Abstract
Objective
Some research suggests that social, political, and cultural life in the U.S. and Canada are growing divergent. We use health lifestyle theories to extend prior research and compare the U.S. and Canada on population health indicators.
Methods
The population health indicators include health behaviors, fertility, and cause-specific mortality for each of the United States (and Washington D.C.), and Canadian Provinces and Territories (N=64).
Results
Canada and the U.S. are significantly different on many health lifestyle variables. But, levels of the health lifestyle variables converge at the U.S./Canada border, and some U.S. States and Canadian Provinces or Territories exhibit similar health lifestyle patterns, regardless of whether they share an international border (these are mapped in the paper).
Conclusions
Although Canada and the U.S. differ on major population health indicators, some States, Provinces, and Territories exhibit marked similarities. Our paper concludes with a discussion about how our comparative perspective might inform population health policies.
There is an ongoing and contentious debate about the degree of similarity between the U.S. and Canada. Academic and popular literature is often characterized by opinion, folklore, misinformation, and stereotypes (Rosenau 2006). Some scholars posit that the differences between Canada and the U.S. are large and that the two countries are as unlike as “Fire and Ice” (Adams 2003), although such research often lacks analytical rigor, relies extensively on quotes from Updike or De Tocqueville, and focuses on a narrow set of opinions or consumption patterns (Smith 2005). We contribute to this debate by using a broad set of health lifestyle indicators for U.S. States (and Washington D.C.) and Canadian Provinces and Territories to empirically examine intra- and inter-national differences. Health lifestyles are important because they reflect the underlying social, cultural, economic, and policy environments of each area; exhibit marked variation across States, Provinces, and Territories; are important indicators of population health; and might be effectively modified by social policies.
The U.S. and Canada
There has been much academic and popular debate about whether the U.S. and Canada are growing apart or becoming more similar. Some cultural studies research argues that Canada and the U.S. are very different in terms of patterns of consumption, family and political values, and acceptance of multi-culturalism (Adams 2003; Byers 2007; Cohen 2007), although others find similar levels of participation in sports and cultural organizations (Helliwell 2003). Despite concerns about the analytical rigor of some prior research (Smith 2005), the general theme that Canada and the U.S. are very different resonates with many scholars.
Prior research often focuses on opinions, values, or patterns of consumption that may be very different between countries (Adams 2003; Byers 2007; Cohen 2007), with less attention given to topics that might show greater affinity between the two nations. We will focus on indicators of population health—including health behaviors, fertility patterns, and causes of death that reflect risky behaviors—a domain that is seldom examined in this area of research. We will expand on research that examines differences between the U.S. and Canada in two ways.
First, we will focus on convergence in health lifestyle characteristics at U.S./Canada border. The U.S. and Canada may have strong affinities at the meeting of their shared and expansive international border. The shared border has resulted in efforts to create alliances in trade and social policy between the U.S. and Canada (Abgrall 2005; Boucher 2005; Evans 2007), and it may allow for common media markets or foster ties among neighbors from different countries. By drawing on State, Province, and Territory level data, we can focus on variation within and between countries. Research that compares national means for variables of interest may understate the variation within countries and the degree of overlap between countries.
Second, we will identify groups of States, Territories, or Provinces that share similar patterns of health indicators, regardless of their geographic proximity. Most research that examines Canada-U.S. alliances focuses on the impact of shared borders on commerce or trade (Abgrall 2005; Anderson and van Wincoop 2003; Boucher 2005; Evans 2007). Shared borders may shape population health, but some research suggests that “border effects” between Canada and the U.S. may be declining in importance (Downs and Sawchuk 2007).
There are several examples of cultural and economic collaboration between the non-bordering areas of the U.S. and Canada. In July 2006 the mayors of Calgary, Alberta and Houston, Texas signed a Bilateral Partnership that encompasses energy, the environment, education, health sciences, culture, arts, tourism, and aerospace (White 2006). Arizona and Alberta also have sought to improve bilateral trade and investment (McLaren, Hunter, and Sherman 2006). Similarities in population health indicators may also span nations and suggest opportunities for policy collaborations, regardless of geographic proximity.
Health Lifestyles
Health lifestyles can offer important insights into differences between Canada and the U.S. Health lifestyles are broad but potentially unobservable orientations toward health that incorporate notions of what constitutes good or poor health, health-related norms, and knowledge about health promotion (Cockerham 2000; Cockerham, Rutten, and Abel 1997). Health lifestyles also reflect policy environments, social conditions, cultural understandings, and economic resources (Bourdieu 1984; Cockerham 2000; Frolich, Corin, and Potvin 2001), which may lead to differences in health lifestyles across States, Provinces, and Territories.
Empirically, we seek to document patterns among U.S. States and Canadian Provinces and Territories for characteristics that are central to population health, relevant for social policy, and that likely reflect the practice of health lifestyles. Prior research has documented important differences in factors like obesity, smoking, and certain causes of death across U.S. States (Ezzati et al. 2006; Mokdad et al. 1999; Pickle, Mungiole, and Gillum 1997; Tauras 2003; Vandegrift and Yoked 2004), or Canadian Provinces and Territories (Stephens et al. 2001; Vanasse et al. 2006). Although some research has compared the U.S. and Canada at the national level (Kaiserman and Rogers 1991; Sanmartin et al. 2006), or has focused on sub-national comparisons of overall mortality (Ross et al. 2000), relatively little research has directly compared States, Provinces, and Territories on important health lifestyle indicators.
We rely on numerous indicators of health lifestyles, including health behaviors (cigarette smoking, binge drinking, and obesity; although obesity is not a behavior per se, it is largely a function of dietary, exercise, and smoking practices), fertility (teenage fertility, and measures of total fertility), and cause specific mortality (from human immunodeficiency virus [HIV], diabetes mellitus, liver disease, accidents, motor vehicle accidents, suicide, and homicide). We sought measures that assess behaviors directly, or that—in the case of cause-specific mortality— are sensitive to health practices or risky behaviors (Mokdad et al. 2004); reflect the social, economic, cultural, and policy environments that shape the practice of health lifestyles in each State, Territory, or Province (Frolich, Corin, and Potvin 2001); and are measured similarly in the publicly available data for each area.
We also examine whether healthcare (i.e., availability and utilization of healthcare) and sociodemographic (i.e., immigration, race/ethnicity, education, unemployment, crime) variables can account for health lifestyle differences between the U.S. and Canada. Health services researchers often emphasize the importance of healthcare availability and utilization for population health, because regular care can allow earlier detection and better treatment of disease. Health insurance is a primary indicator of access to care, but there is no variation on that variable within Canada because they have universal coverage. Instead, we focus on the number of family medicine doctors per capita and hospital beds per capita, as indicators of healthcare availability (Mansfield et al. 1999). Healthcare utilization, as indicated by regular doctor visits, may also improve health. We focus on visits to the dentist in the past 12 months because it was readily available for the U.S. and Canada, and because oral health is strongly tied to infection, diabetes, and cardiovascular disease (Li et al. 2000).
Social epidemiologists and population health researchers often emphasize the importance of socioedemographic factors in shaping population health (Berkman and Kawachi 2000; Link and Phelan 2005). Immigrants often have better health and health behaviors than their native born counterparts because their language and cultural values support healthy behaviors, strong friendship and family connections, and success in the labor force (Antecol and Bedard 2006; Dunn and Dyck 2000; Halli and Anchan 2005). Although the meaning of race/ethnicity varies between the U.S. and Canada, Blacks in the U.S. and Aboriginals in Canada have fewer social and economic opportunities, and worse health than the majority populations in each country (Anand et al. 2001; Williams and Collins 1995).
