Abstract
Azithromycin (AZM) is a major drug used in the treatment and prophylaxis of infections caused by Chlamydia, yet no significant clinical resistance has been reported for these obligate intracellular bacteria. Nevertheless, spontaneous AZM resistance (Azmr) arose in vitro at frequencies ranging from 3 × 10−8 to 8 × 10−10 for clonal isolates of Chlamydia caviae, which is a natural pathogen of guinea pigs. Sequencing of the unique 23S rRNA gene copy in 44 independent Azmr isolates identified single mutations at position A2058 or A2059 (Escherichia coli numbering system). While SP6AZ1 (A2058C) and SP6AZ2 (A2059C) Azmr mutants showed growth defects in cell culture and were less pathogenic in the guinea pig ocular infection model than in the parent SP6, the three isogenic C. caviae isolates grew equally well in the animal. On the other hand, coinoculation of the C. caviae parent strain with one of the Azmr strains was detrimental for the mutant strain. This apparent lack of association between pathology and bacterial load in vivo showed that virulence of the two Azmr mutants of C. caviae was attenuated. While chlamydial growth in vitro reflects the ability of the bacteria to multiply in permissive cells, survival in the host is a balance between cellular multiplication and clearance by the host immune system. The obligate intracellular nature of Chlamydia may therefore limit emergence of resistance in vivo due to the strength of the immune response induced by the wild-type antibiotic-sensitive bacteria at the time of antibiotic treatment.
Chlamydiae are Gram-negative obligate intracellular pathogens that are responsible for a multitude of diseases in humans and in animals. They employ a biphasic developmental cycle consisting of environmentally stable and metabolically inactive but infectious elementary bodies (EBs), responsible for transmission, and strictly intracellular, metabolically active, and replicative reticulate bodies (RBs) (1). Infection starts when one EB is endocytosed by a susceptible eukaryotic cell and resides within a cytoplasmic vacuole termed the inclusion, where it transforms into the RB. After replicating by binary fission, RBs transform back to the infectious form at 18 to 48 h postinfection, depending on the species, before being released to the cell's exterior, where they start a new round of infection in neighboring host cells. Although chlamydiae may cause direct damage to the epithelium through this cycle of infection and cell lysis, the primary pathology is mediated by the host response to the infection (28, 33). Chlamydial infections are indeed characterized by an initial intense inflammation, which is a major cause of the pathology, while repeated or chronic infections may result in increased tissue damage and scarring via acute inflammation and a T-cell-mediated response.
The currently recommended first-line therapeutic regimens for chlamydial infections are 1 week of doxycycline, a tetracycline (Tet) derivative, or a single dose of the macrolide azithromycin (AZM) (31). AZM is also used for chemoprophylaxis of blinding trachoma, a chronic infection caused by ocular serovars of Chlamydia trachomatis, common in underdeveloped and developing countries (12). Tet and macrolide antibiotics inhibit bacterial translation by binding to the 30S and 50S ribosomal subunits, respectively. Although extensive use of drugs has been known to favor the selection of resistance in just about every other bacterial pathogen, including Chlamydia suis in the pig (11), treatment failures for Chlamydia have been attributed mostly to reinfection rather than real genotypic resistance due to chromosomal mutations (15, 36). However, we showed previously that the low number of rRNA operons in Chlamydia presents an actual risk for emergence of resistance against the current preferred therapies. Accordingly, we have shown that the frequency of spontaneous resistance to spectinomycin (5), kasugamycin (7; R. Binet and A. T. Maurelli, submitted for publication), or AZM and other macrolides (6) is at least 2 to 3 logs higher in Chlamydia psittaci 6BC harboring a single rRNA operon than in C. trachomatis serovar L2 with two rRNA chromosomal copies. Only a low level of AZM resistance (0.8 μg/ml) was obtained for C. trachomatis L2 in the laboratory because of a Gln-to-Lys substitution in ribosomal protein L4, which is encoded by a single gene in the bacterial chromosome (6). Because the physiological burden of resistance mutations is an important factor that affects the appearance, stability, and maintenance of the phenotype (2, 19), we suggested that the continued good clinical efficacy of AZM for Chlamydia is linked to the deleterious effects conferred by antibiotic resistance mutations on bacterial fitness, including growth rate, transmission, or virulence. Each antibiotic-resistant mutant of C. trachomatis L2 or C. psittaci 6BC tested is generally affected in its ability to grow and compete with the isogenic parent strain in cell culture. Thus, we can assume that these chlamydial variants would not be as pathogenic to humans as the parent strain unless secondary mutations can compensate for the fitness cost originally incurred by the antibiotic resistance mutation (6).
Studying host-pathogen interactions in humans presents limitations that can be overcome with the use of animal models. For example, guinea pigs infected intravaginally with C. caviae, the agent of guinea pig inclusion conjunctivitis (GPIC), develop a disease which remarkably parallels the human chlamydial genital infection with regard to pathogenesis, pathology, and immunology (26). In addition, ocular infection of guinea pigs with C. caviae generates an acute conjunctivitis that is easily monitored. Hence, this study aimed at analyzing the biological costs of point mutations in the 23S rRNA gene conferring Azmr to C. caviae, in cell culture as well as in vivo in its natural host. Although changes from A to C at position 2058 or 2059 in the 23S rRNA gene lowered the production of infectious particles in cell culture by C. caviae, we did not notice any differences between the abilities of Azmr mutants and the wild-type strain to survive in the host in the absence of antibiotic selection. The in vivo fitness cost conferred by the resistance mutations was seen only in the intensity of the pathological response, and after experiments measuring competition between each Azmr mutant isolate and its isogenic parent in the host. The implications of these results on the biology and potential for emergence of antibiotic resistance in Chlamydia are discussed.
MATERIALS AND METHODS
Titration, antimicrobial susceptibility testing, and isolation of C. caviae mutants in the plaque assay.
The susceptibilities of C. caviae strains to AZM, purchased from Sigma Chemical Co., were determined in a plaque assay using mouse fibroblast L2 cells as described in reference 5. The MIC was defined as the drug concentration that inhibits the development of 105 chlamydial PFU in a confluent L2 monolayer in a 60-mm dish. A maximum concentration of 20 μg/ml AZM was tested, as this concentration was already 10 times the physiological level attained in the body during treatment (16). To isolate spontaneous Azmr variants, confluent monolayers grown in 60-mm dishes were infected with 107 to 108 PFU, corresponding to multiplicities of infection (MOIs) of 1 and 10, respectively, and AZM was added at 2 h postinoculation (p.i.) at concentrations ranging from 0.5 to 2 μg/ml. The frequency of spontaneous mutation to drug resistance was determined by dividing the number of PFU on selective medium by the number of PFU added to the monolayer (as measured by titration of PFU in the absence of antibiotic) (5).
