Abstract
Two mutant strains of Yersinia pestis KIM5+, a Δcrp mutant and a mutant with arabinose-dependent regulated delayed-shutoff crp expression (araC PBAD crp), were constructed, characterized in vitro, and evaluated for virulence, immunogenicity, and protective efficacy in mice. Both strains were highly attenuated by the subcutaneous (s.c.) route. The 50% lethal doses (LD50s) of the Δcrp and araC PBAD crp mutants were approximately 1,000,000-fold and 10,000-fold higher than those of Y. pestis KIM5+, respectively, indicating that both strains were highly attenuated. Mice vaccinated s.c. with 3.8 × 107 CFU of the Δcrp mutant developed high anti-Y. pestis and anti-LcrV serum IgG titers, both with a strong Th2 bias, and induced protective immunity against subcutaneous challenge with virulent Y. pestis (80% survival) but no protection against pulmonary challenge. Mice vaccinated with 3.0 × 104 CFU of the araC PBAD crp mutant also developed high anti-Y. pestis and anti-LcrV serum IgG titers but with a more balanced Th1/Th2 response. This strain induced complete protection against s.c. challenge and partial protection (70% survival) against pulmonary challenge. Our results demonstrate that arabinose-dependent regulated crp expression is an effective strategy to attenuate Y. pestis while retaining strong immunogenicity, leading to protection against the pneumonic and bubonic forms of plague.
Bubonic and pneumonic plague are zoonotic diseases endemic in many parts of the world, including the United States, and have resulted in over 200 million deaths over the course of human history (51). The etiological agent of plague is Yersinia pestis. Although the number of confirmed plague cases that occur worldwide has stabilized over the last 50 years at an average of about 1,700 per year, plague remains a serious public health threat in some regions of the world and outbreaks still occur (19). In addition to the potential for natural infections, Y. pestis is generally considered to be among the top five potential biological weapons (19). Recent efforts to create a safe and effective pneumonic plague vaccine have focused on the development of recombinant subunit vaccines that elicit antibodies against two well-characterized Y. pestis antigens, the F1 capsule and the virulence protein LcrV (2, 8, 40, 53). A plague vaccine based on live attenuated Y. pestis provides the theoretical advantage of simultaneously priming against many antigens, thereby greatly enhancing the likelihood of broad-based protection. In the past, live attenuated strains were generated by selection, rather than precise genetic manipulation, thus raising concern about their genetic composition and stability. The live EV76 vaccine is an apparent pgm mutant that has been used in some countries (49). However, a concern is that the EV76 vaccine strain can cause disease in primates, raising questions about its suitability as a human vaccine (29). Nevertheless, as recently as 2002, USAMRIID researchers noted, “Despite their drawbacks, there is ample evidence that live-attenuated strains of Y. pestis should be considered as potential vaccine candidates” (52). Research toward the development of new, improved live attenuated vaccines should continue and be strongly encouraged (45). In this work, we explore the feasibility of developing a live attenuated Y. pestis vaccine.
The cyclic AMP receptor protein (Crp) is an important transcription factor that regulates the expression of more than 100 genes in Escherichia coli, most of which are involved in catabolism of carbon sources other than glucose (24). E. coli preferentially utilizes glucose and catabolizes other sugars only when the supply of glucose has become depleted (reviewed in reference 39).
Crp modulates expression of genes in many pathogenic bacteria, including Salmonella, Vibrio cholerae, Yersinia enterocolitica, and Y. pestis (10, 38, 44, 54). Crp regulation occurs either directly, by binding to specific DNA sequences near the regulated gene, or indirectly, through the action of CyaR, a regulatory RNA (13). In Salmonella, several virulence factors are known to be regulated by crp, including sirA, which regulates the expression of a number of key invasion genes encoded in Salmonella pathogenicity island 1 (SPI1) (1), including hilA (20). SPI1 encodes a type 3 secretion system and effector molecules that direct Salmonella invasion of mucosal tissues. In addition, crp regulates expression of the spv genes, also required for invasion of mucosal tissues, and several fimbrial operons (14, 33). Strains of Salmonella and Y. enterocolitica with crp deletions are attenuated in mice and stimulate protective immunity against subsequent challenge with the wild-type parent (10, 38). In Y. pestis, the crp gene directly regulates expression of some 37 genes, including ypkA and yopO, which encode a secreted virulence factor, and the laterally acquired plasmid genes pla, a known virulence factor, and pst, encoding the bacteriocin pesticin (38, 54). In a recent report, yopJ, a secreted effector protein involved in immune suppression, was also shown to be negatively regulated by crp (55). Crp is required for expression of the Ysc type 3 secretion system and other virulence factors in Yersinia, and functional loss of crp diminishes Yop secretion by Y. enterocolitica and Y. pestis (38, 54). The effect of a crp mutation on LcrV secretion has not been reported. A Y. pestis crp mutant is attenuated for virulence (54).
An attenuated immunogenic live vaccine must be safe, efficacious, and avirulent and not induce disease symptoms. In addition, it must be able to reach, multiply in, and persist for a while in those lymphoid organs necessary to stimulate a protective immune response. Many well-studied means for attenuating pathogens render strains more susceptible to host defense stresses than wild-type virulent strains and/or impair their ability to effectively colonize host lymphoid tissues. To address these problems, work in our laboratory has led to the development of a regulated delayed attenuation system, applied first to Salmonella, in which the vaccine strains display features of the wild-type virulent pathogen at the time of immunization to enable the strain to effectively colonize lymphoid tissues and then become completely attenuated in vivo to preclude inducing disease symptoms (11). We have applied this new technology to the crp gene in Y. pestis by constructing a strain in which crp expression is dependent on the presence of arabinose, a sugar that is not present in host tissues (22, 25). Arabinose is provided during in vitro growth so that the strain expresses crp, making it fully functional to interact with host tissues. Once the strain has invaded host cells, where free arabinose is not available, crp is no longer expressed and the strain becomes attenuated. We compared the virulence and immunogenicity of the regulated delayed attenuation strain with those of an isogenic Δcrp deletion strain of Y. pestis. We found that the arabinose-regulated crp mutant was attenuated for virulence and induced greater protective immunity against pneumonic plague than did the Δcrp strain.
MATERIALS AND METHODS
Media and reagents.
Tryptose blood agar (TBA) and heart infusion broth (HIB) were from Difco. Y. pestis strains were grown in HIB and on HIB Congo red agar plates at 30°C to confirm the pigmentation (Pgm) phenotype of Y. pestis strains (46). Ampicillin, chloramphenicol (Cm), and l-arabinose were from Sigma (St. Louis, MO). Oligonucleotides were from IDT (Coralville, IA). Restriction endonucleases were from New England Biolabs. Taq DNA polymerase (New England Biolabs) was used in all PCR tests. Qiagen products (Hilden, Germany) were used to isolate plasmid DNA, gel purify fragments, or purify PCR products. T4 ligase, T4 DNA polymerase, and shrimp alkaline phosphatase (SAP) were from Promega.
Bacterial strains and plasmids.
