Abstract
Medicare policymakers have recently become interested in changing the payment incentives around rehospitalizations. Using merged claims data, our analyses indicate 23.5% of Medicare beneficiaries discharged from the hospital to a skilled nursing facility (SNF) were directly readmitted within 30 days at a cost to Medicare of $4.34 billion in 2006. Although these results indicate significant potential savings, we also found that SNF rehospitalizations were heterogeneous in nature and varied considerably across local areas based on practice patterns. Medicare payment reform needs to account for incentives that vary geographically and by type of hospitalization in order to be effective.
Introduction
The rehospitalization of Medicare beneficiaries has emerged as an important area of interest for policymakers. These rehospitalizations have been shown to be frequent, costly, and often preventable. Jencks and colleagues [1] found that almost one-fifth (19.6%) of all Medicare beneficiaries were rehospitalized within 30 days in 2004. Approximately 90% of these rehospitalizations were unplanned, with an estimated cost to the Medicare program of $17.4 billion. This high rate of rehospitalization is due to numerous factors, including the Medicare services received following discharge such as post-acute care (i.e., recuperative or rehabilitative services provided to beneficiaries after acute-care hospital stays) delivered by a skilled nursing facility (SNF), home health care agency or inpatient rehabilitation facility. Roughly 40% of Medicare beneficiaries are discharged to a post-acute setting, with roughly half of these to a SNF, which is a nursing home (or distinct part of a nursing home) devoted to providing skilled nursing care or rehabilitation services.[2]
Importantly, there is considerable geographic variation in both Medicare re-admissions and the use of post-acute care services. In an analysis of 30-day Medicare spending following a hospital discharge, the Medicare Payment Advisory Commission (MedPAC) [3] found that much of the observed variation between hospitals was related to readmissions and post-acute services such as SNF care. Although their analysis did not consider the effect of this spending on quality-of-care, some of this variation presumably reflects inefficient spending on the part of providers.
In this context, Medicare policymakers have become interested in changing the payment incentives around hospital readmissions. Currently, Medicare pays for all readmissions except when patients are rehospitalized within 24 hours after discharge for the same condition for which they were originally hospitalized. There is little incentive for hospitals, SNFs and other providers to coordinate beneficiaries’ care and address wasteful rehospitalizations that occur as a result of inadequate clinical information sharing, inappropriate post-acute placements or other inefficiencies across providers.[4-6] Moreover, in the case of many nursing home residents who have lived in a facility for some time (i.e., long-stay residents), this issue is further magnified given Medicaid’s role as the primary payer of nursing home care. Given Medicare’s coverage of SNF and hospital services, there are often perverse incentives for both providers and payers to shift costs across settings for dually-eligible beneficiaries.[7]
Both MedPAC [3] and the Senate Finance Committee [8] have proposed a bundled Medicare payment system for hospital episodes to encompass the base hospitalization, readmissions, physician services, post-acute care, and other Medicare services. At the margin, this type of payment system would provide a single entity with the incentive to reduce inefficient readmissions, because readmissions would not generate additional revenue under a bundled payment. Additionally, there are also proposed Medicare reforms such as nursing home pay-for-performance (P4P) that have targeted SNF rehospitalizations as a source of potential cost savings.
In spite of the importance of SNF rehospitalizations in recent payment reform discussions, there has not been previous published research documenting their frequency and costs. Moreover, little is known about the underlying nature of these rehospitalizations or how they vary geographically. Thus, the purpose of this paper is to examine SNF rehospitalizations in order to inform current policy discussions.
Background on SNF Rehospitalizations
Over the last several decades, the role of the nursing home has changed dramatically from a purely residential setting where predominantly older, cognitively impaired and functionally dependent individuals lived to a post-acute facility providing skilled care to medically complex patients often discharged directly from intensive care units. To qualify for Medicare SNF services, a beneficiary must require daily skilled nursing or rehabilitative therapy services, generally within 30 days of a hospital stay of at least 3 days in length, and must be admitted to the nursing home due to a condition related to that hospitalization. Medicare offers full coverage on the first 20 days and partial coverage for days 21-100. Based on the Minimum Data Set (MDS), a nursing home resident assessment instrument mandated by the Centers for Medicare and Medicaid Services (CMS), only 307,000 of the roughly 1.1 million unique individuals admitted to a Medicare/Medicaid certified nursing home for the first time were deemed “long-stayers” (i.e., still in the facility 90 days later).[9] This suggests that for many the nursing home has become a “way station” and not necessarily a long-term residence.
