Abstract
The public Indian health care system is plagued by high staff absence, low effort by providers, and limited use by potential beneficiaries who prefer private alternatives. This artice reports the results of an experiment carried out with a district administration and a nongovernmental organization (NGO). The presence of government nurses in government public health facilities (subcenters and aid-posts) was recorded by the NGO, and the government took steps to punish the worst delinquents. Initially, the monitoring system was extremely effective. This shows that nurses are responsive to financial incentives. But after a few months, the local health administration appears to have undermined the scheme from the inside by letting the nurses claim an increasing number of “exempt days.” Eighteen months after its inception, the program had become completely ineffective.
1. Introduction
On paper, India’s public health care system looks like the model for delivering universal health services in a large, poor country. Its comprehensive three-tier design ensures that all households, rural and urban, are close to a free government health facility. A survey of health facilities in rural Rajasthan found that the infrastructure for this system is operational: The average household is within two kilometers of the nearest public facility; qualified medical personnel are employed by the government to staff them; and, although not free, public facilities are still far and away the cheapest option available for qualified medical care (Banerjee, Deaton, and Duflo 2004a, 2004b). Yet the system fails to deliver. Even though government facilities are less expensive and are staffed by trained and certified personnel, most households prefer to see private providers, who not only are unregulated but also are often unqualified (Banerjee and Duflo 2005).
One possible reason for the low usage of government facilities is provider absenteeism. The facilities are closed more often than not, largely because the nurses simply do not show up for work. This article reports the results of a randomized evaluation of an incentives program to improve Assistant Nurse Midwife (ANM) attendance at rural subcenters, which was implemented collaboratively by the nongovernmental organization (NGO) Seva Mandir and the state and local health administrations in the Udaipur District of the State of Rajasthan. Under the program, Seva Mandir used timeclocks to monitor ANM attendance and passed the information on to the government, which used the attendance data with a specific schedule of fines and punishments (introduced expressly for the program) to determine the wages of a given nurse. When the incentives were effectively in place as they were in the first 6 months of the program they led to a dramatic improvement in attendance—a doubling by some measures. After the first 6 months, however, the local health administration deliberately undermined the incentive system. The result was that, 16 months after program inception, there was no difference between the absence rates in treatment and comparison centers; both were extremely high (over 60%). These results show that, like other public service providers, nurses are responsive to properly administered incentives (see Duflo and Hanna [2005] for similar results on informal school teachers). Furthermore, they show that ensuring that nurses come to work is a low priority for the local health administration and that incentive systems are quickly undermined if there is insufficient political will to enforce them. Given this, resources don’t seem to be the main limitation and so pumping more money into the system without attendant reform to reduce absenteeism, as is currently planned under the recently launched National Rural Health Mission, will not solve the underlying problem.
2. Background: Public Health Care System in India
The public health care system in India was designed to ensure comprehensive coverage. The system consists of three tiers. Patients enter at the first tier, consisting of “aid posts” or “subcenters.” These refer more complicated cases to the primary health centers (PHCs) and community health centers (CHCs), which in turn refer them to the district hospitals, the third tier. Subcenters provide only the most basic care (first aid, prenatal and postnatal care, malaria treatment, etc., but not antibiotics) and are staffed by at least one trained ANM. Each PHC is responsible for monitoring the attendance of ANMs at its satellite subcenters.
On a handful of operational measures the system is doing admirably well. Local NGO Seva Mandir’s 2003 Udaipur Health Survey of 100 villages, 1,000 households, and all the private and public health care facilites that serve them (Banerjee, Deaton, Duflo 2004a, 2004b) found there is a subcenter for every 3,600 individuals (the official target is 3,000 per subcenter). Despite the relative low density and high poverty of the population surveyed, the average household was only 1.53 kilometers from the closest public facility. Nearly all the subcenters have an ANM, and those in the most disadvantaged areas have two. The ANMs have completed secondary school and 1.5 years of training. PHCs have 5.8 medical staff, on average, including 1.5 doctors, and 87% of the CHCs have one or more specialists. The average visit to a subcenter costs the patient only Rs. 33 (where approximately 39 rupees equal US$ 1), and a PHC/CHC visit costs Rs. 100 for visits that involve operations and tests. All private practitioners are more expensive: Unqualified practitioners of nontraditional medicine (“bengali doctors”) cost Rs. 105 per visit; qualified private doctors cost Rs. 179; and traditional healers (“bhopas”) cost Rs. 131 (Banerjee, Deaton, and Duflo 2004a, 2004b). Thus, besides being geographically comprehensive, the public health care system is staffed by qualified medical personnel and is cheaper than all other comparable (and some worse) alternatives.
