Abstract
Self-reported experiences of “everyday” discrimination have been linked to indices of cardiovascular disease and overall mortality and findings have been particularly pronounced for African-American populations. However, the biological mechanisms underlying these associations remain unclear. C-Reactive Protein (CRP), a marker of inflammation, is a known correlate of cardiovascular and other health outcomes and has also been linked to several psychosocial processes. To our knowledge, no studies have examined the association between experiences of discrimination and CRP. We examined the cross-sectional association between self-reported experiences of discrimination and CRP in a sample of 296 older African-American adults (70% female, Mean age= 73.1). Experiences of discrimination were assessed with the 9-item Everyday Discrimination Scale and CRP was assayed from blood samples. In linear regression models adjusted for age, sex and education, experiences of discrimination were associated with higher levels of CRP (B=.10, p=.03). This association remained significant after additional adjustments for depressive symptoms (B=.10, p=.04), smoking, and chronic health conditions (heart disease, diabetes, hypertension) that might influence inflammation (B=.11, p=.02). However, results were attenuated when Body Mass Index (BMI) was added to the model (B=.09, p=.07). In conclusion, self-reported experiences of everyday discrimination are associated with higher levels of CRP in older African-American adults, although this association is not completely independent of BMI.
Keywords: Discrimination (psychology), C-Reactive Protein, African-Americans, aging, prejudice
Background
Self-reported experiences of “everyday” discrimination (i.e. fairly minor, day-to-day forms of interpersonal mistreatment) have been linked to a variety of different cardiovascular health outcomes, including elevated blood pressure (Guyll et al., 2001; Lewis et al., 2009; Roberts et al., 2008), early signs of atherosclerosis (Lewis et al., 2006; Troxel et al., 2003), and all-cause mortality (Barnes et al., 2008). In contrast to acute, one-time instances of discrimination, “everyday” experiences of discrimination are conceptualized as chronic, ongoing stressors that may potentially have a more deleterious impact on cardiovascular health (Lewis et al., 2006). Findings linking everyday discrimination to cardiovascular health outcomes have often been more pronounced for African-Americans, compared with whites (Guyll et al., 2001; Lewis et al., 2009; Troxel et al., 2003), leading to some speculation that everyday experiences of discrimination may be a particularly relevant psychosocial risk factor for African-American populations (Lewis et al., 2009; Lewis et al., 2006). Despite the growing body of research in this area, however, little is known about potential biological pathways through which experiences of everyday discrimination might ultimately influence cardiovascular health in African-Americans.
C-reactive protein (CRP), a marker of systemic inflammation, is a known correlate of poor cardiovascular health outcomes (Cushman et al., 2005; Koenig et al., 1999; Ridker et al., 2000). Although other inflammatory markers (e.g. interleukin-6, tumor-necrosis factor-alpha) have been linked to cardiovascular endpoints (Brydon and Steptoe, 2005; Cesari et al., 2003; Owen and Steptoe, 2003; von Haehling et al., 2004), evidence has been particularly compelling for CRP (Ridker et al., 2000; Sesso et al., 2007; Willerson and Ridker, 2004). Further, research suggests that CRP may be a potentially “modifiable” cardiovascular risk factor (Mora et al., 2009; Ridker et al., 2008), thus it also has considerable clinical significance. Across studies, levels of CRP have been found to be consistently elevated in African-Americans, compared with whites (Albert et al., 2004; Gruenewald et al., 2009; Kelley-Hedgepeth et al., 2008; Khera et al., 2005). CRP has also been linked to a number of psychosocial processes, including depressive symptoms (Howren et al., 2009; Kop et al., 2002), hostility (Graham et al., 2006; Ranjit et al., 2007), and chronic stress (Ranjit et al., 2007). To our knowledge, however, no studies have examined the association between experiences of everyday discrimination and CRP.
The current study was designed to examine the association between everyday discrimination and CRP in a community-based sample of older African-American adults. We hypothesized that experiences of discrimination would be positively associated with levels of CRP. Further, given the previously documented associations between experiences of discrimination and depressive symptoms (Barnes et al., 2004; Schulz et al., 2006), and depressive symptoms and CRP (Howren et al., 2009), we also hypothesized that any associations between experiences of everyday discrimination and CRP would be partially mediated by depressive symptoms.
Methods
Participants
Participants were 296 older African-American adults from the Minority Aging Research Study (MARS), an ongoing, longitudinal epidemiologic cohort study of risk factors for cognitive decline in community-dwelling older African-Americans (Arvanitakis et al., 2009). MARS participants were recruited between August 2004 and April 2008 from churches, senior buildings and African-American social organizations in the greater Chicago, Illinois area. Eligible participants were individuals aged 65 and older without known dementia who self-identified as non-Hispanic African-American. Participants were included in these analyses if they had completed the baseline MARS evaluation and had serum available for measurement of CRP.
All aspects of this study were approved by the Institutional Review Board of Rush University Medical Center. All participants provided informed consent.
