Summary
To test the efficacy of a sustainable community-level HIV intervention among sex workers, the Sonagachi Project was replicated, including community organizing and advocacy, peer education, condom social marketing, and establishment of a health clinic. Sex workers were randomly selected in 2 small urban communities in northeastern India (n = 100 each) and assessed every 5–6 months over 15 months (85% retention). Overall condom use increased significantly in the intervention community (39%) compared with the control community (11%), and the proportion of consistent condom users increased 25% in the intervention community compared with a 16% decrease in the control community. This study supports the efficacy of the Sonagachi model intervention in increasing condom use and maintaining low HIV prevalence among sex workers.
Keywords: condom use, condoms, HIV, HIV in India, sex workers, Sonagachi Project
In India, HIV seroprevalence rates among sex workers have ranged from 50–90% in Bombay, Delhi, and Chennai.1-4 However, HIV rates of only 10% have been observed among sex workers in Calcutta, a city on the drug route into the heart of India and one of the most impoverished urban areas in the world.5 Condom use has risen in Calcutta in recent years, from 3% in 1992 to 90% in 1999, compared with steady rates of low condom use among sex workers in other cities in India.4
The surprisingly low rate of HIV infection and high rate of condom use among sex workers in Calcutta may reflect the impact of the Sonagachi Project, a sustainable communitylevel sexually transmitted disease (STD)/HIV intervention program. The components of the intervention model include defining HIV and STDs as occupational health hazards; articulating the human rights of sex workers; providing access to condoms and resources for treating STDs; and creating a sense of community and political awareness. The multipronged program has resulted in economic, political, and occupational power for sex workers in Calcutta. In October 2001, >60,000 sex workers from throughout India convened in Calcutta, with aims to reduce the stigma of sex work by advocating change in societal attitudes toward sexuality and sex work. Stigma related to HIV risk, including the compounded stigma connected with groups and behaviors associated with heightened risk for HIV infection, has earned increased recognition as a key factor hindering HIV identification, prevention, and treatment efforts.6-11
Pathways into sex work in India are 3-fold. First, many women are born into sex work as the family profession. The stigma associated with sex work, often coupled with residual caste system discrimination, severely limits educational and alternative economic opportunities. Second, many young women from rural areas and neighboring countries (e.g., Nepal, Bangladesh) are deceived, sold, or otherwise trafficked into sex work against their will. Driven by the extreme poverty facing their families and the lure of relatively large incomes, some women choose to return to sex work, albeit in a less coercive context, once they are returned to their homes. Sex workers in Calcutta are conservatively estimated to earn an hourly wage almost twice that of women in urban India.12 Finally, some women, given limited options, choose sex work as a means to support their families after being widowed, divorced, or abandoned by their husbands. About 9% of a random sample of sex workers in the Sonagachi “red light” area stated that they entered the profession voluntarily.12 While some sex workers are street-based, the majority work, and often live, in brothels clustered in red light areas of big cities and small towns.
Effective HIV prevention programs among sex workers have been implemented in Brazil,13 Thailand,14 and Zaire.15 Community participation among sex workers in HIV prevention, however, is not guaranteed, as in the demise of a community-based HIV prevention program among sex workers in southern India.16
The World Health Organization has selected the Sonagachi Project as a “model” for STD/HIV intervention.17 While the low HIV rates in Calcutta are impressive, there is little evidence under controlled conditions that Sonagachi is responsible for the results. Although several studies have examined the Sonagachi Project or the sex workers participating in the project,12,18-24 none has been published that demonstrates the efficacy of the Sonagachi model. Accordingly, the staff from the Sonagachi Project designed and conducted a 2-community trial to document the efficacy of the program, and an external research team designed the assessment and conducted the analysis.
METHODS
Research Team Roles
There were 2 teams from the Sonagachi Project: an assessment team and an intervention team. The assessment team was comprised of staff that conducted the project’s ongoing rapid assessment and evaluation activities, and the intervention team included sex worker peer educators and community organizers, as well as professional project staff involved in advocacy work. A team from the University of California, Los Angeles (UCLA), consulted on the design of assessment measures, data analysis, and assurance of fidelity in implementation of assessment and intervention.