But for all that, it still fails in its basic mission of delivering health services. The Udaipur Health Survey found that even the very poor had largely abandoned the public health care system. Though households visited health providers 0.51 times per month, only 0.12 visits were to a public facility. In other words, more than 75% of people needing medical care went to the more expensive traditional healers (0.11 visits) and private providers (0.28). What’s more, the bottom third of the population uses public facilities less than the richest third and instead use traditional healers (Banerjee, Deaton, and Duflo 2004a, 2004b).
Why? One central problem is the high level of absenteeism in medical facilities. Subcenters and PHCs are supposed to be open 6 days a week, 6 hours a day. But in the 2003 survey, where public health facilities were surveyed weekly for over a year (on average 49 observations per facility), subcenters were on average closed 56% of the time. And in only 12% of the cases was this because the nurse was on duty somewhere else around the center; the rest of the time she was simply absent.1 These results are similar to the 43% absenteeism rates found in nationally representative surveys of public health facilities in India (Chaudhury et al. 2006). To make matters worse, the pattern of absence is completely unpredictable (Banerjee and Duflo 2006). These high and erratic absence rates may reduce usage through two effects. First, knowing that the ANM may be absent may make you less likely to go to the center in the first place, which we term a discouragement effect. Second, if you do go and the ANM is absent, you may end up having to go to another provider, which we term a mechanical effect. Indeed, the survey data shows a clear negative correlation between facility utilization and the ANM absence rates. For villages served by facilities that are closed relatively often, the poor are less likely to visit the public facilities and more likely to visit the bhopa. (There is no correlation for the nonpoor.) The causality behind this correlation could just as well go from utilization to provider absence as it could from absence to utilization, but it remains obvious that all major reforms aiming to improve the delivery of public health services to India’s poor must make provider absenteeism a major, if not the first, priority.
3. The Seva Mandir ANM Monitoring Program: History and Description
One of the priorities that emerged from public discussions of results from the 2003 Udaipur Health Survey was to tackle absenteeism in subcenters. Seva Mandir, the NGO that facilitated the survey, had some experience in dealing with absenteeism. Faced with a 40% teacher absence rate in its schools, it introduced a system of strict monitoring and incentives based on presence; this halved teacher absence, increased the number of child-days in the schools by 30 percentage points, and increased test scores by 0.2 of a standard deviation (Duflo and Hanna 2005). In 2004, Seva Mandir opened negotiations with the government to implement a similar monitoring and incentives program for nurses. By this time a number of subcenters had two nurses: a “regular” tenured ANM and an “additional” ANM hired on a yearly contract basis. In November 2005, Seva Mandir and the government agreed that Seva Mandir would monitor the additional ANM for three days a week (the days were agreed to with the local administration) in 16 randomly selected centers (12 two-nurse centers were assigned to be controls). In January 2006, the district administration also passed a directive requiring all nurses in all centers to be at their center every Monday (so no field visit and no meetings were supposed to occur on this day). Seva Mandir was asked to monitor the regular ANMs on Mondays in 33 randomly chosen centers that employed just one ANM; 39 single-ANM centers were left as controls for this experiment.2
In February 2006, the Chief Medical Health Officer (CMHO) of Udaipur District announced the following incentives to complement the monitoring in the randomly assigned centers: ANMs absent for more than 50% of the time on monitored days would have their pay reduced by the number of absences recorded by Seva Mandir’s monitoring system for that month. Further, ANMs absent for more than 50% of the time on monitored days for a second month would be suspended from government service.