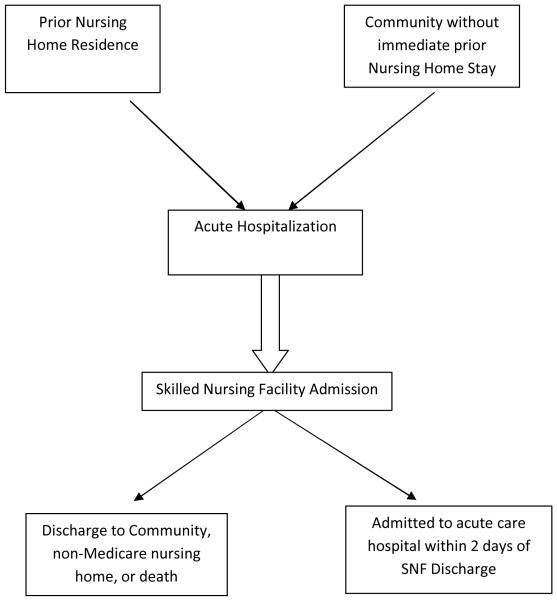
Part of the “churning” of patients within nursing homes relates to rehospitalizations. SNF rehospitalizations can be grouped into two major categories based on whether the base hospitalization occurred from the community or from a nursing home (see Exhibit 1). The first type consists of individuals admitted from the community to the hospital, then discharged to the SNF for post-acute services and then readmitted to the hospital. These new “bounce-backs” are what policy makers often have in mind when they contemplate action to curb SNF rehospitalizations. From a policy perspective, a key issue is distinguishing between the role of the hospital and the role of the SNF in determining “accountability” for these bounce-backs. For example, bounce-backs occurring in the immediate 24-48 hours following hospital discharge may relate strongly to the quality of hospital care. With a longer period from discharge (e.g., 30, 60 or 90 days), the care received in the hospital may become less important relative to the care received in the SNF towards explaining inappropriate or potentially avoidable hospitalizations. Moreover, as the length of the SNF stay increases, the resident’s payment source will usually change from Medicare to Medicaid or out-of-pocket.
Exhibit 1.
Schematic of Rehospitalization from Skilled Nursing Facilities
The second type of SNF rehospitalization originates among individuals with recent prior nursing home use. Following a base hospitalization, these individuals are discharged back to a nursing home under the SNF benefit only to be rehospitalized. Prior to their original hospitalization, these nursing home residents are often covered by Medicaid, but their base hospitalization, post-hospital SNF stay and rehospitalization are reimbursed by Medicare. Thus, hospitalizations and SNF care among nursing home residents are a cost to Medicare, but may reflect failures in care processes via “spillovers” from Medicaid payment policies.[7] Given that most Medicare-paid nursing home stays occur in a common facility alongside Medicaid-paid stays, Medicaid’s investment not only affects the likelihood of the initial hospitalization, but also the likelihood of SNF rehospitalizations due to Medicaid’s role as the dominant payer of common facility resources (e.g., staffing). Research has generally supported the idea that nursing home quality is a common good within facilities extending across payer groups.[10, 11] Thus, the care of long-stay Medicaid residents and short-stay Medicare SNF patients may be linked through the facility’s administration, staffing, culture and other shared features. On the other hand, nursing homes that invest in the clinical services necessary to reduce the likelihood of hospitalization predominantly generate savings for Medicare, while Medicaid often must pay for the increased cost of care in the nursing home. For example, research suggests that states with more generous Medicaid nursing home payment rates have fewer hospitalizations among long-stay residents.[12]
We undertook this study to explore three key questions related to SNF rehospitalizations. For individuals residing in the community and in the nursing home, what is the frequency and cost of SNF rehospitalizations within 30 days after hospital discharge? What is the variation of SNF rehospitalizations across states? Finally, what is the correlation between the rate of SNF rehospitalizations and other Medicare spending?
