Abstract
This report presents a conceptual approach to assessing skills of family caregivers for persons with Alzheimer’s disease and recommends next steps for development of this science. Researchers used multiple methods to develop a conceptual strategy for assessing family caregiver skills. Study participants included clinical/outreach staff from an Alzheimer’s Disease Center, nursing faculty with expertise in dementia care, and family caregivers. Mixed methods contributed to the conceptual clarification of caregiving skill and to the development of three approaches to assessing caregiver skill: caregiver self report, clinician assessment, and direct observational assessment. Caregiver effectiveness has the potential to affect the process of caregiving and outcomes for the person with dementia and caregiver.
Keywords: Alzheimer’s Disease, Family Caregiver Effectiveness, Measurement Development
Introduction
Maintaining family caregiver function has major implications for the person with Alzheimer’s disease (AD), the caregiver, and society as a whole. When family caregivers function well, care receivers experience decreased behavioral symptoms of dementia, improved care and quality of life 1, 2. Family caregivers stand to benefit by experiencing less strain and higher levels of mental and physical health 3, 4. When caregivers appraise their situation more positively, they are less likely to institutionalize their relative and more likely to continue providing in-home care 5. This can translate into lower long-term care costs to society, as nursing home placement constitutes a major component of public health care costs attributed to AD 6 ; and because our current long term care system is unable to absorb the value of unpaid care provided by family members, which approaches 350 billion dollars annually 7.
Family caregiver research has primarily focused on the relationship between care-related demands (disease symptoms and severity) and caregiver psychological and physical health. Surprisingly little is known about caregiver skills in responding to the care recipient’s disease-related disabilities. Behavioral skills of caregivers are particularly important in providing care for people with a dementia syndrome like AD. By the middle stages of the disease, most affected persons require substantial assistance with instrumental and physical activities of daily living, and experience behavioral and emotional symptoms.
Research on family caregiver skills is in its infancy, as there are few known measures of caregiver skill. Gitlin and colleagues used the caregiver self-report Task Management Strategy Index (TMSI) to test the effectiveness of a Home Environmental Skill-building Program (ESP). Desired skills focused on problem-solving and technical skills (task simplification, communication) and home modifications 8–10. At six months caregivers in the treatment intervention reported significantly improved skills, less need for help providing assistance and fewer care receiver problem behaviors; at twelve months caregiver affect improved, with a trend toward maintenance of caregiver skills and reduced care recipient behavioral occurrences 9. A number of other studies tested skill training interventions in which they used proxy measures to assess caregiver skill. One intervention focused on caregiver behavior management skills, problem solving skills and cognitive restructuring. Assessment focused on caregiver self-reported frequency of and distress with behavioral symptoms associated with dementia and positive aspects of caregiving 11. Another intervention focused on anger and depression management skills and used measures of anger, hostility and depression as outcomes 12.
In our own research we initially developed and tested a 60-item assessment of caregiver skill in dealing with behavioral symptoms of dementia 13. This measure was shortened to a 30-item measure and subsequently used in a clinical trial 14. To minimize future participant burden and focus on behavioral symptoms of agitation and aggression, an abbreviated measure of skill building items was developed (Behavior Management Scale Revised [BMS-R]) (15 items) 14–16. Findings suggested that caregivers were able to complete a self-report measure of caregiving skill; that both the 30- and 15-item versions of this measure had acceptable psychometric characteristics; and caregiver skill as a construct appeared to be multidimensional and sensitive to change over time. Limitations of this measure were that it focused on selected behavioral symptoms of dementia and the response format focused on level of agreement with items as opposed to caregiver assessment of their own behavioral skill. Collectively these studies support the growing body of literature which suggests that skill building interventions are effective in improving caregiver appraisal, coping strategies and mental health outcomes 17.
Several other methods of assessing skill are also reported and include: clinician assessment and direct observation. Qualitative research conducted with caregivers of persons with dementia and caregivers of persons with cancer suggest that clinicians are well-equipped to identify the complex processes involved in assessing caregiver skill 18–20. A major limitation of the existing literature is that no known clinician assessment measures of dementia family caregiver skill exist.
Real-time behavioral observations are often viewed as the “gold standard” for understanding behavior. They are designed to capture qualitative information about a situation and also include a rating scale that summarizes strengths and weaknesses of the participant 21. Limitations include time and costs, as the behaviors of interest may not occur during the observational period; intrusiveness, and the potential for modifying behaviors of interest when an observer is present 22. Real-time observations in dementia care have most commonly been used to assess resident and/or staff behaviors and interactions in long term care settings 23, 24. No known direct behavioral observations have been used with dementia family caregivers who provide home-based care.
The purpose of this study was to further refine the concept of family caregiver skill and develop conceptually-based assessments for use with dementia family caregivers using three approaches – caregiver self-report, clinician rating, and direct behavioral observation.
Design and Methods
Study methods included focus groups and ongoing feedback from professionals and family caregivers. Study participants included clinical and outreach staff from a large Midwestern Alzheimer’s Disease Center, nursing faculty who have expertise in dementia care and research, and caregiver support group participants.