Procedures
As part of the MARS protocol, participants completed an in-home face-to-face interview and underwent uniform, structured clinical evaluations by a trained nurse practitioner that included a medical history, physical examination, detailed neuropsychological testing and blood specimen collection by a nurse or phlebotomist. Participants were asked to present prescription and non-prescription medication containers, which were visually inspected. Medication names and dosages were recorded using the Medi-Span system ®. Clinical data were collected on laptop computers, with forms programmed in Blaise, a Pascal-based data entry program (Statistics Netherlands, version 4.23).
Measures
“Everyday” Discrimination
Everyday discrimination was assessed with the Detroit Area Study Everyday Discrimination Scale (Williams et al., 1997). Based on a construct originally defined by Essed (Essed, 1990, 1991), this 9-item scale asks participants to indicate the frequency with which they experience various forms of interpersonal mistreatment in their day-to-day lives. Examples include “You are treated with less courtesy than other people”, “You receive poorer service than other people at restaurants or stores” and “People act as if they think you are not smart” (all items presented in Table 1). Items are framed in the context of general mistreatment, without reference to race, age, or gender. The frequency of each type of discrimination was assessed with a four-point scale (0=never, 1= rarely, 2= sometimes, 3= often). Following procedures established previously (Brown et al., 2006; Schulz et al., 2006), responses were recoded to a binary format (often or sometimes=1, rarely or never=0) and then summed across items to obtain a total score ranging from 0 to 9. This scale has been previously validated in older African-American adults and has been shown to have good internal consistency and validity (Barnes et al., 2004; Taylor et al., 2004). Chronbach’s alpha for the everyday discrimination scale in the MARS cohort was good (0.81).
Table 1.
Items on the Everyday Discrimination Scale
| 1. “You are treated with less courtesy than other people” |
| 2. “You are treated with less respect than other people” |
| 3. “You receive poorer service than other people at restaurants or stores” |
| 4. “People act as if they think you are not smart” |
| 5. “People act as if they are afraid of you” |
| 6. “People act as if they think you are dishonest” |
| 7. “People act as if they are better than you are” |
| 8. “You or your family members are called names or insulted” |
| 9. “You are threatened or harassed” |
Responses to each item are coded as “never/rarely” or “sometimes/often”.
Depressive symptoms
Depressive symptoms over the past week were assessed with the 10-item version of the Center for Epidemiological Studies Depression scale (CES-D) (Radloff, 1977). The CES-D has been widely used in both clinical and community samples (Breslau, 1985; Orme et al., 1986; Roberts, 1980), and has been validated in African-Americans (Williams et al., 2007). The shorter 10-item form was developed to reduce participant burden in older adults, and its correspondence to the original version has been previously established (Kohout et al., 1993). It has also been found to have good internal consistency and test-retest reliability in older adult samples (Irwin et al., 1999). Possible scores on this version of the CES-D range from 0 to 10, with higher scores indicating more depressive symptoms.
C-Reactive Protein (CRP)
Using sterile technique, phlebotomists and nurses skilled in venipuncture collected blood specimens in 2-ml EDTA tubes. The specimens were then spun for 10 minutes, aliquoted into 1.8cc nunc vials, and then placed on dry ice. They were then transported to the storage facility at the Rush Alzheimer’s Disease Center (RADC) where they were stored in a freezer at −80 degrees Celsius. CRP levels were quantified by Endogen Searchlight technologies (Bilerica, MA) using highly sensitive multiplexed sandwich enzyme-linked immunoabsorbent assay (ELISA) arrays designed to detect CRP along with several other inflammatory markers1. The multiplex ELISA arrays were tested for spotting consistency and specificity, to rule out the presence of cross reactivity or non-specific binding resulting from simultaneous testing of CRP along with other inflammatory antibodies. The lower detection limit for CRP was <0.6 mg/mL. Intra-assay coefficient of variability (CV) was 6.8–7.0% and inter-assay CV was 2.9–5.8%. CRP values were adjusted by a correction factor supplied by Searchlight Endogen, based on data obtained from recalibration studies.
Covariates
Several additional variables that might contribute to associations between everyday discrimination and CRP were also assessed. Demographic covariates included age, sex, and education (in years) and were assessed via self-report. Current cigarette smoking was ascertained via questionnaire (“Do you regularly smoke cigarettes now?”) and coded as yes/no. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared using standard protocols for older adults (Chumlea et al., 1986). BMI was categorized as normal (BMI ≤ 24.9), overweight (BMI 25–29.9) or obese (BMI ≥ 30) for descriptive purposes, but was modeled continuously in all analyses. Current hypertension and/or diabetes were rated as present if the participant reported having been diagnosed with the condition or was found to be on medication (based on visual inspection of medications) for the condition. History of vascular disease in the form of stroke, myocardial infarction, congestive heart failure, and claudication was assessed via clinical exam (for stroke only)2, and self-report. A vascular disease history summary score based on the number of these conditions present was created and modeled continuously, with a possible range of 0 to 4.