To monitor presence, Seva Mandir uses time/date-stamping machines locked into a caddy and password-protected to prevent tampering. The ANM is supposed to stamp a register secured to the wall of the subcenter three times a day: once at 9 a.m., once between 11 a.m. and 1 p.m., and once at 3 p.m. She must both sign and stamp following a routine that ensures that only the ANM can sign.
If an ANM does not stamp on a particular day but has a legitimate reason, she indicates this on the register. Some absences are “excused” and count as presences; we refer to those days as “exempt days.” In particular, any absence that is the result of a government-mandated meeting, survey, or other health work is authorized. Some of the most common excused absences include government-sanctioned holidays, sector meetings, block meetings, and other government-sanctioned activities such as immunization and survey work. Exempt days are then supposed to be verified by the ANM’s supervisor in the PHC. Another reason why an ANM may not be able to stamp is if the machine malfunctions. When this happens, ANMs are to call the office within 24 hours. Once a problem call is reported, the monitors attempt to fix the machine as soon as possible. In the intervening period the ANM cannot be monitored and those days appear separately in the system.
The subcenter registers are collected at the beginning of each new month. Program monitors bring the registers from the previous month to the office and coordinators compute ANM absences. Before the fifteenth of each month, an absence note that summarizes the information for the CMHO is prepared. The absence logs are then sent to the PHC in charge of each nurse and the PHCs are supposed to implement the potential deductions. In addition, the absence record shows the exempt days reported by the nurses, which the PHC can then verify as legitimate before implementing any potential deductions. Thus, whether or not the deductions are implemented in practice depends largely on the diligence of the local administration because they check whether the exempt days are indeed exempt (because they are the only ones with this information) and because it is they who pay the salary.
4. Evaluation Methodology and Results
4.1. Baseline Characteristics: Results from the 2002 Continuous Facility Survey
The subcenters in the study served 135 villages in Udaipur District (100 of those villages were covered by the Udaipur Health Survey and 35 were added for this study). These 135 villages were randomly selected among those where Seva Mandir was working (Banerjee, Deaton, and Duflo 2004a, 2004b). For those subcenters included in the original survey, we have detailed data on absence rates and usage during the year 2002–2003. Using this data, it is possible to check that there was no significant difference between treatment and comparison centers in 2002–2003, that is, two years before this experiment (Banerjee, Duflo, and Glennerster 2007).
4.2. Results: Random Checks
The main data for the evaluation came from random unannounced visits to the subcenter by a monitoring field officer. At each such visit, the monitor collected simple data on whether the center was open, whether the nurse(s) was (were) present at or in the vicinity of the subcenter,3 and how many patients were being treated or waiting to be treated. To prove the accuracy of the data, they also took a time/date-stamped picture of the center that included the nurse if she could be found.
The main results of the evaluation are presented graphically in Figures 1 and 2. As we have explained, there are two distinct experiments: the monitoring of the single ANM and the monitoring of the additional ANM in two-ANM centers. Figure 1 shows the fraction of centers where the regular ANM was present in treatment and control centers. We separate out data for Mondays—the days when these ANMs were monitored by having to stamp the register—and for the other days of the week.4 Figure 2 shows the results for the second ANM in two-ANM subcenters. In this case the second ANM is monitored three days a week. Again we show presence for monitored and unmonitored days separately and contrast this with the control.
Figure 1.
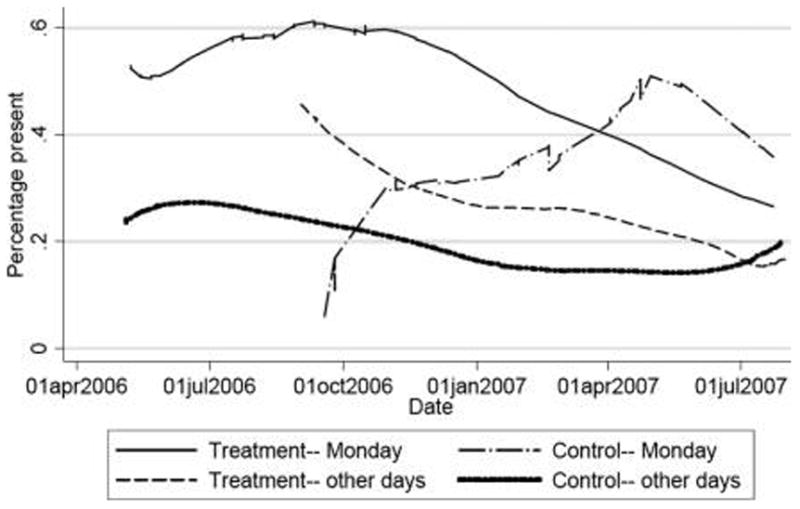
Presence of regular ANM, random checks.
