Abstract
In 2002, several hospitals in the Tenet system were accused of overbilling Medicare for cardiac surgery. This led to increased scrutiny of so-called outlier payments, which are used to compensate hospitals when actual costs far exceed those anticipated under prospective payment. Since then, the overall proportion of coronary artery bypass graft (CABG) procedures associated with outlier payments has fallen from 13 percent in 2000–02 to 8 percent in 2003–06. Still, there is variation across U.S. hospitals, with some hospitals experiencing much higher rates. These findings imply that there is potential for quality improvement to reduce costs while improving morbidity and mortality.
Inpatient surgery is a major component of overall spending in the U.S. Medicare program, accounting for almost half of total inpatient costs. Medicare's prospective payment system (PPS) pays hospitals for inpatient surgical procedures according to predetermined rates, based on diagnosis-related groups (DRGs). DRG categories are defined by principal diagnosis, major procedures performed, and the presence of comorbidities or complications. In addition, the Centers for Medicare and Medicaid Services (CMS) makes extra payments—so-called outlier payments—for procedures and hospitalizations that are unusually expensive.1 A hospital is eligible for outlier payments when its estimated costs for a particular service (submitted charges multiplied by the hospital's cost-to-charge ratio, or CCR) exceed the PPS rate by a specified amount (the stop-loss amount).2
Outlier payments received much public scrutiny in 2002, when several hospitals owned by the Tenet system were accused of using this mechanism to overbill Medicare for cardiac surgery.3 These hospitals were rapidly increasing their charges ahead of their CCRs (possible because hospital cost reports often lag current charges by two years or more), thereby overstating their true costs and triggering excessive outlier payments. Tenet was fined for its billing practices; however, hospital outlier payment rates varied widely outside that health system, with rates exceeding 20 percent for surgical patients at many hospitals. In response, the CMS revised its accounting practices related to outlier payments and raised the stop-loss amount from $21,025 in 2002 to $33,560 in 2003.4
In this study we examined the use of outlier payments with coronary artery bypass graft (CABG) surgery in Medicare (the program of insurance for elderly and disabled Americans). We assessed whether the CMS's efforts have reduced outlier payments over time and variations across hospitals. Because outlier payments are often associated with patients with complications and protracted hospitals stays after surgery, we were particularly interested in relationships between outlier payment rates and hospital quality.
“Our composite measure is a strong predictor of future risk-adjusted mortality and thus a useful measure of hospital quality.”
Study Data And Methods
Subjects and databases
This study used data from the Medicare Provider Analysis and Review (MedPAR) files, 2000–2006. Because services provided to Medicare managed care patients are not consistently captured in the MedPAR files, such patients were excluded from our study. We also excluded patients younger than age sixty-five or older than age ninety-nine.
Patients undergoing isolated CABG procedures were identified using the appropriate procedure codes from the International Classification of Diseases, Ninth Version (ICD-9). To minimize confounding by differences in procedure complexity over time or across hospitals, we excluded patients undergoing concurrent heart valve procedures.
Analysis
Our first goal was to assess changes in the proportion of patients associated with outlier payments over time. For each patient, the presence of an outlier payment, and the associated amount, was obtained from the appropriate MedPAR fields. In assessing secular trends in outlier payments with CABG, we used linear regression to control for year and patients' age, sex, race, acuity at admission, and comorbid conditions, using the methods of Anne Elixhauser and colleagues.5 Standard errors were calculated allowing for within-hospital correlation in patient out-comes.6
We also examined the extent to which outlier payments vary across hospitals and potential explanatory factors. To reflect current payment trends, our analysis was limited to the most recent year for which data were available (2006). We excluded hospitals with fewer than twenty cases (6.7 percent of hospitals, 0.5 percent of patients), to minimize the role of chance in our description of hospital-level variation in outlier payment rates.