High levels of education provide knowledge about effective health management strategies and support the development of social psychological or material resources that allow individuals to improve their health (Mirowsky and Ross 2003). But high levels of unemployment can signify limited opportunities for employment or economic advancement, put individuals at increased risks of poverty and food or housing insecurity, and increase psychosocial stress— factors that may foster unhealthy lifestyles (Preston and Taubman 1994). High levels of nonviolent (i.e., burglary, motor vehicle theft) and violent (i.e., robbery) crime proxy for low levels of social capital, including low levels of trust in neighbors or in local governments, and weak commitments to looking out for the safety, property, and wellbeing of others (Putnam 2000).
Aims
Our first aim is to compare the health lifestyle variables between U.S. States and Canadian Provinces and Territories, with a particular focus on whether the levels of those variables converge at the U.S./Canada border. We will also examine whether healthcare and sociodemographic variables account for U.S./Canada differences in health lifestyle outcomes. Our second aim is to use inductive statistical methods (i.e., latent class analysis) to identify groups of States, Provinces, and Territories that have similar health lifestyle patterns regardless of whether they share an international (U.S./Canada) border. We will also describe patterns in our covariates across health lifestyle groups.
DATA AND METHODS
We use publicly available data for U.S. States, Washington D.C., and Canadian Provinces and Territories. We include Washington D.C. and exclude the U.S. Territories (Puerto Rico, Virgin Islands, Guam, American Somoa, Northern Marianas) because Washington D.C. is the political center of the U.S., is contiguous to the continental U.S., and has readily available data for our covariates. We include the Canadian territories because they play a central role in the political and cultural life of Canada and share borders with Canadian Provinces or U.S. States.
We sought the most current data available for both countries. Data for health behaviors, fertility, age, sex, and health care utilization were available for both countries in 2005. Canada’s most recent mortality data came from 2004, so we also use 2004 mortality data for the U.S. We use 2004 data on crime rates, unemployment, and health care availability and utilization. Canada provides data on immigration, education, race/ethnicity every fifth year, so we use 2006 data for both Canada and the U.S. In total, we have information for 64 observations: 50 U.S. States, Washington D.C., 10 Canadian Provinces, and 3 Canadian Territories.
Dependent Variables
Our key outcome variables include health behaviors, fertility, and mortality from selected causes. The health behavior variables include smoking, obesity, and binge drinking (Centers for Disease Control 2008; Statistics Canada 2008). Smoking is measured as the percentage of the population aged 18 or older who smoke in the U.S. or aged 12 or older who smoke in Canada. Obesity is measured as the percentage of the population aged 18 and older who report a body mass index of 30 or more (body mass is calculated from self-reported heights and weights in both countries). Binge drinking is measured as the percentage of those aged 12 or older who drank 5 or more drinks on at least 1 day within the past 30 days in the U.S., or who drank 5 or more drinks at least 12 times in the past year in Canada.
The fertility measures include the crude birth rate, the total fertility rate, and the age specific fertility rate for women aged 15–19 (Martin et al. 2007; Minister of Industry 2007a). The crude birth rate is measured as the number of births per 1,000 population. The total fertility rate indicates the number of children who will be born to an average woman by age 45, assuming that age-specific fertility rates remain constant over time. The age-specific fertility rate at ages 15–19 measures the number of live births per 1,000 women aged 15–19. Although births to many teenagers may take place within wedlock, early childbearing may have important implications for both women’s and children’s future life chances. More detail on the calculation of the fertility measures can be found elsewhere (Preston, Heuveline, and Guillot 2001).
Mortality from specific causes are identified by International Classification of Disease, Version 10 (ICD-10) codes in both countries (Miniño et al. 2007; Minister of Industry 2007b). We focus on the following causes of death, with the ICD-10 codes in parentheses: human immunodeficiency virus (HIV; B20–B24), diabetes mellitus (E10–E14), chronic liver disease and cirrhosis (K70, K73–74), accidents (V01–X59, Y85–Y86), motor vehicle accidents (a subset of all accidents; V02–V04, V09.0, V09.2, V12–V14, V19.0–V19.2, V19.4–V19.6, V20–V79, V80.3– V80.5, V81.0–V81.1, V82.0–V82.1, V83–V86, V87.0–V87.8, V88.0–V88.8, V89.0, V89.2), suicide (X60–X84, Y87.0), and homicide (X85–Y09, Y87.1). The mortality rates are calculated as the number of deaths per 100,000 population.
Independent Variables
Very few of our dependent variables are readily available for specific age groups or by sex (with the exception of fertility), at the sub-national level. Both the U.S. and Canada release age-standardized mortality rates, but they are standardized to different populations and are not directly comparable. Thus, we adjust for age and sex (Statistics Canada 2008; U.S. Bureau of the Census 2008), as they are strongly associated with health behaviors, fertility, and mortality (Poston and Micklin 2006). Age is measured as the percent of the population that is aged birth to 9 (referent), 10 to 19, 20 to 44, 45 to 54, 55 to 64, and 65 or older. Sex is measured as the percent of the population that is male.
Availability of healthcare is assessed with the numbers of beds per 1,000 population (Kaiser Family Foundation 2008; Statistics Canada 2008) and the number of family medicine or general practice physicians per 100,000 population (Canadian Institute for Health Information 2008; Smart 2007). Healthcare utilization was assessed as the percent of residents aged 18 and older who reported seeing a dentist, for any reason, in the last 12 months (Centers for Disease Control 2008; Statistics Canada 2008). Information on primary care visits was not readily available across the two countries.
Our sociodemographic variables include immigration, race/ethnicity, education, unemployment (Statistics Canada 2008; U.S. Bureau of the Census 2008), and crime (Federal Bureau of Investigation 2005; Sauvé 2005). Immigration is measured as the percent of residents in each area that were born outside of the nation of interest. Race/ethnicity is measured as the percent of residents that are Black or African American, Aboriginal or Native American, or White or other (referent). Education is measured as the percent of adults aged 25 or older that have less than a high school degree, a high school degree but less than a bachelor’s degree, or a college degree or more (referent). Unemployment is measured as the percent of the population aged 15 or older that are not currently employed but that are looking for work. To assess crime, we use the numbers of robbery, burglary, and motor vehicle theft per 100,000 population. These crimes are reported similarly in both countries; we exclude homicide and manslaughter from our analyses because they are highly correlated with homicide mortality, one of our outcome variables. We standardize the three items and take their mean (α = 0.62) to create a single index.
A dummy variable for nationality codes Canadian Provinces and Territories as 1, and U.S. States and Washington D.C. as 0. A dummy for international border is coded as 1 for U.S. States that share a geographic border with a Canadian Province or Territory, or Canadian Provinces or Territories that share a border with a U.S. State; States, Provinces, or Territories that are not on the U.S./Canada border are coded as 0.
Analysis
We employ two analytical strategies in our analyses. First, we estimate three models to examine whether the health lifestyle variables show evidence of convergence at the U.S./Canada border (Aim 1). Model 1 includes the dummy variables for nationality, international border, an interaction between nationality and international border, and age and sex. Model 2 further adjusts for healthcare availability and utilization to examine whether they account for geographic differences in the health lifestyle variables. Model 3 further adjusts for immigration, race/ethnicity, education, unemployment, and crime to examine whether sociodemographic factors account for geographic variation in the health lifestyle variables.
We use logistic regression to model the proportion (calculated by dividing the percentage by 100) who smoke, were obese, or binge drink; linear regression models the total fertility rate and the age-specific fertility rate at ages 15–19; and negative binomial regression models the numbers of births or deaths from selected causes, while using the population size in the same year as a denominator for the crude birth and mortality rates. We use generalized linear models and Stata 10 in these analyses (StataCorp 2007).
Second, we use latent class analysis (LCA) to identify groups of States, Provinces, and Territories that share similar patterns of health lifestyle variables (Aim 2). LCA is an inductive statistical method that uses patterns among observed variables to infer membership in unobserved subpopulations, or “latent classes” (Magidson and Vermunt 2004). In our case, LCA identifies patterns among the observed health lifestyle variables to ascertain which States, Provinces, or Territories reflect distinct subpopulations.