To monitor the stability of the resistance phenotype in C. caviae SP6AZ1 and SP6AZ2, we compared the numbers of PFU obtained in the absence and presence of antibiotic following the growth of each variant for a minimum of 14 days in the plaque assay in the absence of AZM. Sizes of a minimum of 100 plaques were determined at 7 days p.i. and averaged.
PCR and DNA sequencing of the macrolide resistance targets.
Total genomic DNA was prepared from infected cells with DNeasy tissue kits (Qiagen). Part of the C. caviae 23S rRNA gene was amplified by PCR using primer RB45 (5′-CACACCCAACCTATCAAC-3′) and primer 6BC8 (5′-AGCTGTTGATGGTGACCGTAC-3′), purified, and then sequenced using primer AZM-F (5′-TGAACCTAAGCCCTGGTGAATG-3′) as described previously (6). DNA sequences for each antibiotic-resistant isolate were aligned using Clone Manager 9 (Scientific & Educational Software, Durham, NC) and compared to the respective DNA sequence obtained for the wild-type parental strain.
Physiological cost associated with the mutations. (i) Pure culture.
C. caviae infectivity was determined while the strains were growing in pure culture in the absence of antibiotic selection. Confluent mouse fibroblast monolayers in 60-mm dishes were infected with 3 × 105 inclusion-forming units (IFU) of C. caviae wild-type SP6, 1 × 106 IFU of SP6AZ1, or 9 × 105 IFU of SP6AZ2 and incubated at 37°C in 5% CO2. After 2 h of infection, the inoculum was removed and the cells were incubated in infection medium, i.e., Dulbecco's modified Eagle's medium (DMEM) supplemented with 10% fetal bovine serum (FBS), 1× MEM nonessential amino acid solution (Sigma-Aldrich), and 2 μg of cycloheximide per ml. Duplicate dishes were harvested at various times after inoculation. The supernatants were removed, centrifuged at 13,000 rpm for 10 min, resuspended in 400 μl of SPG (250 mM sucrose, 10 mM sodium phosphate, 5 mM l-glutamic acid), pulse-sonicated, and stored at −80°C until they were thawed for determination of the progeny IFU released in the growth medium. Infected cells were scraped from each dish with a rubber scraper, rinsed with 400 μl of SPG, collected into a tube, pulse-sonicated, and stored at −80°C until they were thawed for determination of the progeny IFU contained in the infected cells.
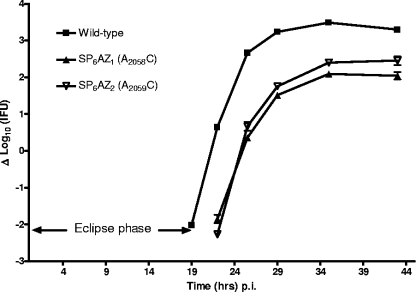
For quantification of C. caviae infectious titers, supernatant and pellet harvests were serially diluted in infection medium and 0.2 ml of each dilution was centrifuged (3,000 rpm, 1 h, 37°C) onto duplicate cultures of McCoy cells grown in flat-bottom 96-well plates (Costar). Plates were incubated for 1 h at 37°C before replacement of the inocula with 0.2 ml of infection medium supplemented with 0.2 μg/ml AZM, when appropriate. After 24 h of incubation, cells were fixed with methanol and stained with a fluorescein isothiocyanate (FITC)-conjugated Chlamydia genus-specific monoclonal antibody (MAb) (Pathfinder Chlamydia culture confirmation system; Bio-Rad). Chlamydial inclusions were counted by fluorescence microscopy and the results expressed as numbers of IFU per sample. For clarity, the number of IFU in the pellet was added to the number of IFU in the supernatant to represent the total number of EBs in the wells. In the infectivity curves shown in Fig. 1, the numbers of EBs produced at 19, 22, 25.5, 29, 35, and 43 h p.i. were related to the number of infectious particles at the time of infection. The rate of 2-fold EB increase was estimated using the Prism 3.0 software program from a plot of ln(PFU) = f(time) (with goodness-of-fit [r2] values of 0.98 for SP6 and 0.99 for SP6AZ1 and SP6AZ2), where the slope is ln2/rate of 2-fold EB increase (h). The rate of EB production is the number of IFU produced at 43 h p.i. divided by the number of infectious particles initially used for infection.
FIG. 1.
Impact of AZM resistance mutations on the growth of C. caviae SP6 variants in mouse fibroblast L2 cells. Confluent mouse fibroblasts in 60-mm dishes were infected with wild-type C. caviae SP6 and two isogenic mutants with mutations in the 23S rRNA gene, SP6AZ1 (A2058C) and SP6AZ2 (A2059C). The growth medium from each dish (i.e., culture supernatant) and then the infected monolayers were collected at regular time intervals. Infectious particles were harvested into 400 μl SPG. IFU were enumerated after infection onto McCoy cells and immunodetection of the chlamydial inclusions at 24 h p.i. The total number of infectious particles was determined by adding both titers, i.e., those of the supernatant and the infected monolayer, at the respective time point. Data are expressed as means ± standard deviations of results from triplicate determinations and are related to the number of IFU added to the monolayer.
(ii) Pairwise competition experiment.
Wild-type C. caviae SP6 and one isogenic representative for each Azmr variant were coinfected at a ratio of ∼1:1 to an MOI of 0.1 in confluent mouse fibroblast monolayers in 60-mm dishes and incubated at 37°C in 5% CO2. After 2 h of infection, the inoculum was removed. The cells were washed twice with DMEM and incubated in infection medium. EBs were harvested in triplicate after sonication of the infected cells at 43 h p.i. and stored at −80°C in 400 μl SPG. Approximately 5 × 105 infectious particles from the mixed infection obtained at 43 h p.i. were passed a second time into fresh monolayers in 60-mm dishes, allowed to grow for another 43 h, and harvested as before. The titers of serial dilutions of each harvest were determined in duplicate using McCoy cells grown in 96-well plates, as described above, in both drug-free (total IFU) and drug-containing (Azmr IFU) DMEM. The competition index (CI) was defined as the ratio of the output mutant/wild-type ratio to the input mutant/wild-type ratio (4).