To assess the role of illness severity, we first assessed relationships between risk factors and outlier payments at the patient level. Using multiple logistic regression, we then characterized the severity of hospitalized patients' illnesses according to the average predicted mortality among patients undergoing CABG in 2006 at each hospital. In the regression we controlled for patients' age, sex, race, acuity at admission, and comorbid conditions. Hospitals were then ranked and sorted into quintiles according to illness severity. Relationships between hospital illness severity (in quintiles) and outlier payment rates were then assessed using chi-square tests.
We then used similar methods to assess the association between hospital quality and outlier payments. To characterize hospital quality, we used a composite measure derived from each hospital's risk-adjusted mortality rate and its procedure volume, shown previously to be superior to risk-adjusted mortality alone in predicting hospital performance.7 Hospital quality was characterized based on data from 2004–05, rather than on contemporaneous (2006) data.
Patients with complicated and prolonged hospitalizations sufficient to trigger outlier payments have much higher mortality than patients without outlier payments. To the extent that mortality is a large component of our composite quality measure, assessing quality and outlier payments on the same patient population would ensure spuriously strong correlations between the two measures. Although based on data from preceding years, our composite measure is a strong predictor of future risk-adjusted mortality and thus a useful measure of hospital quality in this context.8
All statistical analyses were conducted using Stata 10.0. This study was judged exempt by the Institutional Review Board at the University of Michigan.
Study Results
The proportion of patients with outlier payments fell significantly over time (Exhibit 1). Most of the decline occurred in 2003, the year following the Tenet scandal. Outlier payment rates fell from 12.5 percent in 2002 to 8.6 percent to 2003, while average amounts of outlier payments remained relatively constant. Total Medicare payments of this type for isolated CABG fell from $343 million in 2000 to $176 million in 2006.
EXHIBIT 1. Outlier Payments For Isolated Coronary Artery Bypass Graft (CABG) Procedures, Based On Nationwide Medicare Data, 2000–2006.
| Indicator | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | p value |
|---|---|---|---|---|---|---|---|---|
| Total number of patients | 150,917 | 146,008 | 144,586 | 134,128 | 126,126 | 114,738 | 104,329 | –a |
| Total number of patients receiving outlier payments | 20,031 | 19,207 | 18,020 | 11,561 | 8,712 | 9,329 | 9,432 | –a |
| Percent of patients receiving outlier payments | 13.3 | 13.2 | 12.5 | 8.6 | 6.9 | 8.1 | 9.0 | <0.0001 |
| Mean of total outlier payments | $17,127 | $19,469 | $23,045 | $24,922 | $21,033 | $19,688 | $18,699 | <0.0001 |
| Ratio of total outlier payments/total Medicare payments (%) | 8.6 | 9.3 | 10.1 | 7.5 | 5.0 | 5.3 | 5.4 | 0.02 |
| Total outlier payments (millions) | $343 | $374 | $415 | $288 | $183 | $184 | $176 | –a |
| Total Medicare payments (millions) | $3,997 | $4,024 | $4,097 | $3,827 | $3,645 | $3,487 | $3,252 | –a |
SOURCE: Authors' analysis based on Medicare Provider Analysis and Review (MedPAR) data, 2000–2006.
Not applicable.
In addition to the overall reductions in outlier payments, variations in payment rates across hospitals also declined (Exhibit 2). Nonetheless, there remains considerable variation in reimbursement across U.S. hospitals. In 2006, 30.6 percent of hospitals had outlier payment rates below 5 percent, while 20.1 percent of hospitals had outlier payment rates exceeding 15 percent; 422 hospitals (12 percent) had rates of 20 percent or higher (data not shown).
EXHIBIT 2. Distribution In Hospital Rates Of Outlier Payment For Coronary Artery Bypass Graft (CABG) Procedures, Nationwide Medicare Data, 2000 And 2006.
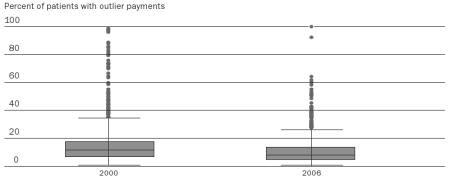 |
SOURCE: Authors' analysis based on Medicare Provider Analysis and Review (MedPAR) data, 2000–2006.