Sites
Two communities in the Cooch Behar district of West Bengal in northeastern India (Cooch Behar and Dinhata) were matched on size, socioeconomic status, and number of sex workers. Communities were randomly assigned to an interven tion and control condition. These communities represented 2 of the 7 urban centers in the district and were separated by a distance that limited cross-site contamination (i.e., most transportation by foot or bicycle). Each community had a red light area that consisted of a neighborhood, about 100 m2 in size, where brothel-based sex workers lived and worked.
Participant Recruitment
The Sonagachi Project sent an assessment team of peer outreach workers and trained research staff to conduct rapid assessments of the red light areas, identifying the population of sex workers in each community. Each community consisted of about 350 sex workers. One hundred sex workers were randomly selected in each area (n = 200), using a 2-stage randomization process. First, the brothel rooms in each red-light area were enumerated (e.g., building, room) and randomly selected using a random number table. Second, the sex workers living in those rooms were enumerated and randomly selected using a random number table. Ten sex workers in each area were oversampled at baseline to account for refusal and loss at the first follow-up. One hundred sex workers in each area were recruited with informed consent and participated in the longitudinal study.
The Institutional Review Boards of UCLA, the Durbar Mahila Samanwaya Committee (sex worker community organization), and the local community groups in Cooch Behar and Dinhata reviewed and approved the protocol. Participants provided voluntary informed consent that was written in simplified terms in the local dialect or delivered verbatim if the participant was illiterate.
Standardizing Resources in Each Community
Health clinics were established in the center of both communities’ red light areas to improve existing care for sex workers in both communities. Health care services, focused on reproductive and sexual health, were free to sex workers and their families but were also available to other members of the community in need. If they gave consent, clinic attendees were tested for syphilis using the Venereal Disease Reference Laboratory (VDRL) test. The clinics were open 2 days a week in each community and operated by a medical doctor specializing in STD/HIV, a female nurse, a male clinic administrator, and 2 female peer health educators. The Sonagachi team trained all personnel, especially in terms of cultural sensitivity for HIV, STDs, and sexual health issues for sex workers.
Enhanced Intervention
In addition to the health clinic and basic STD information, the enhanced intervention group included trainings by a team of local peer educators. Goals were to build skills and confidence in providing education and to foster empowerment and advocacy for local sex workers. The team engaged in ongoing advocacy activities with local stakeholders (e.g., “madams” and brothel owners) and power brokers (e.g., police, mafia, local politicians) who exerted control over the sex workers’ lives, with the goal of building toward increased dignity, autonomy, and self-determination among the sex workers.
Initially, outreach workers were selected among the local sex worker community by the Sonagachi Project intervention team. Charismatic sex workers living and working within the red light area were identified as leaders and trained to perform 2 primary roles involving diffusion processes of the Sonagachi model: empowerment and advocacy. Peer educators “apprenticed” under the Sonagachi trainers and eventually took over their empowerment training and advocacy activities. Empowerment activities included sustained engagement with local sex workers; showing an interest in sex workers’ health and well-being and that of their children; nurturing group solidarity among sex workers; and raising consciousness about sex worker rights. The Sonagachi sex worker/trainers conducted sustained and ongoing training in Sonagachi empowerment methods and messages (e.g., “Sex work is valid work,” “Sex workers deserve to protect themselves”). Additionally, highstatus advocates (i.e., the medical doctor, evaluation team, and Sonagachi representatives) conducted active and ongoing advocacy work with local police, elected officials, appointed policy makers, shop owners, civic and social clubs, and other gatekeepers in the sex worker community (e.g., madams, pimps, local gangs) to effect changes in the structural barriers to condom use by sex workers.
Assessment Procedures
The Sonagachi evaluation team administered the questionnaires in both communities. A baseline assessment was conducted with 3 follow-up assessments at 5- to 6-month intervals over 16 months. Follow-up rates were similar in the intervention and the control communities at each wave from the baseline interviews (n = 100 each condition): Wave 1, 90% intervention, 93% control; wave 2, 85% intervention, 88% control; wave 3, 92% intervention, 80% control. In the intervention community, 84% were interviewed at every follow-up time point; 75% were assessed at every follow-up assessment in the control community.
Assessment Measures
The following domains were assessed at each time point: age, income, time in the profession of sex work, marital status, working arrangements, substance use, condom availability, sex partner information, sexual behavior, STD information, STD knowledge, and HIV/AIDS knowledge. Primary outcome measures included condom utilization and changes in condom use.
Condom Utilization
Condom utilization was defined by the number of condoms used over the number of sexual intercourse acts reported by sex workers for the last day worked. If a condom was used during every act, such individuals were classified as having 100% condom use. Any condom use was defined as having used a condom at least once during a sexual act.