LCA requires that we specify the number of classes identified in each model. Because we do not have an a priori assumption about the number of classes to expect, we compare models that assume between two and nine classes. We use the Akaike Information Criterion (AIC), and Bayesian Information Criterion (BIC) to identify the model that best describes the data with the fewest number of classes (Magidson and Vermunt 2004; Muthén and Muthén 2007). Smaller values of the AIC and BIC indicate better model fit, given the number of parameters estimated by each model. We use Mplus software to conduct LCA (Muthén and Muthén 2007).
Our analyses present tests of significance because some of our variables are derived from surveys and may be measured imprecisely. Nevertheless, because we use the full population of U.S. States and Canadian Provinces and Territories, we may interpret results that appear substantively meaningful, even if they are not statistically significant. Further, because the small number of observations makes it difficult to definitively identify the best number of classes in LCA, our results should be considered illustrative rather than definitive.
RESULTS
Table 1 presents means of the covariates for the 64 States, Provinces, and Territories. The highest percentages of smoking and binge drinking, and nearly the highest percentages of obesity are found among Canadian Provinces or Territories that do not share a border with the U.S. The highest levels of the three fertility measures are found among U.S. States that do not share a border with Canada. With the exception of suicide mortality, the cause-specific mortality rates are also highest among the U.S. States that do not share a border with Canada. Separate analyses (not shown) find that the lower levels of mortality in Canada can be accounted for by the Canadian Territories. The Nunavut, Yukon, and Northwest Territories include large aboriginal populations who have relatively poor health behaviors, but who also have low mortality rates due to their young age distributions.
Table 1.
Mean Levels of Covariates, U.S. States and Canadian Provinces and Territories.
| Canadian Province/Territory | U.S. State | ||||
|---|---|---|---|---|---|
| No shared border with U.S. |
No shared border with U.S. |
Shared border with Canada |
No shared border with Canada |
p-valueb | |
| Health Lifestyle Variablesa | |||||
| Smoking, % | 25.6 | 17.9 | 20.3 | 21.2 | 0.045 |
| Obese, % | 23.5 | 17.2 | 23.6 | 24.7 | 0.016 |
| Binge drinking, % | 30.5 | 23.4 | 24.4 | 22.9 | 0.021 |
| Crude birth rate | 13.5 | 10.8 | 12.9 | 14.0 | 0.012 |
| Total fertility rate | 1.8 | 1.6 | 2.0 | 2.0 | 0.004 |
| Age specific fertility rate 15–19 | 38.5 | 17.5 | 28.9 | 42.9 | 0.002 |
| HIV mortality rate | 0.5 | 1.1 | 1.7 | 4.6 | 0.012 |
| Diabetes mortality rate | 21.4 | 26.1 | 24.6 | 26.2 | 0.635 |
| Liver disease mortality rate | 5.8 | 7.1 | 8.3 | 9.4 | 0.019 |
| Accident mortality rate | 36.2 | 37.6 | 39.6 | 42.4 | 0.516 |
| Motor vehicle accident | |||||
| mortality rate | 11.7 | 11.2 | 15.0 | 17.5 | 0.033 |
| Suicide mortality rate | 26.4 | 12.8 | 13.6 | 12.1 | 0.462 |
| Homicide mortality rate | 3.3 | 4.7 | 3.2 | 6.3 | 0.130 |
| Independent Variables | |||||
| Male, % | 50.0 | 49.8 | 49.7 | 49.2 | 0.071 |
| Age, % | 0.323 | ||||
| birth to 9 | 14.0 | 11.3 | 12.6 | 13.4 | |
| 10 to 19 | 15.6 | 13.7 | 14.3 | 14.0 | |
| 20 to 44 | 21.6 | 20.6 | 19.9 | 20.7 | |
| 45 to 54 | 15.2 | 15.5 | 14.6 | 14.5 | |
| 55 to 64 | 13.9 | 15.6 | 15.5 | 14.4 | |
| 65 or older | 9.9 | 10.8 | 10.8 | 10.4 | |
| Hospital beds | 3.84 | 3.41 | 3.02 | 3.03 | 0.973 |
| Family medicine doctors | 86.2 | 115.5 | 44.2 | 32.6 | 0.003 |
| Dental care past 12 mos, % | 55.5 | 57.7 | 72.1 | 69.9 | 0.003 |
| Foreign born, % | 3.7 | 14.3 | 6.9 | 8.8 | 0.058 |
| Race/ethnicity, % | 0.062 | ||||
| Black | 0.8 | 1.4 | 4.0 | 12.8 | |
| Aboriginal/Native American | 28.8 | 9.0 | 3.1 | 1.4 | |
| Others including whites | 70.4 | 89.6 | 92.9 | 85.8 | |
| Education | 0.009 | ||||
| Less than high school | 30.3 | 21.5 | 9.8 | 14.1 | |
| High school or some college | 54.6 | 60.1 | 60.8 | 58.8 | |
| College degree or more | 15.2 | 18.5 | 29.3 | 27.1 | |
| Unemployed, % | 11.0 | 6.7 | 5.0 | 5.0 | 0.010 |
| Crime | 0.34 | 0.43 | −0.57 | 0.03 | 0.020 |
| Number of observations | 5 | 8 | 11 | 40 | |
The crude birth rate is measured per 1,000 population, the age specific fertility rate is measured per 1,000 women, and the mortality rates are all measured per 100,000 population
Wald tests assess differences in the covariates across the four columns.
Hospital beds and family medicine or general practice doctors per capita are higher in Canada than the U.S., but receipt of dental care in the past year is lower in Canada. The percent of foreign born individuals is highest in Canadian Provinces or Territories that share a border with the U.S. The Black population is highest in U.S. States that do not share a border with Canada, and the Aboriginal/Native American population is largest in Canadian Provinces or Territories that do not share a border with the U.S. The share of the population that has less than a high school degree or that is unemployed is higher in Canada than the U.S. The crime index is higher in Canada, which is consistent with the higher rates of nonviolent crimes in Canada than in the U.S. (Statistics Canada 2001).
Table 2 presents regression coefficients from models that test for convergence in the health lifestyle variables at the U.S./Canada border (Aim 1). Model 1 includes dummy variables for nationality, international border, and the interaction between those dummy variables, and adjusts for age and sex. There are no significant differences in smoking, obesity, or binge drinking, but a persistent (although not always statistically significant) pattern emerges for the fertility and mortality variables. For all three fertility measures and all of the mortality outcomes except for diabetes, Canadian Provinces or Territories that do not border the U.S. have the lowest levels, followed by Provinces or Territories that border the U.S., States that border Canada, and States that do not border Canada. For example, the predicted crude birth rate per 1,000 population from Model 1 is 11.1 for Provinces and Territories that do not border the U.S., 11.6 for Provinces or Territories that border the U.S., 13.4 for States border Canada, and 13.8 for States that do not border Canada. Diabetes mortality exhibits a non-significant pattern of convergence, although it is higher in Canada than the U.S.
Table 2.