Strains and plasmids used in this paper are listed in Table 1. E. coli TOP10 was used for plasmid propagation. During screening for mutants, Y. pestis was grown on TBA plates with added chloramphenicol (10 μg/ml) or 5% sucrose. Y. pestis was grown at 30°C for 24 h with shaking (liquid media) or for 48 h (solid media) (46).
TABLE 1.
Bacterial strains and plasmids used in this study
| Strain or plasmid | Relevant genotype or annotation | Source, reference, or derivation |
|---|---|---|
| Strains | ||
| E. coli | ||
| TOP10 | F−mcrA Δ(mrr-hsdRMS-mcrBC) φ80lacZΔM15 ΔlacX74 recA1 araD139 Δ(ara-leu)7697 galU galK rpsL endA1 nupG | Invitrogen |
| χ6212 | asd-negative DH5α derivative | 31 |
| Y. pestis | ||
| KIM6+ | Pgm+ pMT1 pPCP1, cured of pCD1 | 16 |
| KIM5+ | Pgm+ pMT1 pPCP1 pCD1Ap | 16 |
| KIM5 | Pgm− pMT1 pPCP1 pCD1Ap | 5 |
| χ10010 | Δcrp-18 Y. pestis KIM6+ | This study |
| χ10017 | ΔPcrp21::TT araC PBADcrp Y. pestis KIM6+ | This study |
| Plasmids | ||
| pUC18 | Apr | Invitrogen |
| pKD46 | repA101(Ts) ori λ Red recombinase expression plasmid | 12 |
| pYA3493 | Asd+ pBR ori β-lactamase signal sequence-based periplasmic secretion plasmid | 21 |
| pYA3700 | TT araC PBAD cassette plasmid, Apr | 9 |
| pYA4373 | cat-sacB cassette in the PstI and SacI sites of pUC18 | 48 |
| pYA4443 | Six-His tag in the C-terminal end of lcrV gene cloned into EcoRI and HindIII sites of pYA3493 | pYA3493 |
| pYA4579 | y3957′-′y3955 fragment ligated by overlapping PCR cloned into EcoRI and HindIII sites of pUC18 | pUC18 |
| pYA4581 | SD-crp and y3957′ fragments cloned into XhoI/EcoRI sites and PstI/HindIII sites of pYA3700 | pYA3700 |
| pYA4588 | cat-sacB cassette from pYA4373 cloned into PstI site of pYA4581 | pYA4581 |
Plasmid construction.
All primers used in this paper are listed in Table 2. Primer sets CRP-1/CRP-2 and CRP-3/CRP-4 were used for amplifying the y3957′ (upstream of crp) and ′y3955 (downstream of crp) fragments, respectively. Complementarity between primers CRP-2 and CRP-3 is indicated by bold lettering in Table 2. The ′y3955 and y3957′ fragments were fused by overlapping PCR using primers CRP-1 and CRP-4. The resulting PCR product was digested with EcoRI and HindIII and ligated with pUC18 digested with the same enzymes to construct the plasmid pYA4597.
TABLE 2.
Primers used in this studya
| Name | Sequence |
|---|---|
| CRP-1 | 5′ CGGAAGCTTGAGACTGAAAATAGCGGCGA 3′ (HindIII) |
| CRP-2 | 5′ GCGACTGCAGGCTGCCGAGCTCTTCCCTCTAAAAACCGGCGTTA 3′ |
| CRP-3 | 5′ GAAGAGCTCGGCAGCCTGCAGTCGCTGTTATCCTCTGTTGTTATCG 3′ |
| CRP-4 | 5′ CGGGAATTCCTTTTTGTAAAATAGACACG 3′ (EcoRI) |
| CRP-5 | 5′ CGGGAATTCTTAACGGGTGCCGTAAACGA 3′ (EcoRI) |
| CRP-6 | 5′ CGGCTCGAGGAGGATAACAGCGAATGGTT 3′ (XhoI) |
| CRP-7 | 5′ CGGCTGCAGGCCGAAAGGTATAGCCAAGGT 3′ (PstI) |
| CRP-8 | 5′ CGGAAGCTTCTGATAGATCAACTGCGCGC 3′ (HindIII) |
| CRP-9 | 5′ CGACTTCGCGTACCTCAAAGCT 3′ |
| CRP-10 | 5′ TACATAACCGGAACCACAACCAG 3′ |
| Cm-V | 5′ GTTGTCCATATTGGCCACGTTTA 3′ |
| SacB-V | 5′ GCAGAAGAGATATTTTTAATTGTGGACG 3′ |
| araC-V | 5′ CATCCACCGATGGATAATCGGGTA 3′ |
| lcrV-1 | CGGGAATTCATGATTAGAGCCTACGAACA (EcoRI) |
| lcrV-2 | CGGAAGCTTTCAATGATGATGATGATGGTGTTTACCAGACGTGTCATCTAG (HindIII) |
Restriction endonuclease sites are underlined. Boldface shows the reverse complementary region between CRP-3 and CRP-4.
Primer sets CRP-5/CRP-6 and CRP-7/CRP-8 were used for amplifying the crp fragment containing its original Shine-Dalgarno (SD) sequence (SD-crp) and the y3957′ (−110 to −660 bp upstream of crp) fragment, respectively. The SD-crp and y3957′ fragments were cloned into the XhoI/EcoRI sites and PstI/HindIII sites of pYA3700, respectively, to form pYA4581. Plasmid pYA4581 was PstI digested, blunted by T4 DNA polymerase, and dephosphorylated with SAP. The cat-sacB fragment was cut from pYA4373 using PstI and SacI restriction endonucleases and blunted by T4 DNA polymerase. The two fragments were ligated to form plasmid pYA4588. lcrV encoding a C-terminal six-His tag was amplified from pCD1Ap using primers lcrV-1 and lcrV-2 and cloned into the EcoRI and HindIII sites of pYA3493 to form pYA4443.
Preparation of LcrV antiserum.
Full-length His-tagged LcrV was expressed from E. coli χ6212(pYA4443) and isolated by nickel chromatography. One hundred fifty micrograms of His-tagged LcrV protein was emulsified with Freund's complete adjuvant and injected into New Zealand White female rabbits from Charles River Laboratories. The rabbits were immunized with two booster injections (in Freund's incomplete adjuvant) at 3-week intervals. Antiserum was collected 1 week after the last booster injection.
Strain construction.
Y. pestis mutant strains χ10010 and χ10017 were constructed using the two-step recombination method (48). The procedure was as follows: Y. pestis KIM6+(pKD46) was electroporated with the linear y3957′-cat-sacB-TT araC PBAD SD-crp fragment excised from plasmid pYA4588 using EcoRI and HindIII. Electroporants were selected on TBA-chloramphenicol (Cm) plates and verified by PCR. Colonies with the correct PCR profile were streaked onto TBA-Cm-sucrose plates to verify sucrose sensitivity and onto HIB Congo red-Cm plates to confirm the presence of the pgm locus. This intermediate strain was used for all further constructions. To construct strain χ10017, the chromosomal cat-sac cassette was removed by electroporation with 1 μg of linear DNA (y3957′-TT araC) cut from pYA4581 using HindIII and BamHI. The loss of the cat-sac cassette in sucrose-resistant colonies was confirmed by PCR. Strain χ10010 was constructed by electroporating the intermediate strain with a linear ′y3955-y3957′ fragment cut from pYA4597 using HindIII and EcoRI to delete the entire crp gene. Plasmid pKD46 was cured from a single-colony isolate of the above strains to yield χ10010 (Δcrp) and χ10017 (araC PBAD crp). Under biosafety level 3 (BSL-3) containment, plasmid pCD1Ap was then introduced by electroporation into each strain, yielding χ10010(pCD1Ap) and χ10017(pCD1Ap).