Statistical analyses
Descriptive statistics were used to characterize the sample on demographic, psychosocial, behavioral and disease status variables. We examined unadjusted associations between everyday discrimination and covariates of interest using Pearson correlations or analysis of variance tests (ANOVAs). The unadjusted association between everyday discrimination and CRP was presented graphically for descriptive purposes. Because the distribution of CRP was highly skewed, geometric mean CRP values were used in all descriptive analyses and log-transformed values were used in multivariate analyses. To examine the multivariate association between discrimination and CRP, we fit a series of cross-sectional linear regression models, modeling the logarithm of CRP as a function of everyday discrimination and potential confounders. Our primary model tested the association between discrimination and CRP, after adjusting for age, sex, and education. The second model added a term for depressive symptoms and in the third model we added additional variables to control for smoking, elevated blood pressure, diabetes and number of prior vascular diseases. Our final model added a term for BMI to the third model.
Because of the large number of women in the MARS cohort (all of whom were post-menopausal), and the potential link between hormone use and cardiovascular risk, we also considered adding use of hormone replacement therapy (HRT) as a covariate to our analyses. However, only 32% of women (N=66) in the sample reported HRT use. HRT use was not associated with reports of everyday discrimination (p=0.82), CRP (p=0.89), or CES-D scores (p=0.28) in bivariate analyses, thus we did not add it to our multivariate models.
Because one prior study of everyday discrimination and a less-widely studied marker of inflammation (E-selectin) in whites found stronger associations between everyday discrimination and inflammation in men compared with women (Friedman et al., 2009), we also ran a series of exploratory analyses to determine whether any observed associations between discrimination and CRP differed by sex. The initial exploratory model tested the association between the discrimination by sex interaction and CRP after adjusting for age, education, sex and discrimination. In the second exploratory model, we added additional terms for control variables as described in our second and third models above. Our final exploratory model added a term for BMI. All non-significant interaction terms were dropped from our final models. All analyses were conducted using SAS© software, Version 9.1.3 (2004).
Results
Sample characteristics are presented in Table 2. Participants were 73 years of age (SD=6.3) on average, with approximately 14.5 years of education (SD=3.6). The sample was predominantly female (71%). Twenty-six percent of participants in the sample were normal weight, 30% were overweight and 43.3% were obese. The average BMI was in the overweight range, at 29.4 (SD=5.9). Participants were fairly healthy; the number of prior vascular diseases ranged from 0 to 3 with a mean of less than one, and very few participants smoked. The majority of participants reported having hypertension, and approximately 20% reported having diabetes. The median CRP value was 1.0 mg/L and the interquartile range was .24 to 3.09, with a geometric mean value of 0.84 (SD= 5.52). The average score on the everyday discrimination scale was 1.82 (SD=2.1). Reports of everyday discrimination were positively associated with depressive symptoms (p=0.01) and number of prior vascular diseases (p=0.001), but were not associated with age, sex, education, smoking, high blood pressure or diabetes (all p-values >0.19). Reports of discrimination were not significantly correlated with BMI measured continuously (p=.22); nor did reports of discrimination significantly differ by normal, overweight or obese status (p=.49).
Table 2.
Participant Characteristics, N=296
| Age, mean (SD) | 73.1 (6.3) |
| Education, mean (SD) | 14.5 (3.6) |
| % Female | 71 |
| Discrimination, mean (SD) | 1.8 (2.1) |
| Depressive symptoms, mean (SD) | 1.16 (1.53) |
| % Current Smoker | 7.2 |
| Body Mass Index (SD) | 29.4 (5.9) |
| % with Diabetes | 21 |
| % with High Blood Pressure | 71 |
| History of Vascular Disease | 0.55 (0.24) |
| CRP (mg/L), geometric mean (SD) | 0.84 (5.52) |
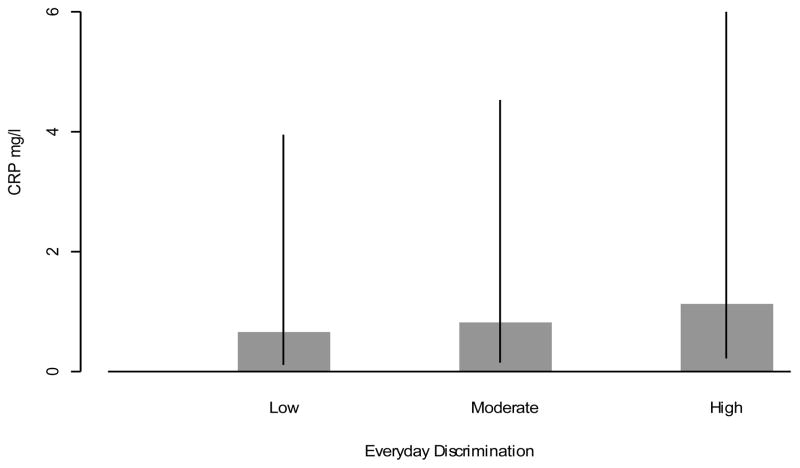
The unadjusted association between everyday discrimination and CRP is graphically illustrated in Figure 1, with everyday discrimination scores categorized into approximate tertiles (low, moderate and high) for descriptive purposes. As can be seen in Figure 1, there was considerable variability within each category of discrimination (as evidenced by the relatively wide confidence intervals); yet there was a clear dose-response relationship between experiences of everyday discrimination and CRP, where each higher level of everyday discrimination was associated with a greater amount of CRP (Figure 1).
Figure 1.
