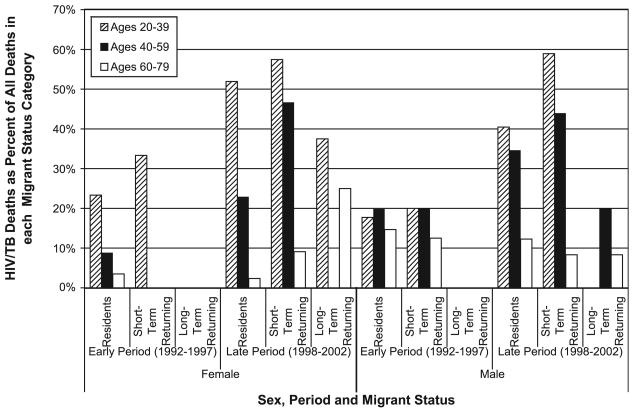
Figure 4.
HIV/TB deaths as a percentage of total deaths in each migrant status category by sex, period, and age. Within each sex–period–migrant status category the percentage of all deaths that are HIV related is displayed. This percentage increases between the first and second periods for all sex–migrant status categories. By far the largest increases are for young (20–59) short-term returning migrants, and especially for females.
Discussion
The aim of the study is to highlight a phenomenon that has recently been exacerbated by the HIV/AIDS epidemic, namely migrant workers curtailing their employment and returning when ill to their rural homes. This is occurring in a socioeconomic context that is characterized by high levels of labor migration among men and rapidly increasing levels among women.
The healthy worker hypothesis conceptualizes migrants as possessing higher levels of motivating qualities like education, health, or access to resources. A study of migration and child mortality in Agincourt showed that better educated women were simultaneously more likely to become temporary migrants and to experience lower risks of mortality in their children [23]. Another Agincourt-based study of circular migration and socioeconomic status showed that temporary migration was positively correlated with ownership of modern assets in the rural household, although negatively related to ownership of livestock assets [6]. Temporary migration thus seems to confer advantages on households but the fact remains that the advantage may be inherent in those persons who are prone to migrate. This bears out the “healthy worker” hypothesis but with a new and tragic twist – that migrants returning to their rural homes when they are sick or dying create a healthcare burden in those rural areas. In fact there is a double loss because dying family members are likely to be the most advantaged in terms of human capital and thus also bread-winners for their households.
Recent literature on the link between circular migration and increased risk of infection with HIV [2,28] describes the impact of migration on rural, “sending” communities. It has been assumed that circular migration causes HIV to spread when migrants infected at their place of work return to their rural homes, but in a recent study migrant couples were shown to be significantly more likely to be HIV discordant than non-migrant couples, and in nearly one-third of all HIV-discordant couples it was the stay-at-home female partner who was HIV infected [29]. Lurie describes how focusing on migrants as the only high-risk group disregards the situation of the many community members who are not migrants but are nonetheless directly and intimately made vulnerable by migration. This advances our understanding of the impact of migration on HIV transmission by recognizing that migration affects both “home” and “away” communities simultaneously. In a similar way the ties between the migrant and “home” community are key to understanding where the burdens of illness and healthcare are experienced. Communities with a high prevalence of absent migrants as well as HIV infection are made vulnerable both to HIV transmission, via the migrant or the home-based partner, and to an increased experience of AIDS-related illness, by compounding the presence of illness in non-migrants with that of short-term returning migrants.
This study shows that in the context of ongoing circular labour migration in South Africa, return migration back to rural homes is associated with advancing illness and death, particularly from HIV/AIDS, which is adding an extra burden to families and health systems in rural areas. The returning home to die phenomenon is associated with loss of household income (through cessation of remittances), increased household health expenditure (for healthcare and funerals), and further loss of household (and community) income given the high opportunity cost of caring for a severely ill person. There is also the effect of additional patient and cost burdens being placed on already strained rural health systems.
Public sector services like health, education, and social welfare need to respond more effectively to the special needs of highly mobile populations and their home communities. A prime example is the responsibility facing the public health service; district and provincial systems require extra resources if they are to mount a proper response. This study provides evidence for the argument that the former “homeland” populations are now supporting a major and growing burden of sickness and death comprised of their members who formerly worked in the metropolitan, mining, and formal agricultural areas, and who return to their rural families when they are sick and dying.