Unstandardized Regression Coefficients for the Average Level of the Health Lifestyle Outcomes, U.S. States and Canadian Provinces and Territories.a
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Percent smoking | |||
| Nationality (Canada=1) | −0.04 | −0.13 | −0.63 |
| International border | −0.10 | −0.09 | 0.05 |
| Nationality*international border | 0.02 | 0.08 | −0.10 |
| Percent obese | |||
| Nationality (Canada=1) | −0.14 | −0.32 | −0.42 |
| International border | −0.08 | −0.05 | 0.02 |
| Nationality*international border | −0.16 | −0.13 | −0.25 |
| Percent binge drinking | |||
| Nationality (Canada=1) | 0.25 | 0.25 | −0.06 |
| International border | −0.04 | −0.04 | −0.08 |
| Nationality*international border | −0.44 | −0.38 | −0.15 |
| Crude birth rate | |||
| Nationality (Canada=1) | −0.22*** | −0.29*** | −0.20*** |
| International border | −0.03* | −0.03** | −0.02** |
| Nationality*international border | 0.08** | 0.09*** | 0.05* |
| Total fertility rate | |||
| Nationality (Canada=1) | −0.38*** | 0.40*** | −0.22* |
| International border | −0.05 | −0.05 | −0.04 |
| Nationality*international border | 0.08 | 0.10 | −0.01 |
| Age specific fertility rate 15–19 | |||
| Nationality (Canada=1) | −24.80*** | −34.07*** | −41.36*** |
| International border | −8.95** | −7.39** | −4.00 |
| Nationality*international border | 17.20** | 17.30** | 10.99* |
| HIV mortality | |||
| Nationality (Canada=1) | −1.42** | −0.48 | −0.29 |
| International border | −0.29 | −0.23 | 0.04 |
| Nationality*international border | 1.06* | 0.97* | −0.25 |
| Diabetes mortality | |||
| Nationality (Canada=1) | 0.18 | −0.24 | −0.68*** |
| International border | 0.05 | 0.09 | 0.10 |
| Nationality*international border | −0.05 | −0.04 | 0.21 |
| Liver disease mortality | |||
| Nationality (Canada=1) | −0.74*** | −0.84*** | −1.10*** |
| International border | −0.17** | −0.16** | −0.12* |
| Nationality*international border | 0.37** | 0.34* | 0.30 |
| Accident mortality | |||
| Nationality (Canada=1) | −0.59*** | −1.09*** | −1.05*** |
| International border | −0.21** | −0.17** | −0.12* |
| Nationality*international border | 0.50*** | 0.43*** | 0.32** |
| Motor vehicle accident mortality | |||
| Nationality (Canada=1) | −0.77*** | −1.50*** | −1.34*** |
| International border | −0.28** | −0.24*** | −0.15** |
| Nationality*international border | 0.68*** | 0.68*** | 0.35* |
| Suicide mortality | |||
| Nationality (Canada=1) | −0.08 | −0.27 | −0.64*** |
| International border | −0.09 | −0.07 | −0.05 |
| Nationality*international border | 0.27 | 0.26 | 0.45*** |
| Homicide mortality | |||
| Nationality (Canada=1) | −2.20*** | −2.83*** | −2.53*** |
| International border | −0.54*** | −0.39** | −0.10 |
| Nationality*international border | 1.90*** | 1.52*** | 0.52 |
p≤0.10;
p≤0.05;
p≤0.01 (2-tailed tests)
Model 1 adjusts for age and sex. Model 2 further adjusts for hospital beds, family medicine doctors, and dental care utilization. Model 3 further adjusts for immigration, race/ethnicity, education, unemployment, and crime.
After adjusting for hospital beds, family medicine doctors, and utilization of dental care in Model 2, the gap between U.S. States and Canadian Provinces or Territories either remained unchanged or became larger in magnitude for the three fertility measures and all of the causes of death except for HIV and diabetes mortality. Healthcare availability and utilization attenuated U.S./Canada differences in HIV mortality, but otherwise could not account for health lifestyle differences between the U.S. States and the Canadian Provinces and Territories.
Model 3 further includes the sociodemographic factors, including immigration, race/ethnicity, education, unemployment, and crime. The coefficients for nationality, shared border, and their interaction are attenuated for the crude birth rate, total fertility rate, HIV mortality, accident mortality, motor vehicle accident mortality, and homicide mortality. However, the coefficients for several of the outcomes become larger in absolute magnitude, including the age-specific fertility rate, diabetes mortality (which is now significantly lower in Canada than the U.S.), liver disease mortality, and suicide mortality. Thus, adjusting for the sociodemographic variables partially accounts for national differences in some health lifestyle outcomes.
Table 3 shows the number of U.S. States and Canadian Provinces or Territories in each latent class, to assess whether there are similarities in health lifestyles among U.S. and Canadian areas, regardless of shared borders (Aim 2). The classes are based on similar patterns in the observed health lifestyle variables. The order of the classes within each model is arbitrary; we list the classes that have both U.S. and Canadian observations first, from classes with the most observations to those with the fewest.
Table 3.
Numbers of U.S. States and Canadian Provinces or Territories in Each Class, by the Number of Classes Assumed in Each Latent Class Model.
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| U.S. | Can | U.S. | Can | U.S. | Can | U.S. | Can | U.S. | Can | U.S. | Can | U.S. | Can | U.S. | Can | |
| Class | ||||||||||||||||
| 1 | 51 | 12 | 43 | 1 | 27 | 11 | 24 | 3 | 25 | 3 | 22 | 2 | 17 | 2 | 19 | 2 |
| 2 | 0 | 1 | 8 | 11 | 23 | 1 | 4 | 9 | 4 | 8 | 4 | 8 | 3 | 8 | 4 | 8 |
| 3 | 0 | 1 | 1 | 0 | 22 | 0 | 21 | 0 | 8 | 1 | 10 | 1 | 14 | 0 | ||
| 4 | 0 | 1 | 1 | 0 | 1 | 0 | 16 | 0 | 14 | 0 | 12 | 0 | ||||
| 5 | 0 | 1 | 0 | 1 | 1 | 0 | 6 | 0 | 1 | 0 | ||||||
| 6 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | ||||||||
| 7 | 0 | 1 | 0 | 1 | 0 | 1 | ||||||||||
| 8 | 0 | 1 | 0 | 1 | ||||||||||||
| 9 | 0 | 1 | ||||||||||||||
| AIC | 2215 | 2056 | 1911 | 1807 | 1715 | 1633 | 1603 | 1569 | ||||||||
| BIC | 2310 | 2190 | 2084 | 2019 | 1965 | 1923 | 1931 | 1936 | ||||||||
Model 1 allows for two classes and shows that the first class holds 63 observations, 51 from the U.S. and 12 from Canada. The second class holds a single observation, the Canadian Territory of Nunavut. Ancillary analyses (not shown) find that the AIC and BIC are smaller (indicating a better model fit) for the two-class model than a model that permits only one class. Several trends emerge in Models 2 through 8. First, all of the models find multiple classes that hold observations from both the U.S. and Canada; at least some regions of each country share patterns on the health lifestyle variables. Second, in addition to Nunavut (identified in Model 1), Washington D.C. (first identified in Model 3) and the Yukon Territory (first identified in Model 5) have such distinctive health lifestyle patterns that they form classes of their own. Third, beginning in Model 4, we find evidence of a class that is comprised solely of multiple U.S. States but no Canadian observations. None of the models identified a class that held only multiple Canadian observations. Finally, the BIC indicates that Model 6 fits better than models with more or less classes. The AIC continues to decline for Models 7 and 8, but it declines by smaller increments than for prior models.
Table 4 presents the means of the covariates across the seven classes estimated in Model 6 on Table 3, with the States, Provinces, and Territories in each class listed in the footnotes. Classes 1 through 4 each contain multiple observations and reflect health lifestyles that are shared across geographic areas. The observations in class 1 are moderately healthy and have relatively healthy behaviors, low levels of mortality from most causes, and moderately low levels of fertility. Class 2 is the healthiest group that contains multiple observations as indicated by low levels of smoking, obesity, and binge drinking; the lowest levels of mortality from all causes except for HIV and diabetes; and the lowest levels of total and teenage fertility.
Table 4.