Geometric Mean levels of CRP and associated confidence intervals by approximate tertiles of Everyday Discrimination
There was a significant association between experiences of everyday discrimination and CRP in multivariate linear regression models adjusted for age, sex and education (B=0.10, t(291)=2.12, p=0.03). This association was largely unchanged after adjusting for depressive symptoms (B=0.10, t(290)=2.10, p=0.04). The association between everyday discrimination and CRP remained significant after additional adjustments for smoking, number of prior vascular diseases, high blood pressure and diabetes (B=0.11, t(286)=2.3, p=0.02). However, adding BMI to the multivariate models slightly attenuated the relationship between everyday discrimination and CRP, although it remained marginally significant (B=0.09, t(281)=1.84, p=0.07).
In exploratory multivariate regression models examining the interaction between everyday discrimination and sex, the everyday discrimination by sex interaction term was non-significant (B=0.15, t(290)=1.52, p=0.13) after adjusting for age, education, sex and discrimination. The interaction term remained non-significant in exploratory analyses after additional adjustments for risk factors and BMI (data not shown).
Discussion
The current study examined the cross-sectional association between self-reported experiences of everyday discrimination and CRP in a sample of older African-American adults. Consistent with prior studies of CRP in older adults, we observed considerable variability in CRP levels (Macy et al., 1997; Ockene et al., 2001), that was apparent across the range of discrimination scores in our cohort. Nonetheless, our findings revealed a significant, dose-response association between everyday discrimination and CRP, where more experiences of discrimination were associated with higher levels of CRP. The association between everyday discrimination and CRP was not explained by depressive symptoms, and was also independent of a number of cardiovascular risk factors previously shown to be associated with everyday discrimination, such as smoking and elevated blood pressure (Guthrie et al., 2002; Guyll et al., 2001; Lewis et al., 2009).
The observed association between everyday discrimination and CRP in our cohort was partially, but not fully, independent of BMI. Across studies, BMI is a strong correlate of CRP (Barinas-Mitchell et al., 2001; Gruenewald et al., 2009; Rexrode et al., 2003; Visser et al., 1999). Findings linking discrimination to BMI, on the other hand, have been mixed. Although it is commonly assumed that experiences of discrimination are significantly associated with BMI (primarily due to discrimination against the overweight and obese, (Andreyeva et al., 2008)), findings in African-American populations have not completely supported this notion (Hebl and Heatherton, 1998), with one study reporting a positive association (Cozier et al., 2009) and another reporting a null association (Hunte and Williams, 2009). Consistent with national data for African-Americans over age 60 (Ogden et al., 2006), participants in the MARS cohort had BMIs that were, on average, in the overweight and obese range. However, neither BMI nor overweight/obese status were significantly associated with reports of discrimination in this cohort. Consequently it is difficult to conceptualize BMI as a mediator, or potential pathway, through which everyday discrimination might impact CRP. Indeed, the estimate of the association between everyday discrimination and CRP remained largely unchanged by the addition of BMI, although the p-value was reduced to marginal significance.
Researchers have only recently begun to systematically explore associations between discriminatory treatment and health outcomes (Pascoe and Richman, 2009; Sloan et al., 2009; Williams and Mohammed, 2009), thus few pathways have been identified that might explain our observed association between everyday discrimination and CRP. Dsyregulation of the hypothalamic-pituatary-adrenal (HPA) axis and low heart rate variability (HRV) have both been identified as possible correlates of elevated levels of CRP (Black, 2002; Lampert et al., 2008), as well as a variety of chronic and interpersonal stressors (Horsten et al., 1999; Miller et al., 2007). Thus, it is reasonable to assume that these are two potential pathways through which everyday discrimination might have influenced levels of CRP in our cohort. To our knowledge, however, these pathways have yet to be examined in relation to everyday discrimination or other forms of discriminatory treatment. Additional research in this area is warranted.
In contrast to a previous report of everyday discrimination and E-selectin in whites (Friedman et al., 2009), associations between everyday discrimination and CRP in our cohort of African-Americans did not differ by sex. African-American men and women reported comparable levels of everyday discrimination and our exploratory analyses found that the effects of discriminatory experiences on CRP were similar for African-American women and men. We had a relatively small number of African-American men relative to women, however, and the power to detect sex differences in our observed association may have been low. It is also possible that sex differences are less apparent in African-Americans because as a group, African-Americans report more exposure to discriminatory treatment in the United States compared to whites (Kessler et al., 1999), regardless of sex.