Conclusion
The apartheid-linked history of sustaining an adequate supply of low-cost labour in South Africa implies that the rural populations played a crucial role in supporting the growth of the largest economy on the African continent. Long-standing inequities are part of the reason that former homeland communities remain underserved and deeply reliant on circular labor migration. Migration has now brought an attendant health risk of its own. This paper describes the influx of sick and dying migrants moving back to the rural areas from which they migrated. Rural communities are already exposed to multi-partner sexual networks as a result of labor migration. Even without the elevated mortality of returning migrants, an increased mortality burden associated with the HIV/AIDS epidemic is pervasive in the non-migrant community. For this reason, the addition of seriously sick people in the community could not come at a worse time for the resident individuals, households, social networks, community institutions, and public services.
Acknowledgements
This work has been supported, in part, by NIA grants R37 AG10168, R37 AG10168-09S2, P30 AG17248 and P30 AG17248-03 and by the Wellcome Trust, UK grant 058893/Z/99/A, the Andrew W. Mellon Foundation, USA, the University of the Witwatersrand and the Medical Research Council, South Africa. Ethical clearance for the Agincourt HDSS has been granted by the University of the Witwatersrand's Committee for Research on Human Subjects (Medical) (No. M960720).
Footnotes
Publisher's Disclaimer: This article may be used for research, teaching and private study purposes. Any substantial or systematic reproduction, re-distribution, re-selling, loan or sub-licensing, systematic supply or distribution in any form to anyone is expressly forbidden.
The publisher does not give any warranty express or implied or make any representation that the contents will be complete or accurate or up to date. The accuracy of any instructions, formulae and drug doses should be independently verified with primary sources. The publisher shall not be liable for any loss, actions, claims, proceedings, demand or costs or damages whatsoever or howsoever caused arising directly or indirectly in connection with or arising out of the use of this material.
This paper has been independently peer-reviewed according to the usual Scand J Public Health practice and accepted as an original article.
References
- 1.Crush J, James W. Crossing boundaries: Mine migrancy in a democratic South Africa. Institute for Democracy in South Africa; Johannesburg: 1995. [Google Scholar]
- 2.Lurie M. Migration and AIDS in Southern Africa: A review. S Afr J Sci. 2000:96. [Google Scholar]
- 3.Hallett R. Desolation on the Veld: Forced removals in South Africa. African Affairs. 1984;83:301–20. [Google Scholar]
- 4.Tollman SM, Kark SL, Kark E. The Pholela Health Centre: Understanding health and disease in South Africa through community-oriented primary care. In: Das Gupta M, Aaby P, Garenne M, Pison G, editors. Prospective community studies in developing countries. Clarendon Press; Oxford: 1997. [Google Scholar]
- 5.Gelderblom D, Kok P. Dynamics, vol. 1: Urbanization: South Africa's challenge. HSRC Publishers; Pretoria: 1994. [Google Scholar]
- 6.Collinson MA, Tollman SM, Kahn K, Clark SJ, Garenne M. Highly prevalent circular migration: Households, mobility and economic status in rural South Africa. In: Tienda M, Findley SE, Tollman S, Preston-Whyte E, editors. Africa on the move: African migration and urbanisation in comparative perspective. University of the Witwatersrand Press; Johannesburg: 2006. [Google Scholar]
- 7.Jochelson K, Mothibeli M, Leger JP. Human immunodeficiency virus and migrant labor in South Africa. Int J Health Serv. 1991;21:157–73. doi: 10.2190/11UE-L88J-46HN-HR0K. [DOI] [PubMed] [Google Scholar]
- 8.Nunn AJ, Wagner HU, Kamali A, Kengeya-Kayondo JF, Mulder DW. Migration and HIV-1 seroprevalence in a rural Ugandan population. AIDS. 1995;9:503–6. [PubMed] [Google Scholar]
- 9.Pison G, Le Guenno B, Lagarde E, Enel C, Seck C. Seasonal migration: A risk factor for HIV infection in rural Senegal. J Acquir Immune Defic Syndr. 1993;6:196–200. [PubMed] [Google Scholar]
- 10.Decosas J, Kane F, Anarfi JK, Sodji KD, Wagner HU. Migration and AIDS. Lancet. 1995;346:826–8. doi: 10.1016/s0140-6736(95)91631-8. [DOI] [PubMed] [Google Scholar]