SDS-PAGE and immunoblot analyses.
Secreted proteins were prepared by using a modification of previously described methods (36). Y. pestis was grown in HIB medium overnight at 26°C. Cells were harvested, washed three times in chemically defined medium PMH2 (16), used to inoculate 40 ml of fresh PMH2 medium to an optical density at 600 nm (OD600) of 0.05, and shaken at 26°C overnight. Cultures were shifted to 37°C for 6 h with mild aeration. The OD600s of cultures were measured, and bacterial cell pellets were collected by centrifugation. The pellets were suspended in sodium dodecyl sulfate (SDS) loading buffer. The volume of sample buffer was adjusted based on the OD600 to normalize the amount loaded. Cells were lysed by being heated at 95°C for 5 min. Culture supernatants were concentrated by precipitation with 10% (wt/vol) trichloroacetic acid overnight at 4°C and collected by centrifugation. Pellets were washed with ice-cold acetone and dissolved in 0.05 M Tris-HCl buffer (pH 9.5). Insoluble materials were removed by centrifugation at 12,500 × g for 15 min, and the soluble protein concentration was determined using a DC protein assay kit (Bio-Rad, Hercules, CA). Samples were heated at 95°C for 5 min, separated by SDS-PAGE, and blotted onto nitrocellulose membranes. The membranes were probed with rabbit anti-LcrV antibodies as described previously (3).
Virulence analysis in mice.
All animal procedures were conducted in animal BSL-3 containment facilities and approved by the Arizona State University Animal Care and Use Committee. Single colonies of Y. pestis KIM5+ strains to be tested in mice were used to inoculate HIB containing 25 μg/ml ampicillin and grown at 26°C overnight. Bacteria were diluted into 10 ml of fresh medium with 0.2% xylose and 2.5 mM CaCl2 to an OD620 of 0.1 and incubated at 26°C for s.c. infections (bubonic plague) or incubated at 37°C for intranasal (i.n.) infections (pneumonic plague) and grown to an OD620 of 0.6. The cells were harvested by centrifugation and suspended in 1 ml of isotonic phosphate-buffered saline (PBS).
Female 7-week-old Swiss Webster mice from Charles River Laboratories were inoculated s.c. with 100 μl of the bacterial suspension. Actual numbers of CFU inoculated were determined by plating serial dilutions onto TBA. To determine the 50% lethal dose (LD50), five groups of six mice/group were inoculated i.n. or s.c. with serial dilutions of bacteria. Mice were monitored twice daily for 21 days, and the LD50 was calculated as described previously (41). For in vivo complementation of strain χ10017(pCD1Ap), 120 mg of l-arabinose dissolved in 100 μl PBS was intraperitoneally administered to mice on the day of inoculation and once a day thereafter (28).
For colonization/dissemination analysis, groups of mice were injected s.c. At the indicated times after infection, 3 mice per strain were euthanized, and samples of blood, lungs, spleen, and liver were removed. The bacterial load for each organ was determined by plating dilutions of the homogenized tissues onto TBA plates containing 25 μg/ml ampicillin and reported as CFU per gram of tissue or CFU per ml blood. Infections were performed in at least two independent experiments.
Determination of protective efficacy.
Y. pestis strains were grown as described above. Two groups of Swiss Webster mice (10/group) were vaccinated s.c. with 3.8 × 107 CFU of χ10010(pCD1Ap) or 3 × 104 CFU of χ10017(pCD1Ap) cells in 100 μl of PBS on day 0. Another two groups of mice (4/group) were injected with 100 μl of PBS as controls. Blood was collected by retro-orbital sinus puncture at 2 and 4 weeks postimmunization and 2 weeks after challenge for antibody measurement. Mice were lightly anesthetized using a ketamine and xylazine mixture administered intramuscularly before bleeding. On day 35, animals were challenged s.c. with Y. pestis KIM5+ at either 1.3 × 105 CFU for the χ10017(pCD1Ap) group or 1.3 × 107 CFU for the χ10010(pCD1Ap) group in 100 μl PBS or lightly anesthetized with a 1:5 xylazine-ketamine mixture and challenged i.n. with 1.4 × 104 CFU in 20 μl PBS. Control groups were challenged with 1.3 × 103 CFU by both routes. All infected animals were observed over a 15-day period for the development of signs of plague infection.
ELISA.
Enzyme-linked immunosorbent assay (ELISA) was used to assay serum IgG antibodies against Yersinia whole-cell lysates (YpL) (47) and purified LcrV antigen of Y. pestis KIM5+. Polystyrene 96-well flat-bottomed microtiter plates (Dynatech Laboratories Inc., Chantilly, VA) were coated with 200 ng/well of YpL or purified LcrV protein. The procedures were same as those described previously (21).
Measurement of cytokine concentrations.
Cytokines were quantitated by a double-sandwich ELISA as described previously (42). Mice in groups of three were euthanized at intervals by terminal bleeding under anesthesia. Pooled blood was allowed to clot overnight at 4°C, and serum was separated by centrifugation at 10,000 × g for 10 min. Sera were filtered once through a 0.22-μm syringe filter, cultured on TBA to confirm that bacteria had been removed, and stored at −70°C prior to assay.
Commercial solid-phase enzyme immunoassays utilizing the multiple-antibody sandwich principle were used to determine cytokines in biological samples. Levels of interleukin-10 (IL-10), tumor necrosis factor alpha (TNF-α), and gamma interferon (IFN-γ) were determined with mouse IL-10, IFN-γ, and TNF-α Ready-Set-Go kits (eBioscience), respectively. Concentrations of cytokines were measured by reading optical density at 450 nm and then calculated in reference to values obtained in standard curves generated for each assay. Assays of pooled sera were repeated three times.
Statistical analysis.
The log rank test was used for analysis of the survival curves. Data are expressed as means ± standard errors (SE). The Student t test was used for other statistical analyses. A P value of <0.05 was considered significant.
RESULTS
Crp synthesis and growth of Y. pestis mutants.