To our knowledge, this is the first study to examine associations between everyday discrimination and CRP. We are aware of one prior study that examined associations between racial/ethnic mistreatment more specifically (i.e. “Have you ever been mistreated because of your race/ethnicity) and CRP and found no association (Albert et al., 2008); suggesting that perceptions of racism per se may not be associated with higher levels of CRP. Because we did not ask specifically about the attribution, or primary reason, for experiences of mistreatment, it is unclear whether the older African-American adults in our cohort are reporting discriminatory treatment as a result of their race, age, or some other attribute. Prior research in this area has been mixed (Guyll et al., 2001; Lewis et al., 2006; Roberts et al., 2008; Troxel et al., 2003). Two studies have found that the attribution for everyday discrimination is not significantly associated with cardiovascular health outcomes in African-Americans (Lewis et al., 2006; Troxel et al., 2003), suggesting that the experiences themselves matter more than what they are attributed to. However, two other studies found that the attribution does matter (Guyll et al., 2001; Roberts et al., 2008), but in one study, attributing discrimination to race/ethnicity was associated with the poorest cardiovascular outcomes in African-Americans (Guyll et al., 2001), while in the other study non-racial attributions were most strongly associated with poor cardiovascular health in African-Americans (Roberts et al., 2008). Interestingly, in all but one of these studies, the association between everyday discrimination and indices of cardiovascular health was also examined in whites (Guyll et al., 2001; Lewis et al., 2006; Troxel et al., 2003), and no associations were found. Taken together, these findings suggest that everyday discrimination may be an important correlate of cardiovascular health for African-American populations, but attributing experiences of discrimination to race/ethnicity may not.
Our study findings should be interpreted in the context of several limitations. To begin with, the observed associations were cross-sectional in nature. Additional research is needed to determine whether experiences of everyday discrimination are associated with increases in CRP over time. A second limitation of the current study is the age of our cohort; the MARS sample is comprised of older adults and it is unclear whether or not findings would generalize to younger populations. Finally, because the MARS study was limited to African-Americans, we do not know whether our findings would extend to other racial/ethnic groups.
Despite these limitations, our study has several strenghts. By focusing on African-Americans, we were able to thoroughly examine a relevant construct (i.e. “everyday” discrimination) in an at-risk group that is disproportionately exposed to these experiences. Older African-Americans in particular are an important sub-population to consider in studies of discrimination and health because these individuals came of age prior to the United States Civil Rights movement, at a time when discriminatory treatment against African-Americans was fairly widespread and legally sanctioned (Klarman, 2004). We were also able to explore within-group differences by examining whether associations differed for African-American men compared to African-American women. Another major strength of our study is the fact that our sample is community-based, rather than laboratory or clinic-based; this increases our ecological validity and overall generalizability to the population we are studying. Finally, we used a well-validated measure of discrimination and controlled for a number of relevant risk factors in our analyses.
To our knowledge, this study is the first to provide evidence linking experiences of everyday discrimination to higher levels of CRP. Although the mechanisms underlying the observed associations have yet to be determined, these findings elucidate one potential pathway through which experiences of everyday discrimination might ultimately influence poor cardiovascular health. Because our sample was limited to older African-American adults, additional research is needed to determine whether these findings extend to younger cohorts and other racial/ethnic groups.
Acknowledgments
The Minority Aging Study (MARS) has grant support from the National Institutes of Health (NIH), National Institute on Aging (NIA), R01 AG22018 and Investigator Initiated Research Grant 07-59818 from the Alzheimer’s Association. Dr. Lewis was supported by the National Heart, Lung and Blood Institute (NHLBI) Grant K01HL 092591. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the NIA, NHLBI, the NIH or the Alzheimer’s Association.
Footnotes
These were novel markers for Alzheimer’s disease and cognitive decline that were assessed as part of the core MARS protocol and for conceptual reasons were not included in the current analyses. The current analyses focused on CRP because of its strong correlation with cardiovascular outcomes and potential role as a modifiable cardiovascular risk factor.