Conceptual clarification of family caregiver skill
A series of focus groups and individual interviews were conducted with clinical and outreach staff for the purpose of refining the concept of caregiver skill with a major focus on caregiver skills concerning behavioral symptoms of dementia. Behavioral symptoms of dementia were selected because these symptoms have consistently been shown to create greatest distress for family caregivers and if unabated, lead to earlier nursing home placement 25–27. Six professional females participated in three focus groups and/or individual follow-up interviews. The majority of participants ranged in age from 40–59 years (83%) and were Caucasian (67%). They represented three areas of practice: nurse practitioner (33%), social worker (33%), and multicultural outreach worker/ community educator (33%). The majority had from 10–25 years of clinical experience with family caregivers of persons with dementia (83%).
Two co-investigators conducted the focus groups, one serving as the group facilitator and the other as recorder. In the initial focus group comments were recorded on a flip-chart throughout the discussion and were summarized in a typed transcript. A transcript that included the initial focus group discussion was reviewed and coded by one co-investigator for common themes, using qualitative content analysis 28 , and verified by the second co-investigator. Once data were integrated they supported a model of Caregiver Skill Building/Effectiveness. Researchers shared the proposed model in another focus group with original focus group participants and nursing faculty who were involved in family caregiver research. Both groups made suggestions to further refine this model.
Development/refinement of caregiver skill measures
Three alternative approaches to assessing family caregiver skill/effectiveness were developed: caregiver self-report, clinician rating, and in-person direct observational assessment. Focus group data, existing literature and measures were used to draft content and specify approaches for each measure. Ongoing individual interviews and a third focus group was conducted with clinical staff. Using their input, measures were refined over a period of four months. Proposed measures and procedures were validated with family caregiver researchers.
Results
Conceptual clarification of caregiver skill
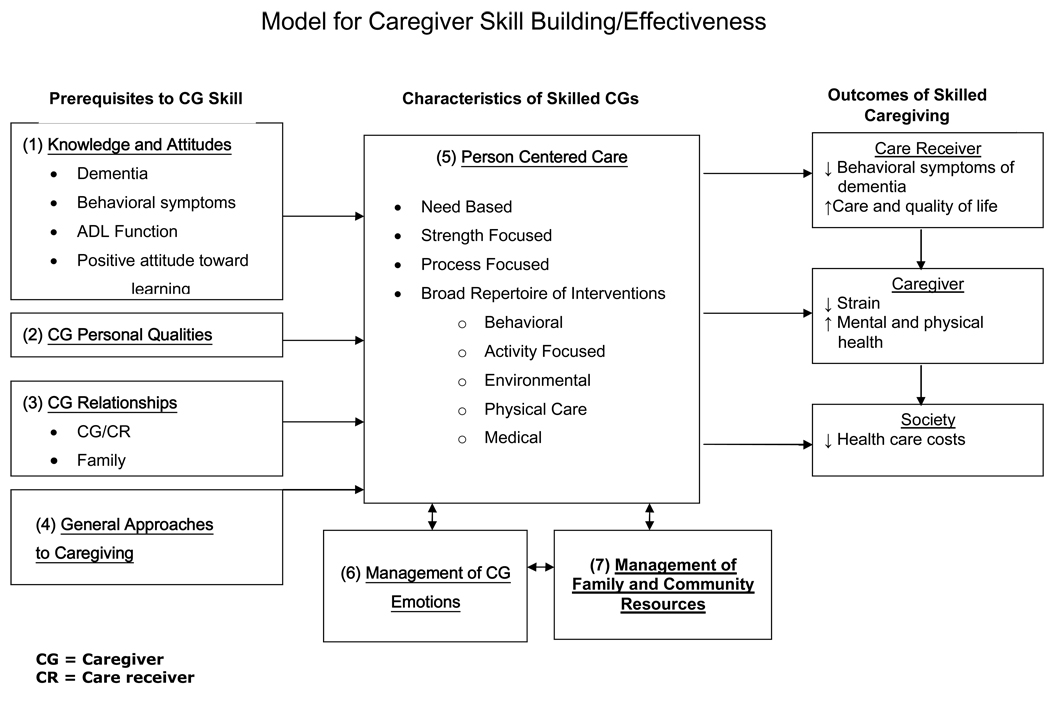
Focus group data and follow-up interviews with staff suggested that a Model of Caregiver Skill Building/Effectiveness included seven central constructs (Figure 1). Prerequisites to caregiver skill focused on: Knowledge, Caregiver Qualities, Caregiver Relationships and General Approaches to Caregiving.
Figure 1.
Model for Caregiver Skill Building/Effectiveness
Knowledge about dementia, behavioral symptoms of dementia, activities of daily living function, and positive attitudes toward learning about caregiving responsibilities were viewed as being essential to skill development.
