Abstract
The hemagglutinin-neuraminidase (HN) glycoprotein plays a critical role in parainfluenza virus replication. We recently found that in addition to the catalytic binding site, HN of human parainfluenza virus type 1 (hPIV-1) may have a second receptor-binding site covered by an N-linked glycan at residue 173, which is near the region of the second receptor-binding site identified in Newcastle disease virus (NDV) HN (I. A. Alymova, G. Taylor, V. P. Mishin, M. Watanabe, K. G. Murti, K. Boyd, P. Chand, Y. S. Babu, and A. Portner, J. Virol. 82:8400-8410, 2008). Sequence analysis and superposition of the NDV and hPIV-3 HN dimer structures revealed that, similar to what was seen in hPIV-1, the N-linked glycan at residue 523 on hPIV-3 HN may cover a second receptor-binding site. Removal of this N-linked glycosylation site by an Asn-to-Asp substitution at residue 523 (N523D) changed the spectrum of the mutant virus's receptor specificity, delayed its elution from both turkey and chicken red blood cells, reduced mutant sensitivity (by about half) to the selective HN inhibitor BCX 2855 in hemagglutination inhibition tests, and slowed its growth in LLC-MK2 cells. The neuraminidase activity of the mutant and its sensitivity to BCX 2855 in neuraminidase inhibition assays did not change, indicating that the mutation did not affect the virus's catalytic-binding site and that all observed effects were caused by the exposure of the purported second receptor-binding site. Our data are consistent with the idea that, similar to the case for hPIV-1, the N-linked glycan shields a second receptor-binding site on hPIV-3 HN.
Hemagglutinin-neuraminidase (HN) is a major glycoprotein on the surface of the parainfluenza virus virion. It has two essentially opposite activities: hemagglutination (HA) defines virus binding to sialic acid (SA)-containing receptors, and neuraminidase (NA) is important for virus progeny release and prevention of virus self-aggregation (14). HN also triggers the F protein to induce membrane fusion (15, 26).
Crystallographic study of Newcastle disease virus (NDV) (an avian paramyxovirus) HN revealed that its HA and NA activities are navigated by two active sites, a catalytic binding site and a second receptor-binding site (hereinafter referred to as catalytic and second sites, respectively) (5, 27, 32). The presence of the second site on NDV HN prevents the parainfluenza virus-selective HN inhibitor BCX 2798 (designed on the basis of the three-dimensional structure of the NDV HN catalytic site [2]) from inhibiting virus HA but not NA activity (4).
Among human parainfluenza virus (hPIV) types 1 through 4 (hPIV-1 to -4), the crystal structure of the hPIV-3 HN is the only one characterized thus far (16). A crystallographic analysis of the hPIV-3 HN complexed with N-acetylneuraminic acid (Neu5Ac), its derivative 2-deoxy-2,3-dehydro-N-acetylneuraminic acid (Neu5Ac2en), or zanamivir (a drug designed on the basis of the crystal structure of the influenza virus NA) revealed the presence of the catalytic site but not a second site on the glycoprotein. However, studies with NDV show that to probe a second site, neuraminic acid analogues other than Neu5Ac, Neu5Ac2en, or zanamivir may be required (32). Recent studies of hPIV-1 with an Asn-to-Ser mutation at residue 173 of its HN (N173S) indicate that, similar to NDV, hPIV-1 has a second site on its HN (1). However, in contrast to NDV HN, the second site on hPIV-1 HN is covered by an N-linked glycan at residue 173. The N173S virus, whose second site is exposed due to the loss of an N-linked glycan, failed to be efficiently eluted from erythrocytes or released from the surface of infected cells and lost its sensitivity to BCX 2798, as shown by hemagglutination inhibition (HI) tests. The N173S virus's NA activity and its susceptibly to BCX 2798 in neuraminidase inhibition (NI) assays did not differ from those of the virus without mutation, indicating that the effects seen were not due to changes in the mutant's catalytic site but rather were due to the appearance of a second site for binding. The remoteness of residue 173 from the proposed location of the catalytic site of hPIV-1 HN was also consistent with that suggestion. The masking of the receptor-binding sites by N-linked glycans is not a unique phenomenon among paramyxoviruses. An N-linked glycan shields the second site on the measles virus H glycoprotein (9) and possibly the receptor-binding site on the Nipah virus G glycoprotein (8).