Stroke was assessed more comprehensively than other forms of vascular disease because it is a major risk factor for cognitive decline/Alzheimer’s disease, the primary focus of the MARS study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Albert MA, Glynn RJ, Buring J, Ridker PM. C-reactive protein levels among women of various ethnic groups living in the United States - (from the Women’s Health Study) Am J Cardiol. 2004;93:1238–1242. doi: 10.1016/j.amjcard.2004.01.067. [DOI] [PubMed] [Google Scholar]
- Albert MA, Ravenell J, Glynn RJ, Khera A, Halevy N, de Lemos JA. Cardiovascular risk indicators and perceived race/ethnic discrimination in the Dallas Heart Study. Am Heart J. 2008;156:1103–1109. doi: 10.1016/j.ahj.2008.07.027. [DOI] [PubMed] [Google Scholar]
- Andreyeva T, Puhl RM, Brownell KD. Changes in Perceived Weight Discrimination Among Americans, 1995–1996 Through 2004–2006. Obesity. 2008;16:1129–1134. doi: 10.1038/oby.2008.35. [DOI] [PubMed] [Google Scholar]
- Arvanitakis Z, Bennett DA, Wilson RS, Barnes LL. Diabetes and Cognitive Systems in Older Black and White Persons. Alzheimer Disease & Associated Disorders Publish Ahead of Print. 2009 doi: 10.1097/WAD.1090b1013e3181a1096bed1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barinas-Mitchell E, Cushman M, Meilahn EN, Tracy RP, Kuller LH. Serum levels of C-reactive protein are associated with obesity, weight gain, and hormone replacement therapy in healthy postmenopausal women. American Journal of Epidemiology. 2001;153:1094–1101. doi: 10.1093/aje/153.11.1094. [DOI] [PubMed] [Google Scholar]
- Barnes LL, de Leon CFM, Lewis TT, Bienias JL, Wilson RS, Evans DA. Perceived Discrimination and Mortality in a Population-Based Study of Older Adults. Am J Public Health. 2008;98:1241–1247. doi: 10.2105/AJPH.2007.114397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes LL, Mendes De Leon CF, Wilson RS, Bienias JL, Bennett DA, Evans DA. Racial differences in perceived discrimination in a community population of older blacks and whites. J Aging Health. 2004;16:315–337. doi: 10.1177/0898264304264202. [DOI] [PubMed] [Google Scholar]
- Black PH. Stress and the inflammatory response: A review of neurogenic inflammation. Brain, Behavior, and Immunity. 2002;16:622–653. doi: 10.1016/s0889-1591(02)00021-1. [DOI] [PubMed] [Google Scholar]
- Breslau N. Depressive symptoms, major depression, and generalized anxiety: a comparison of self-reports on CES-D and results from diagnostic interviews. Psychiatry Res. 1985;15:219–229. doi: 10.1016/0165-1781(85)90079-4. [DOI] [PubMed] [Google Scholar]
- Brown C, Matthews KA, Bromberger JT, Chang Y. The Relation between Perceived Unfair Treatment and Blood Pressure in a Racially/Ethnically Diverse Sample of Women. Am J Epidemiol. 2006;164:257–262. doi: 10.1093/aje/kwj196. [DOI] [PubMed] [Google Scholar]
- Brydon L, Steptoe A. Stress-induced increases in interleukin-6 and fibrinogen predict ambulatory blood pressure at 3-year follow-up. J Hypertens. 2005;23:1001–1007. doi: 10.1097/01.hjh.0000166841.57474.d0. [DOI] [PubMed] [Google Scholar]
- Cesari M, Penninx BWJH, Newman AB, Kritchevsky SB, Nicklas BJ, Sutton-Tyrrell K, Rubin SM, Ding J, Simonsick EM, Harris TB, Pahor M. Inflammatory Markers and Onset of Cardiovascular Events: Results From the Health ABC Study. Circulation. 2003;108:2317–2322. doi: 10.1161/01.CIR.0000097109.90783.FC. [DOI] [PubMed] [Google Scholar]
- Chumlea WC, Roche AF, Mukherjee D. Some anthropometric indices of body composition for elderly adults. J Gerontol. 1986;41:36–39. doi: 10.1093/geronj/41.1.36. [DOI] [PubMed] [Google Scholar]
- Cozier YC, Wise LA, Palmer JR, Rosenberg L. Perceived Racism in Relation to Weight Change in the Black Women’s Health Study. Annals of epidemiology. 2009;19:379–387. doi: 10.1016/j.annepidem.2009.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cushman M, Arnold AM, Psaty BM, Manolio TA, Kuller LH, Burke GL, Polak JF, Tracy RP. C-Reactive Protein and the 10-Year Incidence of Coronary Heart Disease in Older Men and Women: The Cardiovascular Health Study. Circulation. 2005;112:25–31. doi: 10.1161/CIRCULATIONAHA.104.504159. [DOI] [PubMed] [Google Scholar]
- Essed P. Everyday Racism: Reports from Women of Two Cultures. Hunter House, CA.: 1990. [Google Scholar]
- Essed P. Understanding Everyday Racism: An interdisciplinary theory. Sage Publications, Inc; Thousand Oaks, CA: 1991. [Google Scholar]
- Friedman EM, Williams DR, Singer BH, Ryff CD. Chronic discrimination predicts higher circulating levels of E-selectin in a national sample: the MIDUS study. Brain Behav Immun. 2009;23:684–692. doi: 10.1016/j.bbi.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham JE, Robles TF, Kiecolt-Glaser JK, Malarkey WB, Bissell MG, Glaser R. Hostility and pain are related to inflammation in older adults. Brain, Behavior, and Immunity. 2006;20:389–400. doi: 10.1016/j.bbi.2005.11.002. [DOI] [PubMed] [Google Scholar]