Means of Covariates Across the Latent Health Lifestyle Classes Identified in Table 3, Model 6, U.S. States and Canadian Provinces and Territories.a
| Class 1: Moderate healthy |
Class 2: Most healthy |
Class 3: Moderate unhealthy |
Class 4: Most unhealthy |
Class 5: Washington D.C. |
Class 6: Nunavut territory |
Class 7: Yukon territory |
p-value | |
|---|---|---|---|---|---|---|---|---|
| Health Lifestyle Variables | ||||||||
| Smoking, % | 19.7 | 18.0 | 20.6 | 23.5 | 20.1 | 46.1 | 25.7 | 0.013 |
| Obese, % | 23.5 | 19.5 | 23.1 | 27.1 | 21.7 | 25.9 | 17.8 | 0.003 |
| Binge drinking, % | 24.4 | 24.2 | 24.7 | 21.1 | 27.5 | 32.3 | 27.9 | 0.066 |
| Crude birth rate | 13.2 | 10.3 | 15.7 | 14.2 | 14.5 | 23.3 | 10.3 | 0.005 |
| Total fertility rate | 2.0 | 1.6 | 2.2 | 2.1 | 1.8 | 2.7 | 1.5 | 0.019 |
| Age specific fertility rate 15–19 | 33.0 | 16.2 | 39.7 | 52.4 | 63.4 | 107.9 | 12.2 | 0.016 |
| HIV mortality rate | 3.1 | 1.3 | 1.1 | 4.5 | 42.6 | 0.0 | 0.0 | 0.101 |
| Diabetes mortality rate | 25.9 | 26.4 | 19.2 | 29.0 | 40.5 | 0.0 | 16.2 | 0.046 |
| Liver disease mortality rate | 8.3 | 7.5 | 8.6 | 10.3 | 12.8 | 0.0 | 9.7 | 0.055 |
| Accident mortality rate | 35.5 | 32.2 | 42.8 | 51.3 | 39.6 | 47.2 | 81.0 | 0.006 |
| Motor vehicle accident mortality rate | 12.8 | 11.0 | 18.2 | 22.7 | 8.3 | 16.9 | 19.4 | 0.003 |
| Suicide mortality rate | 10.5 | 10.9 | 18.8 | 13.2 | 6.0 | 80.9 | 19.4 | 0.014 |
| Homicide mortality rate | 4.3 | 1.4 | 4.2 | 7.6 | 31.4 | 10.1 | 22.7 | 0.002 |
| Geographic Factors | ||||||||
| Percent Canadian Prov/Terr | 8.3 | 66.7 | 11.1 | 0.0 | 0.0 | 100.0 | 100.0 | 0.017 |
| Percent with international border | 29.2 | 66.7 | 33.3 | 0.0 | 0.0 | 0.0 | 100.0 | 0.475 |
| Independent Variables | ||||||||
| Male, % | 49.2 | 49.2 | 50.6 | 49.0 | 46.9 | 51.7 | 50.6 | 0.037 |
| Age, % | 0.968 | |||||||
| birth to 9 | 12.9 | 10.9 | 14.5 | 13.6 | 11.1 | 23.7 | 11.3 | |
| 10 to 19 | 14.1 | 13.3 | 14.8 | 14.0 | 12.3 | 21.4 | 14.8 | |
| 20 to 44 | 34.8 | 35.2 | 36.1 | 34.9 | 41.2 | 38.1 | 37.4 | |
| 45 to 54 | 14.7 | 15.7 | 14.5 | 14.1 | 13.1 | 9.0 | 18.4 | |
| 55 to 64 | 10.4 | 11.5 | 9.8 | 10.6 | 10.1 | 5.0 | 11.3 | |
| 65 or older | 13.0 | 13.3 | 10.3 | 12.8 | 12.2 | 2.7 | 6.8 | |
| Hospital beds | 2.92 | 3.36 | 3.43 | 3.16 | 6.20 | 1.10 | 1.90 | 0.760 |
| Family medicine doctors | 39.4 | 83.6 | 46.5 | 31.6 | 37.7 | 27.0 | 207.4 | 0.013 |
| Dental care past 12 mos, % | 72.3 | 63.2 | 68.2 | 65.4 | 71.8 | 53.5 | 50.6 | 0.018 |
| Foreign born, % | 10.1 | 10.2 | 7.1 | 6.7 | 12.7 | 1.5 | 9.9 | 0.568 |
| Race/ethnicity, % | 0.070 | |||||||
| Black | 8.7 | 1.7 | 2.1 | 16.7 | 55.4 | 0.3 | 0.4 | |
| Aboriginal/Native American | 2.1 | 2.2 | 9.8 | 1.8 | 0.4 | 85.0 | 25.1 | |
| Others including whites | 89.2 | 96.1 | 88.1 | 81.4 | 44.2 | 14.7 | 74.5 | |
| Education | 0.125 | |||||||
| Less than high school | 13.0 | 18.2 | 11.7 | 17.3 | 16.7 | 47.8 | 17.9 | |
| High school or some college | 58.7 | 58.9 | 63.1 | 59.8 | 34.2 | 40.0 | 61.7 | |
| College degree or more | 28.4 | 22.9 | 25.2 | 23.0 | 49.1 | 12.2 | 20.4 | |
| Unemployed, % | 5.0 | 7.5 | 4.8 | 5.3 | 7.6 | 13.0 | 6.1 | 0.099 |
| Crime | −0.06 | −0.35 | −0.22 | 0.12 | 3.18 | 1.86 | 0.57 | 0.489 |
Class 1: California, Connecticut, Delaware, Hawaii, Illinois, Indiana, Iowa, Kansas, Maryland, Michigan, Minnesota, Nebraska, New Jersey, New York, North Dakota, Ohio, Oregon, Pennsylvania, Rhode Island, Virginia, Washington, Wisconsin (U.S.) and Manitoba, Saskatchewan (Canada). Class 2: Maine, Massachusetts, New Hampshire, Vermont (U.S.) and Alberta, British Columbia, New Brunswick, Newfoundland and Labrador, Nova Scotia, Ontario, Prince Edward Island, Quebec (Canada). Class 3: Alaska, Colorado, Idaho, Montana, Nevada, South Dakota, Utah, Wyoming (U.S.) and Northwest Territories (Canada). Class 4: Alabama, Arizona, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, Missouri, New Mexico, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, West Virginia (U.S.).
The observations in class 3 are moderately unhealthy. Compared to classes 1 and 2, class 3 has higher levels of binge drinking and teenage fertility, and higher rates of liver disease, accidents, motor vehicle accidents, and suicide mortality, but lower rates of HIV and diabetes mortality. Class 4 is the least healthy of the classes that have multiple observations and has the highest percentages of smokers and obesity, the highest teenage fertility rate, and the highest rates of death from all causes except for suicide.
Of the classes that hold multiple States, Provinces, or Territories, class 2 (the healthiest class) has the highest percentage of observations from Canada, and class 4 (the least healthy class) has no observations from Canada. Nevertheless, within classes 1, 2, and 3, there are substantial numbers of observations from both countries. Class 2 (the most healthy class) has the highest number of family medicine doctors per capita and the fewest Blacks or Aborignals/Native Americans, but the highest levels of unemployment, and the lowest levels of education or dental care in the past 12 months. In contrast, classes 3 and 4 (the less healthy classes) are notable for their high percentages of Aboriginals/Native Americans or Blacks, respectively, and their low numbers of family medicine doctors per capita.
Class 5 (Washington D.C.), class 6 (Nunavut), and class 7 (Yukon) have health lifestyle patterns that are held by single observations. Both Washington D.C. and Nunavut have very high teenage fertility rates, and Washington D.C. also has very high levels of mortality from HIV, diabetes, liver disease, and homicide. Washington D.C. has many Blacks and high rates of unemployment and crime, but high levels of education and numerous hospital beds per capita. Nunavut has high levels of smoking, fertility, and suicide; low levels of education and dental care; and high levels of crime and unemployment. But Nunavut has no mortality from HIV, diabetes, or liver disease due to its young population. The Yukon has low levels of teenage fertility and diabetes mortality, high levels of accident mortality, and many doctors per capita.