Figure 2.
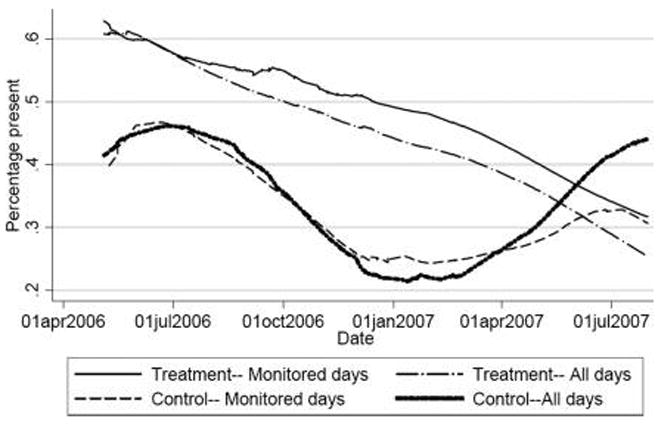
Additional ANM present, two-ANM centers, random checks.
4.2.1. Single ANM Monitoring
In its first 6 months, the monitoring program appears to have had a large effect. In the treatment group, the rate of presence on Mondays is 60% in October. This is well above the rate in the control group on Mondays and in the treatment group on other days of the week, both of which are less than 30%.5 Although the mandate that ANMs should not be in the field but in their subcenter on Mondays applied to all ANMs, both treatment and control, in the autumn of 2006 only treatment-ANMs were more likely to be present on Mondays than on other days. From November onward, however, the rate of presence of the monitored ANM starts to fall, reaching about 25% by July 2007. Meanwhile, the rate of presence on Mondays among unmonitored ANMs actually increased a bit over time (to about 35%) so that, by the end of the period, the treatment ANMs are actually less likely to be present on Mondays than the control ANMs. On other days, their presence also drops over time while that of the comparison ANM stays constant, so that the two also eventually converge.
4.2.2. Centers with Additional ANMs
Figure 2 shows the result of the program for the additional ANM in centers with two ANMs. These ANMs are required to be present (and in treatment sites monitored) for three days a week. Again, the figure shows the rate of presence for monitored days and unmonitored days for both treatment and comparison nurses. There are several interesting patterns in this figure. First, for the regular ANMs, there is initially a substantial treatment effect: the rate of presence of the treatment ANM is about 15 percentage points higher than for the control ANM. Eventually, however, this treatment effect drops to zero. This is due to a fast drop in the rate of presence of the treatment ANM: The rate of presence of the treatment ANM on monitored days drops from over 60% in May 2006 to about 30% in July 2007. The rate of presence on other days starts at the same level (there was initially some confusion as to which days were monitored and which days were not), and then drops faster. Second, the rate of presence of control ANMs also declines during the period, from 40% initially down to 20% in January 2007 and then back up to just above 30%. Part of this increase seems to be due to normal seasonal variation, though we will be able to say more about this when we have a longer time series (there are strong seasonal attendance patterns in the 2003 data as well).
Thus, for both programs, there is initially a large treatment effect that eventually drops to nothing. The rate of presence of both treatment and control ANM by the end of the evaluation period are both staggeringly low, much worse than the 44% documented in 2002–2003.
Table 1 presents the main numerical results. For centers with one ANM, throughout the entire duration of the experiment the average rate of presence on Mondays of the ANM was 54.1% in the treatment centers and 39.4% in the comparison centers. This 14.7 percentage point difference is significant at the 5% level, but it hides a deterioration of the performance over time. In the period from May to the end of October, the rate of presence on monitored days was 59% in the treatment centers and 30% in the control centers. This difference of 27.9 percentage points is also significant at the 5% level (column [4], panel B). From November 2006 to June 2007, however, the average rate of presence falls to 43% in the treatment group and increases to 43% in the comparison group. There is no difference left between the two groups (column [5], panel B).