- Gruenewald TL, Cohen S, Matthews KA, Tracy R, Seeman TE. Association of socioeconomic status with inflammation markers in black and white men and women in the Coronary Artery Risk Development in Young Adults (CARDIA) study. Social Science & Medicine. 2009;69:451–459. doi: 10.1016/j.socscimed.2009.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guthrie BJ, Young AM, Williams DR, Boyd CJ, Kintner EK. African American girls’ smoking habits and day-to-day experiences with racial discrimination. Nurs Res. 2002;51:183–190. doi: 10.1097/00006199-200205000-00007. [DOI] [PubMed] [Google Scholar]
- Guyll M, Matthews KA, Bromberger JT. Discrimination and unfair treatment: relationship to cardiovascular reactivity among African American and European American women. Health Psychol. 2001;20:315–325. doi: 10.1037//0278-6133.20.5.315. [DOI] [PubMed] [Google Scholar]
- Hebl MR, Heatherton TF. The Stigma of Obesity in Women: The Difference is Black and White. Pers Soc Psychol Bull. 1998;24:417–426. [Google Scholar]
- Horsten M, Ericson M, Perski A, Wamala SP, Schenck-Gustafsson K, Orth-Gomer K. Psychosocial Factors and Heart Rate Variability in Healthy Women. Psychosom Med. 1999;61:49–57. doi: 10.1097/00006842-199901000-00009. [DOI] [PubMed] [Google Scholar]
- Howren MB, Lamkin DM, Suls J. Associations of Depression With C-Reactive Protein, IL-1, and IL-6: A Meta-Analysis. Psychosom Med. 2009;71:171–186. doi: 10.1097/PSY.0b013e3181907c1b. [DOI] [PubMed] [Google Scholar]
- Hunte HE, Williams DR. The association between perceived discrimination and obesity in a population-based multiracial and multiethnic adult sample. Am J Public Health. 2009;99:1285–1292. doi: 10.2105/AJPH.2007.128090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin M, Artin KH, Oxman MN. Screening for Depression in the Older Adult: Criterion Validity of the 10-Item Center for Epidemiological Studies Depression Scale (CES-D) Arch Intern Med. 1999;159:1701–1704. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- Kelley-Hedgepeth A, Lloyd-Jones DM, Colvin A, Matthews KA, Johnston J, Sowers MR, Sternfeld B, Pasternak RC, Chae CU for the SI. Ethnic Differences in C-Reactive Protein Concentrations. Clin Chem. 2008;54:1027–1037. doi: 10.1373/clinchem.2007.098996. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40:208–230. [PubMed] [Google Scholar]
- Khera A, McGuire DK, Murphy SA, Stanek HG, Das SR, Vongpatanasin W, Wians FH, Jr, Grundy SM, de Lemos JA. Race and Gender Differences in C-Reactive Protein Levels. Journal of the American College of Cardiology. 2005;46:464–469. doi: 10.1016/j.jacc.2005.04.051. [DOI] [PubMed] [Google Scholar]
- Klarman MJ. From Jim Crow to Civil Rights: The Supreme Court and the Struggle for Racial Equality. Oxford University Press; 2004. [Google Scholar]
- Koenig W, Sund M, Frohlich M, Fischer HG, Lowel H, Doring A, Hutchinson WL, Pepys MB. C-Reactive Protein, a Sensitive Marker of Inflammation, Predicts Future Risk of Coronary Heart Disease in Initially Healthy Middle-Aged Men: Results From the MONICA (Monitoring Trends and Determinants in Cardiovascular Disease) Augsburg Cohort Study, 1984 to 1992. Circulation. 1999;99:237–242. doi: 10.1161/01.cir.99.2.237. [DOI] [PubMed] [Google Scholar]
- Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993;5:179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- Kop WJ, Gottdiener JS, Tangen CM, Fried LP, McBurnie MA, Walston J, Newman A, Hirsch C, Tracy RP. Inflammation and coagulation factors in persons >65 years of age with symptoms of depression but without evidence of myocardial ischemia. The American Journal of Cardiology. 2002;89:419–424. doi: 10.1016/s0002-9149(01)02264-0. [DOI] [PubMed] [Google Scholar]
- Lampert R, Bremner JD, Su S, Miller A, Lee F, Cheema F, Goldberg J, Vaccarino V. Decreased heart rate variability is associated with higher levels of inflammation in middle-aged men. Am Heart J. 2008;156(759):e751–757. doi: 10.1016/j.ahj.2008.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Barnes LL, Bienias JL, Lackland DT, Evans DA, Mendes de Leon CF. Perceived Discrimination and Blood Pressure in Older African American and White Adults. J Gerontol A Biol Sci Med Sci. 2009;64A:1002–1008. doi: 10.1093/gerona/glp062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Everson-Rose SA, Powell LH, Matthews KA, Brown C, Karavolos K, Sutton-Tyrrell K, Jacobs E, Wesley D. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: the SWAN Heart Study. Psychosom Med. 2006;68:362–368. doi: 10.1097/01.psy.0000221360.94700.16. [DOI] [PubMed] [Google Scholar]
- Macy EM, Hayes TE, Tracy RP. Variability in the measurement of C-reactive protein in healthy subjects: implications for reference intervals and epidemiological applications. Clin Chem. 1997;43:52–58. [PubMed] [Google Scholar]
- Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychological Bulletin. 2007;133:25–45. doi: 10.1037/0033-2909.133.1.25. [DOI] [PubMed] [Google Scholar]
- Mora S, Musunuru K, Blumenthal RS. The clinical utility of high-sensitivity C-reactive protein in cardiovascular disease and the potential implication of JUPITER on current practice guidelines. Clin Chem. 2009;55:219–228. doi: 10.1373/clinchem.2008.109728. [DOI] [PubMed] [Google Scholar]