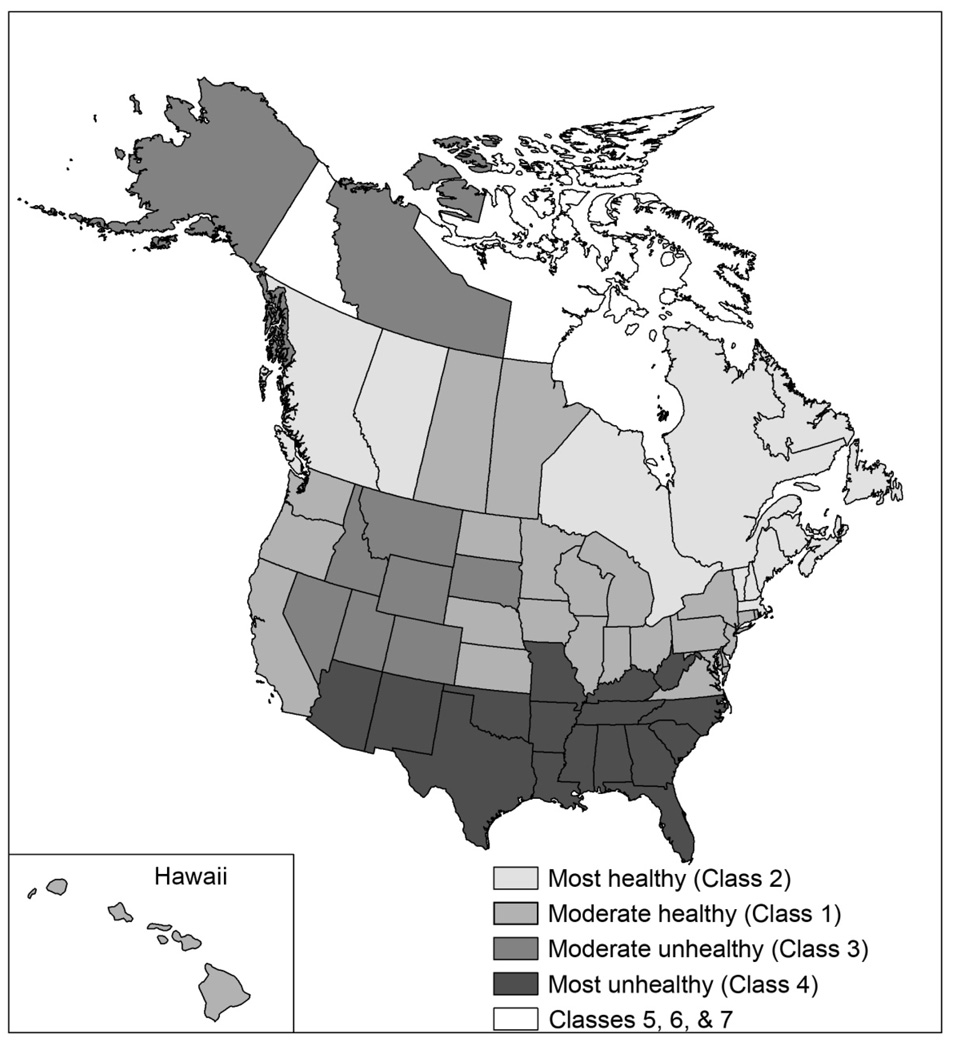
Figure 1 maps the observations in the classes described in Table 4, and reveals spatial patterns that are not defined solely by shared international borders. Class 1 is comprised largely of States in the Midwestern, Eastern, and West Coast (including Hawaii) U.S., and two Provinces in central Canada. Class 2 contains U.S. States and Canadian Provinces in the most Northeastern parts of North America, as well as two provinces in Western Canada. Class 3 is largely comprised of the Rocky Mountain region of the United States, along with Alaska and the Northwest Territories of Canada. Class 4—the least healthy class—is comprised solely of Southern and Southwestern U.S. States.
Figure 1.
Health Lifestyle Regions of the U.S. and Canada
CONCLUSION
Our first aim was to examine whether the health lifestyle variables converge at the U.S./Canada border. Consistent with the claims made by cultural studies researchers (Adams 2003; Byers 2007; Cohen 2007), we find important differences in health lifestyle between the U.S. and Canada. Compared to the U.S., Canada had lower crude birth rates, total fertility rates, and teenage fertility rates, and lower mortality rates from HIV, liver disease, accidents, motor vehicle accidents, and homicide, after adjusting for age and sex.
But we also found evidence of convergence in the health lifestyle variables at the U.S./Canada border. States, Provinces, and Territories that have an international border exhibit midrange levels on the health lifestyle variables, with greater differences between areas of the U.S. and Canada that do not border. This convergence is consistent with prior research that focuses on trade and social policies (Abgrall 2005; Anderson and Smith 1999; Boucher 2005; Evans 2007), and with research that finds that membership in sports and cultural organizations is similar in the U.S. and Canada (Helliwell 2003).
Health lifestyle theories suggest that orientations toward health are shaped by important social, cultural, economic, political, and historical factors (Bourdieu 1984; Cockerham 2000; Cockerham, Rutten, and Abel 1997). Healthcare availability (i.e., hospital beds and family medicine doctors per capita) and utilization (i.e., dental care utilization) were largely able to account for U.S./Canada differences in HIV mortality. But the greater availability of healthcare in Canada did not generally account for their better health, potentially because some healthcare services may provide few health benefits (Mansfield et al. 1999). Separate analyses (not shown) examined whether states with high rates of health insurance were the most similar to Canadian Provinces and Territories (Sanmartin et al. 2006), but the health insurance variable was too collinear with the indicator for nationality to be included in our final analyses.
The sociodemographic variables that are the primary focus of population health researchers and social epidemiologists (Berkman and Kawachi 2000; Link and Phelan 2005) were able to attenuate (but seldom fully close) U.S./Canada differences in two measures of total fertility and four of the causes of death. In contrast, national differences in diabetes and suicide mortality only became apparent after adjusting for the sociodemographic variables. Neither our healthcare nor sociodemographic variables could fully explain national differences in the health lifestyle variables. Although data on income inequality or the availability or utilization of public parks or sidewalks were unavailable to us, such variables may further help to explain health lifestyle differences between the U.S. and Canada.
Our second aim was to examine patterns in the health lifestyle variables among U.S. States and Canadian Provinces and Territories, regardless of whether they share an international border. Our models consistently identified two or three classes that held observations from both the U.S. and Canada. At least in terms of health lifestyles, Canada is not as different from the U.S. as some cultural studies scholars might suggest (Adams 2003; Byers 2007; Cohen 2007)— none of the classes that held multiple observations were comprised solely of Canadian Provinces or Territories. But Washington D.C. and the Yukon and Nunavut territories did not share similar health lifestyle patterns with any other State, Province, or Territory in our analyses. In contrast, the U.S. South and Southwest exhibit distinctive health lifestyle patterns that are not shared with any Province or Territory in Canada.
Our analyses include multiple strengths. First, we use multiple population health indicators to examine health lifestyles, a domain that has received little attention in prior research that compares the U.S. and Canada. We have greater confidence in our findings of convergence at the U.S./Canada border, given that the estimated relationships are similar for multiple outcomes. Second, our analyses demonstrate the importance of understanding variation within and between nations. Prior work often examines national means for selected covariates, but we found substantial variation within countries throughout our analyses. Finally, we use an innovative method—latent class analysis—to identify shared health lifestyle patterns.