Guinea pigs.
Female Hartley strain guinea pigs, each weighing 450 to 500 g, were obtained from Charles River Laboratories (Boston, MA). All animals were housed individually in cages covered with fiberglass filter tops and given food and water ad libitum and maintained on a 12:12 light-dark cycle. Each experimental group routinely consisted of five animals. All animal experiments and protocols were approved by the Animal Care and Use Committee of the Arkansas Children's Hospital Research Institute.
Conjunctival infection of guinea pigs.
Guinea pigs were infected in the conjunctiva of both eyes by instilling 20 μl of SPG containing 104 IFU of C. caviae directly into the conjunctival sac. This dose ensures 100% infection and produces a strong pathological response that is easily quantified by gross observation. Pathological changes were assessed daily on each eye by using a 0-to-4+ scale while evaluating palpebral and bulbar conjunctiva for erythema, edema, and exudation (27). The scores are defined as follows: 1+, slight erythema or edema of either the palpebral or the bulbar conjunctiva; 2+, definite erythema or edema of either the palpebral or the bulbar conjunctiva; 3+, definite erythema or edema of both the palpebral and the bulbar conjunctiva; 4+, definite erythema or edema of both the palpebral and the bulbar conjunctiva and the presence of exudate. In order to maintain consistency, only one individual evaluated the pathology. Conjunctival material for the isolation and quantification of chlamydiae was collected from the conjunctiva by using a Dacron swab and then placing the swab in sucrose-phosphate transport medium. There was no effect of the swab collection on the conjunctival pathology. Numbers of IFU were determined by culture in McCoy cells. In order to quantify the AZM mutants, swab material was cultured in the presence of AZM. The total number of wild-type IFU was then determined by subtracting the number of IFU obtained in the AZM culture from that obtained in the culture without AZM. Groups of animals were compared statistically using a 2-factor (group and time) analysis of variance (ANOVA) with repeated measures.
RESULTS
Isolation of distinct clonal populations of virulent C. caviae.
Guinea pig inclusion conjunctivitis is a naturally occurring chlamydial disease which is normally self-limiting and leaves the animal partially resistant to reinfection. The causative agent was first recovered from conjunctival scrapings by Murray in 1964 (22) and was obtained by Almen Barron at passage 5 or 6 in the late 1960s. It has been subsequently propagated in the Barron/Rank laboratory since that time, first in chick embryos and then in tissue culture, without any kind of clonal purification. Consequently, C. caviae laboratory stocks are expected to be very polymorphic. Clonal virulent populations of C. caviae were prepared by purifying and then expanding single plaques formed by the bacteria collected from the eye of an infected guinea pig in the plaque assay. This assay is based on the ability of the bacteria to invade into, replicate within, and lyse mouse fibroblast L2 cells in a confluent monolayer (3). An agarose overlay containing all the nutrients necessary to sustain cell viability is applied to the cell monolayer at the end of the invasion period so that infectious particles (EBs) released from the infected cells can reinfect neighboring cells only. Therefore, the initial infection of a single eukaryotic cell by a single EB will lead to the formation of an individual plaque that can be visualized by staining the monolayer, usually after 5 to 7 days for C. caviae; purified; and serially expanded to obtain a clonal bacterial population. Accordingly, we prepared 10 clonal isolates of C. caviae (SP1 to SP10) originating from the eye of a guinea pig infected 9 or 12 days earlier (Table 1).
TABLE 1.
Ribosomal mutations observed in spontaneous Azmr isolates of C. caviaea
| Day (postinoculation) of recovery from animal | Wild-type clonal strainb | Frequency of spontaneous AZM resistancec | No. of isolates with mutation at indicated position in 23S rRNA gene (representative strain) |
|||
|---|---|---|---|---|---|---|
| A2058C | A2058G | A2059C | A2059G | |||
| 9 | SP1 | (4.3 ± 7.1) × 10−9 | 6 (SP1AZ1) | 0 | 0 | 0 |
| SP2 | (2.7 ± 7.1) × 10−9 | 0 | 0 | 1 (SP2AZ1) | 0 | |
| SP5 | 10−9 | 0 | 0 | 3 (SP5AZ1) | 0 | |
| SP6 | 10−9 | 1 (SP6AZ1) | 0 | 1 (SP6AZ2) | 0 | |
| 12 | SP3 | (2.9 ± 3.4) × 10−8 | 23 (SP3AZ1) | 0 | 0 | 0 |
| SP4 | 7.7 × 10−10 | 1 (SP4AZ1) | 0 | 0 | 0 | |
| SP7 | 10−9 | 0 | 1 (SP7AZ1) | 0 | 0 | |
| SP8 | (2.0 ± 2.8) × 10−9 | 4 (SP8AZ1) | 0 | 0 | 1 (SP8AZ3) | |
| SP9 | (4.5 ± 6.3) × 10−9 | 0 | 0 | 1 (SP9AZ1) | 0 | |
| SP10 | 2.0 × 10−9 | 1 (SP10AZ2) | 0 | 1 (SP10AZ1) | 0 | |
Strains in bold were used in in vitro and in vivo studies.
Infectious particles from a single plaque were expanded during three to four developmental cycles to obtain clonal populations of C. caviae.
The frequencies of appearance of resistant mutants are relative to the total number of PFU infecting a confluent mouse fibroblast monolayer growing in a 60-mm dish ± the standard deviation.
Genetic characterization of spontaneous Azmr variants from virulent clonal C. caviae isolates.
To select for resistant mutants, we generally infect confluent monolayers in 60-mm dishes with 107 to 108 infectious particles at concentrations of antibiotic high enough to inhibit the large inoculum (5-7). Accordingly, the 10 clonal populations of C. caviae obtained after four serial expansions of 10 individual plaques in the absence of drug were grown in the plaque assay in the presence of 0.5 to 2 μg/ml AZM. Plaques surviving the antibiotic pressure appeared at frequencies ranging from about 3 × 10−8 to 8 × 10−10, depending on the isolates, highlighting the variability and possibly genetic differences between the different clonal isolates of C. caviae (Table 1). Forty-five spontaneous Azmr plaques were isolated and expanded in the presence of AZM for DNA analysis as previously described. Each resistant mutant showed a single mutation in the unique 23S rRNA gene at position A2058 or A2059 (Escherichia coli numbering system); both of these mutations are known to confer the highest levels of macrolide resistance in other organisms (35), including C. psittaci 6BC (6). Two independent Azmr mutants (i.e., SP6AZ1 and SP6AZ2) (Table 1) were then compared for growth in pure culture or in competition with their isogenic parent (i.e., SP6), in vitro and in vivo.