Methods
Medicare inpatient and SNF claims and eligibility data, as well as MDS assessments for individuals in a nursing home (with or without a SNF episode) were obtained under CMS data use agreements (No. 18900 and No. 19106). We identified all SNF episodes over the period 2000 through 2006 which were within 30 days of hospital discharge prior to the SNF admission. In order to be classified as a rehospitalization in our study, the readmission would have to occur within 30 days from the original hospital discharge. This 30-day cutoff was employed to facilitate comparability between our estimates and earlier research.[1, 3] We also determined whether beneficiaries were discharged from a SNF due to a Medicare rehospitalization within 2 days of the SNF discharge. Those individuals with a SNF episode terminated after 2 days without a hospitalization were considered not to have been rehospitalized even though they may have been rehospitalized subsequently. Thus, we ultimately counted only those SNF rehospitalizations that occurred both within 30 days of the initial hospital discharge and within 2 days of SNF discharge.
Based upon Medicare inpatient claims, we determined the total Medicare reimbursements associated with the identified rehospitalization episode including all reimbursements from all claims making up the rehospitalization. All SNF episodes were stratified based upon whether the beneficiary had an MDS assessment or SNF stay within 90 days prior to the date of SNF admission.
Rehospitalizations were assigned to the calendar year in which the SNF episode began even though the rehospitalization may have occurred in the next year. We separately calculated annual rehospitalization rates for those SNF episodes following a qualifying hospital stay that were preceded by being in a nursing home and those that were not preceded by being in a nursing home. We then calculated the rates of rehospitalization and the Medicare hospital reimbursements associated with those events during 2006 by state. We excluded Alaska, Hawaii, and other U.S. territories due to the small number of SNFs in these areas. These state-level analyses focus on 2006 because the patterns of inter-state variation across all years were very similar.
Finally, using the online Dartmouth Atlas of Health Care [13], we downloaded state level estimates published on the site regarding the number of different Medicare physician claims that were observed in the Carrier files in the last two years of life. This measure serves as a proxy for resource utilization that is unrelated to hospital care and provides an indicator of whether the geographic patterns of SNF rehospitalizations that we observe are related to broader measures of resource consumption in the population of chronically ill Medicare beneficiaries. These data were summarized over all fee-for-service decedents between 2002 and 2005. We then correlated these state level measures of multiple physician use with the overall rate of SNF rehospitalizations in 2006.
Results
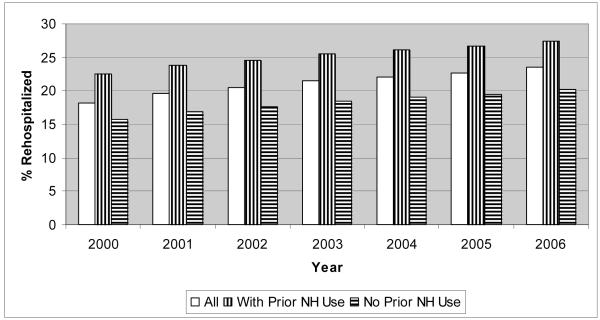
The number of SNF episodes per year ranged from 1.3 million in 2000 to 1.79 million in 2006. The overall proportion of SNF episodes ending in a hospitalization within 30 days of the original hospital discharge rose from 18.2% in 2000 to over 23.5% in 2006 (Exhibit 2). Thus, the rate of SNF rehospitalization grew 29% over the study period. In each year, the likelihood of rehospitalization was higher among those who had previously been in a nursing home than was the case for those who had not been in a nursing home prior to their qualifying hospitalization. In 2006 for example, the rehospitalization rate was 26.8% for those who had previously been in a nursing home and 19.4% for those who previously resided in the community.
Exhibit 2.
Trends in Rehospitalization Rates from Skilled Nursing Facilities: 2000-2006
Source: Authors’ calculations using Medicare inpatient and skilled nursing facility claims and eligibility data and the Minimum Data Set, Centers for Medicare and Medicaid Services.
Exhibit 3 presents state specific data on the rates of rehospitalization and the associated reimbursements. In 2006, there were 1,789,472 SNF episodes, 419,669 (23.5%) of which resulted in a rehospitalization within 30 days. Total Medicare reimbursements associated with these rehospitalizations were in excess of $4.34 billion and the average Medicare payment per rehospitalization was $10,352. As shown in the final column, the rehospitalization of individuals who had previously been in a nursing home accounted for nearly $2.23 billion (or 51.4%) of total expenditures, yet they accounted for only 806,017 (or 45.0%) of total SNF episodes. The overall rate of 30-day SNF rehospitalization varied substantially by state in 2006. Only 15.1% of 8,380 SNF episodes in Utah had a rehospitalization, whereas 28.2% of the 23,690 SNF episodes in Louisiana were rehospitalized. There are nine states with 30-day rehospitalization rates in excess of 25%, whereas there are nine states with rates under 17%.