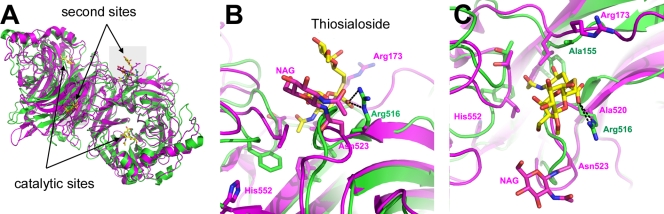
In this study, we first investigated whether hPIV-3 had a second site for binding covered by an N-linked glycan on its HN. Superposition of the HN dimer structures of NDV (32) and hPIV-3 (16) using PyMOL (6) suggested that the N-linked glycan at residue 523 may cover a second site on hPIV-3 HN (Fig. 1). Only the first carbohydrate, N-acetylglucosamine (NAG) on Asn523, was visible in the crystal structure of hPIV-3 HN, but it is easy to imagine a more complex carbohydrate interfering with access to the proposed second site (Fig. 1B). This second site appears to be present on hPIV-3 HN, because there is conservation of a hydrophobic pocket formed from residues (drawn on the figure but not labeled) Leu174, Thr186, Val187, and Phe563 (residues Phe156, Thr168, Phe553, and Leu561 in NDV HN) to accommodate the acetamido methyl group of SA. Furthermore, although the Arg516 of NDV HN that interacts with the carboxylate group of thiosialoside is not conserved in hPIV-3 HN, there is an arginine, Arg173, in hPIV-3 HN that could play the same role. Interestingly, Arg173 of hPIV-3 HN is replaced by Ala155 in NDV HN, whereas Arg516 in NDV HN is replaced by Ala520 in hPIV-3 HN (Fig. 1C). Computer modeling data also pointed out that Asn523 is remote from the catalytic site on hPIV-3 HN (Fig. 1A). Thus, structural analysis suggests the presence of a second site for binding very close to Asn523 of hPIV-3 HN. The data from structural analyses contradict the suggestion from a couple of recent publications that the His-to-Gln mutation at residue 552 (H552Q) of hPIV-3 HN at the dimer interface (Fig. 1B and C) leads to the formation of a second site (17, 19). This conclusion was based on the observation of increased receptor-binding avidity of the H552Q mutant, while its NA activity (e.g., catalytic site) was not changed. Our computer modeling data indicate that His552 is remote from the location of the hydrophobic pocket that forms a second recognition site for the acetamido methyl group of the SA receptor (Fig. 1B and C).
FIG. 1.
Superposition of the HN dimer structures of NDV (green) and hPIV-3 (magenta). (A) The relative locations of the catalytic and second sites. The area highlighted in gray is shown in panels B and C. (B) Location of the second site with thiosialoside (shown in yellow) bound in the NDV HN crystal structure. The NAG carbohydrate N-linked to Asn523 is shown; residues that form the conserved hydrophobic pocket accommodating the methyl of the SA acetamido group are drawn without labeling. (C) The same region as in panel B, rotated 90° around a horizontal axis. The hydrogen bonds made between Arg516 and the carboxylate group of SA in NDV HN are shown as black dotted lines.
Because the hPIV-3 reverse genetic system is not commercially available, to find a second site on hPIV-3 HN, we used the Sendai virus (SeV) reverse genetic system (11) and rescued a recombinant SeV (E strain) in which fragments of the HN and F genes were replaced by those from hPIV-3 (C243 strain) [rSeV(hPIV-3FHN)], as described previously (30). The HN gene in rSeV(hPIV-3FHN) contained the ectodomain and transmembrane domain and half of the cytoplasmic tail from hPIV-3. The other half of the cytoplasmic tail was retained from SeV because it was required for the HN protein to incorporate into the virion through interaction with the SeV matrix protein (22, 24, 25). The F ectodomain of rSeV(hPIV-3FHN) was replaced by that of hPIV-3 to maintain a type-specific interaction with HN (from hPIV-3), which is required for efficient membrane fusion (7, 15, 31). The rescued rSeV(hPIV-3FHN) virus (hereinafter referred to as the parent virus) was plaque purified and amplified on LLC-MK2 cells. The HN gene was further mutated at Asn523 to Asp or at His552 to Gln to create the N523D and H552Q mutant viruses, respectively. To confirm the insertion of the mutations, viral RNAs were extracted from the infected cell supernatants; cDNA synthesis and PCR amplification were done using the One-Step reverse transcription (RT)-PCR system (Qiagen, Valencia, CA). Sequences of the F gene of all viruses and the HN gene of the parent virus did not reveal any mutations; sequences of the HN gene of N523D and H552Q viruses confirmed the desired substitutions.
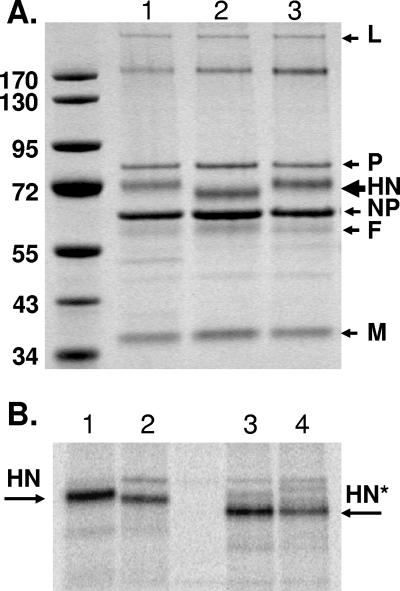
First, we characterized the mobilities of the virus proteins in sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) under reducing conditions (Fig. 2). Analysis showed identical migration patterns of all proteins for the parent (lane 1) and H552Q virus (lane 3). The patterns were identical in the N523D virus except for HN (lane 2) (Fig. 2A). HN of the N523D virus had greater electrophoretic mobility, corresponding to a molecular mass of approximately 5,000 Da less (as determined by the Totallab TL100 1D software program, version 2008.01; Nonlinear USA Inc., Durham, NC) than the total mass of the HN of the parent virus (71,000 Da). After treatment with the peptide N-glycosidase F (PNGase F), HNs of the parent (lane 3) and the N523D mutant (lane 4) viruses migrated to identical positions (Fig. 2B). This confirmed that the altered mobility of HN of the N523D mutant was not due to the mutation at residue 523 by itself but was due to the loss of the N-linked glycan.
