Abstract
Background
Food security (i.e., a condition in which all people, at all times, have physical and economic access to sufficient, safe and nutritious food to meet their dietary needs and food preferences for an active and healthy life) has been noted to be lower in indigenous communities in Canada. We investigated the prevalence of inadequate food security, or food insecurity, among Inuit households with preschool children.
Methods
We conducted a cross-sectional survey of the health status of 388 randomly selected Inuit children aged three to five years in 16 Nunavut communities during the period from 2007 to 2008. From the survey data, we classified levels of food insecurity specifically among children. We also classified levels of overall food insecurity of the household of each child. We calculated the weighted prevalence of levels of child food insecurity and of household food insecurity.
Results
Nearly 70% of Inuit preschoolers resided in households rated as food insecure (69.6%; 95% confidence interval [CI] 64.7%–74.6%). Overall, 31.0% of children were moderately food insecure, and 25.1% were severely food insecure, with a weighted prevalence of child food insecurity of 56.1% (95% CI 51.0%–61.3%). Primary care-givers in households in which children were severely food insecure reported experiencing times in the past year when their children skipped meals (75.8%), went hungry (90.4%) or did not eat for a whole day (60.1%). Primary caregivers in households in which children were moderately food insecure reported experiencing times in the past year when they worried food would run out (85.1%), when they fed their children less expensive food (95.1%) and when their children did not eat enough because there was no money for food (64.3%).
Interpretation
We observed a high prevalence of household food insecurity, with a substantial proportion of children with severely food insecure status. Interventions are needed to ensure a healthy start in life for Inuit preschoolers.
According to the 1996 World Food Summit, food security exists when “all people, at all times, have physical and economic access to sufficient, safe and nutritious food to meet their dietary needs and food preferences for an active and healthy life.”1 Food security is essential for public health2 and important for child development. Suboptimal food security, or food insecurity, has deleterious effects on children’s academic performance and psychosocial development.3,4 In Canada, food insecurity is higher in the three territories than in the provinces.5 According to limited data, a high degree of food insecurity exists among Inuit in particular.6,7 Further, in most remote communities, the cost of food is at least double that in southern Canadian cities.8
We assessed the prevalence of food insecurity among Inuit preschool-aged children.
Methods
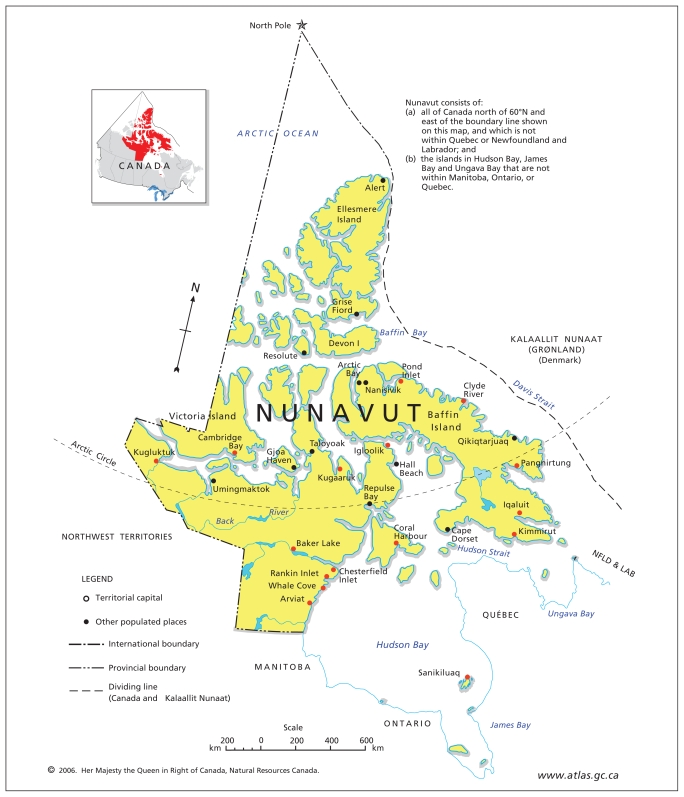
We conducted a cross-sectional survey of the health of preschool-aged Inuit children in the late summer and fall of 2007 and 2008 in 16 of the 25 communities of Nunavut. The communities we included in the survey represented all three regions of the territory. These communities were Arviat, Baker Lake, Cambridge Bay, Chesterfield Inlet, Clyde River, Coral Harbour, Igloolik, Iqaluit, Kimmirut, Kugaaruk, Kugluktuk, Pangnirtung, Pond Inlet, Rankin Inlet, Sanikiluaq and Whale Cove (Figure 1). The surveyed communities were situated in a geographic area from latitude 56° 32′N to 72° 40′N. We did not include certain communities in the survey because of logistic constraints related to flight schedules and high study-related costs relative to the numbers of children in the target age-group in those communities.