Changes in Condom Use
Change in condom use was examined by defining sex workers as adopters or relapsers. Adopters were those who converted from <100% condom use at baseline to 100% condom use at follow-up. Relapsers were those who switched from 100% condom use at baseline to <100% condom use at follow-up.
Data Analysis
Differences in baseline characteristics were examined using χ2 tests for categorical variables and t tests for continuous variables. Change in condom use from baseline to follow-up assessments was examined using the McNemar test, stratified on intervention condition. Changes in condom use were examined as changes in 100% condom use as well as changes in any condom use. Differences in percent condom use by intervention condition over time were examined by using a random effects regression model.25 The intervention effect was evaluated by comparing slopes between the conditions over time.
RESULTS
Table 1 outlines the baseline characteristics of the sex workers by intervention condition. Baseline characteristics were comparable between the 2 sites except marital status, HIV/AIDS knowledge, and 100% condom use. A higher proportion of sex workers in the control community reported being married (43%), compared with 28% in the intervention community (χ2 = 4.91, P = 0.03). A higher proportion of sex workers in the intervention community knew at least 1 HIV/AIDS preventive method (67%), compared with 41% in the control community (χ2 = 13.61, P = 0.0002). Furthermore, a higher proportion of sex workers in the control group reported 100% condom use (47%), compared with 32% in the intervention group at the time of study initiation (χ2 = 4.71, P = 0.03).
TABLE 1.
Baseline Characteristics of Commercial Sex Workers by Intervention Condition
| Characteristics | Intervention (n = 100) |
Control (n = 100) |
Overall (n = 200) |
|---|---|---|---|
| Mean (SD) | |||
| Age in years | 26 (6.76) | 27 (7.30) | 27 (7.04) |
| Weekly income in rupees | 573 (457.74) | 522 (487.22) | 548 (472.21) |
| Time in profession in months | 100 (88.25) | 110 (81.87) | 105 (85.06) |
| Percentage | |||
| Married* | 28 | 43 | 36 |
| Work at other “red light” area | 25 | 29 | 27 |
| Alcohol use | 34 | 36 | 35 |
| Injecting drug use | 3 | 0 | 2 |
| Condom availability | 80 | 79 | 80 |
| Have a “babu” | 48 | 53 | 51 |
| Contractual agreement | |||
| Self | 76 | 68 | 72 |
| Adhyia or Chukri | 24 | 32 | 28 |
| Stay with husband or fixed client | 44 | 55 | 50 |
| Type of sexual practices | |||
| Penovaginal | 96 | 99 | 98 |
| Penorectal | 5 | 9 | 7 |
| Penooral | 21 | 24 | 23 |
| Group sex | 15 | 16 | 16 |
| Condom use | 46 | 54 | 50 |
| 100% condom use* | 32 | 47 | 40 |
| Knows at least 1 STD preventive method | 79 | 82 | 81 |
| Knows at least 1 HIV/AIDS preventive method* | 67 | 41 | 54 |
| Refused a client for a particular sex | 62 | 53 | 58 |
| Refused sex with a client who refused condom | 42 | 38 | 40 |
| Perceives oneself to be at risk for STDs/AIDS | 59 | 55 | 57 |
| Verbally abused in the last 3 months | 20 | 21 | 21 |
P < 0.05.
Most sex workers perceived that they were at risk for STD/HIV. About one-third were married and more than half had a regular sexual partner; about 1 in 4 had been verbally abused in the past 3 months. Most had been working in the profession for at least 7 years and earned >500 rupees per month, the equivalent of $12 US. Only about one-third of the sex workers reported using alcohol and very few injected drugs. Almost all risk stemmed from penovaginal sex, with relatively low rates of oral sex and almost no anal sex. Over their lifetime, >40% of participants had sought treatment for an STD. Blood samples from a subset of study participants (baseline = 79%; wave 1 = 73%; wave 2 = 87%; wave 3 = 81%) were used to conduct VDRL tests for syphilis exposure; about 60% had been exposed in their lifetime. However, low rates of current STD infection were identified from external physical examinations (<1%) and internal examinations (<10%). The initial base rates of STD were too low to allow us to use STD as an outcome measure of the intervention.