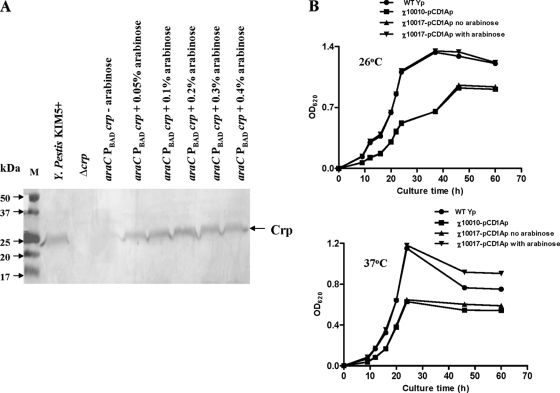
We constructed mutant Y. pestis strains χ10010 (Δcrp) and χ10017 (araC PBAD crp). In the araC PBAD crp mutant χ10017, crp expression is dependent on the presence of arabinose. Crp was not detected in either the Δcrp strain χ10010 or the araC PBAD crp strain χ10017 grown in the absence of arabinose (Fig. 1A). Upon arabinose addition, χ10017 synthesized roughly the same amount of Crp as did wild-type Y. pestis.
FIG. 1.
Crp synthesis and growth of Y. pestis mutants. (A) Measurement of Crp synthesis in Y. pestis KIM5+, χ10010 (crp18), and χ10017 (araC PBAD crp). Strains were grown in HIB at 37°C overnight, and Crp synthesis was detected by Western blotting using anti-Crp sera. M, protein marker. (B) Growth of Y. pestis strains in HIB medium at 26°C or 37°C. •, Y. pestis KIM5+; ▪, χ10010(pCD1Ap) (Δcrp); ▴, χ10017(pCD1Ap) (araC PBAD crp) without arabinose; ▾, χ10017(pCD1Ap) with 0.05% arabinose. WT, wild type.
Once we had confirmed that Crp synthesis was arabinose regulated, we moved plasmid pCD1Ap into both mutants and examined their growth in liquid media. Strains χ10010(pCD1Ap) and χ10017(pCD1Ap) without arabinose grew more slowly and did not reach the same final OD620 as did Y. pestis KIM5+ at 26°C or 37°C in HIB medium (Fig. 1B). When 0.05% arabinose was included in the growth medium, χ10017(pCD1Ap) grew at the same rate as did the wild type.
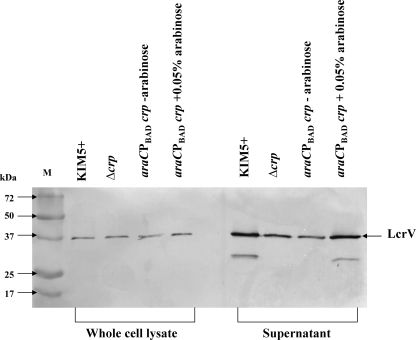
LcrV synthesis and secretion in Y. pestis KIM5+ and mutant derivatives.
Crp is required for expression of the Ysc type 3 secretion system and other virulence factors in Yersinia, and functional loss of crp diminishes Yop secretion by Y. enterocolitica and Y. pestis (7, 23, 38). However, the effect of a crp mutation on LcrV secretion has not been reported. Therefore, we compared LcrV production in cells and supernatants from Y. pestis KIM5+, χ10010(pCD1Ap), and χ10017(pCD1Ap). We observed no difference in LcrV synthesis in whole-cell lysates among strains (Fig. 2). There was a reduction in the amount of LcrV detected in supernatants between the wild type and strains χ10010(pCD1Ap) (Δcrp) and χ10017(pCD1Ap) (araC PBAD crp). Wild-type levels of secreted LcrV were restored when strain χ10017(pCD1Ap) was grown with 0.05% arabinose (Fig. 2).
FIG. 2.
Measurement of LcrV synthesis and secretion in Y. pestis by Western blot analysis. Whole-cell lysates and supernatant fractions were separated by SDS-PAGE and detected by Western blotting. For each sample, equivalent amounts of protein were loaded. The araC PBAD crp strain χ10017(pCD1Ap) was grown with and without 0.05% arabinose.
Virulence of Y. pestis mutants in mice.
To investigate the contribution of Crp to Y. pestis virulence, we infected Swiss Webster mice s.c. with Y. pestis KIM5+, χ10010(pCD1Ap) (Δcrp), or χ10017(pCD1Ap) (araC PBAD crp). Strain χ10017(pCD1Ap) was grown in the presence of arabinose prior to inoculation. The LD50 of Y. pestis KIM5+ was <10 CFU, consistent with previous results (50). The LD50 of the Δcrp mutant χ10010(pCD1Ap) was >3 × 107 CFU. The LD50 of strain χ10017(pCD1Ap) was 4.3 × 105 CFU, and the mean time to death was delayed 2 to 9 days compared to the wild type. The LD50 of χ10017(pCD1Ap) was the same as that of KIM5+ (LD50, <10 CFU) when inoculated mice were injected with arabinose, indicating full complementation of the attenuation phenotype. In a preliminary experiment, we found that both the Δcrp and araC PBAD crp mutants were attenuated when administered by the intranasal route, with LD50s of >1 × 104 CFU. However, mice inoculated with 7 × 103 to 9 × 103 CFU of either mutant were not protected from subsequent intranasal challenge with 5 × 103 CFU of KIM5+ (data not shown) and, therefore, we did not repeat those experiments.
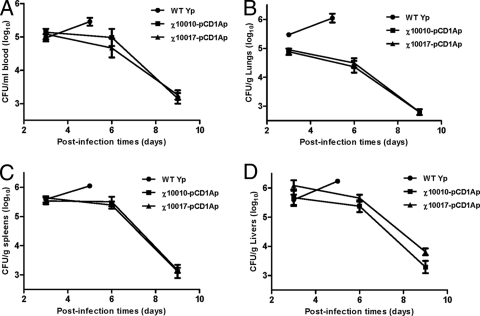
We evaluated the ability of the Y. pestis mutants to disseminate systemically compared to Y. pestis KIM5+ by monitoring, over a 9-day period, the lungs, spleen, liver, and blood of groups of mice injected with each of the strains. Because of the difference in LD50s among the three strains, we inoculated mice with different doses of each. For this type of experiment, we typically choose a dose that is higher than the LD50. However, since we were not able to establish an LD50 value for the Δcrp strain (>1 × 107 CFU), we chose a dose that matched the highest dose for which we had data. For the araC PBAD crp mutant, we chose a dose that was 10-fold above the LD50. Thus, mice were inoculated with 1.5 × 103 CFU of Y. pestis KIM5+, 4.2 × 107 CFU of χ10010(pCD1Ap), or 3.8 × 106 CFU of χ10017(pCD1Ap). The kinetics of infection were similar for the two mutants. At 3 days postinfection (p.i.), the numbers of bacteria recovered from the blood, liver, and spleen were similar for all strains (Fig. 3). About half as many χ10010 and χ10017 cells as those of the wild-type strain were recovered from lungs. The numbers of mutants recovered from all tissues decreased steadily on days 6 and 9. All mice inoculated with Y. pestis KIM5+ succumbed to the infection before day 9, and therefore, we do not include any of those mice in our figure for that time point.
FIG. 3.