Caregiver Qualities such as insight, commitment, honesty with themselves, creativity, flexibility, persistence, patience, sense of humor, ability to reframe experiences or circumstances, ability to make decisions, and analytical abilities were viewed as being readily apparent with skilled caregivers. Skilled caregivers were described as having a broad repertoire of qualities that assist them in dealing with caregiving activities; are goal directed, and integrate their personal style in their caregiving approaches. They have intuition, introspective abilities, insight and observe when “things are not right.” They are flexible in approaching life and their changing caregiving responsibilities throughout the disease process. They are able to “roll with the punches.” Skilled caregivers are able to reframe their experience and talk more about “blessings than burdens.” They analyze situations carefully, are creative problem solvers, and modify their behavior or the situation accordingly. Less skilled caregivers have a limited repertoire of qualities and may be more rigid or inconsistent in capitalizing on their own strengths. Less skilled caregivers have more difficulty seeing options, changing their roles as impaired family member needs change, are less flexible, more inconsistent and more rigid in their expectations and interpretations. They are more resistant to trying new approaches and are more likely to get “bogged down” by caregiving responsibilities.
Caregiver Relationships including the past and current relationship between the caregiver and impaired family member, and other family members were also viewed as prerequisites to caregiving effectiveness. Skilled caregivers are more likely to have “received something positive” from their impaired family member in the past. Skilled caregivers capitalize on past family relationships, maintain open communication with family members, are creative in getting their help, and flexible in negotiating alternatives. Less skilled caregivers have often had a “stormier” past relationship with their impaired family member or one that negatively affects how they perceive, interact and/or intervene with their family member (i.e., experiences with alcoholism). As a result, their extended family may be less supportive with poorer patterns of communication. Less skilled caregivers have more difficulty negotiating their personal and family needs, along with their caregiving responsibilities.
General approaches to caregiving referred to the caregiver’s ability to handle the day to day tasks required to take care of a person with dementia. These approaches included: knowing the family member’s strengths and limitations, focusing on the family member’s current needs, knowing how to make basic requests to the family member, and in general assisting the family member to have a fulfilling quality of life. Skilled caregivers are more likely to be proactive in the care of their family member, focusing on their cognitive and physical strengths rather than their weaknesses. These caregivers have a vast collection of creative ideas for day-to-day care which incorporate the well-being of the family member, rather than the caregiver’s needs or wants. They also allow their family member to make choices and remain engaged when appropriate, rather than always instructing the family member on the “right” way. Skilled caregivers focus on those things their family can still do, rather than what they have lost. They also do not focus on the past, but rather the current environment. Unskilled caregivers are more likely to be strict with their actions and behaviors and tend to view the day as something to “get through”.
The determining factors to identifying skilled versus less skilled caregivers focused on whether caregivers provide Person Centered Care, Manage their own Emotions, and Manage Family and Community Resources. Person Centered Care (PCC) was described as focusing on the impaired family member’s needs rather than the disease or the task, strengths rather than limitations, and the process rather than the outcome. PCC could be provided by the family caregiver or others and involves a broad repertoire of philosophical approaches and interventions. It addresses not only Maslow’s hierarchy of needs 29 but focuses on the “actualization in the moment.” The implication was that PCC would avert and prevent difficult behaviors associated with dementia. Interventions that supported PCC included a broad repertoire of approaches such as: behavioral, activity, environmental, provision of direct physical care, and attention to medical needs. Focus group participants suggested that skilled caregivers “know their impaired family member,” are more likely to draw upon positive caregiver qualities, provide “just right challenges” for the impaired family member, function as a “detective,” have certain standards, and accept the impaired family member “as is.” They assess their impaired family members’ strengths, set realistic expectations, and work around their limitations. They know when to “step in” and do not create “excess disability.” They think of care as an activity versus a task; they normalize activities and involve their family member in daily life. Less skilled caregivers are more likely to focus on the disease rather than the person, what their family member “can’t do” rather than what they “can do.” They are more likely to provide task-centered, scheduled care, and have more difficulty setting appropriate limits. They have more difficulty understanding the connections between the disease, behavior, and caregiver interactions, and have fewer interventions in their repertoire.
Focus group participants suggested that management of Caregiver Emotions was another component of caregiver skill and that current emotional status could influence effectiveness but didn’t necessarily mean caregivers had less potential for skill development. They readily identified that caregiving was stressful, using descriptors commonly seen in the caregiver literature such as burdened, overwhelmed, depressed, grieving and angry 30. They suggested that skilled caregivers use “higher order” skills and perceptions, build upon character strengths developed through prior difficult experiences, accept their life situation at some level and integrate these experiences into their “life platter.” They have the ability to reframe life experiences, are more likely to balance the caregiving process with their own self-care needs; and “move on” at some level to transform this difficult experience into something that is manageable and positive by drawing upon their sense of spirituality, finding meaning, or investing in others. Less skilled caregivers have more difficulty accepting “what is,” are more overwhelmed, tend to get “more bogged down” by emotions, resist adapting their attitudes and vigorously “resist the inevitable.” Their feelings and past history may interfere with the care they provide. For example, one staff member described a situation where the impaired husband and caregiver wife had frequently ‘bickered’ in the past. The wife expected this type of relationship to continue in the present and kept ‘badgering’ the husband. When he was more apathetic and did not respond as he had in the past she continued trying to ‘provoke’ him.. After a support group meeting when she said, “I finally realized it’s me who has to change” staff found that she became less confrontational in the relationship with her husband.