Exhibit 3.
Frequency and Cost of Skilled Nursing Facility (SNF) Rehospitalizations by State, 2006
| State | Number of SNF Episodes |
% Rehospitalized |
Total Rehospitalization Payments (in millions) |
% of SNF Episodes with Prior NH Stay Rehospitalized |
Rehospitalization Payments with Prior NH Stay (in millions) |
|---|---|---|---|---|---|
| Alabama | 30,143 | 22.2 | $56.67 | 25.6 | $26.81 |
| Arkansas | 19,584 | 24.1 | $42.78 | 25.6 | $21.63 |
| Arizona | 16,862 | 20.3 | $36.99 | 25.1 | $14.45 |
| California | 122,477 | 23.8 | $425.11 | 29.1 | $227.05 |
| Colorado | 17,032 | 17.6 | $30.63 | 21.4 | $13.20 |
| Connecticut | 38,061 | 23.4 | $93.20 | 28.6 | $50.01 |
| District of Columbia | 2,651 | 24.1 | $9.69 | 29.3 | $4.95 |
| Delaware | 5,743 | 22.3 | $13.00 | 25.7 | $5.68 |
| Florida | 137,144 | 23.4 | $283.89 | 28.0 | $140.91 |
| Georgia | 35,777 | 23.2 | $75.91 | 25.6 | $38.92 |
| Iowa | 20,472 | 16.3 | $28.12 | 17.1 | $14.43 |
| Idaho | 6,135 | 16.4 | $9.41 | 18.9 | $3.54 |
| Illinois | 104,619 | 26.9 | $280.00 | 30.9 | $156.20 |
| Indiana | 50,810 | 22.4 | $110.68 | 25.7 | $53.81 |
| Kansas | 16,248 | 19.9 | $28.44 | 21.2 | $14.79 |
| Kentucky | 31,177 | 24.9 | $66.94 | 28.3 | $35.33 |
| Louisiana | 23,690 | 28.2 | $74.14 | 28.8 | $46 .88 |
| Massachusetts | 60,000 | 22.6 | $146.73 | 28.0 | $76.36 |
| Maryland | 43,175 | 26.4 | $170.32 | 32.1 | $87.68 |
| Maine | 10,862 | 16.9 | $16.92 | 20.4 | $6.68 |
| Michigan | 65,477 | 25.8 | $175.35 | 30.2 | $85.26 |
| Minnesota | 30,164 | 19.1 | $54.42 | 23.1 | $25.03 |
| Missouri | 43,162 | 23.9 | $90.86 | 26.6 | $49.73 |
| Mississippi | 16,769 | 28.1 | $40.49 | 31.4 | $23.76 |
| Montana | 5,295 | 15.7 | $7.12 | 17.1 | $2.89 |
| North Carolina | 51,134 | 21.2 | $95.19 | 24.9 | $43.01 |
| North Dakota | 4,082 | 16.6 | $6.05 | 16.9 | $2.55 |
| Nebraska | 12,480 | 18.6 | $22.31 | 20.2 | $10.48 |
| New Hampshire | 7,934 | 17.7 | $13.06 | 20.8 | $6.33 |
| N ew Jersey | 85,079 | 26.1 | $238.21 | 30.5 | $132.28 |
| New Mexico | 5,101 | 18.3 | $9.82 | 22.1 | $3.72 |
| Nevada | 5,896 | 22.8 | $19.21 | 26.1 | $7.55 |
| New York | 114,243 | 25.3 | $348.36 | 29.5 | $195.00 |
| Ohio | 109,838 | 24.0 | $249.44 | 28.1 | $129.28 |
| Oklahoma | 17,927 | 25.7 | $45.65 | 27.5 | $22.99 |
| Oregon | 11,294 | 17.4 | $18.84 | 22.1 | $7.63 |
| Pennsylvania | 92,729 | 22.5 | $198.08 | 25.9 | $99.08 |
| Rhode Island | 7,614 | 23.9 | $17.41 | 28.4 | $9.30 |
| South Carolina | 22,312 | 22.0 | $43.46 | 26.3 | $19.80 |
| South Dakota | 4,494 | 16.3 | $6.38 | 17.4 | $3.56 |
| Tennessee | 42,370 | 25.0 | $90.42 | 28.9 | $45.72 |
| Texas | 106,433 | 25.1 | $301.11 | 27.7 | $155.87 |
| Utah | 8,380 | 15.1 | $12.99 | 19.2 | $4.58 |
| Virginia | 44,250 | 22.6 | $83.51 | 26.7 | $38.49 |
| Vermont | 3,280 | 15.7 | $5.14 | 17.0 | $2.17 |
| Washington | 26,685 | 19.7 | $55.53 | 24.2 | $23.76 |
| Wisconsin | 37,424 | 18.8 | $65.43 | 21.3 | $30.33 |
| West Virginia | 12,741 | 24.3 | $27.25 | 27.1 | $12.13 |
| Wyoming | 2,223 | 16.1 | $3.56 | 18.9 | $1.76 |
| TOTAL | 1,789,472 | 23.5 | $4,344.23 | 26.8 | $2,233.35 |
Source: Authors’ calculations using Medicare inpatient and skilled nursing facility claims and eligibility data and the Minimum Data Set, Centers for Medicare and Medicaid Services.