Cost of Azmr mutations to the growth of C. caviae in vitro.
A single mutation in the single 23S rRNA C. caviae gene conferred high-level resistance to AZM, with a MIC greater than 20 μg/ml in the plaque assay, compared to 100 ng/ml for the parental C. caviae strain. This suggests that the mutants should have a clear growth advantage over the sensitive parent in the presence of drug. However, to be able to survive in a natural environment, a bacterium carrying a mutated allele must also compete with the wild-type ancestor bacterial population in the absence of drug. The outcome of the competition process depends on the bacterium's relative fitness, defined as the efficiency of multiplication and transmission of the mutant cell in comparison with that of the wild-type ancestor strain (2). C. caviae SP6 Azmr variants harboring the A2058C (i.e., SP6AZ1) and A2059C (i.e., SP6AZ2) mutations in the 23S rRNA gene formed plaques in mouse fibroblast L2 monolayers that were 34% and 53% smaller, respectively, than those formed by the parent strain in the absence of drug (Table 2). Since the three C. caviae isolates are isogenic, apart from their rRNA mutations, this observed decrease in plaque size is directly linked to the effect of the mutations on the bacterial physiology in vitro.
TABLE 2.
Physiological costs due to mutations in the 23S rRNA gene associated with Azmr in C. caviae SP6
| C. caviae strain | 23S rRNA mutationa | Plaque sizeb (mm) | Duration of eclipse phase (h)c | Rate of 2-fold EB increase (min)c,e | EB generation rate (fold increase)f | Competition indexg at indicated no. of passages |
|
|---|---|---|---|---|---|---|---|
| One (43 h p.i.) | Two (86 h p.i.)h | ||||||
| SP6 | None (wild type) | 0.98 ± 0.14 | 19 | 20 | 1,530 ± 427 | NA | NA |
| SP6AZ1 | A2058C | 0.65 ± 0.13 | 19-22d | 29 | 113 ± 51 | 0.15 ± 0.03 | 0.06 ± 0.01 |
| SP6AZ2 | A2059C | 0.46 ± 0.17 | 22 | 21.6 | 256 ± 94 | 0.28 ± 0.05 | 0.17 ± 0.07 |
E. coli numbering system.
The sizes of a minimum of 34 individual plaques were determined for each strain in the absence of antibiotic at 7 days p.i. and averaged.
Data obtained from Fig. 1.
The eclipse phase lasted for more than 19 h but less than 22 h.
The rate of 2-fold EB increase was estimated as described in Materials and Methods.
The number of IFU produced at 43 h p.i. divided by the number used at the time of infection was different for each of the three C. caviae strains (P < 0.0001; t test).
The competition index is defined as the ratio of the output mutant/wild-type ratio at the indicated time p.i. to the input mutant/wild-type ratio. NA, not applicable.
Determined after a second 43-h passage.
The developmental cycle of Chlamydia spp. alternates between replication and growth as RBs and conversion to EBs for transmission (1). When we followed the formation of infectious particles throughout one developmental cycle in the absence of drug (Fig. 1), it was clear that both C. caviae Azmr mutants were delayed in the RB-to-EB transition, as seen by their extended eclipse phase, i.e., the period in which infectious progeny EBs have differentiated into noninfectious RBs, in comparison to the level for the parent strain (Table 2). Yet, the doubling time for EB formation during the exponential phase of the development cycle was severely affected only for SP6AZ1 with the A2058C mutation, i.e., 29 min versus 21.5 and 20 min for SP6AZ2 with the A2059C mutation and the wild-type SP6 C. caviae parent, respectively (Table 2). Nevertheless, EB production seemed to plateau at the same time for each of the three isolates, i.e., at about 34 h p.i. (Fig. 1). As a result, the final rate of EB production per development cycle was about 10-fold lower for the two Azmr mutants than for the isogenic sensitive strain (Table 2).
The fitness cost conferred by the A2058C and A2059C mutations in the 23S rRNA gene was further confirmed during coinfection of wild-type C. caviae SP6 with each Azmr isogenic variant in L2 cell monolayers in the absence of selection. The competition indices (CIs) (4) ranged from 0.15 to 0.28 at the end of the first round of competition and 0.06 to 0.17 after the second round, therefore demonstrating that both mutants were clearly outcompeted by the parent strain in vitro (Table 2).
Cost of Azmr mutations to the growth of C. caviae in single infection in vivo.
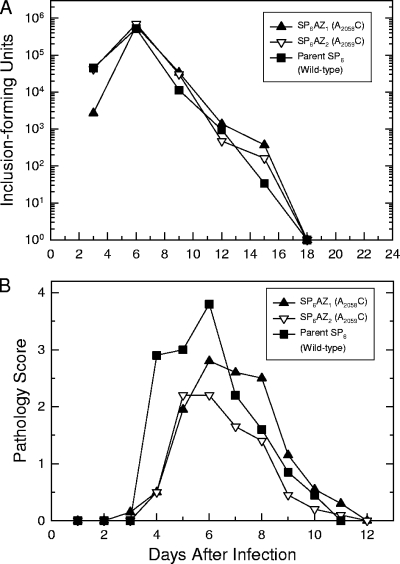
Because the bacterial traits defining fitness in an in vitro situation might be different from the ones important in the natural biological niche, we studied the growth and virulence of two Azmr C. caviae mutants and their isogenic parent in guinea pigs by using the ocular infection model. When groups of five guinea pigs were inoculated in both eyes with 104 IFU of the wild-type parent SP6, the course of the infection closely paralleled that reported previously for the wild-type polymorphic laboratory strain (Fig. 2). Infection reached a peak at about day 6 and was essentially cleared by day 18, with a resolution of the pathological response by day 12. When the Azmr mutants were inoculated into the conjunctiva, there was no difference in the recovery of IFU after the peak of infection, nor was there a difference in the numbers of days in which the organisms were shed (Fig. 2A). This showed that the A2058C and A2059C mutations in the 23S rRNA gene had no effect on the ability of the organism to infect and grow in the natural environment. Nevertheless, the intensity of conjunctival inflammation as reflected by the pathology score (Fig. 2B) was significantly attenuated for the two Azmr mutants in comparison to the level for the parent strain (P < 0.001). Indeed, while the parent SP6 reached a maximum pathology score of 4, SP6AZ1 reached a maximum pathology score of 3 and SP6AZ2 a score of 2. This showed that the two Azmr mutations lowered C. caviae virulence without affecting the ability of the bacteria to persist in the host in single infection.