FIG. 2.
SDS-PAGE analysis of the purified parent and mutant viruses' proteins. (A) Viruses were grown in LLC-MK2 cells, concentrated, and purified through a 35% sucrose cushion. Two micrograms of purified parent (lane 1), N523D (lane 2), or H552Q (lane 3) virus was loaded on a 10% Bis-Tris gel. Gel was stained with Page Blue protein stain (Fermentas, Inc., Glen Burnie, MD) to visualize proteins. (B) LLC-MK2 cell monolayers were infected with viruses. At 20 h after infection, the cells were metabolically radiolabeled with [35S]methionine-cysteine (500 μCi per 107 cells) (Perkin-Elmer, Boston, MA). Cells were then lysed and subjected to immunoprecipitation with anti-hPIV-3 HN monoclonal antibody. Half of the immunoprecipitate was treated with PNGase F (New England Biolabs, Beverly, MA) to remove N-glycosylated moieties. The untreated HNs of the parent (lane 1) or N523D (lane 2) and PNGase F-treated HNs (indicated by asterisks) of the parent (lane 3) or N523D (lane 4) are shown. Molecular mass standards (in kilodaltons) are shown to the left of the gel.
Analysis of HN and F incorporation into the mutant viruses showed that the proportion of each glycoprotein to the M protein (an internal viral protein whose incorporation into the viral particle should not be affected by HN mutation) in the N523D virus were similar to those of the parent virus (Table 1). In contrast, significantly more HN and less F incorporation than in the parent were observed in the H552Q virus (P < 0.02), indicating that H552Q mutation changes the properties of the virions. The proportion of NP/M did not differ among all three viruses.
TABLE 1.
Incorporation of HN, F, and NP into the parent and mutant virusesa
| Protein proportion analyzed | Value for virusb |
||
|---|---|---|---|
| Parent | N523D virus | H552Q virus | |
| HN/M | 1.12 ± 0.12 | 1.14 ± 0.21 | 1.27 ± 0.09* |
| F/M | 0.55 ± 0.11 | 0.63 ± 0.16 | 0.43 ± 0.05* |
| NP/M | 1.49 ± 0.09 | 1.51 ± 0.25 | 1.52 ± 0.08 |
Protein contents of concentrated viruses were analyzed in 10% Bis-Tris SDS-PAGE (Invitrogen). Proteins in a gel were localized by staining with Page Blue protein staining solution (Fermentas, Inc., Glen Burnie, MD). The images were analyzed using Totallab TL100 1D (v. 2008.01; Nonlinear USA Inc., Durham, NC). The results are the means of results from nine different virus preparations ± SD. *, P < 0.02 compared with results for the parent virus by Student's t test.
Determined by division of HN, F, or NP band's intensity by that of the M band.
To determine how the N523D and H552Q substitutions influence the mutants' binding properties, we performed hemagglutination assays using chicken and turkey red blood cells (ChRBC and TrRBC, respectively) with a prevalence of α2,3Gal or α2,6Gal SA receptors, correspondingly (10, 28). An earlier study showed that hPIV-3 has stronger affinity to SAα2,6 receptors (23); thus, it preferentially binds to TrRBC. The hemagglutination assays were performed with sucrose gradient-purified and concentrated viruses (29) at pHs 5.4 and 7.0, as described previously (1, 2) (Table 2). pH 7.0 was used because HN binds to the SA receptors at that neutral pH level during parainfluenza virus attachment. During virus replication, interaction of HN with SA receptors occurs in the Golgi compartments and secretory granules (12, 13), where the pH level is acidic (18); thus, pH 5.4 was used to characterize this interaction. As a control for the parent virus, wild-type hPIV-3 was used in our experiments. There were no differences found between these two viruses in the binding and the elution assays, indicating that modifications introduced into the cytoplasmic domain of the parent virus did not influence its binding properties. The hemagglutination tests showed that all viruses agglutinate TrRBC at both pH levels. In addition to TrRBC, both mutant viruses acquired the ability to agglutinate ChRBC at either pH level. However, the level of hemagglutination unit (HAU) titers with ChRBC was lower for the H552Q virus than for the N523D virus. The H552Q virus completely eluted from ChRBC at 4°C in less than 2 h and at 33°C in less than 1 h at either pH. The N523D virus did not elute from ChRBC for a minimum of 12 h of incubation at 4°C at either pH and for a minimum of 1 h of incubation at 33°C at either pH. Because the level of parainfluenza virus NA activity is minimal at 4°C (3, 20), our data suggest that the affinity of H552Q virus to α2,3Gal cell receptors is much lower than that of N523D virus. All tested viruses eluted from TrRBC within 1 h of incubation at 33°C at pH 5.4; at pH 7.0, only the parent virus showed the ability to elute, while both mutants remained attached to the TrRBC. The data from binding and elution assays indicated stronger binding of the N523D and H552Q viruses than of the parent virus to both ChRBC and TrRBC, resulting in delayed elution from erythrocytes.