Kinetics of infection with Y. pestis KIM5+ and mutant derivatives in mouse tissues. Bacteria were inoculated s.c. with 1.5 × 103 CFU of Y. pestis KIM5+, 4.2 × 107 CFU of χ10010(pCD1Ap), or 3.8 × 106 CFU of χ10017(pCD1Ap), and at various times CFU per organ in the blood (A), lungs (B), spleens (C), and livers (D) were determined. Error bars represent standard deviations. We examined 3 mice/group/time point, and the experiment was performed twice with similar results. WT, wild type.
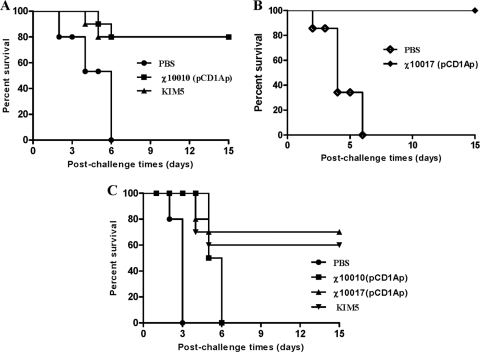
Evaluation of protective immunity.
Groups of mice were immunized with a single dose of χ10010(pCD1Ap) (Δcrp), 10017(pCD1Ap) (araC PBAD crp), or Y. pestis KIM5 (Pgm−) and challenged 35 days later. For these experiments, we wanted to use the highest possible immunizing dose for each strain. We based our decision on immunizing doses for each strain on the LD50 data, shown above. Therefore, we immunized with a dose of 3 × 104 CFU of 10017(pCD1Ap), 3.8 × 107 CFU of 10010(pCD1Ap), or 2.5 × 107 CFU of Y. pestis KIM5 (Pgm−), respectively. Our results after challenge show that a single s.c. dose of χ10010(pCD1Ap) or Y. pestis KIM5 (Pgm−) provided excellent protection against a 1 × 106-LD50 s.c. challenge (Fig. 4A). A single s.c. dose of χ10017(pCD1Ap) provided complete protection against a 10,000-LD50 s.c. challenge without any symptoms (Fig. 4B). Immunization with strain χ10010(pCD1Ap) delayed the time of death but ultimately did not provide protection against a 100-LD50 i.n. challenge. Immunization with the Y. pestis strain χ10017(pCD1Ap) or the pgm mutant strain KIM5 provided significant protection (P < 0.001), protecting most of the mice against a 100-LD50 i.n. challenge (Fig. 4C). None of the mice immunized with PBS survived challenge by either route (Fig. 4).
FIG. 4.
Survival of immunized and nonimmunized mice after Y. pestis KIM5+ challenge. (A) Swiss Webster mice vaccinated s.c. with 3.8 × 107 CFU of χ10010(pCD1Ap) or 2.5 × 107 CFU of Y. pestis KIM5 (Pgm−) were challenged with 1.3 × 107 CFU of Y. pestis KIM5+ via the s.c. route. (B) Swiss Webster mice vaccinated s.c. with 3.0 × 104 CFU of χ10017(pCD1Ap) were challenged with 1.4 × 105 CFU of Y. pestis KIM5+ via the s.c. route. (C) Swiss Webster mice vaccinated s.c. with 3.8 × 107 CFU of χ10010(pCD1Ap), 3.0 × 104 CFU of χ10017(pCD1Ap), or 2.5 × 107 CFU of KIM5 were challenged via the i.n. route with 1.4 × 104 CFU of Y. pestis KIM5+. For panels A and B, survival of immunized mice was significantly greater than that for PBS controls in all experiments (P < 0.001). For panel C, survival of mice immunized with χ10017(pCD1Ap) or KIM5 was significantly greater than that of mice immunized with strain χ10010(pCD1Ap) or PBS controls (P < 0.001). There were 10 mice per vaccination group and 4 mice per control group for each experiment. The experiment was performed twice.
Serum immune responses.
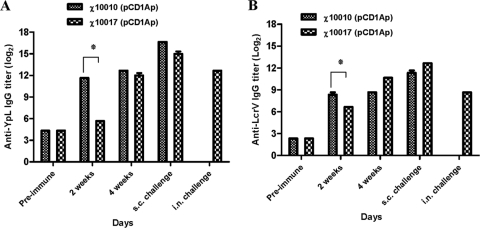
Serum IgG responses to YpL and LcrV from immunized mice were measured by ELISA. High anti-YpL (Fig. 5A) titers were slower to develop for the arabinose-regulated crp mutant, χ10017(pCD1Ap), than for the Δcrp mutant, χ10010(pCD1Ap), but by week 4, the titers were similar. Also by week 4, the anti-LcrV (Fig. 5B) serum IgG titers were somewhat higher in mice immunized with χ10017(pCD1Ap) than in mice immunized with χ10010(pCD1Ap). Titers against both antigens were boosted in mice challenged s.c. No boosting was observed in the mice immunized with χ10017(pCD1Ap) after i.n. challenge.
FIG. 5.
The IgG response in sera of mice inoculated with χ10010(pCD1Ap) or χ10017(pCD1Ap). (A) Y. pestis KIM5+ whole-cell lysate (YpL) was used as the coating antigen. (B) Recombinant LcrV was used as the coating antigen. *, P < 0.01.
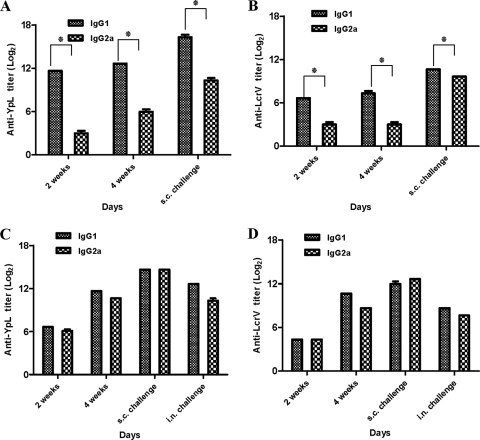
Th1 cells direct cell-mediated immunity and promote class switching to IgG2a, and Th2 cells provide potent help for B-cell antibody production and promote class switching to IgG1 (17). The Δcrp strain χ10010(pCD1Ap) elicited a strong Th2-biased response against both antigens, with high IgG1 titers and low IgG2 titers (Fig. 6A and B). Strain χ10017(pCD1Ap) induced a more balanced Th1/Th2 response (Fig. 6C and D). Challenge did not have much effect on the IgG1/IgG2a ratios, except for the anti-LcrV response in mice immunized with χ10010(pCD1Ap), where the response became more balanced.
FIG. 6.
Serum IgG1 and IgG2a responses to YpL and recombinant LcrV. (A) IgG1 and IgG2a antibody levels to YpL in sera of mice immunized s.c. with χ10010(pCD1Ap). (B) IgG1 and IgG2a antibody levels to recombinant LcrV in sera of mice subcutaneously immunized with χ10010(pCD1Ap). (C) IgG1 and IgG2a antibody levels to YpL in sera of mice subcutaneously immunized with χ10017(pCD1Ap). (D) IgG1 and IgG2a antibody levels to recombinant LcrV in sera of mice subcutaneously immunized with χ10017(pCD1Ap). *, P < 0.01.