FIG. 2.
Impact of AZM resistance mutations on the virulence of C. caviae SP6 variants in the natural host. Ten thousand IFU from the three isogenic C. caviae isolates, SP6, SP6AZ1 (A2058C), and SP6AZ2 (A2059C), were separately inoculated in both eyes in five animals per sample. Two independent experiments were performed and showed the same trend. The mean course of infection for one set is presented. (A) Recovery of infectious particles. Two swabs were collected every third day from the second eye. IFU were enumerated after infection onto McCoy cells from one swab, and the other was stored at −80°C. The data points represent the mean numbers of IFU for the 5 animals in the group. There were no significant differences among the 3 groups as determined by a 2-factor ANOVA with repeated measures. (B) Conjunctival pathology. Conjunctival pathology was scored every day for each eye on a scale from 0 to 4. The scores represent the means of results from 10 eyes. The scores for both eyes of an animal were always consistent, i.e., different by no more than 1 number. The pathology of animals infected with both SP6AZ1 and SP6AZ2 was significantly different from that obtained with the parent strain (P < 0.001), as determined by a 2-factor ANOVA with repeated measures.
Cost of Azmr mutations to the growth of C. caviae in competitive infection in vivo.
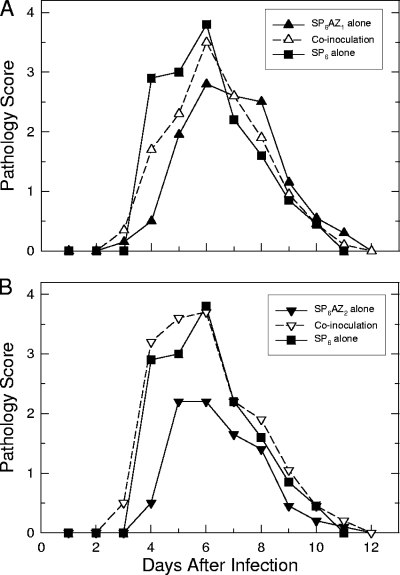
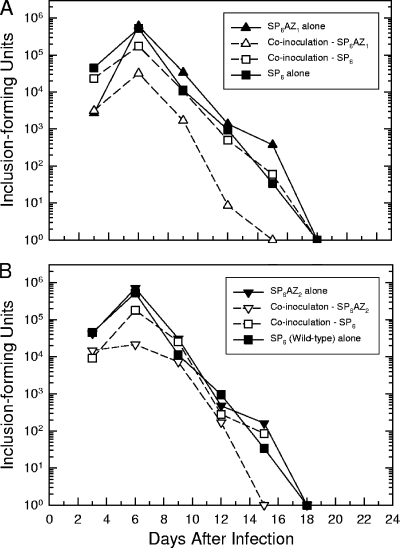
The ability of the two 23S rRNA mutants to persist in the host similarly to the wild-type strain was surprising, considering that the developmental cycles of the two mutants were affected in cell culture. Consequently, we tested SP6AZ1 and SP6AZ2 for their abilities to compete with the isogenic parent strain in the natural (guinea pig) environment. Equal numbers of mutant and wild-type bacteria were mixed and then inoculated in the conjunctiva of guinea pigs, and the infection was monitored over 18 days as described above. In general, the pathology scores in the coinoculation group were significantly higher than that obtained with the mutant alone (Fig. 3A and B), although in the coinoculation group containing SP6AZ1, the pathology score was still somewhat lower than that obtained with the parent strain alone (Fig. 3A). Nevertheless, these data demonstrated that the pathological response to the wild-type strain was dominant in the host. Interestingly, in contrast with the previous single infections, we observed a nearly 1-log reduction in the recovery of each mutant in the presence of the SP6 isolate over the course of infection in comparison to the level for the parent strain in the mixture (P < 0.001). The competition indices (4) calculated at 6 to 12 days postinfection ranged from 0.18 to 0.02 for SP6AZ1 and 0.12 to 0.61 for SP6AZ2. Then, both mutants were cleared from the host at 15 days p.i., whereas the parent was cleared 3 days later, at 18 days p.i. (Fig. 4A and B). This showed that both Azmr variants were clearly outcompeted by the antibiotic-sensitive parent strain in the ocular infection model in the absence of drug. Interestingly, while significantly more bacteria of the parent strain than of either mutant were recovered in the coinoculation group, the parent strain still did not grow as well as it did when inoculated into the animal alone. Consequently, the A2058C and A2059C mutations in the 23S rRNA gene, conferring resistance to AZM, bear a fitness cost to C. caviae's abilities to grow in cell culture and to compete with the wild-type strain in the natural host environment.
FIG. 3.
Conjunctival pathology observed after single infection or coinoculation of wild-type C. caviae SP6 and the two 23S rRNA mutants, SP6AZ1 (A2058C) and SP6AZ2 (A2059C), in the natural host. Ten thousand IFU from the wild type and one Azmr isogenic mutant of C. caviae were coinoculated in both eyes of five animals per sample. Conjunctival pathology was scored as described in the legend to Fig. 2. Results from the coinfection experiments are shown with dotted lines, while 12 results from the single infections (from Fig. 2B) are shown with solid lines. (A) The scores of the coinoculation group (P < 0.008) and the SP6AZ1-alone group (P < 0.001) were significantly different from that of the SP6-alone group as determined by a 2-factor ANOVA with repeated measures; however, the score of the SP6AZ1-alone group was significantly lower than that of the coinoculation group (P < 0.016). (B) The score of the coinoculation group (P < 0.008) was not significantly different from that of the SP6-alone group as determined by a 2-factor ANOVA with repeated measures. However, the score of the SP6AZ2-alone group (P < 0.001) was significantly lower than those of both the coinoculation group (P < 0.001) and the SP6-alone group (P < 0.001).
FIG. 4.