Table 1.
Difference between treatment and comparison centers.
| Centers with One ANM |
Centers with Two ANMs |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Entire Period |
Difference between Treatment and Control |
Entire Period |
Difference between Treatment and Control |
|||||||
| Treatment (1) |
Control (2) |
Difference (3) |
May–Oct. (4) |
Nov.–June (5) |
Treatment (6) |
Control (7) |
Difference (8) |
May–Oct. (9) |
Nov.–June (10) |
|
| A. On all days | ||||||||||
| Monitored ANM present | 0.382 (0.022) | 0.220 (0.019) | 0.104 (0.049) | 0.243 (0.093) | 0.073 (0.047) | 0.473 (0.024) | 0.324 (0.033) | 0.137 (0.066) | 0.101 (0.091) | 0.133 (0.069) |
| Number of clients (if center is open) | 0.724 (0.085) | 0.590 (0.089) | 0.077 (0.186) | 0.170 (0.489) | 0.161 (0.174) | 0.728 (0.079) | 0.744 (0.109) | −0.033 (0.174) | 0.024 (0.219) | −0.106 (0.205) |
| Number of visits | 496 | 481 | 977 | 268 | 638 | 420 | 207 | 627 | 254 | 344 |
| B. On monitored days | ||||||||||
| Monitored ANM present | 0.541 (0.036) | 0.394 (0.058) | 0.147 (0.073) | 0.279 (0.148) | 0.029 (0.105) | 0.522 (0.043) | 0.342 (0.054) | 0.142 (0.111) | 0.041 (0.092) | 0.142 (0.111) |
| Number of clients (if center is open) | 0.906 (0.124) | 0.464 (0.150) | 0.441 (0.247) | −0.089 (0.431) | 0.514 (0.279) | 0.778 (0.117) | 0.852 (0.205) | −0.185 (0.251) | 0.024 (0.219) | −0.185 (0.251) |
| Number of visits | 194 | 71 | 265 | 146 | 119 | 138 | 79 | 217 | 254 | 217 |
Notes: Standard errors in parenthesese below the mean (or difference). The difference in means is obtained from a regression where we control for the day of the week in which the visit took place. The standard errors of the difference in means is corrected for clustering a the center level.
The results for the additional ANM in two-ANM centers are somewhat different. Over the entire period, the program increased the probability of the additional ANM being present by 13.7 percentage points (from 32.4% to 47.3%) on all days (column [8], panel A) and by 14.2 percentage points on monitored days. Unlike the monitoring of the regular nurses, the program effect initially increased over time, mainly because the absence rate of all the additional ANMs was initially fairly high (probably because they had all recently joined and had only temporary contracts). The program impact is thus higher in the period from November 2006 to June 2007 (though the graph shows that it becomes essentially zero by the end of that period).
Table 1 shows that even when the incentive was effective at increasing presence, it had essentially no impact on the number of patients treated, which in any case is very low. Between 0.46 and 0.9 clients are being seen in the center at any given time when the center is open, fewer even lower than the two to three clients observed in 2002–2003. The number of clients, conditional on the center being open, is not significantly different in treatment and control in sub-centers with either one or two ANMs. Finally, clients do not appear to respond much to the greater likelihood of ANMs being present on the monitored days (Mondays). Although there are more clients on Mondays than on other days in one-ANM treatment centers, the difference is small (0.9 compared to 0.7) and the pattern does not follow through to monitored days in two-ANM subcenters. This might mean that people have so completely given up on the public health system that they do not take any notice of the improvement; it might also mean that it takes time to change behavior and so temporary improvements (as this one turned out to be) have no impact. The results are also consistent with people not wanting the kind of health care that is provided by the public system.