Several limitations warrant mention. First, two of the dependent variables were measured differently between the U.S. and Canada. Smoking was assessed for those aged 18 and older in the U.S., but for those aged 12 or older in Canada. The binge drinking variables were assessed for different time periods. U.S. respondents were asked about binge drinking on at least one occasion in the last 30 days, but Canadian respondents were asked about binge drinking on at least 12 occasions in the past year. But the variables for obesity, fertility, and causes of death were measured using the same definitions across the U.S. and Canada, in part because many of those are key variables that nations use to track the health of their populations (Poston and Micklin 2006). Importantly, the results from our latent class analyses were virtually unchanged when excluding the variables for smoking and binge drinking.
Second, our variables are measured at different time points, depending on their availability for both the U.S. and Canada. The mortality, crime, unemployment, and healthcare data come from 2004; the health behavior, fertility, and age and sex variables came from 2005; and the data for immigration, education, and race/ethnicity come from 2006. But the marked continuity in aggregate variables over time suggests that measuring our variables across 3 years likely introduces little error into our analyses. Finally, although States, Provinces, and Territories offer distinctive policy and legal environments that might shape health lifestyles, there is substantial variation between rural and urban areas, or across large geographic areas that we could not examine, due to the limited data available for smaller unites of analysis.
By identifying important similarities between some U.S. States and some Canadian Provinces and Territories, our results may aid the development of international collaboration in the design of health policies. Indeed, health policies that are found to be effective in some areas may be similarly effective across the international border in areas that share similar health lifestyle patterns. Policy makers might also use our results to identify specific regions within their own countries that merit specific attention. The U.S. South and Southwest are distinctive in their very unhealthy behaviors, high levels of teenage fertility, and high levels of mortality from many lifestyle related causes. Further, Washington D.C. and the Nunavut and Yukon Territories exhibit unique health lifestyle patterns, so local policy makers in those places may need to be especially innovative in their approaches to improving population health.
In sum, the U.S. and Canada are both different and similar. On average, Canada has lower fertility and lower rates of death from many causes. But we also find important similarities in health lifestyles—key indicators of population health—along the U.S./Canada border and for specific regions within each country. Policy makers may benefit from finding peers within their own country or across the international border when seeking to understand the consequences of health lifestyle factors for health care financing, or when looking for similar populations that have tried policies (successful or not) that aim to improve population health. Both the U.S. and Canada may achieve a better understanding of the health of their populations and improve their health policy knowledge by looking to areas across the border.
Footnotes
Direct all correspondence to the first author at University of Texas School of Public Health, 1200 Herman Pressler, RAS E-907, Houston, TX, 77030; Patrick.M.Krueger@uth.tmc.edu. Upon request, the first author will share all data and coding information to those who wish to replicate our study. We thank Tom Dickenson for his help with mapping the results in this article, and acknowledge administrative support from the University of Texas Population Research Center (NICHD R24 HD42849) and the University of Colorado Population Program (NICHD R21 HD51146).
Contributor Information
Patrick M. Krueger, University of Texas School of Public Health
Tajudaullah Bhaloo, University of Texas School of Public Health.
Pauline Vaillancourt Rosenau, University of Texas School of Public Health.
REFERENCES
- Abgrall Jean-Francois. A Survey of Major Cross-Border Organizations between Canada and the United States. Ottawa, ON: Policy Research Initiative, Government of Canada; 2005. [Google Scholar]
- Adams Michael. Fire and Ice: The United States, Canada and the Myth of Converging Values. Toronto: Penguin Press; 2003. [Google Scholar]
- Anand Sonia S, Yusef Salim, Jacobs Ruby, Darlene Davis A, Yi Qilong, Gerstein Hertzel, Montague Patricia A, Lonn Eva. Risk Factors, Atherosclerosis, and Cardiovascular Disease among Aboriginal People in Canada" The Study of Health Assessment and Risk Evaluation in Aboriginal Peoples (Share-Ap) The Lancet. 2001;358:1147–1153. doi: 10.1016/s0140-6736(01)06255-9. [DOI] [PubMed] [Google Scholar]
- Anderson JE, van Wincoop E. Gravity with Gravitas: A Solution to the Border Puzzle. American Economic Review. 2003;93:170–192. [Google Scholar]
- Anderson Michael, Smith Stephen. Do National Borders Really Matter? Canada-US Regional Trade Considered. Review of International Economics. 1999;7:219–227. [Google Scholar]
- Antecol Heather, Bedard Kelly. Unhealthy Assimilation: Why Do Immigrants Converge to American Health Status Levels? Demography. 2006;43:337–360. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- Berkman Lisa F, Kawachi Ichiro. Social Epidemiology. New York: Oxford University Press; 2000. [Google Scholar]
- Boucher Christian. Toward North American or Regional Cross-Border Communities: A Look at Economic Integration and Socio-Cultural Values in Canada and the United States. Ottawa, ON: Policy Research Initiative, Government of Canada; 2005. [Google Scholar]
- Bourdieu Pierre. In: Distinction: A Social Critique of the Judgment of Taste. Nice Richard., editor. Cambridge, MA: Harvard University Press; 1984. Translated by. [Google Scholar]
- Byers Michael. Intent for a Nation: What Is Canada For? Toronto, ON: Douglas and McIntyre; 2007. [Google Scholar]
- Canadian Institute for Health Information. Supply, Distribution, and Migration of Canadian Physicians, 2007. Ottawa, Ont: CIHI; 2008. [Google Scholar]
- Centers for Disease Control. Behavioral Risk Factor Surveillance System. 2008 Retrieved from http://www.cdc.gov/brfss on May, 2008.
- Cockerham William C. The Sociology of Health Behavior and Health Lifestyles. In: Bird Chloe E, Conrad Peter, Fremont Allen M., editors. Handbook of Medical Sociology (5th Ed.) Upper Saddle River, NJ: Prentice Hall; 2000. pp. 159–172. [Google Scholar]
- Cockerham William C, Rutten Alfred, Abel Thomas. Conceptualizing Contemporary Health Lifestyles: Moving Beyond Weber. The Sociological Quarterly. 1997;38:321–342. [Google Scholar]
- Cohen Andrew. The Unfinished Canadian. Toronto: McClelland and Stewart; 2007. [Google Scholar]
- Downs André, Sawchuk Gary. Do Cross-Border Regions Matter for Trade? Canada-US Border Effects and Cross-Border Regions. Ottawa, ON: Policy Research Initiative, Government of Canada; 2007. [Google Scholar]
- Dunn James R, Dyck Isabel. Social Determinants of Health in Canada's Immigrant Population: Results from the National Population Health Survey. Social Science & Medicine. 2000;51:1573–1593. doi: 10.1016/s0277-9536(00)00053-8. [DOI] [PubMed] [Google Scholar]
- Evans Carolyn L. National Border Effects: Location, Not Nationality, Matters. Review of International Economics. 2007;15:347–369. [Google Scholar]
- Ezzati Majid, Martin Hilarie, Skjold Suzanne, Vander Hoom Stephen, Murray Christopher J L. Trends in National and State-Level Obesity in the USA after Correction for Self-Report Bias: Analysis of Health Surveys. Journal of the Royal Society of Medicine. 2006;99:250–257. doi: 10.1258/jrsm.99.5.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Bureau of Investigation. Crime in the United States, 2004. Washington, DC: U.S. Department of Justice; 2005. [Google Scholar]
- Frolich Katherine L, Corin Ellen, Potvin Louise. A Theoretical Proposal for the Relationship between Context and Disease. Sociology of Health and Illness. 2001;23:776–797. [Google Scholar]
- Halli Shiva S, Anchan John P. Structural and Behavioral Determinants of Immigrant and Non-Immigrant Health Status: Results from the Canadian Community Health Survey. Journal of International Migration and Integration. 2005;6:93–123. [Google Scholar]
- Helliwell John F. Do Borders Matter for Social Capital? Economic Growth and Civic Culture in U.S. States and Canadian Provinces. In: Osberg Lars., editor. The Economic Implications of Social Cohesion. Toronto, ON: University of Toronto Press; 2003. pp. 19–42. [Google Scholar]
- Kaiser Family Foundation. State Health Facts. 2008 Retrieved from www.statehealthfacts.org on December, 2008.