Figure 1.
Map of Nunavut showing communities (red dots) that participated in the Nunavut Inuit Child Health Survey, 2007–2008.
All Inuit children aged three to five years of age who resided in the surveyed communities were eligible to participate. We recruited the children using lists supplied by community health centres, which maintain lists by age of all young children in their respective communities to facilitate vaccine delivery. We also used a list of the households in which three-to five-year-old children resided that had participated in the International Polar Year Inuit Health Survey for Adults (www.inuithealthsurvey.ca). Randomization of both lists and selection of participating children were carried out by a member of the field research staff using a random number table. For households with more than two children in the target age group, we selected the child whose birthday was closest to the date of the survey.
We developed the study with the participation of members of the Qanuippitali Steering Committee of the Nunavut Inuit Health Survey. The committee included representatives of the Nunavut Association of Municipalities, Nunavut Tunngavik Inc., the Government of Nunavut Department of Health and Social Services, the University of Toronto and the Centre for Indigenous Peoples’ Nutrition and Environment at McGill University. We obtained a scientific research licence from the Nunavut Research Institute and a certificate of ethical acceptability from the Institutional Review Board of the McGill Faculty of Medicine. We asked the primary caregivers of children participating in the survey to view an informational DVD and then sign a form consenting to their children’s participation in the study.
Face-to-face interviews with primary caregivers were conducted at the local health centre of each community by members of the research team who were bilingual in English and Inuit language or dialects. The interview process involved the administration of demographic questionnaires and the 18-item Household Food Security Survey Module (slightly modified by Indian and Northern Affairs Canada)7 of the United States Department of Agriculture.9,10 Ten of these 18 questions are specific to the food security status of the adults in a surveyed household and eight are specific to the food security status of children in the household. The questions used in the interview are provided in Table 1.
Table 1.
Prevalence of affirmative responses* to questions about food security
| Questions (based on the previous 12 months) | Prevalence, %(95% CI) | |||
|---|---|---|---|---|
| All respondents | Child food secure | Moderately child food insecure | Severely child food insecure | |
| 1. Did you ever worry whether the food for you and your family would run out before you have money to buy more? | 65.9 (60.8–70.9) | 35.9 (28.0–43.7) | 85.1 (78.8–91.4) | 94.5 (89.3–99.6) |
| 2. Were there times when the food for you and your family just did not last, and there was no money to buy more? | 66.6 (61.5–71.8) | 32.4 (24.2–40.7) | 91.1 (86.0–96.3) | 96.1 (92.1–100) |
| 3. Were there times when you and your family could not afford to eat healthy food? | 54.6 (49.3–59.8) | 19.1 (12.1–26.1) | 77.9 (71.1–84.7) | 87.6 (79.9–95.4) |
| 4. Were there times when you could only feed your children less expensive foods because you were running out of money to buy food? | 62.9 (57.7–68.1) | 20.9 (13.6–28.1) | 95.1 (90.9–99.3) | 96.5 (92.4–100) |