TABLE 2.
Binding to and elution from RBCs by parent and mutant virusesa
| pH | Virus name or description | RBC type | HAU titer |
||
|---|---|---|---|---|---|
| Binding at 4°C, 1 h | Elution at 4°C, 2 to 12 h | Elution at 33°C, 1 h | |||
| 5.4 | hPIV-3 | Tr | 256 | 256 | <1 |
| Ch | <1 | <1 | <1 | ||
| Parent | Tr | 256 | 256 | <1 | |
| Ch | <1 | <1 | <1 | ||
| N523D | Tr | 256 | 256 | <1 | |
| Ch | 32 | 32 | 32 | ||
| H552Q | Tr | 512 | 512 | <1 | |
| Ch | 8 | <1 | <1 | ||
| 7.0 | hPIV-3 | Tr | 256 | 256 | <1 |
| Ch | <1 | <1 | <1 | ||
| Parent | Tr | 256 | 256 | <1 | |
| Ch | <1 | <1 | <1 | ||
| N523D | Tr | 256 | 256 | 128 | |
| Ch | 32 | 32 | 8 | ||
| H552Q | Tr | 256 | 256 | 256 | |
| Ch | 16 | <1 | <1 | ||
Viruses were initially standardized with 0.5% TrRBC in a 96-well plate to provide 256 HAU at pH 7.0 after incubation for 1 h at 4°C. Then, hemagglutination assays with 0.5% ChRBC or TrRBC were performed at pH 5.4 or 7.0. Elution of viruses from RBCs was recorded after incubation for 2 to 12 h at 4°C or for 1 h at 33°C.
The changes in the N523D and H552Q virus receptor specificities toward an α2,3 type of sialylation are reflected in their ability to grow at high titers in embryonated chicken eggs. Ten-day-old embryonated chicken eggs were inoculated with viruses at a dose of 105 PFU per egg. Three days after inoculation, the virus titer in the allantoic fluid was determined by indirect immunofluorescence assay. LLC-MK2 cells in 96-well plates were infected with virus dilutions in Dulbecco's modified Eagle's medium (DMEM) containing 0.3% bovine serum albumin (BSA) and 1 μg/ml acetylated trypsin and incubated at 33°C for 24 h in 5% CO2. Then, the cells were washed with phosphate-buffered saline (PBS), fixed with ice-cold methanol-acetic acid (95/5 [vol/vol]), and stained with an anti-SeV nucleoprotein (NP) murine IgG monoclonal antibody, followed by incubation with a fluoresce in isothiocyanate (FITC)-conjugated secondary antibody (Sigma-Aldrich, Inc., St. Louis, MO). Counts of an individual focus-forming unit (FFU) formed by cells expressing NP antigen under a fluorescence microscope (Nikon Eclipse TE 300; Nikon Inc., Japan) showed that the parent virus replicates in eggs at titers of about 104 to 106 FFU/ml, whereas infection of eggs with both N523D and H552Q virus provided 107 to 108 FFU/ml.
To further characterize the mutants' binding properties, we determined their sensitivities to the selective parainfluenza virus HN inhibitor BCX 2855 (shown to be highly effective in blocking hPIV-3 HA and NA activities [2, 30]) in HI assays with TrRBC as described previously (2). The concentration of the compound that showed 50% agglutination was considered the 50% inhibitory concentration (IC50). Our data from at least three independent HI assays showed that the N523D and H552Q viruses were moderately less sensitive (about 50% less) to BCX 2855 than were the parent virus and wild-type hPIV-3. The IC50 volumes were 6.2 ± 0.0 μM (standard deviation [SD]) for both mutants, 2.6 ± 0.8 μM (SD) for the parent virus, and 2.3 μM ± 0.5 (SD) for wild-type hPIV-3. The data from all binding and elution assays, growth in embryonated chicken eggs, and HI assays indicated acceleration of the mutant viruses' binding.