The only encouraging finding is that the program seems to have no negative spillover effect on presence on other days. In fact, the rate of presence is actually significantly higher on unmonitored days in treatment than control in the first period. In single-ANM centers, for example, presence on unmonitored days is 23 percentage points higher in the initial period and remains marginally higher even in the second period (by 8 percentage points). For two-ANM subcenters, having the additional ANM monitored does not appear to have any impact on the unmonitored ANM.
4.3. Time/Date-Stamping Data
What accounts for these results? Why did nurses stop coming to work? Figure 3, which shows administrative data for each monitored day (for additional ANMs), points quite clearly to the answer. In February 2006, the ANMs were present for the full day on about 50% of the monitored days, present for a half-day on about 5% of the days, absent on almost 20% of the days, on casual leave on 5%, excused on about 17%, and had a machine problem on about 3% of the days. Over time, the full and half-day rate of presence decreases (as we see in the random checks) but the rate of absence does not increase. The shortfall is made up by a greater number of exempt days and days where the ANM did not stamp because of “machine problems.” Although not separately shown, the same pattern is evident for the single-ANM subcenters on Mondays only, which is notable because Mondays are supposed to be free from meetings and other activities outside the center. The result of this increase in exempt days and “machine problems” is that although there was a sharp increase in actual absence very few ANMs were sanctioned in the later months of the program. This in contrast to the start of the program, when deductions had taken place.
Figure 3.
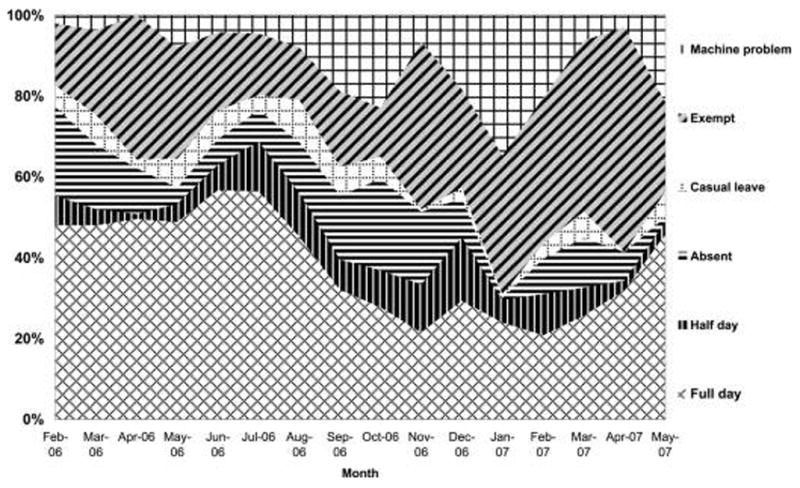
ANM attendance according to official records, monitored days.
The “machine problems” are likely to be the ANMs’ response to the incentive system. When a machine is broken, the nurse does not have to stamp until she gets a new one or gets hers fixed. But she cannot get a new one if she is not at the subcenter to meet the program monitor. So if the nurse deliberately stops coming to the subcenter after her machine starts malfunctioning, she does not need to stamp (and is therefore not monitored anymore). Over time, we saw a number of machines that had clearly been deliberately broken.6 It also took longer and longer to find the ANM after she reported a problem. In response, starting in September 2007, the rules were changed so that an ANM had to deposit a broken machine at a Seva Mandir office near her subcenter and then pick it up within three days. This might solve this problem.
The increase in the number of “exempt days” is likely a systemic response. The exempt days can only be granted by the PHC (so the ANM can perform other duties or attend meetings), so the PHC officials can always check if there are any fake exempt days. The ANM cannot lie about the number of exempt days without the complicity of those PHC officials to whom she reports. In turn, the activities at the PHC are monitored by the CMHO of the district, who also gets data and graphs showing the increase in the number of exempt days over time from Seva Mandir. We have tried to obtain a list of the number of exempt days directly from the administration to check whether the ANMs were inventing more exempt days or whether the number of meetings and other field activities had indeed increased. This turned out to be impossible: The center does not maintain the list, and the PHC officials would not share theirs. However, we were able to confirm that the number of official meetings had not increased (indeed, the records show that the ANMs do not report more meetings). What changed was an increase in reported activities in the field (such as “surveys” or “immunization work”), where it is impossible to monitor whether or not the ANM was actually doing the work. Some excuses that had been ruled out as invalid by the head of the district health administration such as “case mobilization,” the euphemism for encouraging people to get sterilized have also crept back in these registers. In short, one of two essentially equivalent things is happening: (1) the PHC, knowing full well that being asked to go unmonitored to the field means essentially a license to stay home, is providing those excuses to the ANM; or (2) the ANM is making them up, and the PHC is not sanctioning them for doing this. In either case, the health administration has undermined the system it had itself put in place, so that the incentives (which remain on the books) no longer have any bite.