Induction of cytokines.
Cytokines are critical to the development and functioning of both the innate and adaptive immune responses. They are secreted by immune cells that have encountered pathogens, thereby activating and recruiting additional immune cells to respond to the infection. LcrV is an immunomodulator, inhibiting production of TNF-α and IFN-γ and inducing IL-10 in eukaryotic cells both in vivo and in vitro (4, 30, 32). To evaluate the effect of reduced LcrV secretion in the two mutants (Fig. 2), we compared production of IL-10, IFN-γ, and TNF-α in infected mice. Groups of three Swiss-Webster mice were inoculated s.c. with 1,500 CFU of Y. pestis KIM5+, 4.2 × 107 CFU of χ10010(pCD1Ap), or 3.8 × 106 CFU of χ10017(pCD1Ap). A group of uninfected mice served as controls. Blood was collected via cardiac puncture at days 3 and 6 p.i. for cytokine analysis. We could detect IL-10 but not IFN-γ or TNF-α in the sera of animals infected with Y. pestis KIM5+, but IL-10 and proinflammatory factors such as IFN-γ and TNF-α were not detected in mice infected with χ10010(pCD1Ap) and χ10017(pCD1Ap) (data not shown).
DISCUSSION
We have been developing live bacterial vaccine strains that display regulated delayed attenuation, such that upon immunization, the vaccine strain exhibits all the phenotypic qualities of the wild type, allowing it to establish an infection necessary to stimulate an immune response. After 5 to 10 rounds of replication, the strain becomes attenuated, precluding its ability to cause disease. We have shown this in detail previously for Salmonella (11), and here we apply this concept to Y. pestis. With this goal in mind, we constructed and evaluated an araC PBAD crp strain and, for comparison, an isogenic Δcrp strain. Our results indicate that crp affects virulence in Y. pestis, consistent with what was found in a recent study in which a Y. pestis Δcrp strain was shown to be highly attenuated when administered subcutaneously to mice (54). In that study, the authors found that the s.c. LD50 in mice was approximately 1 × 104-fold higher than that of wild-type Y. pestis strain 201 (54). The Δcrp mutant used in our study was completely avirulent, with an LD50 >1 × 106-fold greater than that of the wild type. Possible reasons for this difference include the use of different mouse strains (BALB/c versus Swiss Webster), the use of different parental strains, and differences in the way that the crp mutant was constructed (deletion versus insertion). These discrepancies aside, our work confirms that a Y. pestis crp mutant is highly attenuated when administered subcutaneously.
The increased LD50 observed for both crp mutants by s.c. and i.n. routes indicates that Crp regulates genes important in establishing a lethal infection during bubonic and pneumonic plague. A number of factors may play a role in the loss of virulence. In the absence of crp expression, there is a reduction in the in vitro growth rate as observed by Zhan et al. (54). The pla gene, important for systemic spread of Y. pestis from subcutaneous sites, requires Crp for maximal expression (23, 54). Pla is also involved in the development of pneumonic plague (27), which may explain why we observed lower titers of the two mutants than of the wild type in lung tissue on day 3.
Yop secretion is reduced in crp mutants (23, 38). The Yop virulon comprises both the Yop effector proteins and the proteins necessary for injecting them into host cells. The injected Yops perturb cytoskeleton dynamics, disrupt phagocytosis, and block the production of proinflammatory cytokines, thus favoring the survival of the invading Yersinia (6, 7, 37). Our results show that LcrV secretion was also reduced (Fig. 2). Although controversial, some reports indicate that LcrV stimulates the release of IL-10 through interactions with Toll-like receptor 2 and CD14 receptors, which downregulate synthesis of the proinflammatory cytokines IFN-γ and TNF-α (4, 43). Thus, the reduction of Yop and LcrV secretion may play a role in the avirulence of crp mutants.
It has been suggested that crp regulates expression of caf1, which encodes the F1 protein that forms a capsule on Y. pestis at 37°C (54). However, since caf1 mutants (F1−) are fully virulent in mice and nonhuman primates (15), we focused our attention on the expression of antigens such as Yops and LcrV that will provide protection against all Y. pestis strains.
Strain χ10010(pCD1Ap) (Δcrp) induced a strong Th2 bias, while strain χ10017(pCD1Ap), featuring regulated crp expression, elicited a more balanced Th1/Th2 response (Fig. 6). Both mutants examined in this study provided protection against s.c. challenge (Fig. 4). However, only strain χ10017(pCD1Ap) provided significant protection against pneumonic challenge (Fig. 4C), similar to the pgm mutant strain KIM5. These results are consistent with what is known about the immunogenicity requirements for protection against Y. pestis. Protection against bubonic plague has been correlated with antibody production (26, 45), while protection against pneumonic plague is known to require cell-mediated immunity induced by IFN-γ and TNF-α (34, 35). The strong Th2 response generated by the Δcrp strain leads to a primarily antibody-based response with little priming of cellular immunity, while the more balanced Th1/Th2 response generated by χ10017(pCD1Ap) should provide both antibody and cellular priming (17). The fact that we did not detect IL-10, IFN-γ, and TNF-α in the sera of mice immunized with χ10017(pCD1Ap) may be a reflection of the low sensitivity of the assay that we used (18). Our results support the idea that regulated delayed attenuation is a powerful new tool for designing live Yersinia vaccines to stimulate both humoral and cellular immunity.
One of the strategies that we have adopted as for developing live attenuated Salmonella vaccine strains has been to include multiple attenuating mutations as a way to ensure an acceptable degree of safety. As we move forward toward developing a live Y. pestis vaccine, we will use a similar approach. In future studies, we plan to construct Y. pestis vaccine strains with multiple attenuating mutations and evaluate them for immunogenicity, pathological effects on host tissues, and protective efficacy.
Acknowledgments
This research was supported by National Institutes of Health grant AI057885.
All authors declare no conflict of interest.
Editor: J. B. Bliska
Footnotes
Published ahead of print on 19 January 2010.