Management of Family and Community Resources was identified as an additional needed skill. Skilled caregivers are successful in “marshalling” resources, open to resource possibilities, receptive to seeking out support and input from others, know how to get information about available resources, navigate the system, and how to negotiate what they need from outside resources. They view other family members and service providers as potential collaborators rather than competitors and understand that care provided by others may be the “best care.” They use multiple resources and approaches and may have to make a “leap of faith” in using resources such as adult day care. Less skilled caregivers may have had ‘stormier’ past family relationships, are more closed to exploring resources, less receptive to seeking out and accepting help from others, less knowledgeable about how to acquire information about resources, and have more difficulty negotiating with family members and/or service providers. They may feel they are the only one who can provide care and may be tied to past promises “never to place their family member in adult day care or in a nursing home.”
The outcomes of this proposed model are multidimensional, including potential Care receiver, Caregiver, and Societal Outcomes. These proposed outcomes have been identified in the existing dementia family caregiving literature 1, 3, 7, 30, 31
Development of a conceptual model to guide measurement strategies
Using our conceptual model seen in Figure 1, we identified key conceptual categories that should be reflected in skill building measures (See Table 1).
Table 1.
Blueprint of Conceptual Categories by Assessment Method and Number of Proposed Items
| Conceptual Categories in Each Measure | Number of Proposed Items by Assessment Method | |||
|---|---|---|---|---|
| CABS-SRa | CABS-PRLb | CABS-PRSc | CABS—DOd | |
| Knowledge and Attitudes toward Learning | 5 | 4 | ||
| Caregiver Personal Qualities | 6 | 7 | 1 | 1 |
| Caregiver Relationships | 2 | 2 | 1 | 1 |
| General Approaches to Caregiving | 11 | |||
| Providing Person Centered Care | 45 | 7 | 4 | 1 |
| Managing Caregiver Emotions | 4 | 5 | 1 | 1 |
| Managing Family and Community Resources | 1 | 2 | ||
| Overall Effectiveness | 1 | 1 | 2 | 2 |
| Total Items | 75 | 28 | 9 | 6 |
CABS—SR: Caregiver Assessment of Behavioral Skill-Self Report
CABS—PRL: Caregiver Assessment of Behavioral Skill-Professional Long Form
CABS—PRS: Caregiver Assessment of Behavioral Skill-Professional Short Form
CABS—DO: Caregiver Assessment of Behavioral Skill-Direct Observation
Development/refinement of caregiver self report skill measure
The Caregiver Assessment of Behavioral Skill—Self Report measure (CABS—SR) was developed by using selected items from the Caregiver Skill Building measure used in our prior study 14 ; identifying additional items that represented skill prerequisites and characteristics of skilled caregivers (Figure 1); and using existing literature on behavioral symptoms of dementia (i.e., memory-related, affective/depressive, psychotic, aggressive/agitated, approaches during personal care) 21, 32, 33. The following challenges were faced in constructing the proposed measure: 1) the need to convey both the context of a care receiver’s symptom and identify potential skilled/ less skilled caregiver responses to these symptoms (i.e., If my relative becomes anxious or worried I reassure him/her that everything will be okay; If my relative threatens to hurt him/herself or others, I put him/her in a locked room); 2) the need to identify a range of response formats that caregivers find realistic (i.e., 1=’I do not do this very well’ to 4=’I do this very well’ and 0=’Seldom true’ to 2=’True most of the time’); and 3) the realization that the proposed measure was best suited for caregivers of moderately impaired persons with dementia who have a range of cognitive, behavioral, and physical symptoms associated with dementia. Clinical staff and researchers reviewed multiple drafts of the proposed measure, resulting in refined item content and response format.
Five family caregivers also reviewed the proposed measure and responded by mail. Their comments suggested that the form was readable and easy to complete. The majority of these caregivers were male (60%), all were Caucasian and spouses ranging in age from 50–79 years, and had provided care from 5 months to 4 years. They described their family member as mildly impaired and rated themselves as having somewhat to moderately effective skills. Caregivers who had provided care for a longer time identified fewer items as ‘not relevant’ to their situation. A final bank of 76 conceptually based items, thought to represent the scope of caregiver skills, was created (Table 1, Column 1).