Given the large inter-state differences, we sought to understand how SNF rehospitalizations varied with other aspects of health care spending on Medicare beneficiaries. Because hospital costs make up such a large proportion of total Medicare spending, particularly among chronically ill populations like those using SNF care, we contrasted state level SNF rehospitalization rates with Dartmouth Atlas data on the number of physician visits per Medicare beneficiaries in the last two years of life over the reasonably contemporaneous period of 2002 to 2005. Our analyses suggest a very strong relationship between the number of physicians’ visits and the rate of 30-day SNF rehospitalization (Pearson and Spearman correlation coefficient = 0.79).
DISCUSSION
The results of this paper suggest SNF rehospitalizations have been growing in frequency, they are quite costly, and they vary considerably across regions of the US. Over the 2000-2006 period, the rate of SNF rehospitalization grew by 29%. By 2006, over one-fifth (23.5%) of all hospital discharges to a SNF returned to the hospital directly from SNF at a total cost of $4.34 billion per year to the Medicare program. In attempting to understand the substantial variation across regions, we observe a strong correlation between SNF rehospitalizations and physician visits per Medicare beneficiaries in the last two years of life. These results suggest that the propensity to hospitalize and utilize other Medicare services is often a local-area phenomenon.
Although certain SNF rehospitalizations are unavoidable, previous research has suggested that a high proportion occur for conditions that are preventable. Specifically, MedPAC [14] has found that five conditions—congestive heart failure (CHF), respiratory infection, urinary tract infection (UTI), sepsis, and electrolyte imbalance—for which rehospitalization is potentially avoidable account for 78% of all 30-day SNF rehospitalizations. When we apply this rate to our aggregate cost figure, it suggests Medicare spent $3.39 billion (78% of $4.34 billion) in 2006 on potentially avoidable SNF rehospitalizations. Moreover, patient “churning” across SNFs and hospitals is known to introduce a number of negative health outcomes associated with medical errors as well as the stressors of the hospitalization experience known to cause delirium and functional decline.[15, 16]
From a policy perspective, the key is to provide SNFs with the resources and incentives to avoid these rehospitalizations. Towards this end, this paper helps to illustrate three important lessons for policymakers. First, because Medicare pays SNFs and hospitals on a fee-for-service basis, there is little incentive for either sector to worry about cost-shifting or inefficient resource use. As our paper suggests, the cost implications of patient churning across hospitals and SNFs are huge.
Second, not all SNF rehospitalizations relate to the same underlying policy factors. For example, we have made the distinction between rehospitalizations among individuals previously residing in the community relative to individuals with prior nursing home use. Rehospitalizations among both groups are frequent and costly, but SNF rehospitalizations among individuals who previously resided in the community will predominantly occur in hospital-based facilities or other SNFs specializing in Medicare-financed SNF care, whereas rehospitalizations among patients with prior nursing home use will often occur from facilities with high levels of Medicaid-financed care. In the latter case, policymakers may also want to consider the importance of state Medicaid policy “spillovers” to the Medicare post-acute SNF population.[7] For example, the generosity of Medicaid payment rates and the presence of bed-hold policies have been shown to influence nursing home hospitalizations.[12] Finally, given the strong correlation between SNF rehospitalizations and Medicare physician use in the last two years of life, our results suggest that rehospitalizations are likely to be substantially influenced by local area factors such as provider norms, practice patterns, bed availability, and presence and willingness to use hospice.