| 5. Were there times when it was not possible to feed the children a healthy meal because there was not enough money? | 51.0 (45.8–56.1) | 4.4 (0.9–7.8) | 80.4 (72.8–87.9) | 96.0 (91.0–100) |
| 6. Were there times when the children in the house were not eating enough because there was no money to buy enough food? | 44.9 (39.6–50.2) | 1.5 (0.1–3.0) | 64.3 (54.9–73.7) | 96.7 (93.2–100) |
| 7. Did you or other adults in your household ever cut the size of your meals or skip meals because there wasn’t enough money for food? | 38.2 (32.8–43.6) | 8.9 (3.7–14.2) | 44.5 (34.9–54.0) | 81.6 (72.5–90.7) |
| 8. How often did this happen?† | 30.0 (25.0–35.1) | 4.7 (0.8–8.7) | 32.8 (23.9–41.7) | 70.8 (60.4–81.2) |
| 9. Did you ever eat less than you felt you should because there wasn’t enough money to buy food? | 38.7 (33.4–44.0) | 3.9 (0.7–7.2) | 47.5 (38.7–56.4) | 88.5 (82.1–94.9) |
| 10. Were you ever hungry but didn’t eat because you couldn’t afford enough food? | 29.6 (24.7–34.6) | 1.6 (0–3.5) | 26.1 (17.6–34.7) | 82.8 (74.1–91.5) |
| 11. Did you lose weight because you didn’t have enough money for food? | 17.7 (13.7–21.7) | 1.7 (0–3.3) | 13.1 (6.7–19.5) | 51.4 (40.8–62.0) |
| 12. Did you or other adults in your household ever not eat for a whole day because there wasn’t enough money for food? | 18.6 (14.5–22.8) | 0 | 8.0 (3.6–12.4) | 64.3 (53.6–75.0) |
| 13. How often did this happen?† | 18.6 (14.5–22.8) | 0 | 8.0 (3.6–12.4) | 64.3 (53.6–75.0) |
| 14. Did you ever cut the size of the children’s meals because there wasn’t enough money for food? | 22.7 (18.1–27.3) | 0.8 (0–2.3) | 12.6 (6.2–19.1) | 73.3 (63.5–83.0) |
| 15. Did any of the children ever skip meals because there wasn’t enough money for food? | 20.3 (16.0–24.7) | 0 | 4.1 (0.4–7.8) | 75.8 (66.0–85.6) |
| 16. How often did any of the children ever skip meals because there wasn’t enough money for food?† | 17.4 (13.3–21.5) | 0 | 4.1 (0.4–7.8) | 64.3 (53.6–74.9) |
| 17. Were the children ever hungry but you just couldn’t afford more food? | 25.6 (20.9–30.4) | 0 | 9.4 (4.3–14.5) | 90.4 (84.3–96.5) |
| 18. Did your children ever not eat for a whole day because there wasn’t enough money for food? | 15.3 (11.3–19.2) | 0 | 0.5 (0–1.5) | 60.1 (49.5–70.7) |
Note: CI = confidence interval.
”Yes,” “often” and “sometimes” were considered to be affirmative responses.
”Almost every month,” “some months” and “1–2 months” were considered to be affirmative responses.
Using the definitions and classification scale established by Health Canada, we classified the food security status of adults in each household and that of children in each household. On the 18-item questionnaire, 0–1 affirmative responses to the 10 adult-specific questions indicated “food secure” adults, and 0–1 affirmative responses to the eight child-referenced questions indicated “food secure” children. A status of “moderately food insecure” for adults was indicated by 2–5 affirmative responses to the adult-referenced questions and, for children, by 2–4 affirmative responses to the child-referenced questions. A status of “severely food insecure” for adults was indicated by six or more affirmative responses to the adult-referenced questions and, for children, by five or more affirmative responses to the child-referenced questions.11 Among children, groups described by Health Canada as “severely food insecure” correspond to the designation of “very low food security” used by the United States Department of Agriculture.”12 Severe food insecurity exists when there is evidence of reduced food intake and disrupted eating patterns.