As shown in Table 2, changes in 100% condom use were examined from baseline to follow-up assessments, stratified by intervention condition. For changes in 100% condom use in the intervention group, 35 sex workers (39%) were classified as adopters between the baseline and the first follow-up assessment. Only 4 relapsers (4%) were observed. This difference was statistically significant (McNemar test = 26.64, P < 0.0001). When we assessed changes in 100% condom use in the control group, we found no statistically significant difference between 17 adopters (18%) and 11 relapsers (12%).
TABLE 2.
Change in Condom Use From Baseline to Follow-up Assessments, Stratified on Intervention Condition
| 100% Condom Use n (%) |
Any Condom Use n (%) |
|
|---|---|---|
| Baseline to wave 1—intervention community (n = 90) | ||
| Change in condom use | ||
| Adopters | 35 (38.9)* | 21 (23.3)* |
| Relapsers | 4 (4.4) | 4 (4.4) |
| Baseline to wave 1—control community (n = 93) | ||
| Change in condom use | ||
| Adopters | 17 (18.3) | 21 (22.6) |
| Relapsers | 11 (11.8) | 9 (9.7) |
| Baseline to wave 2—intervention community (n = 85) | ||
| Change in condom use | ||
| Adopters | 35 (41.2)* | 21 (24.7)* |
| Relapsers | 6 (7.1) | 8 (9.41) |
| Baseline to wave 2—control community (n = 88) | ||
| Change in condom use | ||
| Adopters | 16 (18.2) | 18 (20.4)* |
| Relapsers | 7 (8.0) | 6 (6.8) |
| Baseline to wave 3–intervention community (n = 92) | ||
| Change in condom use | ||
| Adopters | 37 (40.2)* | 36 (39.1)* |
| Relapsers | 6 (6.5) | 1 (1.1) |
| Baseline to wave 3–control community (n = 80) | ||
| Change in condom use | ||
| Adopters | 19 (23.8) | 16 (20) |
| Relapsers | 10 (12.5) | 12 (15) |
| Baseline to all 3 waves—intervention community (n = 84)† | ||
| Change in condom use | ||
| Adopters | 27 (32.1)* | 14 (16.7) |
| Relapsers | 6 (7.1) | 8 (9.5) |
| Baseline to all 3 waves—control community (n = 75)† | ||
| Change in condom use | ||
| Adopters | 7 (9.3)* | 7 (9.3)* |
| Relapsers | 19 (25.3) | 20 (26.7) |
Adopters are defined as those who converted from <100% condom use (or no condom use) at baseline to 100% condom use (or any condom use) at follow-up. Relapsers are defined as those who switched from 100% condom use (or any condom use) at baseline to <100% condom use (or no condom use) at follow-up.
P < 0.05 based on McNemar test statistic.
100% condom use or any condom use in all 3 waves.
Similar patterns were observed in changes in 100% condom use between the baseline and second follow-up assessment. We observed a significant difference between the 35 adopters (41%) and 6 relapsers (7%) (McNemar test = 20.51, P < 0.0001). In the control community, we found no significant difference between 16 adopters (18%) and 7 relapsers (8%). Changes in 100% condom use between the baseline and third follow-up assessment in the intervention group indicated that 37 sex workers (40%) were classified as adopters, whereas there were only 6 relapsers (7%) (McNemar test = 22.35, P < 0.0001). In the control group, we found no significant difference between 19 adopters (24%) and 10 relapsers (13%).
We were also interested in examining sex workers who remained as adopters throughout subsequent follow-up assessments. In the intervention community, we observed 27 adopters (32%) between the baseline to first follow-up who maintained 100% condom use in 2nd and 3rd follow-up assessments. Remarkably, we observed only 6 relapsers (7%) (McNemar test = 13.36, P = 0.0003). In the control community, only 7 sex workers (9%) maintained 100% condom use, whereas 19 sex workers (25%) failed to maintain 100% condom use. This difference was statistically significant (McNemar test = 5.54, P = 0.0186). Changes in condom use from baseline to follow-up assessments followed similar patterns (Table 2).