Competition between wild-type C. caviae SP6 and the two 23S rRNA mutants, SP6AZ1 (A2058C) and SP6AZ2 (A2059C), in the natural host. Coinoculation was performed as described in the legend to Fig. 3. Two swabs were collected every third day from one eye. IFU were enumerated after inoculation onto McCoy cells with (AZM IFU) and without (total IFU) AZM. The number of wild-type IFU was calculated as the total number of IFU minus the number of Azmr IFU. Results from the coinfection experiments are shown with dotted lines, while results from the single infections (from Fig. 2A) are shown with solid lines. (A) The level of SP6AZ1 in the coinoculation group was significantly lower than the levels of SP6AZ1 alone (P < 0.001), SP6 alone (P < 0.001), and SP6 in the coinoculation group (P < 0.001) as determined by a 2-factor ANOVA with repeated measures. The level of SP6AZ1 alone was not significantly lower than that of SP6 alone, but the level of SP6 in the coinoculation group was significantly different from that of SP6 alone (P < 0.001). (B) The level of SP6AZ2 in the coinoculation group was significantly lower than the levels of SP6AZ2 alone (P < 0.001), SP6 alone (P < 0.001), and SP6 in the coinoculation group (P < 0.001) as determined by a 2-factor ANOVA with repeated measures. The level of SP6AZ2 alone was significantly lower than that of SP6 alone (P < 0.02), and the level of SP6 in the coinoculation group was significantly different from that of SP6 alone (P < 0.001).
DISCUSSION
Azithromycin is probably the most frequently used antibiotic against Chlamydia infections today (31), yet mutations which confer Azmr in these obligate intracellular pathogen do not appear to be selected for in vivo (14, 15, 36). Of particular interest for this study, tetracycline-resistant isolates of C. suis, a swine strain of Chlamydia, started to appear in pig farms only 50 years after the introduction of chlortetracycline as a growth promoter to poultry, swine, and cattle (18). Consequently, emergence of antibiotic resistance is not an impossible scenario for chlamydiae, despite their isolated niche, which limits the opportunity for acquisition of antibiotic resistance genes from other organisms, and their particular biphasic developmental cycle, which constitutes an evolutionary bottleneck (34). We previously showed that the low number of rRNA operons in chlamydiae allows for the development of spontaneous AZM resistance in vitro (6). The present study is a continuation of these studies for analyzing the impacts of such mutations on bacterial physiology and virulence in vitro and in vivo, using C. caviae, a natural pathogen of guinea pigs, as a model.
Treatment failures (defined as Chlamydia persistence 1 month after treatment) following macrolide therapy have been reported for humans as well as animals, but most reports do not address the role of genetic resistance in the recurrence of chlamydial infections (15, 21, 24, 29, 36). We found that spontaneous high-level AZM resistance arose in C. caviae at frequencies that fall within the ones determined for C. psittaci 6BC or Mycobacterium avium, two other bacterial groups characterized by the presence of a single rRNA operon (6). Spontaneous AZM resistance occurred at frequencies ranging from 10−8 to 10−10, depending on the clonal population of C. caviae isolated from the host, suggesting that significant genomic differences exist among the bacteria present in the initial laboratory stock. High-level AZM resistance arose in C. caviae following a single mutation in the single 23S rRNA gene, resulting in either an A-to-C or an A-to-G mutation at position 2058 or 2059. Such mutations have been found to confer resistance to other clinically relevant antibiotics, such as the macrolide erythromycin and the lincosamide clindamycin, in other important bacterial pathogens, including mycobacteria and C. psittaci 6BC (6). Note that the A2058G substitution in 23S rRNA, which is the most common macrolide resistance mutation encountered (10, 35), was found in none of the 30 strains with spontaneous mutations conferring Azmr isolated previously for C. psittaci 6BC and in only 1 out of 45 independent mutants of C. caviae analyzed in this study, i.e., SP7. It is tempting to speculate that SP7 possesses genetic factors such as an intragenic or extragenic compensatory mutation to balance the cost of this mutation to chlamydiae (8, 20).
The rate of increase in frequency of resistance to an antibiotic is directly proportional to the efficacy of the drug and the extent of its use and is inversely proportional to the cost that resistance imposes on bacterial fitness, i.e., the strain's rate of infectious transmission and its ability to compete with other strains (2). When we compared the growth in cell culture of the susceptible parent to that of two isogenic C. caviae Azmr variants in the absence of selection, it was clear that the A2058C and A2059C mutations in the 23S RNA gene drastically affected the transmissibility of C. caviae, in agreement with our previous study with C. psittaci 6BC (6). The rate of formation of infectious particles was about 10 times lower for the Azmr mutants, and they were rapidly outcompeted by the parent strain in cell culture, where growth conditions had been optimized for chlamydial growth. In the more stressful natural environment of the guinea pig, both mutants were outcompeted and cleared 3 days earlier than the wild-type strain from the eyes of infected guinea pigs. Consequently, the two Azmr C. caviae isolates would likely not persist in the absence of selection unless compensatory mutations are selected to adapt to the costs of chromosomal antibiotic resistance (8, 19, 20).
The processes of microbial infections are intimately linked to the immune responses of the host in its effort to resolve the infection. Although the A2058C and A2059G mutations in the 23S rRNA gene inhibited bacterial growth in cell culture, both mutants were surprisingly able to survive in the host as long as the parent in the ocular infection model: infections were self-limiting, peaked at about 6 days postinoculation, and lasted about 18 days for all three isolates, provided that the mutants were not in competition with the parent. To the best of our knowledge, such a discrepancy between growth in vitro and persistence in the host has never been described for any chlamydial isolates previously. The ability of the innate immune system to quickly recognize and respond to an invading pathogen is essential for controlling the infection. Clearly, survival in the host is a combination of both bacterial multiplication in the host and bacterial clearance by the host antimicrobial defense system. Growth of the two Azmr mutants was likely affected in vivo too, leading to fewer infected cells and hence lower levels of chemokine/cytokine production and a weaker inflammatory response than in animals infected with the parent wild-type C. caviae strain, which grew faster but induced a stronger inflammatory response. As a consequence, the survival rates of the fast-growing and the slow-growing strains were similar in the host in pure infection. In coinfection experiments, it is clear that the wild-type and the Azmr C. caviae isolates compete for growth and likely for nutrients, since the parent strain was not able to multiply to the same extent as when inoculated in the guinea pigs alone. Nevertheless, survival of the mutants was outbalanced by the strong host response elicited by the wild type, resulting in earlier clearance of the drug-resistant isolates. Mutations in rRNA that affect the general translational ability of the bacteria and thus the activity of multiprotein complexes such as secretion systems are, in addition, likely to increase the vulnerability of bacteria in the host.