We determined the overall level of household food insecurity by combining the food security rating of the adults with that of the children in each household. When both the adults and children in a household were rated as having food secure status, we considered the household to be food secure. We considered a household to be moderately food insecure when either the adults or children (or both) in the household were moderately food insecure and neither were severely food insecure. We considered a household to be severely food insecure when either the adults or children (or both) in the household were severely food insecure.
We determined the prevalence of overweight and obesity among participants based on body mass index (Kg/m2) measures standardized for age and sex.13 We calculated the weighted prevalence and 95% confidence intervals [CIs] of food insecurity and affirmative responses to individual questionnaire items stratified by community. Sampling weights reflected the proportion of participating children in each community. We obtained the denominator (i.e., total number of Inuit children aged three to five years of age residing in the surveyed communities) from the lists of names and ages supplied by the community health centres.
The total population of Inuit children between three and five years of age in the communities surveyed was 1487, representing 77% of three- to five-year-old Inuit children in Nunavut. Our sample size per community ranged from 12 to 35.
Results
Of 537 households we contacted that had three- to five-year-olds, 75 declined to participate when initially contacted, and 74 cancelled or failed to attend their scheduled visit at the survey clinic. The rate of participation was thus 72.3% (i.e., 388 participants), representing 26% of Inuit three- to five-year-olds in the 16 communities surveyed. We obtained information on food security for 374 (96.4%) of the 388 children. Parents of the remaining 14 children were not able to stay for the full duration of the interview session.
A total of 184 boys and 204 girls participated. The majority of the primary caregivers we interviewed were either biological (68.4%) or adoptive parents (21.6%). The weighted age of participating children was 4.4 years (95% CI 4.3~4.4). We observed a high prevalence of obesity (28.0%) and overweight (39.3%) among participating children. We also observed a high prevalence of public housing, income support, crowding and homes in need of major repairs. Daily contact with extended family and participation in traditional food-sharing networks were highly prevalent (Table 2).
Table 2.
Prevalence of demographic characteristics, body weight and food insecurity among participants
| Characteristic | Prevalence,* % (95% CI) |
|---|---|
| Demographics | |
| Public housing | 69.7 (64.8–74.6) |
| Income support — any household member | 42.7 (37.5–47.9) |
| Home in need of major repairs | 37.0 (31.7–42.3) |
| No. of people in home | 5.9 (5.7–6.1) |
| Crowding† | 53.9 (48.6–59.3) |
| Children to adults, 19–64 y in home (ratio) | 1.6 (1.5–1.7) |
| Weekly cost for groceries, Can$ | 428.5 (399.2–457.7) |
| Consumed traditional food in the past day | 44.2 (38.9–49.6) |
| Daily contact with extended family | 69.7 (64.7–74.7) |
| Received traditional food from sharing networks in the past year | 75.6 (71.0–80.1) |
| Distributed traditional food | 81.2 (76.8–85.5) |
| Body weight | |
| Overweight | 39.3 (33.9–44.7) |
| Obese | 28.0 (23.1–33.0) |
| Overall household food security‡ | |
| Food secure | 30.4 (25.4–35.4) |
| Food insecure | 69.6 (64.7–74.6) |
| Moderately | 35.3 (30.1–40.5) |
| Severely | 34.4 (29.2–39.5) |
| Child food security | |
| Food secure | 43.9 (38.7–49.0) |
| Food insecure | 56.1 (51.0–61.3) |
| Moderately | 31.0 (26.1–35.9) |
| Severely | 25.1 (20.4–29.9) |
Note: CI = confidence interval.
Data were weighted to the total number of Inuit children aged three to five years in each community.
Defined as more than one person per room where rooms are defined as bedrooms, kitchen or living room.
Determined by combining data for adult-specific food security (data not shown) and data for child-specific food security.