- 11.Quinn TC. Population migration and the spread of Types 1 and 2 Human Immunodeficiency virus. PNAS. 1994;91:2407–14. doi: 10.1073/pnas.91.7.2407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abdool Karim Q, Abdool Karim SS, Singh B, Short R, Ngxongo S. Seroprevalence of HIV infection in rural South Africa. AIDS. 1992;6:1535–9. doi: 10.1097/00002030-199212000-00018. [DOI] [PubMed] [Google Scholar]
- 13.Lurie MN, Harrison A, Wilkinson D, Abdool Karim SS. Circular migration and sexual networking in rural KwaZulu-Natal: Implications for the spread of HIV and other sexually transmitted diseases. Health Transition Rev. 1997;17(Suppl 3):17–27. [Google Scholar]
- 14.Evian C. AIDS and Social Security. AIDS Scan. 1995;7:8–11. [Google Scholar]
- 15.Dladla AN, Hiner CA, Qwana E, Lurie MN. Speaking to rural women: The sexual partnerships of rural South African women whose partners are migrants. Society in Transition. 2001:32. [Google Scholar]
- 16.Tollman S, Herbst K, Garenne MJ, Gear SS, Kahn K. The Agincourt Demographic and Health Study: Site descriptions, baseline findings and implications. South Afr Med J. 1999;89:858–64. [PubMed] [Google Scholar]
- 17.Collinson MA, Mokoena O, Mgiba N, Kahn K, Tollman SM, Garenne M, Shackleton S, Malomane E. Agincourt Demographic Surveillance System (Agincourt DSS) In: Sankoh O, Kahn K, Mwageni E, Ngom P, Nyarko P, editors. Population and Health in Developing Countries. Vol 1: Population, Health and Survival at INDEPTH sites. International Development Research Centre; Ottawa: 2002. [Google Scholar]
- 18.Marsh DR, Fikree FF. Verbal autopsy: An alternate technique for assigning cause of death. J Pak Med Assoc. 1994;44:178–9. [PubMed] [Google Scholar]
- 19.Snow RW, Armstrong JRM, Forster D, Winstanley MT, Marsh VM, Newton CRJC, Waruiru C, Mwangi I, Winstanley PA, Marsh K. Childhood deaths in Africa: Uses and limitations of verbal autopsies. Lancet. 1992;340:351–5. doi: 10.1016/0140-6736(92)91414-4. [DOI] [PubMed] [Google Scholar]
- 20.Mirza NM, Macharia WM, Wafula EM, Agwanda RO, Onyango FE. Verbal autopsy: A tool for determining cause of death in a community. East Afr Med J. 1990;67:693–8. [PubMed] [Google Scholar]
- 21.Chandramohan D, Maude GH, Rodrigues LC, Hayes RJ. Verbal Autopsies for Adult Deaths: Issues in their Development and Validation. Int J Epidemiol. 1994;23:213–22. doi: 10.1093/ije/23.2.213. [DOI] [PubMed] [Google Scholar]
- 22.Kamali A, Wagner HU, Nakiyingi J, Sabiiti I, Kengeya-Kayondo JF, Mulder DW. Verbal autopsy as a tool for diagnosing HIV-related adult deaths in rural Uganda. Int J Epidemiol. 1996 Jun;25(3):679–84. doi: 10.1093/ije/25.3.679. [DOI] [PubMed] [Google Scholar]
- 23.Collinson MA. Health impacts of social transition: A study of female temporary migration and its impact on child mortality in rural South Africa. University of the Witwatersrand; Johannesburg: 2007. MSc dissertation. [Google Scholar]
- 24.Allison P. Discrete-time methods for the analysis of event histories. In: Leinhardt S, editor. Sociological methodology. Jossey-Bass; San Francisco: 1982. pp. 61–98. [Google Scholar]
- 25.Anon . Event history analysis: Regression for longitudinal event data. Sage Publications; Beverly Hills, CA: 1984. [Google Scholar]
- 26.Petersen T. Analysis of event histories. In: Sobel ME, editor. Handbook of statistical modeling for the social and behavioral sciences. Plenum Press; New York: 1995. pp. 453–517. [Google Scholar]
- 27.Tollman SM, Kahn K, Garenne M, Gear JSS. Reversal in mortality trends: evidence from the Agincourt field site, South Africa, 1992–1995. AIDS. 1999;13:1091–7. doi: 10.1097/00002030-199906180-00013. [DOI] [PubMed] [Google Scholar]
- 28.Wolff B, Collinson MA, Tollman SM. The impact of labour migration on sexual behaviour in a rural sending area in South Africa: Results from the Agincourt male labour migration study. Under review. [Google Scholar]
- 29.Lurie MN, Williams BG, Zuma K, Mkaya-Mwamburi D, Garnett G, Sturm AW, Sweat MD, Gittelsohn J, Abdool Karim SS. The impact of migration on HIV-1 transmission in South Africa: A study of migrant and nonmigrant men and their partners. Sex Transm Dis. 2003;30:149–56. doi: 10.1097/00007435-200302000-00011. [DOI] [PubMed] [Google Scholar]