REFERENCES
- 1.Ahmer, B. M., J. van Reeuwijk, P. R. Watson, T. S. Wallis, and F. Heffron. 1999. Salmonella SirA is a global regulator of genes mediating enteropathogenesis. Mol. Microbiol. 31:971-982. [DOI] [PubMed] [Google Scholar]
- 2.Alvarez, M. L., H. L. Pinyerd, J. D. Crisantes, M. M. Rigano, J. Pinkhasov, A. M. Walmsley, H. S. Mason, and G. A. Cardineau. 2006. Plant-made subunit vaccine against pneumonic and bubonic plague is orally immunogenic in mice. Vaccine 24:2477-2490. [DOI] [PubMed] [Google Scholar]
- 3.Branger, C. G., J. D. Fetherston, R. D. Perry, and R. Curtiss III. 2007. Oral vaccination with different antigens from Yersinia pestis KIM delivered by live attenuated Salmonella typhimurium elicits a protective immune response against plague. Adv. Exp. Med. Biol. 603:387-399. [DOI] [PubMed] [Google Scholar]
- 4.Brubaker, R. R. 2003. Interleukin-10 and inhibition of innate immunity to Yersiniae: roles of Yops and LcrV (V antigen). Infect. Immun. 71:3673-3681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brubaker, R. R. 1983. The Vwa+ virulence factor of Yersiniae: the molecular basis of the attendant nutritional requirement for Ca2+. Rev. Infect. Dis. 5(Suppl. 4):S748-S758. [DOI] [PubMed] [Google Scholar]
- 6.Cornelis, G. R. 2002. Yersinia type III secretion: send in the effectors. J. Cell Biol. 158:401-408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cornelis, G. R., A. Boland, A. P. Boyd, C. Geuijen, M. Iriarte, C. Neyt, M. P. Sory, and I. Stainier. 1998. The virulence plasmid of Yersinia, an antihost genome. Microbiol. Mol. Biol. Rev. 62:1315-1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cornelius, C. A., L. E. Quenee, K. A. Overheim, F. Koster, T. L. Brasel, D. Elli, N. A. Ciletti, and O. Schneewind. 2008. Immunization with recombinant V10 protects cynomolgus macaques from lethal pneumonic plague. Infect. Immun. 76:5588-5597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Curtiss, R., III, and W. Kong. August 2006. Regulated bacterial lysis for gene vaccine vector delivery and antigen release. U.S. patent 2006/0140975.
- 10.Curtiss, R., III, and S. M. Kelly. 1987. Salmonella typhimurium deletion mutants lacking adenylate cyclase and cyclic AMP receptor protein are avirulent and immunogenic. Infect. Immun. 55:3035-3043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Curtiss, R., III, S. Y. Wanda, B. M. Gunn, X. Zhang, S. A. Tinge, V. Ananthnarayan, H. Mo, S. Wang, and W. Kong. 2009. Salmonella enterica serovar typhimurium strains with regulated delayed attenuation in vivo. Infect. Immun. 77:1071-1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Datsenko, K. A., and B. L. Wanner. 2000. One-step inactivation of chromosomal genes in Escherichia coli K-12 using PCR products. Proc. Natl. Acad. Sci. U. S. A. 97:6640-6645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Lay, N., and S. Gottesman. 2009. The Crp-activated small noncoding regulatory RNA CyaR (RyeE) links nutritional status to group behavior. J. Bacteriol. 191:461-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Eisenstein, B. I., E. H. Beachey, and S. S. Solomon. 1981. Divergent effects of cyclic adenosine 3′,5′-monophosphate on formation of type 1 fimbriae in different K-12 strains of Escherichia coli. J. Bacteriol. 145:620-623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Friedlander, A. M., S. L. Welkos, P. L. Worsham, G. P. Andrews, D. G. Heath, G. W. Anderson, Jr., M. L. Pitt, J. Estep, and K. Davis. 1995. Relationship between virulence and immunity as revealed in recent studies of the F1 capsule of Yersinia pestis. Clin. Infect. Dis. 21(Suppl. 2):S178-S181. [DOI] [PubMed] [Google Scholar]
- 16.Gong, S., S. W. Bearden, V. A. Geoffroy, J. D. Fetherston, and R. D. Perry. 2001. Characterization of the Yersinia pestis Yfu ABC inorganic iron transport system. Infect. Immun. 69:2829-2837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gor, D. O., N. R. Rose, and N. S. Greenspan. 2003. TH1-TH2: a procrustean paradigm. Nat. Immunol. 4:503-505. [DOI] [PubMed] [Google Scholar]
- 18.Hillyer, L. M., and B. Woodward. 2003. Interleukin-10 concentration determined by sandwich enzyme-linked immunosorbent assay is unrepresentative of bioactivity in murine blood. Am. J. Physiol. Regul. Integr. Comp. Physiol. 285:R1514-R1519. [DOI] [PubMed] [Google Scholar]
- 19.Inglesby, T. V., D. T. Dennis, D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. D. Fine, A. M. Friedlander, J. Hauer, J. F. Koerner, M. Layton, J. McDade, M. T. Osterholm, T. O'Toole, G. Parker, T. M. Perl, P. K. Russell, M. Schoch-Spana, and K. Tonat. 2000. Plague as a biological weapon: medical and public health management. Working Group on Civilian Biodefense. JAMA 283:2281-2290. [DOI] [PubMed] [Google Scholar]
- 20.Johnston, C., D. A. Pegues, C. J. Hueck, A. Lee, and S. I. Miller. 1996. Transcriptional activation of Salmonella typhimurium invasion genes by a member of the phosphorylated response-regulator superfamily. Mol. Microbiol. 22:715-727. [DOI] [PubMed] [Google Scholar]
- 21.Kang, H. Y., J. Srinivasan, and R. Curtiss III. 2002. Immune responses to recombinant pneumococcal PspA antigen delivered by live attenuated Salmonella enterica serovar typhimurium vaccine. Infect. Immun. 70:1739-1749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Katzman, R. L., E. Lisowska, and R. W. Jeanloz. 1970. Invertebrate connective tissue. Isolation of D-arabinose from sponge acidic polysaccharide. Biochem. J. 119:17-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim, T. J., S. Chauhan, V. L. Motin, E. B. Goh, M. M. Igo, and G. M. Young. 2007. Direct transcriptional control of the plasminogen activator gene of Yersinia pestis by the cyclic AMP receptor protein. J. Bacteriol. 189:8890-8900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kolb, A., S. Busby, H. Buc, S. Garges, and S. Adhya. 1993. Transcriptional regulation by cAMP and its receptor protein. Annu. Rev. Biochem. 62:749-795. [DOI] [PubMed] [Google Scholar]
- 25.Kong, W., S. Y. Wanda, X. Zhang, W. Bollen, S. A. Tinge, K. L. Roland, and R. Curtiss III. 2008. Regulated programmed lysis of recombinant Salmonella in host tissues to release protective antigens and confer biological containment. Proc. Natl. Acad. Sci. U. S. A. 105:9361-9366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kummer, L. W., F. M. Szaba, M. A. Parent, J. J. Adamovicz, J. Hill, L. L. Johnson, and S. T. Smiley. 2008. Antibodies and cytokines independently protect against pneumonic plague. Vaccine 26:6901-6907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lathem, W. W., P. A. Price, V. L. Miller, and W. E. Goldman. 2007. A plasminogen-activating protease specifically controls the development of primary pneumonic plague. Science 315:509-513. [DOI] [PubMed] [Google Scholar]