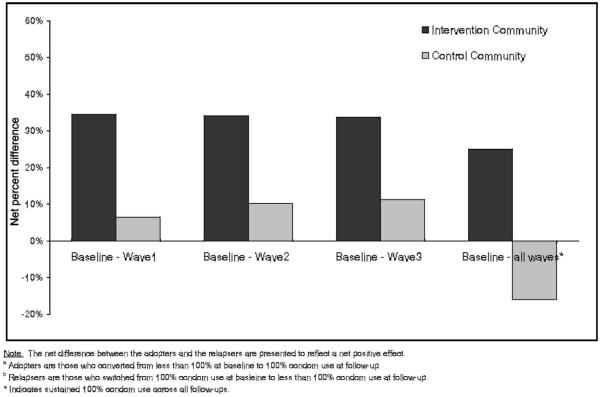
Figure 1 outlines the net difference in 100% condom use between adopters and relapsers by intervention condition. In the intervention community, we consistently observed significantly more adopters than relapsers at each assessment. In the control community, however, the net differences between the adopters and relapsers were not significant. In fact, the comparison of adopters and relapsers between baseline and all waves indicated that there were significantly more relapsers than adopters in the control community.
FIGURE 1.
Net difference in 100% condom use between adopters (a) and relapsers (b), stratified by intervention condition.
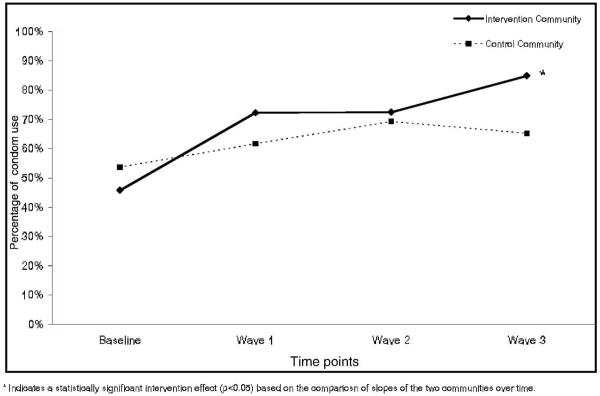
Figure 2 shows the percentage of condom use by intervention status. The percentage of condom use was examined using a random effects regression model, controlling for baseline differences in marital status and HIV/AIDS knowledge. We observed an increase in condom use in both the intervention and the control communities. However, condom use increased significantly more among sex workers in the intervention community than among those in the control community in a linear fashion over the 3 follow-up periods (B = 0.3447, P = 0.002).
FIGURE 2.
Percentage of condom use by intervention condition.
DISCUSSION
The Sonagachi Project has achieved worldwide recognition for its innovative approach to public health,26,27 including World Health Organization funding and coverage in The New York Times.28 The project organized an international meeting of sex workers in 2001 that mobilized thousands of sex workers in the Millennium Mila Mela Conference, demonstrating its impact as a social movement. However, there were few previous empirical data on which to evaluate the efficacy of this intervention.
Although it involved only 2 communities, the Sonagachi intervention resulted in significant increases in condom use in a relatively short period that were sustained for 16 months. Consistent condom use was demonstrated by an additional 40% of sex workers, a figure that was sustained over 3 assessments over 16 months. Fewer than 5% relapsed over that period in the intervention community. Comparable increases were not found in the control communities.
It is important to note that knowledge of STD- and AIDS-preventive methods were high prior to implementing the intervention. However, condom use was not similarly high. The rate of STDs was so low (<1%) that it was not feasible to demonstrate reductions in STD infection over the 16 months.
This is a relatively low-cost intervention that has benefits that extend beyond HIV prevention. The most significant cost is the establishment of a clinic that is available to provide treatment of STDs and training of sex workers to deliver prevention messages and promote condom use. Yet, there were significant increases in condom use once these resources were established in a community far removed from the initial intervention site in Calcutta. More than half of the sex workers had a regular sexual partner, a “babu.” Although we did not assess changes in communication between marital partners or babus, there were spontaneous reports that the intervention helped sex workers communicate and be assertive with their spouses, babus, and stakeholders. In addition to the treatment of STDs for sex workers, the health clinic also provided free health care to their families, clients, and other persons living in the red light areas. Having access to these resources may increase the perception of one’s status, as well as the status of sex workers in the community.
As this intervention was mounted over a very long period in Calcutta, a set of social entrepreneurial programs became attached (e.g., a micro-savings and lending cooperative, literacy programs, cultural programs, schools). Over the 16-month period, sex workers in the local sites had only just begun to build these resources, prioritizing services and education for their children and literacy for sex workers. However, with a forum for community dialogue and the experience of sex worker peer organizers from Calcutta, benefits accrued over time and continue to be implemented.