What is responsible for Chlamydia pathogenesis is still a matter of debate and is likely the combination of the innate host responses and antigen-specific adaptive cellular immune responses which induce immunopathological tissue damage (28). Azmr mutations in the C. caviae SP6 isolate attenuated chlamydial virulence, as both SP6AZ1 and SP6AZ2 elicited pathological responses that were weaker than those elicited by the wild-type strain. Interestingly, there was a correlation between the reduction in the size of the plaques formed by the isolates in mouse fibroblast L2 cells and the reduction in conjunctival pathology: plaques formed by SP6AZ1, with the A2058C mutation, were bigger than those formed by SP6AZ2, with the A2059C mutation (34% and 53% the size seen for the parent SP6, respectively), and SP6AZ1 was also more virulent than SP6AZ2 in the ocular infection model. Interestingly, a similar relationship between plaque size and virulence had previously been noted for trachoma serovariants of C. trachomatis (17). However, Ramsey et al. recently proposed that chlamydial virulence is linked to the bacterial replication rate and the number of infectious particles produced per developmental cycle rather than to plaque size per se (25).
Though Azmr mutations at positions 2058 or 2059 of both C. psittaci 6BC BCRB and the C. caviae SP6 23S rRNA gene confer fitness costs associated with plaque size, growth in L2 mouse fibroblast cells, and presumably virulence, the A2058C mutation has a stronger physiological influence on C. psittaci 6BC than on C. caviae SP6. As the overall genetic context/environment affects the fitness cost associated with drug resistance, similar resistance mutations would bear different consequences, depending on strains, serovars, or even isolates of chlamydiae. It is likely that the more frequent resistant mutants emerged in bacteria that were better equipped to handle the resistance mutation, with fewer negative consequences to the bacterial physiology, rather than in bacteria that had a higher mutation rate. Under this hypothesis, the A2058C Azmr mutation would confer less fitness cost to the C. caviae isolate SP3, where this mutation appeared at a frequency of about 10−8, than to the isolate SP4, where the A2058C mutation emerged at a much lower rate.
It is clear that many interacting factors would influence the probability of AZM resistance development in chlamydial infections. Antibiotic resistant mutants selected in vivo tend to be ones with little or no fitness cost in vitro (13, 23, 30). For chlamydial mutants to persist in vivo, they would have to overcome the host clearance response induced by the wild-type bacterial population. However, it is not yet clear how much of this response would be elicited during treatment. Efficient antichlamydial treatments prevent transmission, cure the infection, and prevent the development of immunopathology. Nevertheless, they could also interfere with the acquisition of protective immunity, creating what has been termed an arrested immunity stage contributing to the current increases in the rates of C. trachomatis incidence and reinfection (9). AZM and other macrolides have additional immunomodulatory and anti-inflammatory properties that may also affect the development of a protective and/or pathological host response (32). If bacterial multiplication is essential for the acquisition of protective immunity, it would be interesting to examine if the two 23S rRNA mutants of C. caviae SP6 would be able to overcome the wild-type strain in the presence of AZM in the host. These results may further improve the understanding of chlamydial therapy and biology.
Acknowledgments
This work was supported by grants AI44033 (A.T.M.) and AI59650 (R.G.R.) from the National Institute of Allergy and Infectious Diseases, NIH.
Rachel Binet thanks Nancy E. Adams for cell culture assistance and Fatima Mareini for determination of C. caviae AZM MIC.
Footnotes
Published ahead of print on 11 January 2010.
REFERENCES
- 1.Abdelrahman, Y. M., and R. J. Belland. 2005. The chlamydial developmental cycle. FEMS Microbiol. Rev. 29:949-959. [DOI] [PubMed] [Google Scholar]
- 2.Andersson, D. I., and B. R. Levin. 1999. The biological cost of antibiotic resistance. Curr. Opin. Microbiol. 2:489-493. [DOI] [PubMed] [Google Scholar]
- 3.Banks, J., B. Eddie, J. Schachter, and K. F. Meyer. 1970. Plaque formation by Chlamydia in L cells. Infect. Immun. 1:259-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Binet, R., and A. T. Maurelli. 2005. Fitness cost due to mutations in the 16S rRNA associated with spectinomycin resistance in Chlamydia psittaci 6BC. Antimicrob. Agents Chemother. 49:4455-4464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Binet, R., and A. T. Maurelli. 2005. Frequency of spontaneous mutations that confer antibiotic resistance in Chlamydia spp. Antimicrob. Agents Chemother. 49:2865-2873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Binet, R., and A. T. Maurelli. 2007. Frequency of development and associated physiological cost of azithromycin resistance in Chlamydia psittaci 6BC and C. trachomatis L2. Antimicrob. Agents Chemother. 51:4267-4275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Binet, R., and A. T. Maurelli. 2009. Transformation and isolation of allelic exchange mutants of Chlamydia psittaci using recombinant DNA introduced by electroporation. Proc. Natl. Acad. Sci. U. S. A. 106:292-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bottger, E. C., B. Springer, M. Pletschette, and P. Sander. 1998. Fitness of antibiotic-resistant microorganisms and compensatory mutations. Nat. Med. 4:1343-1344. [DOI] [PubMed] [Google Scholar]
- 9.Brunham, R. C., and M. L. Rekart. 2008. The arrested immunity hypothesis and the epidemiology of chlamydia control. Sex. Transm. Dis. 35:53-54. [DOI] [PubMed] [Google Scholar]
- 10.Doucet-Populaire, F., K. Buriankova, J. Weiser, and J. L. Pernodet. 2002. Natural and acquired macrolide resistance in mycobacteria. Curr. Drug Targets Infect. Disord. 2:355-370. [DOI] [PubMed] [Google Scholar]