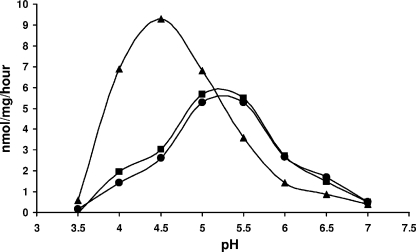
To exclude the possibility that increased binding of the mutants is a result of the changes in their catalytic sites, we analyzed the enzymatic activities of the concentrated purified viruses with a standard fluorometric assay using 2′-(4-methylumbelliferyl)-α-d-N-acetylneuraminic acid (MUNANA) (Sigma-Aldrich, Inc., St. Louis, MO) as the substrate (21), with some modifications described previously (1) (Table 3 and Fig. 3). To determine whether the modifications in the cytoplasmic domain of the parent virus influenced properties of its NA, wild-type HPIV-3 was included as a control. Similar to the results obtained in the binding-elution assays, there were no differences found between the parent and wild-type HPIV-3 in experiments characterizing their NA activity (Table 3). Comparison of the optimum pH levels for the viruses' NA activities showed that pH 5.4 was the optimum for the parent and the N523D virus and pH 4.4 was the optimum for the H552Q virus (Fig. 3). Next, we conducted enzyme kinetic assays at pHs 4.5, 5.4, and 7.0 to determine the maximum velocity (Vmax) (an approximation for NA activity in relation to the amount of HN) and the Michaelis constant (Km) (an approximation of the substrate concentration required for significant catalysis to occur). These assays confirmed the shift in the optimum pH for H552Q virus, which showed the highest level of NA activity (as reflected by the Vmax) at pH 4.5 (Table 3). The highest level of enzymatic activity for the parent and N523D viruses was observed at pH 5.4. Analysis of the Vmax and Km parameters at pHs 5.4 and 7.0 (used in binding and elution assays) showed no significant difference between the parent and the N523D virus in terms of NA activity or the affinity of the catalytic site to the substrate (as reflected by Km), indicating that the substitution at residue 523 does not affect the mutant virus catalytic site. Comparison of the Vmax and Km parameters at both pH levels for parent and H552Q virus showed significant reductions in the case of the H552Q virus (P < 0.01), indicating that substitution at residue 552 does affect the mutant's catalytic site by reducing enzymatic activity and increasing its affinity to the substrate. The changes in the H552Q catalytic site did not significantly influence its sensitivity to BCX 2855 in the NI assays. Thus, the IC50s (the concentrations of the compound required to reduce the NA activity to 50% of that of untreated virus) were similar (about 6.2 μM) for the wild-type hPIV-3, the parent, and both mutants (data not shown). Our characterization of H552Q virus NA activity contradicts the suggestion that a histidine-to-glutamine substitution at residue 552 of hPIV-3 HN does not change the mutant's NA activity (e.g., catalytic site) (19). His552 is only three residues from Glu549, a residue conserved in all NAs (human, viral, and bacterial) that interacts with one of the three arginines in the catalytic site. It may be that the H552Q mutation can transmit structural changes to the catalytic site, thus affecting its NA activity. Our data from the optimum pH analysis and enzyme kinetic assays logically explain an increase in H552Q virus receptor specificity, increased binding to erythrocytes, and delayed elution. Increases in receptor specificity and the binding of H552Q virus to ChRBC can result from increases in both incorporation of HN into the mutant particle (Table 1) and substrate affinity (e.g., affinity to the receptors) (Table 3). The inability of H552Q virus to elute from TrRBC at pH 7.0 at 33°C can result from the reduction of mutant NA activity. Thus, our findings suggest that the mutation H552Q does not create a second site on the HN molecule of hPIV-3. Our data also suggest, for the N523D virus, that the increased spectrum of receptor specificity (toward ChRBC; e.g., α2,3 sialylation) and the inability to elute from ChRBC at both pH levels and from TrRBC at pH 7.0 at 33°C can be due only to the appearance of a second site on its HN as a result of the loss of the N-linked glycan at residue 523. The ability of the N523D virus to agglutinate ChRBC indicates that the second site has an affinity for SAα2,3 receptors. Taken together, our findings support the suggestions that the location of a second site on hPIV-3 HN correlates with that proposed by superposition of the NDV and hPIV-3 HN dimer structures and that the N-linked glycan at residue 523 masks a second site of hPIV-3 HN (similar to that proposed for hPIV-1).
TABLE 3.