Notwithstanding our findings, the study had several limitations. First, only 2 communities were included, which limits the generalizability of our results. Nevertheless, we found significant differences in consistent condom use, suggesting the effectiveness of the Sonagachi intervention among sex workers in the 2 communities and other locales in India. It would be helpful, however, to increase the number of communities within India, and to test the intervention in locales outside of India, so as to increase external validity.
While steps were taken to avoid contamination, the research team noted some movement back and forth between the 2 communities and an awareness of the existence of an enhanced intervention among some sex workers in the control community. However, we still found significant differences in condom use across the sites. Given the inclusion of only 2 communities, it is also possible that differences in these communities, other than the intervention, contributed to differential rates of condom use. However, efforts were made by the research team, working in concert with members of the Calcutta-based team, to ensure parity across the selected communities in terms of size, language, religion, and other sociodemographic factors.
An additional limitation is that condom use was by self-report only. While we implemented VDRL testing at baseline and in subsequent waves as an independent marker of sexual risk, STD rates were too low to be of use in documenting sexual risk behavior. To reduce social desirability, separate teams of interviewers and intervention staff were maintained, interviewers were trained to remain nonjudgmental, and participants were identified by a code number only for the assessment and assured of confidentiality. Additionally, while not intended as an outcome measure for this study, the Calcutta-based team kept monthly records of the number of condoms sold (at a nominal, subsidized price) outside the clinic; the records indicate increases in condom sales over time and higher numbers of condoms distributed in the intervention community from the second wave onward as compared with the control community. While we cannot be assured that these condoms were used, condom supply measures tend to corroborate the self-reports of condom use among the sex workers, thus increasing our confidence in the results.
Lastly, the implementation of a control site that did not receive the enhanced intervention against STDs and HIV raises ethical dilemmas. However, efforts were made by the research team to address the ethical concerns. First, the provision of a free, accessible health clinic for sex workers in both of the sites was an improvement over the usual standard of care. Second, there was no guarantee that the intervention would be effective. And most importantly, in discussions between the U.S.-based research team and the Calcutta-based Sonagachi intervention team, it was agreed that at the end of the study period the control community would cross over; the Sonagachi team moved into the control community after the study period to provide the enhanced intervention.
Too often, effective interventions are conceptualized based on theories of social change and launched by university researchers. This intervention was designed by the community,29,30 is sustained by the community, and is taken to new communities by sex workers. In this replication, the mounting and design of the intervention were controlled by the Calcutta team of sex workers from the Sonagachi Project. The research team only conducted the evaluation of a project conceived and refined over time by the community. Greater emphasis must be placed on interventions arising from communities if HIV prevention programs are to be sustained and broadly implemented.
REFERENCES
- 1.Gangakhedkar R, Bentley M, Divekar A, et al. Spread of HIV infection in married monogamous women in India. JAMA. 1997;278:2090–2092. [PubMed] [Google Scholar]
- 2.National AIDS Control Organisation . Country Scenario 1997-98. Ministry of Health and Family Welfare; New Delhi, India: 1998. pp. 15–31. [Google Scholar]
- 3.Centers for Disease Control and Prevention Health: HIV/AIDS time bomb ticking in India. IPS Wire. 1997 December 1; [Google Scholar]
- 4.UNAIDS . Female Sex Worker HIV Prevention Projects: Lessons Learnt From Papua New Guinea, India, and Bangladesh. UNAIDS; Geneva, Switzerland: 2000. [Google Scholar]