Policy reforms under consideration to address the high rate of SNF rehospitalizations include both system-wide and SNF-specific initiatives. In terms of broader reforms, the idea of bundling Medicare payment across providers around a hospital episode has gained considerable traction among Medicare policymakers.[3, 8] The advantage of this approach is that it encourages efficiency and care coordination within an episode to avoid unnecessary rehospitalizations and other wasteful spending.
In terms of efforts focused specifically at SNF rehospitalization, CMS began the three-state randomized Nursing Home Value-Based Purchasing (NHVBP) demonstration in July 2009. In conjunction with other quality dimensions (i.e., staffing, survey deficiencies and MDS-based quality measures), nursing homes with lower avoidable hospitalization rates will be rewarded with higher incentive-based payments. By law, the NHVBP must be budget neutral, with Medicare performance payments to nursing homes with lower hospitalization rates, for example, balanced against the savings to Medicare from reduced hospitalizations. From the 2006 state-specific data presented in Exhibit 3, the high rate of 30-day SNF rehospitalization in the three participating states—Arizona (20.3%), New York (25.3%), and Wisconsin (18.8%)—suggests the real potential for the NHVBP to generate offsetting savings for the purposes of rewarding nursing homes.
Although payment reforms such as bundling and P4P have promise, skeptics have raised a range of potential issues including the increased incentives for selection of the most profitable patients, withholding of patient care, upcoding and fraud, along with the technical difficulties of case-mix adjustment and quality measurement and monitoring. In returning to our lessons highlighted above, the results presented in this paper also underscore two other considerations: 1) a Medicare-only solution will not address the potential for spillovers from other payer groups (e.g., long-stay Medicaid nursing home residents); and 2) local behavioral norms may be less responsive to payment incentives or, at least, may not be uniform.
Towards the first issue, the Medicare-only focus of payment reforms such as bundling may distort behavior in facilities caring for a sizeable proportion of long-stay Medicaid residents. As noted, we observed higher Medicare SNF rehospitalization rates among individuals with immediate prior nursing homes stays. In many of these nursing homes, the rehospitalization of Medicare SNF patients may relate closely to the generosity and method of Medicaid payment and the share of Medicaid residents within the nursing home. State Medicaid programs have little incentive to adopt policies that lower Medicare hospital and SNF spending. Bundling could be expanded to include Medicaid, but the coordination costs and the political capital needed to do so would be very high. In many regards, some type of Medicare-Medicaid capitated model might be the best approach towards aligning broader incentives across multiple payers and providers. However, very few providers and patients have been willing to “lock-in” to capitated models with the frail elderly and disabled due to the perceived risk. As such, their potential success on a broader scale may be limited.
Towards the second issue, variation across areas in SNF rehospitalizations suggests that payment reform might be one of several potential measures towards curbing inefficient service use. Interestingly, even after adjusting for case-mix and demographics, the variation across areas is not simply a function of the rate of potentially avoidable hospitalizations.[12] That is, some of the variation in rehospitalizations across areas is also present across conditions which are not considered to be avoidable. This result speaks to the strong area norms such as practice styles and the supply of providers that extend beyond payment and other financial considerations. Although strong Medicare financial incentives may lessen the variation across areas, it may make sense to couple payment incentives with other system-wide interventions such as spending benchmarks, shared provider-patient decision making and the promotion of centers of medical excellence.[17]
In summary, there is need for demonstrations of these policy models, because each has considerable technical and practical implementation challenges that could undermine their effectiveness. In designing these demonstrations, we encourage policymakers to consider the heterogeneity of Medicare rehospitalizations and the significant role of local provider norms. Although several Medicare reforms currently under discussion move beyond particular providers to consider the “system,” our findings suggest that a true system-level reform must extend beyond Medicare and must consider more than simply financial incentives.
Acknowledgments
This work was supported with funding from the Robert Wood Johnson Foundation’s Changes in Health Care Financing Organization (HCFO) initiative (Grant no. 64435) and a National Institute on Aging (NIA) program project (Grant no. p01 AG27296). David Grabowski was supported in part by an NIA career development award (Grant no. K01 AG24403). The authors are grateful to Jeffrey Hiris for programming assistance in constructing the analysis file.