Development of a clinician skill measure
Two nurse practitioners worked with the nurse co-investigator to develop the Caregiver Assessment of Behavioral Skill—Professional Long version (CABS—PRL). The nurse co-investigator initially developed a 28-item assessment (CABS—PRL; Table 1, Column 2) that reflected the six major concepts reflected in Figure 1. Responses to these items ranged from 1=Extremely limited to 4=Exceptionally effective. The major challenge reported by nurse practitioners in a busy clinical research setting was the length of the form and amount of time it would take to be knowledgeable about each content area. Over a 4-month period the group worked collaboratively to develop a 9-item professional short measure (CABS—PRS; Table 1, Column 3) that included 3 open-ended questions that identify behavioral symptoms of dementia that caregivers find most challenging and approaches caregivers use in responding to these behaviors. Six additional quantitative items determine clinicians’ assessment of skill level concerning caregiver: personal qualities, relationships, person centered care, management of caregiver emotions, management of family and community resources, and overall effectiveness. Response format to these items ranges from 1–4 (1= ‘Extremely limited effectiveness’ to 4=’Exceptional effectiveness’). It is recommended that the CABS—PRL long form be used in home care or other settings where professionals have extended contact with a family caregiver and the CABS—PRS short form be used when professionals have limited clinical time or contact with family caregivers.
Development of a direct observational assessment of caregiver behavioral skill
While the “gold standard” of measurement is often viewed as real-time behavioral observations we faced a number of challenges in developing the Caregiver Assessment of Behavioral Skill: Direct Observation version (CABS—DO). Namely: 1) would the behaviors of interest occur during a limited period of observation, 2) how would observers’ presence affect the impaired family member and their caregiver, and 3) did we have personnel and the budget to support this costly effort? We reviewed simulation literature 22, 34 to determine if this would be a reasonable alternative. Initially we used a DVD of 19 clinical scenarios extracted from a video series designed to teach family and professional caregivers how to manage behavioral symptoms of dementia 35. Seven family caregivers viewed these scenarios to rate the relevance to their own caregiving situation. The majority of these participants were female (86%), ranged in age from 50–69 years (86%), Caucasian (57%), adult child caregivers (71%), had provided care for 5–6 years (57%), and reported that these scenarios rarely occurred (M=1.82, Range 1=’not at all’ to 5=’almost all the time’). Several professionals also viewed these scenarios and concurred with family caregivers that these scenes were not relevant in home-based settings. In summary, major limitations of the video simulation approach included: lack of relevance of clinical situations to family caregivers, the need to have a television monitor and DVD capability readily available, and length of administration time. An important missing element was how to observe the actual interaction between the caregiver and impaired family member as portrayed by one clinician who said, “I learn a lot about a family by just seeing how they interact when they come to or leave the clinic.”
The proposed CABS—DO focuses on moderately impaired persons with probable/possible Alzheimer’s disease, those who require some assistance with activities of daily living (ADLs), but are still communicative and able to participate in their own care. This approach would not be appropriate for impaired family members with physical impairments such as blindness, stroke, paralysis or marked upper body tremors, or who have difficulty swallowing. With this version, family caregivers were asked to provide their impaired family member with instructions to perform three simple ADL tasks: drink from a cup, comb their hair, and put on a sweater or jacket. This is a modified approach to assessing impaired family member ADL function 36. We decided to focus on ADL function rather than behavioral symptoms for the following reasons: the difficulties of presenting behavioral symptoms in a simulated setting; the ease of presenting simple ADL tasks in a busy clinical setting; and this approach allowed us to examine a sample of impaired family member/caregiver interaction. Our guidelines called for two raters to assess the family member and caregiver using a 6-item scale (Table 1, Column 4). Family caregiver skill was assessed by using identical quantitative items and response format proposed in the CABS—PRS short assessment (1=’Extremely limited effectiveness’ to 4=’Exceptional effectiveness’). Impaired family member ADL function was assessed using a 3 separate items with a rating scale from 1–4 (1=‘Unable to do’ to 4=’Independently completes task’), that are not part of the 6 items noted on Table 1, Column 4.
Discussion
Caregiver skills with persons who have Alzheimer’s disease can be broadly defined as a set of learned cognitive, behavioral, and emotional response strategies to disease symptoms of the affected individual. This definition has two key features. First, learning is specified as the basis for skill acquisition, highlighting the importance of caregiver experience with disease symptoms and the potential for modification. Second, the definition includes three interconnected response modalities: cognitive, behavioral and emotional response strategies. Caregiving skills have been described as going beyond mere information acquisition or knowledge building; as involving goal directed and well-organized behaviors that are a combination of an art, craft and science; and including complex behaviors that are well integrated, acquired over time and vary depending upon the caregiver 20.
The overall short-term measurement objectives were to obtain a clinically valid sample of caregiver responses that were indicative of family caregiver skill; and to develop multiple methods to assess family caregiver skill: Caregiver Self Report, Professional Assessment (Long and Short Forms), and Direct Observation. The caregiver self-report assessment focuses on typical patterns of caregiver response to behavioral symptoms in the home environment during the past month (CABS—SR). This method is inexpensive to implement and captures current skill levels in the most clinically meaningful setting, but can only be interpreted in the context of current behavioral symptom frequency and intensity. The two clinician rating methods can be used in different settings. The long professional measure (CABS—PRL) can be used in home care settings where professionals have extended contact with family caregivers. The short professional measure (CABS—PRS) can be used in busy clinical settings where nurse practitioners and/or social workers have limited caregiver contact. The direct observation assessment (CABS—DO) focuses on caregiver communication and responses to care receiver activities of daily living and potential behavioral responses. Although costly to implement, this method has the advantage of providing a standardized presentation of behavioral stimuli. Increased knowledge about these assessment methods will lay the foundation for more effective interventions that address family caregiver clinical needs over the course of the disease.