5. Conclusion
Why did the district administration feel compelled to take the teeth out of a very successful system of incentives that it had introduced? First, the idea that the nurses should be given some incentives came from the head of the district, so health administrators (the CMHO and the PHC doctors) probably could not refuse to implement it. However, the CMHO and other health officials were the ones who faced pressure from the ANMs to get rid of it. Rather than press to cancel the system, which would have been somewhat embarrassing given that it required only that the ANMs come to work half of the time, it was easier to arrange things so that the incentives were not binding. This was a convenient way to save face by complying (at least on paper) with orders, even though it meant Seva Mandir was wasting resources by monitoring the nurses. Because the rules were respected, it gave the district head no means of taking disciplinary action against anybody.
But there remains a bigger puzzle. Why was the health administration free to let the nurses off? Although a system only nominally in place might be enough to satisfy their obligation to their superiors, why are the officials not under pressure from the would-be beneficiaries through the political system to actually deliver improved services? A part of the answer is that the local governments have little power over the health administration. The only way to pressure health officials is via the areas’ representative in the state assembly (the MLA). The MLA represents many villages, each with multiple demands. Unless the health system is a top priority for a large number of these villages, it may not ever claim enough of the MLA’s attention to make a difference. And improving the health system is probably not at the top of the list of what people are demanding. This need not mean that people don’t care about health care; on the contrary, households report spending 7.3% of their monthly budget on health care (Banerjee, Deaton, and Duflo 2004a, 2004b). It could mean that they have decided the government is unlikely to be particularly effective at providing health care and have therefore focused on the private market. That would explain why, even when the nurses were coming to work (in the first six months of the program) and as this was announced in the communities, the demand for their services did not increase.7 Moreover, from the standpoint of a single village, this is an equilibrium: Even if they decided that better public health care is a priority for them, the MLA is unlikely to do anything about it unless the other villages also care about it, in which case the MLA would probably need to intervene at the systemic level, and so create a vicious circle of low demand and low supply (as discussed in Banerjee and Duflo 2006).8
Moreover, it is always difficult to evaluate the quality of health care that one is receiving. Das and Sanchez-Paramo (2004) show that there is no evidence that people can identify sources of quality care. Moreover, many of the people we talked to strongly mistrusted the ANM, whom they suspected of being interested only in sterilization, even without their consent. Finally, because few people come to see them even when they sit in the centers all day, it is easy to see why the nurses may not be intrinsically motivated to do their job and feel justified in resisting any attempts to force them to come to work.
Any program for reforming the system—even if it made providers more accountable—must therefore grapple with the problem of lack of demand. There are some obvious, small things that would help. For starters, taking the sterilization program out of the hands of ANMs would almost surely be good for demand. The case for general improvements (better infrastructure, medicines, equipment, etc.) to make the centers more attractive is vitiated by provider absence. Under the National Rural Health Mission, government health spending will go up from 0.9% of GDP in 2005 to between 2% and 3% by 2012; every subcenter will get Rs. 10,000 (about US$ 250) a year for medicines and equipment. But because even the additional nurses were absent it is clear that spending on additional resources is unlikely to improve demand if the ANMs remain absent and the centers are not open. Whether all of this would be enough to undo the effects of long-term neglect and lack of accountability remains an open question. In any case, it is not possible to reform something like the health system unless one of the larger stake-holders—the state, the people, a big political party—decides to put it near the top of its agenda. Until then, neither additional resources nor greater incentives will do much more than putting a bandage on a patient who is already dead.