NA activities of parent and mutant virusesa
| Virus name or description | Result at pH: |
|||||
|---|---|---|---|---|---|---|
| 4.5 |
5.4 |
7.0 |
||||
| Mean Vmax ± SD (nmol/μg/min) | Mean Km ± SD (mM) | Mean Vmax ± SD (nmol/μg/min) | Mean Km ± SD (mM) | Mean Vmax ± SD (nmol/μg/min) | Mean Km ± SD (mM) | |
| hPIV-3 | 4.1 ± 0.1 | 0.6 ± 0.1 | 9.2 ± 0.4 | 14.5 ± 0.3 | 0.9 ± 0.1 | 16.9 ± 0.8 |
| Parent | 3.8 ± 0.4 | 0.6 ± 0.1 | 9.0 ± 0.2 | 14.1 ± 0.8 | 1.1 ± 0.2 | 17.7 ± 0.9 |
| N523D | 3.0 ± 0.2 | 0.6 ± 0.1 | 9.1 ± 0.5 | 15.0 ± 0.4 | 0.8 ± 0.1 | 13.7 ± 1.0 |
| H552Q | 14.7 ± 0.4* | 0.9 ± 0.1* | 4.8 ± 0.3* | 11.1 ± 0.8* | 0.3 ± 0.1* | 7.5 ± 0.8* |
Enzyme kinetic assays were conducted in the range of 0.08-20 mM substrate (MUNANA) in citrate-phosphate buffer (McIlvaine's buffer system), 4 mM CaCl2 at 33°C on Spectra Max M5 microplate reader (Molecular Devices, Sunnyvale, CA). Plates were scanned each 2 min for 20 times. Results are mean values from at least three independent experiments. *, P < 0.01 compared with results for the parent virus by Student's t test.
FIG. 3.
Neuraminidase activities of the parent and mutant viruses at different pH levels. Purified concentrated parent (•), N523D (▪) mutant, and H552Q (▴) mutant viruses were analyzed for optimum pH for NA activity by using a modified fluorometric assay (1) with 200 μM MUNANA in citrate-phosphate buffer (McIlvaine's buffer system) at a pH range of 3.0 to 8.0. One microgram of total viral proteins was used for the reaction. HN protein loading was determined by parallel SDS-PAGE analysis of viral proteins. Specific signal is expressed as nanomoles of product formed per milligram of HN after 1 h of incubation at 37°C.
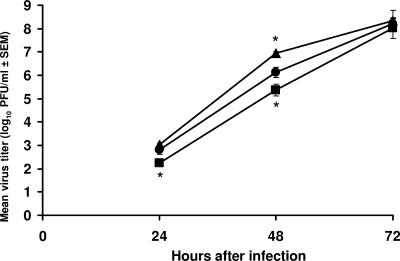
Previously we found that the N173S virus, which has an exposed second site on hPIV-1 HN due to the loss of an N-linked glycan at residue 173, failed to replicate at high titers in infected cells during the first 48 h because of its inability to effectively release from the surface of the cells due to unbalanced binding and NA activities (1). Similarly, the growth of N523D virus in cells infected with a multiplicity of infection (MOI) of 0.0001 was from approximately 4- to 6-fold lower than that of the parent virus 24 and 48 h after infection (P < 0.05), in contrast to the H552Q virus, in which growth was significantly accelerated after 48 h (P < 0.05) (Fig. 4). The titers for all tested viruses did not differ 72 h after infection. Similar dynamics of viruses' growth were observed for an MOI in the range of 0.001 to 1 (data not shown). The results from growth curve assays were in agreement with the proposition that delayed growth of N523D virus results from the exposure of the second site on its HN and, as a consequence, its inability to efficiently release from the surface of infected cells, whereas the accelerated growth of H552Q virus results from the changes in the virus's catalytic site. Elevated NA activity of H552Q virus at a low pH level can more effectively (faster and to a greater extent than in the virus without a mutation) destroy SA residues in the secretory compartments. The newly assembled mutant virions would be more easily released from the cell surface than those of the parent, thus explaining high titers of H552Q virus 48 h after infection.
FIG. 4.
Growth kinetics of the parent and mutant viruses. LLC-MK2 cells in 24-well plates were infected with the parent (•), N523D (▪), and H552Q (▴) viruses at an MOI of 0.0001. After 1 h of incubation at room temperature, the cells were washed with PBS and DMEM supplemented with 0.3% BSA, and 1 μg/ml acetylated trypsin was added to the wells. Virus titers were determined for culture supernatant fluids by plaque assays at the times indicated on the x axis. Values presented are the means of results from at least three independent experiments, plotted with error bars indicating the standard errors of the means (SEM). *, P < 0.05 compared with results for the parent virus by Student's t test.
To determine whether hPIV-3 mutants with an exposed second site (N523D) are circulating in nature, we sequenced viruses in 30 nasal wash samples obtained from Le Bonheur Children's Medical Center, Memphis, TN, from children hospitalized due to respiratory complications from hPIV-3 infection. Total RNA was extracted from 250 μl of nasal wash and used for HN gene amplification using the OneStep RT-PCR Kit. The DNA fragments were subcloned into the pCR vector by using a TA cloning kit (Invitrogen, Carlsbad, CA). At least 10 clones per sample were selected, and the plasmid DNA was sequenced. We found hPIV-3 mutants exhibiting the loss of the N-linked glycan at residue 523 in 1 to 3 clones in 4 human samples. Clones from 3 samples had the asparagine-to-glutamine mutation, and a clone from 1 sample had an asparagine-to-serine mutation. This clearly shows circulation of the hPIV-3 mutants with unmasked second sites in nature. However, additional analyses are needed to determine the clinical significance of these viruses.