- Ockene IS, Matthews CE, Rifai N, Ridker PM, Reed G, Stanek E. Variability and Classification Accuracy of Serial High-Sensitivity C-Reactive Protein Measurements in Healthy Adults. Clin Chem. 2001;47:444–450. [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Orme JG, Reis J, Herz EJ. Factorial and discriminant validity of the Center for Epidemiological Studies Depression (CES-D) scale. J Clin Psychol. 1986;42:28–33. doi: 10.1002/1097-4679(198601)42:1<28::aid-jclp2270420104>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- Owen N, Steptoe A. Natural killer cell and proinflammatory cytokine responses to mental stress: associations with heart rate and heart rate variability. Biol Psychol. 2003;63:101–115. doi: 10.1016/s0301-0511(03)00023-1. [DOI] [PubMed] [Google Scholar]
- Pascoe EA, Richman LS. Perceived Discrimination and Health: A Meta-Analytic Review. Psychological Bulletin. 2009;135:531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- Ranjit N, Diez-Roux AV, Shea S, Cushman M, Seeman T, Jackson SA, Ni H. Psychosocial Factors and Inflammation in the Multi-Ethnic Study of Atherosclerosis. Arch Intern Med. 2007;167:174–181. doi: 10.1001/archinte.167.2.174. [DOI] [PubMed] [Google Scholar]
- Rexrode KM, Pradhan A, Manson JE, Buring JE, Ridker PM. Relationship of total and abdominal adiposity with CRP and IL-6 in women. Annals of Epidemiology. 2003;13:674–682. doi: 10.1016/s1047-2797(03)00053-x. [DOI] [PubMed] [Google Scholar]
- Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM, Jr, Kastelein JJ, Koenig W, Libby P, Lorenzatti AJ, MacFadyen JG, Nordestgaard BG, Shepherd J, Willerson JT, Glynn RJ. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359:2195–2207. doi: 10.1056/NEJMoa0807646. [DOI] [PubMed] [Google Scholar]
- Ridker PM, Hennekens CH, Buring JE, Rifai N. C-Reactive Protein and Other Markers of Inflammation in the Prediction of Cardiovascular Disease in Women. N Engl J Med. 2000;342:836–843. doi: 10.1056/NEJM200003233421202. [DOI] [PubMed] [Google Scholar]
- Roberts CB, Vines AI, Kaufman JS, James SA. Cross-Sectional Association between Perceived Discrimination and Hypertension in African-American Men and Women: The Pitt County Study. Am J Epidemiol. 2008;167:624–632. doi: 10.1093/aje/kwm334. [DOI] [PubMed] [Google Scholar]
- Roberts RE. Reliability of the CES-D scale in different ethnic contexts. Psychiatry Research. 1980;2:125–134. doi: 10.1016/0165-1781(80)90069-4. [DOI] [PubMed] [Google Scholar]
- SAS. SAS Institute, Inc; Cary, NC.: 2004. [Google Scholar]
- Schulz AJ, Israel BA, Gravlee CC, Mentz G, Williams DR, Rowe Z. Discrimination, Symptoms of Depression, and Self-Rated Health Among African American Women in Detroit: Results From a Longitudinal Analysis. American Journal of Public Health. 2006;96:1265–1270. doi: 10.2105/AJPH.2005.064543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sesso HD, Wang L, Buring JE, Ridker PM, Gaziano JM. Comparison of Interleukin-6 and C-Reactive Protein for the Risk of Developing Hypertension in Women. Hypertension. 2007;49:304–310. doi: 10.1161/01.HYP.0000252664.24294.ff. [DOI] [PubMed] [Google Scholar]
- Sloan RP, Shapiro PA, DeMeersman RE, Bagiella E, Brondolo EN, McKinley PS, Slavov I, Fang Y, Myers MM. The effect of aerobic training and cardiac autonomic regulation in young adults. Am J Public Health. 2009;99:921–928. doi: 10.2105/AJPH.2007.133165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor TR, Kamarck TW, Shiffman S. Validation of the Detroit Area Study Discrimination Scale in a community sample of older African American adults: the Pittsburgh healthy heart project. Int J Behav Med. 2004;11:88–94. doi: 10.1207/s15327558ijbm1102_4. [DOI] [PubMed] [Google Scholar]
- Troxel WM, Matthews KA, Bromberger JT, Sutton-Tyrrell K. Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychol. 2003;22:300–309. doi: 10.1037/0278-6133.22.3.300. [DOI] [PubMed] [Google Scholar]
- Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB. Elevated C-Reactive Protein Levels in Overweight and Obese Adults. JAMA. 1999;282:2131–2135. doi: 10.1001/jama.282.22.2131. [DOI] [PubMed] [Google Scholar]
- von Haehling S, Jankowska EA, Anker SD. Tumour necrosis factor-alpha and the failing heart - Pathophysiology and therapeutic implications. Basic Res Cardiol. 2004;99:18–28. doi: 10.1007/s00395-003-0433-8. [DOI] [PubMed] [Google Scholar]
- Willerson JT, Ridker PM. Inflammation as a Cardiovascular Risk Factor. Circulation. 2004;109:II-2–10. doi: 10.1161/01.CIR.0000129535.04194.38. [DOI] [PubMed] [Google Scholar]
- Williams CD, Taylor TR, Makambi K, Harrell J, Palmer JR, Rosenberg L, Adams-Campbell LL. CES-D four-factor structure is confirmed, but not invariant, in a large cohort of African American women. Psychiatry Research. 2007;150:173–180. doi: 10.1016/j.psychres.2006.02.007. [DOI] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial Differences in Physical and Mental Health. J of Health Psychol. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]