Acknowledgments
We thank the National Institutes of Health (grant P01-AG005842) and the MacArthur Foundation for financial support. The Center for Health and Well Being at Princeton University partly funded the baseline survey. We thank the collector of Udaipur District, Mr. Shikhar Agarwal, for his help and support of our research program in Udaipur. At Seva Mandir we thank Neelima Khetan, Bhagirath Gop, Smita Singh, and Dr. Sanjana Brij-Mohan for their tireless efforts to make this program work and for many stimulating discussions. At J-PAL, Cindy Palladines, Priyanka Agarwal, Payal Hathi, Dhruva Kothari, Neil “Buddy” Shah, Anuja Singh, and Andrew Fraker provided outstanding research assistance. At Vidhya Bhawan, Tushita Lodha kept our sanity and our finances in check, and Pramod Tiwari was a superb team leader.
Footnotes
For a more detailed discussion of the results, see Banerjee and Duflo (2005).
In Banerjee, Duflo, and Glennerster (2007), the working paper version of this paper, we explain why the treatment and control groups ended up being unequal.
Because nurses were supposed to be in their office on the monitored days, we did not attempt to find them elsewhere in the field.
In the first few weeks of the evaluation, owing to a miscommunication in the field, random checks occurred only on Mondays in the treatment centers and only on other days in the comparison centers. In all the analysis that follows, we control for the day of the week in which the random check happened.
Unfortunately, there were no random checks in control subcenters until 1 September 2006. Moreover, there were very few such checks in September, so that the initial first “jump” in presence of the control ANM on Sunday is likely to be an artifact of the low number of observations and thus should not be overinterpreted.
Some of the machines looked as if they had been hurled into a wall. The ANMs also explicitly told Seva Mandir that this is what they would do.
In the Seva Mandir teacher-incentive project, which was much more sustained and effective, there was likewise no response in terms of greater enrollment or student attendance.
The key point is that fixing the health system requires systemic reform, whereas (say) providing a well is simply a matter of a financial allocation to the village.
Contributor Information
Abhijit V. Banerjee, Email: banerjee@mit.edu, MIT and Abdul Latif Jameel Poverty Action Lab.
Rachel Glennerster, Email: rglenner@mit.edu, MIT and Abdul Latif Jameel Poverty Action Lab.
Esther Duflo, Email: eduflo@mit.edu, MIT and Abdul Latif Jameel Poverty Action Lab.
References
- Banerjee Abhijit, Deaton Angus, Duflo Esther. Wealth, Health, and Health Services in Rural Rajasthan. AER Papers and Proceedings. 2004a;94(2):326–330. doi: 10.1257/0002828041301902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee Abhijit, Deaton Angus, Duflo Esther. Health Care Delivery in Rural Rajasthan. Economic and Political Weekly. 2004b;39(9):944–949. [Google Scholar]
- Banerjee Abhijit, Duflo Esther. Working paper, MIT. 2005. Improving Health-care Delivery in India. [Google Scholar]
- Banerjee Abhijit, Duflo Esther. Addressing Absence. Journal of Economic Perspectives. 2006;20(1):117–132. doi: 10.1257/089533006776526139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee Abhijit, Duflo Esther, Glennerster Rachel. Putting a Band-Aid on a Corpse: Nurse Incentives in the Indian Public Health Care System. Working paper, MIT. 2007 doi: 10.1162/JEEA.2008.6.2-3.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhury Nazmul, Hammer Jeffrey, Kremer Michael, Muralidharan Karthik, Rogers F Halsey. Missing in Action: Teacher and Health Worker Absence in Developing Countries. Journal of Economic Perspectives. 2006;20(1):91–116. doi: 10.1257/089533006776526058. [DOI] [PubMed] [Google Scholar]
- Das Jishnu, Sanchez-Paramo Carolia. Working paper, Development Research Group, World Bank. 2004. Short But Not Sweet: New Evidence on Short Duration Morbidities from India. [Google Scholar]
- Duflo Esther, Hanna Rema. NBER Working Paper No. 11880; BREAD Working Paper No. 103. 2005. Monitoring Works: Getting Teachers to Come to School. [Google Scholar]