Additional studies are also needed to establish the role of the second site in the interaction with the catalytic site, involvement in the binding process, and influence on the F protein. The findings from these proposed studies may significantly improve our knowledge of hPIV-3 biology.
Acknowledgments
This work was supported in part by grant PO1 A1054955 from the National Institute of Allergy and Infectious Diseases and by the American Lebanese Syrian Associated Charities (ALSAC).
We thank BioCryst Pharmaceuticals, Inc. (Birmingham, AL), for providing BCX 2855; Pamela Freiden and Dmitri Falkner for technical assistance; and David Galloway, ELS, for editorial comments regarding the manuscript.
Footnotes
Published ahead of print on 6 January 2010.
REFERENCES
- 1.Alymova, I. V., G. Taylor, V. P. Mishin, M. Watanabe, K. G. Murti, K. Boyd, P. Chand, Y. S. Babu, and A. Portner. 2008. Loss of the N-linked glycan at residue 173 on human parainfluenza virus type 1 hemagglutinin-neuraminidase exposes a second receptor-binding site. J. Virol. 82:8400-8410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alymova, I. V., G. Taylor, T. Takimoto, T. H. Lin, P. Chand, Y. S. Babu, C. Li, X. Xiong, and A. Portner. 2004. Efficacy of novel hemagglutinin-neuraminidase inhibitors BCX 2798 and BCX 2855 against human parainfluenza viruses in vitro and in vivo. Antimicrob. Agents Chemother. 48:1495-1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amonsen, M., D. F. Smith, R. D. Cummings, and G. M. Air. 2007. Human parainfluenza viruses hPIV1 and hPIV3 bind oligosaccharides with alpha2-3-linked sialic acids that are distinct from those bound by H5 avian influenza virus hemagglutinin. J. Virol. 81:8341-8345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bousse, T. L., G. Taylor, S. Krishnamurthy, A. Portner, S. K. Samal, and T. Takimoto. 2004. Biological significance of the second receptor binding site of Newcastle disease virus hemagglutinin-neuraminidase protein. J. Virol. 78:13351-13355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crennell, S., T. Takimoto, A. Portner, and G. Taylor. 2000. Crystal structure of the multifunctional paramyxovirus hemagglutinin-neuraminidase. Nat. Struct. Biol. 7:1068-1074. [DOI] [PubMed] [Google Scholar]
- 6.DeLano, W. 2002. The PyMOL molecular graphics system. DeLano Scientific, Palo Alto, CA.
- 7.Deng, R. T., Z. Y. Wang, A. M. Mirza, and R. M. Iorio. 1995. Localization of a domain on the paramyxovirus attachment protein required for the promotion of cellular fusion by its homologous fusion protein spike. Virology 209:457-469. [DOI] [PubMed] [Google Scholar]
- 8.Guillaume, V., H. Aslan, M. Guerbois, T. F. Wild, R. Buckland, and J. P. Langedijk. 2006. Evidence of a potential receptor-binding site on the Nipah virus G protein (NiV-G): identification of globular head residues with a role in fusion promotion and their localization on an NiV-G structural model. J. Virol. 80:7546-7554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hashiguchi, T., M. Kajikawa, N. Maita, M. Takeda, K. Kuroki, K. Sasaki, D. Kohda, Y. Yanagi, and K. Maenaka. 2007. Crystal structure of measles virus hemagglutinin provides insight into effective vaccines. Proc. Natl. Acad. Sci. U. S. A. 104:19535-19540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ito, T., Y. Suzuki, L. Mitnaul, A. Vines, H. Kida, and Y. Kawaoka. 1997. Receptor specificity of influenza A viruses correlates with the agglutination of erythrocytes from different animal species. Virology 227:493-499. [DOI] [PubMed] [Google Scholar]
- 11.Kato, A., Y. Sakai, T. Shioda, T. Kondo, M. Nakanishi, and Y. Nagai. 1996. Initiation of Sendai virus multiplication from transfected cDNA or RNA with negative or positive sense. Genes Cells 1:569-579. [DOI] [PubMed] [Google Scholar]
- 12.Klenk, H. D., L. A. Caliguiri, and P. W. Choppin. 1970. The proteins of the parainfluenza virus SV5. II. The carbohydrate content and glycoproteins of the virion. Virology 42:473-481. [DOI] [PubMed] [Google Scholar]
- 13.Klenk, H. D., and P. W. Choppin. 1970. Glycosphingolipids of plasma membranes of cultured cells and an enveloped virus (SV5) grown in these cells. Proc. Natl. Acad. Sci. U. S. A. 66:57-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lamb, R. A., and G. D. Parks. 2007. Paramyxoviridae: the viruses and their replication, p. 1449-1496. In D. M. Knipe and P. M. Howley (ed.), Fields virology. Lippincott Williams & Wilkins, Philadelphia, PA.