The weighted prevalence of three- to five-year-olds living in households that were moderately food insecure was 35.3%, and in households that were severely food insecure, it was 34.4%. The proportion of three- to five-year-olds living in households that were food insecure was thus 69.6% (95% CI 64.7%–74.6%). In the category of child-specific food insecurity, 31.0% of three- to five-year-olds lived in homes that were moderately food insecure and 25.1% lived in homes that were severely food insecure. The weighted prevalence of child food insecurity was thus 56.1% (95% CI 51.0%–61.3%) (Table 2).
Among all respondents, 15.3% (95% CI 11.3%–19.2%) gave affirmative responses (i.e., often, sometimes or yes) to the question, “In the last 12 months, did your children ever not eat for a whole day because there wasn’t enough money for food?” Among respondents from homes rated as having severe child food insecurity, 60.1% (95% CI 49.5%–70.7%) answered this question affirmatively. When asked “In the last 12 months, were the children ever hungry but you just couldn’t afford more food?” 25.6% (95% CI 20.9%–30.4%) of all respondents and 90.4% (95% CI 84.3%–96.5%) of respondents from homes with severe child food insecurity answered affirmatively. The weighted prevalence of affirmative answers to the question of whether children ever skipped meals was 20.3% among all respondents and 75.8% among respondents from homes with severe child food insecurity.
Responses from homes with moderate child food insecurity indicated a high prevalence of worry that food will run out, times when children were fed less expensive foods, times when it was not possible to feed children a healthy meal and times when children were not eating enough because there was no money to buy enough food (Table 1).
Interpretation
We observed a high prevalence of food insecurity among homes with preschoolers in Nunavut, with nearly 70% of children residing in homes with household food insecurity and 56% residing in households with child food insecurity. By contrast, the Canadian Community Health Survey, Cycle 2.2, found that 9.2% of Canadian households, 5.2% of Canadian households with children, and 33.3% of off-reserve Aboriginal households experienced food insecurity in 2004, based on the same 18-item scale and classification system we used in our study.11
Based on responses to three questions in the National Population Health Survey of 1998–1999 by Statistics Canada, 10% of Canadians were living in households identified as food insecure during the survey period.14 Based on responses to three similar questions in the Canadian Community Health Survey, Cycle 1.1, 21% of households in the Yukon Territory, 28% of those in the Northwest Territories and 56% of those in Nunavut were classified as food insecure.5 By contrast, 83% of homes in Kugaaruk, Nunavut, and 40% of homes in Kangiqsujuaq, Nunavik, were identified as food insecure in studies conducted by Indian and Northern Affairs Canada using the modified 18-item Household Food Security Survey Module.6,7
The higher prevalence of household food insecurity compared with child food insecurity in our study has been observed in populations in which adults tend to modify their dietary intakes in order to protect children in food insecure households.15–17
We observed a high degree of daily contact with extended family and participation during the previous year in traditional food-sharing networks among participants. Such support systems may, to some degree, help families with young children cope with shortages in access to market foods. Traditional foods are rich in nutrients, contribute to higher dietary quality and can promote good health in Inuit communities.18–21
We observed a high prevalence of food insecurity in a population at risk for overweight and obesity. Overweight and obesity have been found by several studies3,22–24 to be related to food insecurity. Their prevalence may reflect poor overall dietary quality caused by the ready availability and common consumption of energy-dense and highly processed foods in the Arctic.20,21
Limitations
The questions related to food security in our survey were specific to whether participants had the financial means to buy groceries and did not cover access to traditional indigenous food-related systems. Given this limitation, further investigation is needed in which the availability of traditional foods is also evaluated to determine overall food security status among indigenous peoples in Canada.25–27
Conclusion
Food insecurity is all too prevalent in homes with Inuit preschoolers in Canadian Arctic communities. Our data suggest that support systems need to be strengthened for Inuit families with young children.