If caregiving skill can be improved it is likely that caregivers will function more effectively in their caregiving role. Improved caregiver function has the potential to improve care for the impaired family member, including such outcomes as decreasing behavioral symptoms of dementia and improving quality of life 1. Improved caregiver function may also reduce caregiver strain and improve caregiver mental and physical health 3, 4. These combined effects have the potential to increase length of time to care receiver nursing home placement 31 and decrease the long-term costs to society of providing this care 7.
Short-term research goals focused on determining if these three methods of assessing caregiver skill had content validity and were feasible. Long range research aims focus on: 1) Determining to what extent these three measures of caregiver skill are associated with: a) care receiver disease severity (cognitive impairment, behavioral symptoms of dementia, and activity of daily living impairment); b) caregiver characteristics such as: demographic variables, knowledge, personal qualities, and relationships with the care receiver and family members; and c) level of caregiver skill in providing person centered care, managing their emotions, and managing family and community resources. 2) Evaluating whether these measures have predictive validity and are able to predict care receiver and caregiver criterion measures such as care receiver behavioral symptoms of dementia, care and quality of life; caregiver perceived strain, and mental and physical health; and society costs related to care receiver institutionalization. It is hypothesized that caregivers with higher levels of skill development will express improved care receiver symptoms, care and quality of life; decreased caregiver strain and improved mental and physical health; and decreased health care costs, particularly related to institutionalization 7, 31. The next phase of our research will assess psychometric properties of these three skill building measures and degree of predictive validity of potential care receiver and caregiver outcomes.
The studies in this report contribute to the growing body of literature which suggest that the quality of caregiving, caregiver effectiveness, and caregiver skills ‘matter’ 9, 20, 37. It is hypothesized that caregiver effectiveness affects not only the process of caregiving but outcomes for both the impaired family member and caregiver 2, 38, 39 and may reduce long term care costs to society as a whole 7. A major limitation to moving this work forward has been the absence of standardized methods to assess family caregiver skill.
Acknowledgments
Grant Support National Institute of Nursing Research and National Institute on Aging R01 NR 04561, R01 NR 04903, P30 AG10161
The authors thank family caregivers, faculty at the Rush University College of Nursing, and staff at Rush Alzheimer’s Disease Center who have participated in various phases of this research program: Danielle Arends RN, GNP, Julie Bach, LCSW, MSW, Barbara Eubeler, Susan Frick, MSW, Karen L. Graham, MSEd, Dimitra Loukissa, PhD, RN, Olimpia Paun, PhD, RN, Suzanne Perraud, PhD, RN, Raj C. Shah, MD, Elanda Shannon, Pamela A. Smith, MEd, and Anna Treinkman, RN, ANP.
We would also like to acknowledge the significant contribution of Dr. David W. Gilley, to the conceptualization, analytic interpretation, and portions of drafted text of this manuscript.
Biographies
Carol J. Farran DNSc, RN, FAAN is Professor and Division Director of the PhD Graduate Program and The Nurses Alumni Association Chair in Health and the Aging Process in the College of Nursing, Rush University Medical Center.
Judith J. McCann, PhD, RN is a Professor in the College of Nursing and a Research Scientist with the Rush Institute for Healthy Aging at Rush University Medical Center.
Louis F. Fogg, PhD, is Assistant Professor at Rush University Medical Center’s College of Nursing as well as Assistant Professor in Behavioral Sciences and Nursing at Rush Medical College.
Caryn D. Etkin, PhD, MPH is a Project Manager in the College of Nursing at Rush University Medical Center.
Contributor Information
Carol J. Farran, Rush University College of Nursing, 600 S. Paulina Street, AAC 1080, Chicago, IL 60612, 312-942-6154, Carol_J_Farran@rush.edu.
Judith J. McCann, Rush University College of Nursing and Rush Institute for Healthy Aging, 1645 W. Jackson Blvd, Suite 615, Chicago, IL 60612, 312-942-3283, Judy_J_McCann@rush.edu.
Louis G. Fogg, Rush University College of Nursing, 600 S. Paulina Street, AAC 1080 Chicago, IL 60612, 312-942-6239, Louis_Fogg@rush.edu.
Caryn D. Etkin, Rush University College of Nursing, 600 S. Paulina Street, AAC 1080, Chicago, IL 60612, 312-942-5242, Caryn_Etkin@rush.edu.