NOTES: The boxes show the twenty-fifth, fiftieth, and seventy-fifth percentiles for the hospital outlier payment rates, while the whiskers indicate the fifth and ninety-fifth percentiles. Dots show hospitals outside this range.
Older patients and those with urgent or emergent admissions were more likely than other patients to engender outlier payments (Exhibit 3). There were no clinically important differences in race and sex among patients with and without outlier payments. Paradoxically, patients with outlier payments had fewer comorbidities than those without such payments, likely as a result of acute, postoperative conditions' “crowding out” comorbidities (pre-existing conditions) on Medicare claims.9
EXHIBIT 3. Patient And Hospital Characteristics Of Patients With And Without Outlier Payments, Based On 2006 Medicare Data.
| Demographics | Patients with outlier payments | Patients without outlier payments | p value | Odds ratio (OR) | 95% CI of OR |
|---|---|---|---|---|---|
| Number of patients | 9,432 | 94,897 | –a | –a | |
| Number of hospitals | 1,054 | 1,144 | –a | –a | |
| Patient characteristics | |||||
| Age (% 75+ years) | 50.7 | 43.5 | <0.001 | 1.31 | (1.25, 1.37) |
| Sex (% female) | 34.5 | 32.1 | <0.001 | 1.07 | (1.02, 1.13) |
| Race (% black) | 6.1 | 5.3 | 0.001 | 1.18 | (1.08, 1.30) |
| Admission acuity (% urgent/emergent | 65.7 | 50.6 | <0.001 | 1.85 | (1.77, 1.94) |
| Comorbidity (% 2+) | 57.7 | 65.9 | <0.001 | 0.70 | (0.67, 0.73) |
| Provider characteristics | |||||
| Teaching (%) | 25.1 | 27.0 | 0.0002 | 0.97 | (0.92, 1.02) |
| Hospital volume tercile | |||||
| Low | 42.6 | 33.1 | <0.001 | ||
| Medium | 31.5 | 33.7 | <0.001 | 0.76 | (0.72, 0.80) |
| High | 25.9 | 33.2 | <0.001 | 0.63 | (0.59, 0.67) |
SOURCE: Authors' analysis based on Medicare Provider Analysis and Review (MedPAR) data, 2006.
NOTE: CI is confidence interval
Not applicable.
Nonetheless, age and illness severity did not explain variation in outlier payment rates across hospitals. Severity varied moderately across hospital quintiles, with predicted mortality rates ranging from 3.5 percent to 5.0 percent. However, outlier payments were nearly identical across the five quintiles of severity among hospitalized patients (Exhibit 4).
EXHIBIT 4. Medicare Outlier Payment Rates, In 2006, According To Illness Severity And Hospital Quality, As Defined By A Composite Risk Measure Of 2004–05 Procedure Volume And Risk-Adjusted Mortality.
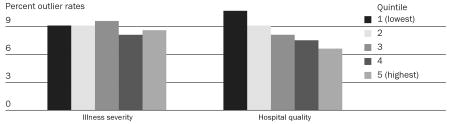 |
SOURCE: Authors' analysis based on Medicare Provider Analysis and Review (MedPAR) data, 2004–2006.
NOTE: Illness severity was based on 2006 predicted mortality rates.
In contrast, hospital quality was strongly associated with outlier payment rates (Exhibit 4). Quality, estimated by a composite measure of risk-adjusted mortality, varied markedly across hospital quintiles, from 2.1 percent to 8.3 percent (data not shown). Hospitals in the lowest quintile of quality had outlier payment rates of 10.8 percent, compared with only 6.7 percent in the highest-quality hospitals (p < 0.0001).
Discussion
In the wake of the Tenet billing scandal of 2002, Medicare outlier payments for cardiac surgery fell dramatically. The CMS's 60 percent increase in the national stop-loss amount between 2002 and 2003 no doubt contributed to the abrupt decline in those years. Closing the loophole that allowed hospitals with high charges to use their statewide average cost-to-charge ratio is another likely factor in falling outlier payment rates. Finally, government fines and private-sector lawsuits against Tenet may have prompted other hospitals to become more conservative in their billing practices.