Acknowledgements
For guidance throughout the project, the authors thank the members of the Steering Committee of the Nunavut Inuit Health Survey (the Nunavut Association of Municipalities, Nunavut Tunngavik Inc., Government of Nunavut Department of Health and Social Services, the University of Toronto and the Centre for Indigenous Peoples’ Nutrition and Environment of McGill University).
Footnotes
Previously published at www.cmaj.ca
See related research article by Luo and colleagues, page 235, and related commentary by Cunningham, page 228
Competing interests: None declared.
Contributors: Grace Egeland was principal investigator of the International Polar Year Inuit Health Survey; she interpreted the results of the survey and drafted the manuscript. Grace Egeland and Isaac Sobol guided the content and design of the survey. Zhirong Cao was involved in the analysis of the data. Angela Pacey facilitated the collection of field data and conducted background research. Angela Pacey, Zhirong Cao and Isaac Sobol critically reviewed the manuscript for important intellectual content. All of the authors approved the final version of the manuscript submitted for publication.
Funding: Financial support for this study was provided by the Government of Canada Program for International Polar Year, the Canadian Institute for Health Research, Health Canada, and Indian and Northern Affairs Canada.
This article has been peer reviewed.
REFERENCES
- 1.Agricultural and Agri-Food Canada. Canada’s action plan for food security: a response to the World Food Summit. Ottawa (ON): The Department; 1998. [(accessed 2010 Jan. 5)]. Available: www.agr.gc.ca/index_e.php?s1=misb&s2=fsec-seca&page=action. [Google Scholar]
- 2.Vozoris NT, Tarasuk VS. Household food insufficiency is associated with poorer health. J Nutr. 2003;133:120–6. doi: 10.1093/jn/133.1.120. [DOI] [PubMed] [Google Scholar]
- 3.Alaimo K, Olson CM, Frongillo EA., Jr Food insufficiency and American school-aged children’s cognitive, academic, and psychosocial development. Pediatrics. 2001;108:44–53. [PubMed] [Google Scholar]
- 4.Jyoti DF, Fronqillo EA, Jones SJ. Food insecurity affects school children’s academic performance, weight gain and social skills. J Nutr. 2005;135:2831–9. doi: 10.1093/jn/135.12.2831. [DOI] [PubMed] [Google Scholar]
- 5.Ledrou I, Gervais J. Food insecurity. Health Rep. 2005;16:47–51. [PubMed] [Google Scholar]
- 6.Indian and Northern Affairs Canada. Nutrition and food security in Kangiqsujuaq, Nunavik. Ottawa (ON): The Department; 2004. [Google Scholar]
- 7.Indian and Northern Affairs Canada. Nutrition and food security in Kugaaruk, Nunavut: baseline survey for the Food Mail Pilot Project. Ottawa (ON): The Department; 2003. [Google Scholar]
- 8.Indian and Northern Affairs Canada. The revised northern food basket. Ottawa (ON): The Department; 2007. [(accessed 2009 Nov. 25)]. Available: www.ainc-inac.gc.ca/nth/fon/fc/pubs/nfb/nfb-eng.pdf. [Google Scholar]
- 9.Bickel G, Nord M, Price C, et al. Guide to measuring household food security, revised 2000. Alexandria (VA): Food and Nutrition Service, United States Department of Agriculture; 2000. [(accessed 2009 Nov. 25)]. Available: www.fns.usda.gov/fsec/files/fsguide.pdf. [Google Scholar]
- 10.Nord M, Andrews M, Carlson S. Household food security in the United States, 2005. Economic research report No. 29. Washington (DC): Economic Research Service, United States Department of Agriculture; 2006. [(accessed 2009 Nov. 25)]. Available: www.fns.usda.gov/fsec/files/fsguide.pdf. [Google Scholar]
- 11.Office of Nutrition Policy and Promotion. Canadian Community Health Survey Cycle 2.2, Nutrition (2004). Income-related household food security in Canada. Ottawa (ON): Health Canada; 2007. [Google Scholar]