- 28.Loessner, H., A. Endmann, S. Leschner, K. Westphal, M. Rohde, T. Miloud, G. Hammerling, K. Neuhaus, and S. Weiss. 2007. Remote control of tumour-targeted Salmonella enterica serovar Typhimurium by the use of L-arabinose as inducer of bacterial gene expression in vivo. Cell. Microbiol. 9:1529-1537. [DOI] [PubMed] [Google Scholar]
- 29.Meyer, K. F., G. Smith, L. Foster, M. Brookman, and M. Sung. 1974. Live, attenuated Yersinia pestis vaccine: virulent in nonhuman primates, harmless to guinea pigs. J. Infect. Dis. 129(Suppl.):S85-S120. [DOI] [PubMed] [Google Scholar]
- 30.Motin, V. L., R. Nakajima, G. B. Smirnov, and R. R. Brubaker. 1994. Passive immunity to Yersiniae mediated by anti-recombinant V antigen and protein A-V antigen fusion peptide. Infect. Immun. 62:4192-4201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nakayama, K., S. M. Kelly, and R. Curtiss III. 1988. Construction of an asd+ expression-cloning vector: stable maintenance and high level expression of cloned genes in a Salmonella vaccine strain. Biotechnology (NY) 6:693-697. [Google Scholar]
- 32.Nedialkov, Y. A., V. L. Motin, and R. R. Brubaker. 1997. Resistance to lipopolysaccharide mediated by the Yersinia pestis V antigen-polyhistidine fusion peptide: amplification of interleukin-10. Infect. Immun. 65:1196-1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.O'Byrne, C. P., and C. J. Dorman. 1994. The spv virulence operon of Salmonella typhimurium LT2 is regulated negatively by the cyclic AMP (cAMP)-cAMP receptor protein system. J. Bacteriol. 176:905-912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Parent, M. A., K. N. Berggren, L. W. Kummer, L. B. Wilhelm, F. M. Szaba, I. K. Mullarky, and S. T. Smiley. 2005. Cell-mediated protection against pulmonary Yersinia pestis infection. Infect. Immun. 73:7304-7310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Parent, M. A., L. B. Wilhelm, L. W. Kummer, F. M. Szaba, I. K. Mullarky, and S. T. Smiley. 2006. Gamma interferon, tumor necrosis factor alpha, and nitric oxide synthase 2, key elements of cellular immunity, perform critical protective functions during humoral defense against lethal pulmonary Yersinia pestis infection. Infect. Immun. 74:3381-3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Perry, R. D., A. G. Bobrov, O. Kirillina, H. A. Jones, L. Pedersen, J. Abney, and J. D. Fetherston. 2004. Temperature regulation of the hemin storage (Hms+) phenotype of Yersinia pestis is posttranscriptional. J. Bacteriol. 186:1638-1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Perry, R. D., S. C. Straley, J. D. Fetherston, D. J. Rose, J. Gregor, and F. R. Blattner. 1998. DNA sequencing and analysis of the low-Ca2+-response plasmid pCD1 of Yersinia pestis KIM5. Infect. Immun. 66:4611-4623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Petersen, S., and G. M. Young. 2002. Essential role for cyclic AMP and its receptor protein in Yersinia enterocolitica virulence. Infect. Immun. 70:3665-3672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Postma, P. 1986. Catabolite repression and related phenomena. Symp. Soc. Gen. Microbiol. 39:21-49. [Google Scholar]
- 40.Powell, B. S., G. P. Andrews, J. T. Enama, S. Jendrek, C. Bolt, P. Worsham, J. K. Pullen, W. Ribot, H. Hines, L. Smith, D. G. Heath, and J. J. Adamovicz. 2005. Design and testing for a nontagged F1-V fusion protein as vaccine antigen against bubonic and pneumonic plague. Biotechnol. Prog. 21:1490-1510. [DOI] [PubMed] [Google Scholar]
- 41.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty per cent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 42.Sheehan, K. C., N. H. Ruddle, and R. D. Schreiber. 1989. Generation and characterization of hamster monoclonal antibodies that neutralize murine tumor necrosis factors. J. Immunol. 142:3884-3893. [PubMed] [Google Scholar]
- 43.Sing, A., D. Rost, N. Tvardovskaia, A. Roggenkamp, A. Wiedemann, C. J. Kirschning, M. Aepfelbacher, and J. Heesemann. 2002. Yersinia V-antigen exploits toll-like receptor 2 and CD14 for interleukin 10-mediated immunosuppression. J. Exp. Med. 196:1017-1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Skorupski, K., and R. K. Taylor. 1997. Cyclic AMP and its receptor protein negatively regulate the coordinate expression of cholera toxin and toxin-coregulated pilus in Vibrio cholerae. Proc. Natl. Acad. Sci. U. S. A. 94:265-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Smiley, S. T. 2008. Current challenges in the development of vaccines for pneumonic plague. Expert Rev. Vaccines 7:209-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Straley, S. C., and W. S. Bowmer. 1986. Virulence genes regulated at the transcriptional level by Ca2+ in Yersinia pestis include structural genes for outer membrane proteins. Infect. Immun. 51:445-454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sun, W., K. L. Roland, C. G. Branger, X. Kuang, and R. Curtiss III. 2009. The role of relA and spoT in Yersinia pestis KIM5+ pathogenicity. PLoS One 4:e6720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sun, W., S. Wang, and R. Curtiss III. 2008. Highly efficient method for introducing successive multiple scarless gene deletions and markerless gene insertions into the Yersinia pestis chromosome. Appl. Environ. Microbiol. 74:4241-4245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Titball, R. W., and E. D. Williamson. 2004. Yersinia pestis (plague) vaccines. Expert Opin. Biol. Ther. 4:965-973. [DOI] [PubMed] [Google Scholar]
- 50.Une, T., and R. R. Brubaker. 1984. In vivo comparison of avirulent Vwa- and Pgm- or Pstr phenotypes of Yersiniae. Infect. Immun. 43:895-900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Weekly Epidemiological Record. 2003. Human plague in 2000 and 2001. Wkly. Epidemiol. Rec. 78:130-135. [PubMed] [Google Scholar]
- 52.Welkos, S., M. L. Pitt, M. Martinez, A. Friedlander, P. Vogel, and R. Tammariello. 2002. Determination of the virulence of the pigmentation-deficient and pigmentation-/plasminogen activator-deficient strains of Yersinia pestis in non-human primate and mouse models of pneumonic plague. Vaccine 20:2206-2214. [DOI] [PubMed] [Google Scholar]
- 53.Williamson, E. D., H. C. Flick-Smith, E. Waters, J. Miller, I. Hodgson, C. S. Le Butt, and J. Hill. 2007. Immunogenicity of the rF1+rV vaccine for plague with identification of potential immune correlates. Microb. Pathog. 42:11-21. [DOI] [PubMed] [Google Scholar]
- 54.Zhan, L., Y. Han, L. Yang, J. Geng, Y. Li, H. Gao, Z. Guo, W. Fan, G. Li, L. Zhang, C. Qin, D. Zhou, and R. Yang. 2008. The cyclic AMP receptor protein, CRP, is required for both virulence and expression of the minimal CRP regulon in Yersinia pestis biovar microtus. Infect. Immun. 76:5028-5037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhan, L., L. Yang, L. Zhou, Y. Li, H. Gao, Z. Guo, L. Zhang, C. Qin, D. Zhou, and R. Yang. 2009. Direct and negative regulation of the sycO-ypkA-ypoJ operon by cyclic AMP receptor protein (CRP) in Yersinia pestis. BMC Microbiol. 9:178. [DOI] [PMC free article] [PubMed] [Google Scholar]