- 11.Dugan, J., D. D. Rockey, L. Jones, and A. A. Andersen. 2004. Tetracycline resistance in Chlamydia suis mediated by genomic islands inserted into the chlamydial inv-like gene. Antimicrob. Agents Chemother. 48:3989-3995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Emerson, P. M., M. Burton, A. W. Solomon, R. Bailey, and D. Mabey. 2006. The SAFE strategy for trachoma control: Using operational research for policy, planning and implementation. Bull. World Health Organ. 84:613-619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gagneux, S., C. D. Long, P. M. Small, T. Van, G. K. Schoolnik, and B. J. Bohannan. 2006. The competitive cost of antibiotic resistance in Mycobacterium tuberculosis. Science 312:1944-1946. [DOI] [PubMed] [Google Scholar]
- 14.Hong, K. C., J. Schachter, J. Moncada, Z. Zhou, J. House, and T. M. Lietman. 2009. Lack of macrolide resistance in Chlamydia trachomatis after mass azithromycin distributions for trachoma. Emerg. Infect. Dis. 15:1088-1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Horner, P. 2006. The case for further treatment studies of uncomplicated genital Chlamydia trachomatis infection. Sex. Transm. Infect. 82:340-343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jain, R., and L. H. Danziger. 2004. The macrolide antibiotics: a pharmacokinetic and pharmacodynamic overview. Curr. Pharm. Des. 10:3045-3053. [DOI] [PubMed] [Google Scholar]
- 17.Kari, L., W. M. Whitmire, J. H. Carlson, D. D. Crane, N. Reveneau, D. E. Nelson, D. C. Mabey, R. L. Bailey, M. J. Holland, G. McClarty, and H. D. Caldwell. 2008. Pathogenic diversity among Chlamydia trachomatis ocular strains in nonhuman primates is affected by subtle genomic variations. J. Infect. Dis. 197:449-456. [DOI] [PubMed] [Google Scholar]
- 18.Lenart, J., A. A. Andersen, and D. D. Rockey. 2001. Growth and development of tetracycline-resistant Chlamydia suis. Antimicrob. Agents Chemother. 45:2198-2203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lenski, R. E. 1998. Bacterial evolution and the cost of antibiotic resistance. Int. Microbiol. 1:265-270. [PubMed] [Google Scholar]
- 20.Maisnier-Patin, S., and D. I. Andersson. 2004. Adaptation to the deleterious effects of antimicrobial drug resistance mutations by compensatory evolution. Res. Microbiol. 155:360-369. [DOI] [PubMed] [Google Scholar]
- 21.Misyurina, O. Y., E. V. Chipitsyna, Y. P. Finashutina, V. N. Lazarev, T. A. Akopian, A. M. Savicheva, and V. M. Govorun. 2004. Mutations in a 23S rRNA gene of Chlamydia trachomatis associated with resistance to macrolides. Antimicrob. Agents Chemother. 48:1347-1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murray, E. S. 1964. Guinea pig inclusion conjunctivitis virus. I. Isolation and identification as a member of the pstittacosis-lymphogranuloma-trachoma group. J. Infect. Dis. 114:1-12. [DOI] [PubMed] [Google Scholar]
- 23.O'Neill, A. J., T. Huovinen, C. W. Fishwick, and I. Chopra. 2006. Molecular genetic and structural modeling studies of Staphylococcus aureus RNA polymerase and the fitness of rifampin resistance genotypes in relation to clinical prevalence. Antimicrob. Agents Chemother. 50:298-309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Owen, W. M., C. P. Sturgess, D. A. Harbour, K. Egan, and T. J. Gruffydd-Jones. 2003. Efficacy of azithromycin for the treatment of feline chlamydophilosis. J. Feline Med. Surg. 5:305-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ramsey, K. H., I. M. Sigar, J. H. Schripsema, C. J. Denman, A. K. Bowlin, G. A. Myers, and R. G. Rank. 2009. Strain and virulence diversity in the mouse pathogen Chlamydia muridarum. Infect. Immun. 77:3284-3293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rank, R. G., A. K. Bowlin, R. L. Reed, and T. Darville. 2003. Characterization of chlamydial genital infection resulting from sexual transmission from male to female guinea pigs and determination of infectious dose. Infect. Immun. 71:6148-6154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rank, R. G., C. Dascher, A. K. Bowlin, and P. M. Bavoil. 1995. Systemic immunization with Hsp60 alters the development of chlamydial ocular disease. Invest. Ophthalmol. Vis. Sci. 36:1344-1351. [PubMed] [Google Scholar]
- 28.Roan, N. R., and M. N. Starnbach. 2008. Immune-mediated control of Chlamydia infection. Cell. Microbiol. 10:9-19. [DOI] [PubMed] [Google Scholar]
- 29.Roblin, P. M., and M. R. Hammerschlag. 1998. Microbiologic efficacy of azithromycin and susceptibilities to azithromycin of isolates of Chlamydia pneumoniae from adults and children with community-acquired pneumonia. Antimicrob. Agents Chemother. 42:194-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sander, P., B. Springer, T. Prammananan, A. Sturmfels, M. Kappler, M. Pletschette, and E. C. Bottger. 2002. Fitness cost of chromosomal drug resistance-conferring mutations. Antimicrob. Agents Chemother. 46:1204-1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Senn, L., M. R. Hammerschlag, and G. Greub. 2005. Therapeutic approaches to Chlamydia infections. Expert Opin. Pharmacother. 6:2281-2290. [DOI] [PubMed] [Google Scholar]
- 32.Srivastava, P., H. C. Jha, S. Salhan, and A. Mittal. 2009. Azithromycin treatment modulates cytokine production in Chlamydia trachomatis infected women. Basic Clin. Pharmacol. Toxicol. 104:478-482. [DOI] [PubMed] [Google Scholar]
- 33.Stephens, R. S. 2003. The cellular paradigm of chlamydial pathogenesis. Trends Microbiol. 11:44-51. [DOI] [PubMed] [Google Scholar]
- 34.Stephens, R. S., G. Myers, M. Eppinger, and P. M. Bavoil. 2009. Divergence without difference: phylogenetics and taxonomy of Chlamydia resolved. FEMS Immunol. Med. Microbiol. 55:115-119. [DOI] [PubMed] [Google Scholar]
- 35.Vester, B., and S. Douthwaite. 2001. Macrolide resistance conferred by base substitutions in 23S rRNA. Antimicrob. Agents Chemother. 45:1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang, S. A., J. R. Papp, W. E. Stamm, R. W. Peeling, D. H. Martin, and K. K. Holmes. 2005. Evaluation of antimicrobial resistance and treatment failures for Chlamydia trachomatis: a meeting report. J. Infect. Dis. 191:917-923. [DOI] [PubMed] [Google Scholar]