- 5.National AIDS Control Organisation . Combatting HIV/AIDS in India 2000-2001. Ministry of Health and Family Welfare, Government of India; [Accessed June 17, 2003]. 2001. Available at: http://naco.nic.in. [Google Scholar]
- 6.UNAIDS . HIV and AIDS-Related Stigmatization, Discrimination and Denial: Forms, Contexts, and Determinants. UNAIDS; Geneva, Switzerland: 2000. [Google Scholar]
- 7.UNAIDS . Report on the Global HIV/AIDS Epidemic. UNAIDS; Geneva, Switzerland: 2002. [Google Scholar]
- 8.Fortenberry JD, McFarlane M, Bleakley A, et al. Relationships of stigma and shame to gonorrhea and HIV screening. Am J Public Health. 2002;92:378–381. doi: 10.2105/ajph.92.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Valdiserri RO. HIV/AIDS stigma: an impediment to public health. Am J Public Health. 2002;92:341–342. doi: 10.2105/ajph.92.3.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chesney MA, Smith AW. Critical delays in HIV testing and care. Am Behav Scientist. 1999;42:1162–1174. [Google Scholar]
- 11.Herek GM. AIDS and stigma. Am Behav Scientist. 1999;42:1106–1116. [Google Scholar]
- 12.Rao V, Gupta I, Lokshin M, et al. Sex workers and the cost of safe sex: the compensating differential for condom use among Calcutta prostitutes. J Dev Econ. 2003;71:585–603. [Google Scholar]
- 13.Pegacao Brazil: sex and self-worth. AIDS Action. 1991;15:5. [PubMed] [Google Scholar]
- 14.Panos Institute . The Hidden Cost of AIDS: The Challenge of HIV to Development. The Panos Institute; London: 1992. [Google Scholar]
- 15.Schoeof BG. AIDS action-research with women in Kinshasa, Zaire. Soc Sci Med. 1993;37:1401–1413. doi: 10.1016/0277-9536(93)90170-9. [DOI] [PubMed] [Google Scholar]
- 16.Asthana S, Oostvogels R. Community participation in HIV prevention: problems and prospects for community-based strategies among female sex workers in Madras. Soc Sci Med. 1996;43:133–148. doi: 10.1016/0277-9536(95)00348-7. [DOI] [PubMed] [Google Scholar]
- 17.Nagelkerke NJD, Jha P, de Vlas SJ, et al. Modeling HIV/AIDS epidemics in Botswana and India: impact of interventions to prevent transmission. Bull World Health Organ. 2002;80:89–96. [PMC free article] [PubMed] [Google Scholar]
- 18.Nath MB. Women’s health and HIV: experience from a sex workers’ project in Calcutta. Gend Dev. 2000;8:100–108. doi: 10.1080/741923417. [DOI] [PubMed] [Google Scholar]
- 19.Bandyopadhyay N, Banerjee B. Sex workers in Calcutta organize themselves to become agents for change. Sex Health Exch. 1999;2:6–8. [PubMed] [Google Scholar]
- 20.Chakraborty AK, Jana S, Das A, et al. Community based survey of STD/HIV infection among commercial sexworkers in Calcutta (India): part I: some social features of commercial sexworkers. J Commun Dis. 1994;26:161–167. [PubMed] [Google Scholar]
- 21.Jana S, Chakraborty AK, Das A, et al. Community based survey of STD/HIV infection among commercial sex-workers in Calcutta (India): part II: sexual behaviour, knowledge and attitude towards STD. J Commun Dis. 1994;26:168–171. [PubMed] [Google Scholar]
- 22.Kumar S. Model for sexual health found in India’s West Bengal. Lancet. 1998;351:46. doi: 10.1016/S0140-6736(05)78070-3. [DOI] [PubMed] [Google Scholar]
- 23.Singh IP. STD-HIV intervention programme: the Sonagachi model. Health Millions. 1998;24:11–13. [PubMed] [Google Scholar]
- 24.Evans C, Lambert H. Health-seeking strategies and sexual health among female sex workers in urban India: implications for research and service provision. Soc Sci Med. 1997;44:1791–1803. doi: 10.1016/s0277-9536(96)00288-2. [DOI] [PubMed] [Google Scholar]
- 25.Littell RC, Milliken GA, Stroup WW, et al. SAS7 System for Mixed Models. SAS Institute; Cary, NC: 1996. [Google Scholar]
- 26.Jana S, Bandyopadhyay N, Mukherjee S, et al. STD/HIV intervention with sex workers in West Bengal, India. AIDS. 1998;12(suppl B):S101–108. [PubMed] [Google Scholar]
- 27.Jana S. Herpes, cytomegalovirus, and other STDs in high risk group. Indian J Sex Transm Dis. 1996;17:11–14. [Google Scholar]
- 28.Dugger CW. Calcutta’s prostitutes lead the fight on AIDS. The New York Times. 1999 January 4;:A1, A8. [Google Scholar]
- 29.Kelly JA. Community implementation of HIV research intervention; Paper presented at: Center for HIV Identification, Prevention and Treatment Services (CHIPTS) Colloquia at the AIDS Service Center; Pasadena, CA. March 25, 1999. [Google Scholar]
- 30.Kelly JA. Community-level interventions are needed to prevent new HIV infections. Am J Public Health. 1999;89:299–301. doi: 10.2105/ajph.89.3.299. [DOI] [PMC free article] [PubMed] [Google Scholar]