- 12.Nord M, Hopwood HA. Comparison of household food security in Canada and the United States. Appendix A: Food security classification used by Health Canada. Washington (DC): United States Department of Agriculture Economic Research Service, economic research report (ERR) 67; 2008. [(accessed 2009 May 20)]. Available: www.ers.usda.gov/Publications/ERR67/ERR67.pdf. [Google Scholar]
- 13.Cole TJ, Bellizi MC, Flegal KM, et al. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Che J, Chen J. Food insecurity in Canadian households. Health Rep. 2001;12:11–22. [PubMed] [Google Scholar]
- 15.McIntyre L, Connor SK, Warren JW. Child hunger in Canada: results of the 1994 national longitudinal survey of children and youth. CMAJ. 2000;163:961–5. [PMC free article] [PubMed] [Google Scholar]
- 16.McIntyre L, Glanville NT, Raine KD, et al. Do low-income lone mothers compromise their nutrition to feed their children? CMAJ. 2003;168:686–91. [PMC free article] [PubMed] [Google Scholar]
- 17.Cristofar SP, Basiotis PP. Dietary intakes and selected characteristics of women ages 19–50 years and their children ages 1–5 years by reported perception of food sufficiency. J Nutr Educ. 1992;24:53–8. [Google Scholar]
- 18.Kuhnlein HV, Receveur O. Local cultural animal food contributes high levels of nutrients for Arctic Canadian Indigenous adults and children. J Nutr. 2007;137:1110–4. doi: 10.1093/jn/137.4.1110. [DOI] [PubMed] [Google Scholar]
- 19.Egeland GM, Berti P, Soueida R, et al. Age differences in vitamin A intake among Canadian Inuit. Can J Public Health. 2004;95:465–9. doi: 10.1007/BF03403995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuhnlein HV, Receveur O, Soueida R, et al. Arctic indigenous peoples experience the nutrition transition with changing dietary patterns and obesity. J Nutr. 2004;134:1447–53. doi: 10.1093/jn/134.6.1447. [DOI] [PubMed] [Google Scholar]
- 21.Egeland GM, Charbonneau-Roberts G, Kuluguqtuq J, et al. Back to the future —using traditional food and knowledge to promote a healthy future among Inuit. In: Kuhnlein HV, Erasmus B, Spigelski D, editors. Indigenous peoples’ food systems: the many dimensions of culture, diversity, environment and health. New York (NY): Food and Agriculture Organization of the United Nations; 2009. [Google Scholar]
- 22.Gundersen C, Lohman BJ, Garasky S, et al. Food security, maternal stressors, and overweight among low-income us children: results from the national health and nutrition examination survey (1999–2002) Pediatrics. 2008;122:e529–e40. doi: 10.1542/peds.2008-0556. [DOI] [PubMed] [Google Scholar]
- 23.Rose D, Bodor JN. Household food insecurity and overweight status in young school children: results from the early childhood longitudinal study. Pediatrics. 2006;117:464–73. doi: 10.1542/peds.2005-0582. [DOI] [PubMed] [Google Scholar]
- 24.Casey PH, Simpson PM, Gossett JM, et al. The association of child and household food insecurity with childhood overweight status. Pediatrics. 2006;118:e1406–13.25. doi: 10.1542/peds.2006-0097. [DOI] [PubMed] [Google Scholar]
- 25.Lambden J, Receveur O, Kuhnlein HV. Traditional food attributes must be included in studies of food security in the Canadian Arctic. Int J Circumpolar Health. 2007;66:308–19. doi: 10.3402/ijch.v66i4.18272. [DOI] [PubMed] [Google Scholar]
- 26.Power EM. Conceptualizing food security for aboriginal people in Canada. Can J Public Health. 2008;99:95–7. doi: 10.1007/BF03405452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chan HM, Fediuk K, Hamilton S, et al. Food security in Nunavut, Canada: barriers and recommendations. Int J Circumpolar Health. 2006;65:416–31. doi: 10.3402/ijch.v65i5.18132. [DOI] [PubMed] [Google Scholar]