Contributor Information
Vincent Mor, Brown University.
Orna Intrator, Brown University.
Zhanlian Feng, Brown University.
David C. Grabowski, Harvard Medical School.
NOTES
- [1].Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009 Apr 2;360(14):1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- [2].Agency for Healthcare Research and Quality HCUPnet. 2009 doi: 10.1080/15360280802537332. [cited 2009 July 21]; Available from: hcupnet.ahrq.gov. [DOI] [PubMed]
- [3].Medicare Payment Advisory Commission . Report to the Congress: Medicare Payment Policy. Medicare Payment Advisory Commission; Washington, DC: Jun, 2008. [Google Scholar]
- [4].Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, et al. Comprehensive discharge planning and home follow-up of hospitalized elders: a randomized clinical trial. Jama. 1999 Feb 17;281(7):613–20. doi: 10.1001/jama.281.7.613. [DOI] [PubMed] [Google Scholar]
- [5].Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006 Sep 25;166(17):1822–8. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- [6].Coleman EA, Mahoney E, Parry C. Assessing the quality of preparation for posthospital care from the patient’s perspective: the care transitions measure. Medical care. 2005 Mar;43(3):246–55. doi: 10.1097/00005650-200503000-00007. [DOI] [PubMed] [Google Scholar]
- [7].Grabowski DC. Medicare and Medicaid: conflicting incentives for long-term care. Milbank Q. 2007;85(4):579–610. doi: 10.1111/j.1468-0009.2007.00502.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Senate Finance Committee . Transforming the Health Care Delivery System: Proposals to Improve Patient Care and Reduce Health Care Costs. Washington, DC: Apr 29, 2009. [Google Scholar]
- [9].Mor V, Zinn J, Gozalo P, Feng Z, Intrator O, Grabowski DC. Prospects for transferring nursing home residents to the community. Health Affairs (Millwood) 2007 Nov-Dec;26(6):1762–71. doi: 10.1377/hlthaff.26.6.1762. [DOI] [PubMed] [Google Scholar]
- [10].Grabowski DC, Gruber J, Angelelli JJ. Nursing Home Quality as a Common Good. Rev Econ Stat. 2008;90(4):754–64. doi: 10.1162/rest.90.4.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Konetzka RT, Norton EC, Sloane PD, Kilpatrick KE, Stearns SC. Medicare prospective payment and quality of care for long-stay nursing facility residents. Med Care. 2006 Mar;44(3):270–6. doi: 10.1097/01.mlr.0000199693.82572.19. [DOI] [PubMed] [Google Scholar]
- [12].Intrator O, Grabowski DC, Zinn J, Schleinitz M, Feng Z, Miller S, et al. Hospitalization of nursing home residents: the effects of states’ Medicaid payment and bed-hold policies. Health Serv Res. 2007 Aug;42(4):1651–71. doi: 10.1111/j.1475-6773.2006.00670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Dartmouth Atlas of Health Care Data Tables. 2009 [cited 2009 June 19]; Available from: http://cecsweb.dartmouth.edu/atlas08/datatools/datatb_s1.php.
- [14].Donelan-McCall N, Eilersen T, Fish R, Kramer A. Small Patient Population and Low Frequency Event Effects on the Stability of SNF Quality Measures. Medicare Payment Advisory Commission; Washington, DC: 2006. [Google Scholar]
- [15].Coleman EA, Min SJ, Chomiak A, Kramer AM. Posthospital care transitions: patterns, complications, and risk identification. Health services research. 2004 Oct;39(5):1449–65. doi: 10.1111/j.1475-6773.2004.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Teno JM, Mitchell SL, Skinner J, Kuo S, Fisher E, Intrator O, et al. Churning: the association between health care transitions and feeding tube insertion for nursing home residents with advanced cognitive impairment. J Palliat Med. 2009 Apr;12(4):359–62. doi: 10.1089/jpm.2008.0168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Wennberg JE, Fisher ES, Skinner JS. Geography and the debate over Medicare reform. Health affairs (Project Hope) 2002 Jul-Dec;:W96–114. doi: 10.1377/hlthaff.w2.96. Suppl Web Exclusives. [DOI] [PubMed] [Google Scholar]