REFERENCES
- 1.Belle SH, Burgio L, Burns R, et al. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: A randomized, controlled trial. Annals Intern Med. 2006;145:727–738. doi: 10.7326/0003-4819-145-10-200611210-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raia P. Habilitation therapy: A new starscape. In: Volicer L, Bloom-Charette L, editors. Enhancing the Quality of Life in Advanced Dementia. Philadelphia: Taylor & Francis; 1999. pp. 21–37. [Google Scholar]
- 3.Mittleman MS, Roth DL, Clay OJ, Haley WE. Preserving health of alzheimer caregivers: Impact of a spouse caregiver intervention. Am J Geriatr Psychiatry. 2007;15:780–789. doi: 10.1097/JGP.0b013e31805d858a. [DOI] [PubMed] [Google Scholar]
- 4.Schulz R, Beach SR. Caregiving as a risk factor for mortality: The caregiver health effects study. Journal of the American Medical Association. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 5.Gilley DW, Farran CJ, MCann J, Bienias JL, Evans DA. Efficacy of two psychosocial interventions on caregiver distress to dementia behavioral symptoms. The Gerontologist. 2005;45:616. [Google Scholar]
- 6.Ernst R, Hay JW. The US economic and social costs of alzheimer's disease revisited. American Journal of Public Health. 1994;84:1261–1264. doi: 10.2105/ajph.84.8.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gibson MJ, Houser A. Valuing the invaluable: A new look at the economic value of family caregiving. Washington, DC: AARP Public Policy Institute; 2007. [PubMed] [Google Scholar]
- 8.Gitlin LN, Winter L, Corcoran M, Dennis MP, Schinfeld S, Hauck WW. Effects of the home environmental skill-building program on the caregiver-care recipient dyad: 6-month outcomes from the philadelphia REACH initiative. The Gerontologist. 2003;43:532–546. doi: 10.1093/geront/43.4.532. [DOI] [PubMed] [Google Scholar]
- 9.Gitlin LN, Hauck WW, Dennis MP, Winter L. Maintenance of effects of the home environmental skill-building program for family caregivers and individuals with alzheimer's disease and related disorders. Journal of Gerontology: Medical Sciences. 2005;60A:368–374. doi: 10.1093/gerona/60.3.368. [DOI] [PubMed] [Google Scholar]
- 10.Gitlin LN, Corcoran M, Winter L, Boyce A, Hauk WW. A randomized, controlled trial of a home environmental intervention: Effect on efficacy and upset in caregivers and on daily function of persons with dementia. The Gerontologist. 2001;41:4–14. doi: 10.1093/geront/41.1.4. [DOI] [PubMed] [Google Scholar]
- 11.Burgio L, Stevens A, Guy D, Roth DL, Haley WE. Impact of two psychosocial interventions on white and african american family caregivers of individuals with dementia. The Gerontologist. 2003;43:568–579. doi: 10.1093/geront/43.4.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coon DW, Ory MG, Schultz R. Family caregivers: Enduring and emergent themes. In: Coon DW, Gallagher-Thompson D, Thompson LW, editors. Innovative Interventions to Reduce Dementia Caregiver Distress. New York: Springer Publishing Company; 2003. pp. 3–27. [Google Scholar]
- 13.Langham W, McCann JJ, Farran CJ. Psychometric analysis of the caregiver skill building scale. 2000 [Google Scholar]
- 14.Farran CJ, Gilley DW, McCann JJ, Bienias JL, Lindeman DA, Evans DA. Psychosocial interventions to reduce depressive symptoms of dementia caregivers: A randomized clinical trial comparing two approaches. Journal of Mental Health and Aging. 2004;10:337–350. [Google Scholar]
- 15.Farran CJ, McCann JJ, Bienias JL, Gilley D. Development and testing of a caregiver skill building measure. The Gerontologist. 2002;42(Special Issue I):339–340. [Google Scholar]
- 16.Farran CJ, Gilley DG, McCann JJ, Bienias JL, Lindeman DA, Evans DA. Efficacy of behavioral interventions for dementia caregivers. Western Journal of Nursing Research. 2007;29:944–960. doi: 10.1177/0193945907303084. [DOI] [PubMed] [Google Scholar]
- 17.Kennet J, Burgio L, Schulz R. Interventions for in-home caregivers: A review of research 1990 to present. In: Schultz R, editor. Handbook on Dementia Caregiving. New York: Springer Publishing Company; 2000. pp. 61–125. [Google Scholar]
- 18.Farran CJ, Loukissa D, Perraud S, Paun O. Alzheimer' s disease caregiving information and skills. part II: Family caregiver issues and concerns. Research in Nursing and Health. 2004;27:40–51. doi: 10.1002/nur.20006. [DOI] [PubMed] [Google Scholar]
- 19.Farran CJ, Loukissa D, Perraud S, Paun O. Alzheimer's disease caregiving information and skills. part I: Care recipient issues and concerns. Research in Nursing & Health. 2003;26:366–375. doi: 10.1002/nur.10101. [DOI] [PubMed] [Google Scholar]