Between 2000 and 2006, total Medicare outlier payments for isolated CABG fell by approximately $170 million annually. Although this amount may seem modest (relative to the overall costs of inpatient surgery), CABG is only one of a long list of inpatient procedures for which outlier payments are common. To the extent that mechanisms underlying the decline with CABG have reduced outlier payments with other procedures, the total savings for Medicare could be substantial.
Outlier payment rates and quality
Al though persistent differences in billing and accounting practices may be an important driver of variation in hospital outlier payment rates, hospital quality is another. In this study, outlier payment rates at high-quality hospitals were 40 percent lower than at low-quality hospitals. This finding is perhaps not surprising. High-quality hospitals have fewer patients with adverse outcomes, who tend to have longer lengths-of-stay and require intensive care, reoperations, and other expensive interventions that collectively trigger outlier payments. Nonetheless, our study is among the first to demonstrate a direct relationship between hospital quality and outlier payments. Of course, hospital quality may be related to many other expenses besides outlier payments. For example, poor quality may push more patients to higher-paying DRG levels, necessitate more specialist consultations and tests during hospitalization, and lead to higher requirements for home health care and extended care facilities after discharge.
Limitations
Our study has several important limitations. First, we examined only Medicare payments. This patient population is important to the extent that more than half of all CABG procedures in the United States are performed on patients age sixty-five and older. Nonetheless, reimbursement practices and policies with regard to outlier payments likely vary widely, and thus our findings cannot be generalized to private-sector payers.
Second, our analysis was based on Medicare claims data. Given the well-recognized limitations of administrative data in capturing comorbidities and other risk factors, we may have underestimated the impact of illness severity on outlier payments.10 For CABG, however, it seems unlikely that hospital case-mix is a major determinant of variation in outlier payment rates across facilities. Our previous research assessing the importance of risk adjustment with this procedure suggests little variation in case-mix across hospitals.11
There are also limitations associated with using administrative data to assess hospital quality. Our composite measure is more robust in capturing systematic variation and forecasting future hospital performance than individual quality indicators are (for example, volume or risk-adjusted mortality alone). To the extent that this composite remains an imperfect proxy of hospital quality however, our study likely underestimates the relationship between quality and outlier payment rates.
Outlier payments and surgery costs
The CMS could take additional steps to eliminate unwanted variations in hospital outlier payments with CABG and other procedures. Much as it hopes to discourage so-called never events and other adverse outcomes by refusing to pay for them, the CMS could reduce or eliminate outlier payments for patients whose outlier status relates to potentially avoidable complications.12 Its ongoing efforts to increase bundling of surgical episode payments could also include tighter restrictions on outlier payments.13 Payment reform might not be the only approach to reducing outlier payments, however. Our findings linking hospital quality to outlier payments suggest that quality improvement may be an equally important component of the CMS's efforts to reduce the costs of inpatient surgery.
Acknowledgments
This study was supported by the National Institute on Aging (Grant nos. 1R21AG027819-01 and P01AG019783-07S1). The views expressed herein do not necessarily represent the views of the Centers for Medicare and Medicaid Services or the U.S. government.
Notes
- 1.Centers for Medicare and Medicaid Services. Acute Inpatient PPS Outlier Payments. [9 April 2009];2006 October; http://www.cms.hhs.gov/AcuteInpatientPPS/04_outlier.asp.
- 2.Medicare fiscal intermediaries determine hospital CCRs based on cost reports filed by hospitals. The CCR represents the estimated true costs of services (within defined categories) listed on the hospital's cost report, divided by gross charges in effect during the cost report period.