- Kaiserman Murray J, Rogers Byron. Tobacco Consumption Declining Faster in Canada Than in the US. American Journal of Public Health. 1991;81:902–904. doi: 10.2105/ajph.81.7.902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Xiaojing, Kolltveit Kristin M, Tronstad Leif, Olsen Ingar. Systemic Diseases Caused by Oral Infection. Clinical Microbiology Reviews. 2000;13:547–558. doi: 10.1128/cmr.13.4.547-558.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link Bruce G, Phelan Jo. Fundamental Sources of Health Inequlities. In: Mechanic David, Rogut Lynn B, Colby David C, Knickman James R., editors. Policy Challenges in Modern Health Care. Piscataway, NJ: Rutgers University; 2005. pp. 71–84. [Google Scholar]
- Magidson Jay, Vermunt Jeroen K. Latent Class Analysis. In: Kaplan David., editor. The Sage Handboodk of Quantitative Methodology for the Social Sciences. Thousand Oaks, CA: Sage Publications; 2004. pp. 175–198. [Google Scholar]
- Mansfield Christopher J, Wilson James L, Kobrinski Edward J, Mitchell Jim. Premature Mortality in the United States: The Roles of Geographic Area, Socioeconomic Status, Household Type, and Availability of Medical Care. American Journal of Public Health. 1999;89:893–898. doi: 10.2105/ajph.89.6.893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin Joyce A, Hamilton Brady E, Sutton Paul D, Ventura Stephanie J, Menacker Fay, Kirmeyer Sharon, Munson Martha L. Births: Final Data for 2005. vol. 56. Hyattsville, MD: National Center for Health Statistics; 2007. [PubMed] [Google Scholar]
- McLaren Dawn, Hunter Pamela, Sherman Brian. A Pilot Study of Bilateral Trade between Canada and Arizona. 2006 Retrieved from www.canaz.net on May 30, 2008. [Google Scholar]
- Miniño Araldi M, Heron Melonie P, Murphy Sherry L, Kochanek Kenneth D. Deaths: Final Data for 2004. vol. 55. Hyattsville, MD: National Center for Health Statistics; 2007. [PubMed] [Google Scholar]
- Minister of Industry. Births: 2005. Ottawa, ON: Statistics Canada; 2007a. [Google Scholar]
- Minister of Industry. Mortality, Summary List of Causes. Ottawa, ON: Statistics Canada; 2007b. [Google Scholar]
- Mirowsky John, Ross Catherine E. Education, Social Status, and Health. Hawthorne, NY: Aldine De Gruyter; 2003. [Google Scholar]
- Mokdad Ali H, Marks James S, Stroup Donna F, Gerberding Julie L. Actual Causes of Death in the United States 2000. Journal of the American Medical Association. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Mokdad Ali H, Serdula Mary K, Dietz William H, Bowman Barbara A, Marks James S, Koplan Jeffrey P. The Spread of the Obesity Epidemic in the United States, 1991–1998. Journal of the American Medical Association. 1999;282:1519–1522. doi: 10.1001/jama.282.16.1519. [DOI] [PubMed] [Google Scholar]
- Muthén Linda K, Muthén Bengt O. Mplus User's Guide: Statistical Analysis with Latent Variables (5th Ed.) Los Angeles, CA: Muthén & Muthén; 2007. [Google Scholar]
- Pickle Linda W, Mungiole Michael, Gillum Richard F. Geographic Variation in Stroke Mortality in Blacks and Whites in the United States. Stroke. 1997;28:1639–1647. doi: 10.1161/01.str.28.8.1639. [DOI] [PubMed] [Google Scholar]
- Poston Dudley L, Micklin Michael. Handbook of Population. New York: Springer; 2006. [Google Scholar]
- Preston Samuel H, Heuveline Patrick, Guillot Michel. Malden, MA: Blackwell; 2001. Demography: Measuring and Modeling Population Processes. [Google Scholar]
- Preston Samuel H, Taubman P. Socioeconomic Differences in Adult Mortality and Health Status. In: Martin Linda G, Preston Samuel H., editors. Demography of Aging. Washington, D.C: National Academy Press; 1994. pp. 279–318. [Google Scholar]
- Putnam Robert D. Bowling Alone: The Collapse and Revival of American Community. New York: Simon & Schuster; 2000. [Google Scholar]
- Rosenau, Vaillancourt Pauline M. U.S. Newspaper Coverage of the Canadian Health System - a Case of Seriously Mistaken Identity? The American Review of Canadian Studies. 2006;36:27–58. [Google Scholar]
- Ross Nancy A, Wolfson Michael C, Dunn James R, Berthelot Jean-Marie, Kaplan George A, Lynch John W. Relation between Income Inequality and Mortality in Canada and in the United States: Cross Sectional Assessment Using Census Data and Vital Statistics. British Medical Journal. 2000;320:898–902. doi: 10.1136/bmj.320.7239.898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanmartin Claudia, Berthelot Jean-Marie, Ng Edward, Murphy Kellie, Blackwell Debra L, Gentleman Jane F, Martinez Michael E, Simile Catherine. Comparing Health and Health Care Use in Canada and the United States. Health Affairs. 2006;25:1133–1142. doi: 10.1377/hlthaff.25.4.1133. [DOI] [PubMed] [Google Scholar]
- Sauvé Julie. Crime Statistics in Canada, 2004. Juristat: Statistics Canada; 2005. [Google Scholar]
- Smart Derek R. Physician Characteristics and Distribution in the U.S., 2007 Edition. Chicago, IL: American Medical Association; 2007. [Google Scholar]
- Smith Joel. Fire and Ice: A Book Review. American Review of Canadian Studies. 2005;35:157. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 10.0. College Station, TX: Stata Press; 2007. [Google Scholar]
- Statistics Canada. The Daily: Crime Comparisons between Canada and the United States,2000. 2001 Retrieved from www.statcan.gc.ca on December, 2008. [Google Scholar]
- Statistics Canada. Canada's National Statistical Agency. 2008 Retrieved from http://www.statcan.ca/ on May, 2008. [Google Scholar]
- Stephens Thomas, Pederson Linda L, Koval John J, Macnab Jennifer. Comprehensive Tobacco Control Policies and the Smoking Behaviour of Canadian Adults. Tobacco Control. 2001;10:317–322. doi: 10.1136/tc.10.4.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tauras John A. Public Policy and Smoking Cessation among Young Adults in the United States. Health Policy. 2003;68:321–332. doi: 10.1016/j.healthpol.2003.10.007. [DOI] [PubMed] [Google Scholar]
- U.S. Bureau of the Census. U.S. Census Bureau, Current Population Survey (Cps) 2008 Retrieved from http://www.census.gov/cps/ on December, 2008.
- Vanasse A, Demers M, Heriari A, Courteau J. Obesity in Canada: Where and How Many? International Journal of Obesity. 2006;30:677–683. doi: 10.1038/sj.ijo.0803168. [DOI] [PubMed] [Google Scholar]
- Vandegrift Donald, Yoked Tommer. Obesity Rates, Income, and Urban Sprawl: An Analysis of US States. Health and Place. 2004;10:221–229. doi: 10.1016/j.healthplace.2003.09.003. [DOI] [PubMed] [Google Scholar]
- White Bill. Message from the Mayor. International Newsletter, Office of International Affairs & Development, City of Houston. 2006;2(1) [Google Scholar]
- Williams David R, Collins Chiquita. U.S. Socioeconomic and Racial Differences in Health: Patterns and Explanations. Annual Review of Sociology. 1995;21:349–386. [Google Scholar]