- 20.Schumacher KL, Stewart BJ, Archbold PG, Dodd MJ, Dibble SL. Family caregiving skill: Development of the concept. Research in Nursing and Health. 2000;23:191–203. doi: 10.1002/1098-240x(200006)23:3<191::aid-nur3>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 21.Kielhofner G. Model of Human Occupation: Theory and Application. 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2002. [Google Scholar]
- 22.Gaba D, Howard SK, Flanagan B, Smith BE, Fish KJ, Botney R. Assessment of clinical performance duirng simulated crises using both technizal and behavioral ratings. Anesthesiology. 1998;89:8–18. doi: 10.1097/00000542-199807000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Burgio LD, Stevens AB. Behavioral interventions and motivational systems in the nursing home. In: Schulz R, M G, PL M, editors. Annual Review of Gerontology and Geriatrics. New York: Springer Publishing; 1999. pp. 284–320. [Google Scholar]
- 24.McCann JJ, Gilley DG, Hebert LE, Beckett LA, Evans DA. Concordance between direct observation and staff rating of behavior in nursing home residents with alzheimer's disease. Journal of Gerontology: Psychological Sciences. 1997;52B:P63–P72. doi: 10.1093/geronb/52b.2.p63. [DOI] [PubMed] [Google Scholar]
- 25.Danhauer SC, McCann J, Gilley D, Beckett L, Bienias JL, Evans D. Do behavioral disturbances in persons with alzheimer's disease predict caregiver depression over time? Psychology and Aging. 2004;19:198–202. doi: 10.1037/0882-7974.19.1.198. [DOI] [PubMed] [Google Scholar]
- 26.Gilley DW, Bienias JL, Wilson RS, Bennett DA, Beck TL, Evans DA. Influence of behavioral symptoms on rates of institutionalization for persons with alzheimer's disease. Psychological Medicine. 2004;34:1129–1135. doi: 10.1017/s0033291703001831. [DOI] [PubMed] [Google Scholar]
- 27.Hooker K, Bowman SR, Coehlo DP, et al. Behavioral change in persons with dementia: Relationships with mental and physical health of caregivers. Journal of Gerontology: Psychological Sciences. 2002;57B:P453–P460. doi: 10.1093/geronb/57.5.p453. [DOI] [PubMed] [Google Scholar]
- 28.Miles M, Huberman A. Qualitative Data Analysis. 2nd ed. Thousand Oaks: Sage Publications; 1994. [Google Scholar]
- 29.Maslow AH. A theory of human motivation. Psychological Review. 1943;50:370–396. [Google Scholar]
- 30.Lawton M, Moss M, Kleban M, Glicksman A, Rovine M. A two-factor model of caregiving appraisal and psychological well-being. Journal of Gerontology: Psychological Sciences. 1991;46:181–189. doi: 10.1093/geronj/46.4.p181. [DOI] [PubMed] [Google Scholar]
- 31.Mittleman MS, Haley WE, Clay OJ, Roth DL. Improving caregiver well-being delays nursing home placement of patients with alzheimer's disease. Neurol. 2006;67:1592–1599. doi: 10.1212/01.wnl.0000242727.81172.91. [DOI] [PubMed] [Google Scholar]
- 32.Kitwood T. Dementia Reconsidered: The Person Comes First. Philadelphia: Open University Press; 1997. [Google Scholar]
- 33.Teri L, Gibbons LE, McCurry SM, et al. Exercise plus behavioral management in patients with alzheimer disease. JAMA. 2003;290:2015–2022. doi: 10.1001/jama.290.15.2015. [DOI] [PubMed] [Google Scholar]
- 34.Boulet JR, Murray D, Kras J, Woodhouse J, McAllister J, Ziv A. Reliability and validity of a simulation-based acute care skills assessment for medical students and residents. Anesthesiology. 2003;99:1270–1280. doi: 10.1097/00000542-200312000-00007. [DOI] [PubMed] [Google Scholar]
- 35.Teri L. Managing and understanding behavior problems in alzheimer's disease and related disorders. Seattle: 1991. [Google Scholar]
- 36.Kuriansky JB, Gurland BJ, Fleiss JL. The assessment of self-care capacity in geriatric psychiatric patients by objective and subjective methods. Journal of Clinical Psychology. 1976;32:95–102. doi: 10.1002/1097-4679(197601)32:1<95::aid-jclp2270320129>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 37.Burgio LD, Solano N, Fisher SE, Stevens A, Gallagher-Thompson D. Skill-building: Psychoeducational strategies. In: Coon DavidW, Gallagher-Thompson Dolores, Thompson LarryW., editors. Innovative Interventions to Reduce Dementia Caregiver Distress. New York: Springer Publishing Company, Inc; 2003. pp. 119–138. [Google Scholar]
- 38.McClendon MJ, Smyth KA, Neundorfer MN. Long-term-care placement and survival of persons with alzheimer's disease. Journal of Gerontology: Psychological Sciences. 2006;61B:P220–P227. doi: 10.1093/geronb/61.4.p220. [DOI] [PubMed] [Google Scholar]
- 39.McClendon MJ, Smyth KA, Neundorfer MN. Survival of persons with alzheimer's disease: Caregiver coping matters. The Gerontologist. 2004;44:508–519. doi: 10.1093/geront/44.4.508. [DOI] [PubMed] [Google Scholar]