- 15.Lamb, R. A., R. G. Paterson, and T. S. Jardetzky. 2006. Paramyxovirus membrane fusion: lessons from the F and HN atomic structures. Virology 344:30-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lawrence, M. C., N. A. Borg, V. A. Streltsov, P. A. Pilling, V. C. Epa, J. N. Varghese, J. L. McKimm-Breschkin, and P. M. Colman. 2004. Structure of the haemagglutinin-neuraminidase from human parainfluenza virus type III. J. Mol. Biol. 335:1343-1357. [DOI] [PubMed] [Google Scholar]
- 17.Palermo, L. M., M. Porotto, C. C. Yokoyama, S. G. Palmer, B. A. Mungall, O. Greengard, S. Niewiesk, and A. Moscona. 2009. Human parainfluenza virus infection of the airway epithelium: viral hemagglutinin-neuraminidase regulates fusion protein activation and modulates infectivity. J. Virol. 83:6900-6908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paroutis, P., N. Touret, and S. Grinstein. 2004. The pH of the secretory pathway: measurement, determinants, and regulation. Physiology 19:207-215. [DOI] [PubMed] [Google Scholar]
- 19.Porotto, M., M. Fornabaio, G. E. Kellogg, and A. Moscona. 2007. A second receptor binding site on human parainfluenza virus type 3 hemagglutinin-neuraminidase contributes to activation of the fusion mechanism. J. Virol. 81:3216-3228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Porotto, M., M. Murrell, O. Greengard, L. Doctor, and A. Moscona. 2005. Influence of the human parainfluenza virus 3 attachment protein's neuraminidase activity on its capacity to activate the fusion protein. J. Virol. 79:2383-2392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Potier, M., L. Mameli, M. Belishem, L. Dallaire, and S. B. Melancon. 1979. Fluorometric assay of neuraminidase with a sodium (4-methylumbelliferyl-alpha-D-N-acetylneuraminate) substrate. Anal. Biochem. 94:287-296. [DOI] [PubMed] [Google Scholar]
- 22.Sanderson, C. M., H. H. Wu, and D. P. Nayak. 1994. Sendai virus M protein binds independently to either the F or the HN glycoprotein in vivo. J. Virol. 68:69-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Suzuki, T., A. Portner, R. A. Scroggs, M. Uchikawa, N. Koyama, K. Matsuo, Y. Suzuki, and T. Takimoto. 2001. Receptor specificities of human respiroviruses. J. Virol. 75:4604-4613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Takimoto, T., T. Bousse, E. C. Coronel, R. A. Scroggs, and A. Portner. 1998. Cytoplasmic domain of Sendai virus HN protein contains a specific sequence required for its incorporation into virions. J. Virol. 72:9747-9754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Takimoto, T., K. G. Murti, T. Bousse, R. A. Scroggs, and A. Portner. 2001. Role of matrix and fusion proteins in budding of Sendai virus. J. Virol. 75:11384-11391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Takimoto, T., G. L. Taylor, H. C. Connaris, S. J. Crennell, and A. Portner. 2002. Role of the hemagglutinin-neuraminidase protein in the mechanism of paramyxovirus-cell membrane fusion. J. Virol. 76:13028-13033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Takimoto, T., G. L. Taylor, S. J. Crennell, R. A. Scroggs, and A. Portner. 2000. Crystallization of Newcastle disease virus hemagglutinin-neuraminidase glycoprotein. Virology 270:208-214. [DOI] [PubMed] [Google Scholar]
- 28.Thompson, C. I., W. S. Barclay, and M. C. Zambon. 2004. Changes in in vitro susceptibility of influenza A H3N2 to a neuraminidase inhibitor drug during evolution in the human host. J. Antimicrob. Chemother. 53:759-765. [DOI] [PubMed] [Google Scholar]
- 29.Thompson, S. D., W. G. Laver, K. G. Murti, and A. Portner. 1988. Isolation of a biologically active soluble form of the hemagglutinin-neuraminidase protein of Sendai virus. J. Virol. 62:4653-4660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Watanabe, M., V. P. Mishin, S. A. Brown, C. J. Russell, K. Boyd, Y. S. Babu, G. Taylor, X. Xiong, X. Yan, A. Portner, and I. V. Alymova. 2009. Effect of hemagglutinin-neuraminidase inhibitors BCX 2798 and BCX 2855 on growth and pathogenicity of Sendai/human parainfluenza type 3 chimera virus in mice. Antimicrob. Agents Chemother. 53:3942-3951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yao, Q. Z., X. L. Hu, and R. W. Compans. 1997. Association of the parainfluenza virus fusion and hemagglutinin-neuraminidase glycoproteins on cell surfaces. J. Virol. 71:650-656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zaitsev, V., M. von Itzstein, D. Groves, M. Kiefel, T. Takimoto, A. Portner, and G. Taylor. 2004. Second sialic acid binding site in Newcastle disease virus hemagglutinin-neuraminidase: implications for fusion. J. Virol. 78:3733-3741. [DOI] [PMC free article] [PubMed] [Google Scholar]