- 3.Moynihan R. Another U.S. Healthcare Giant Is Hit by Scandal. BMJ. 2003;327(7424):1128. [Google Scholar]; Silverman E. Tough Negotiations in Store between Plans and Hospitals. Managed Care. 2003;12(10):42–45. [PubMed] [Google Scholar]; The Real Tenet Scandal. Wall Street Journal. 2002 December 31; [Google Scholar]
- 4.Among other changes, the CMS closed a longstanding accounting loophole often exploited by hospitals. In previous years, hospitals were allowed to use the statewide average CCR if their own CCRs fell outside three standard deviations from the statewide average. By raising their charges sufficiently, hospitals could reduce their CCRs low enough to trigger the statewide average provision. In this scenario, a hospital's very high covered charges would be multiplied by a much higher CCR, leading to a substantial overstatement of covered costs and much higher outlier payments. The CMS eliminated this statewide average provision in 2003.
- 5.Elixhauser A, et al. Comorbidity Measures for Use with Administrative Data. Medical Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. Cambridge, Mass.: MIT Press; 2002. [Google Scholar]
- 7.Based on hierarchical models and empirical Bayes techniques, this composite measure predicts a hospital's true risk-adjusted mortality by combining two important measures: its actual risk-adjusted mortality and its procedure volume. The weight placed on each input varies across hospitals, with more weight placed on mortality when it was measured reliably (that is, at hospitals that have higher caseloads). The remaining weight is then placed on hospital volume, thus accounting for empirical relationships between volume and mortality with this procedure. This approach ensures an optimal combination of these two measures, as the direct measure (mortality) is weighted to the extent it is reliable, and the proxy measure (volume) is weighted only to the extent necessary.; Staiger DO, et al. Empirically Derived Composite Measures of Surgical Performance. Medical Care. 2009;47(2):226–233. doi: 10.1097/MLR.0b013e3181847574. [DOI] [PubMed] [Google Scholar]; Snijders TAB, Bosker RJ. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. California: Sage Publications; 1999. [Google Scholar]
- 8.Ibid.
- 9.Finlayson EV, et al. Adjusting Surgical Mortality Rates for Patient Comorbidities: More Harm than Good? Surgery. 2002;132(5):787–794. doi: 10.1067/msy.2002.126509. [DOI] [PubMed] [Google Scholar]; Iezzoni LI, et al. Chronic Conditions and Risk of In-Hospital Death. Health Services Research. 1994;29(4):435–460. [PMC free article] [PubMed] [Google Scholar]; Shwartz M, et al. The Importance of Comorbidities in Explaining Differences in Patient Costs. Medical Care. 1996;34(8):767–782. doi: 10.1097/00005650-199608000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Fisher ES. The Accuracy of Medicare's Hospital Claims Data: Progress Has Been Made, but Problems Remain. American Journal of Public Health. 1992;82(2):243–248. doi: 10.2105/ajph.82.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]; Baron JA, et al. Internal Validation of Medicare Claims Data. Epidemiology. 1994;5(5):541–544. [PubMed] [Google Scholar]; Malenka DJ, et al. Using Administrative Data to Describe Case-mix: A Comparison with the Medical Record. Journal of Clinical Epidemiology. 1994;47(9):1027–1032. doi: 10.1016/0895-4356(94)90118-x. [DOI] [PubMed] [Google Scholar]
- 11.Dimick JB, Birkmeyer JD. Ranking Hospitals on Surgical Quality: Does Risk-Adjustment Always Matter? Journal of the American College of Surgeons. 2008;207(3):347–351. doi: 10.1016/j.jamcollsurg.2008.04.014. [DOI] [PubMed] [Google Scholar]
- 12.Effective 1 October 2008, as mandated by the Deficit Reduction Act of 2005, the CMS will require Medicare-participating hospitals to disclose all hospital-acquired conditions (HACs). For HACs and the included “never events,” the CMS will pay Medicare-participating hospitals as though the secondary diagnosis, or never event, was not present. See Center for Medicare Advocacy. CMS to Hospitals: If It Should Never Happen, We Will Never Pay. [9 April 2009]; http://www.medicareadvocacy.org/Reform_08_09.25.NeverEvents.htm..
- 13.Hackbarth G, Reischauer R, Mutti A. Collective Accountability for Medical Care—To-ward Bundled Medicare Payments. New England Journal of Medicine. 2008;359(1):3–5. doi: 10.1056/NEJMp0803749. [DOI] [PubMed] [Google Scholar]


