Abstract
BACKGROUND:
In October 2006, federal funding was announced for the development of a national strategy to fight cardiovascular disease (CVD) in Canada. The comprehensive, independent, stakeholder-driven Canadian Heart Health Strategy and Action Plan (CHHS-AP) was delivered to the Minister of Health on February 24, 2009.
OBJECTIVES:
The mandate of CHHS-AP Theme Working Group (TWG) 6 was to identify the optimal chronic disease management model that incorporated timely access to rehabilitation services and end-of-life planning and care. The purpose of the present paper was to provide an overview of worldwide approaches to CVD and cardiac rehabilitation (CR) strategies and recommendations for CR care in Canada, within the context of the well-known Chronic Care Model (CCM). A separate paper will address end-of-life issues in CVD.
METHODS:
TWG 6 was composed of content representatives, primary care representatives and patients. Input in the area of Aboriginal and indigenous cardiovascular health was obtained through individual expert consultation. Information germane to the present paper was gathered from international literature and best practice guidelines. The CCM principles were discussed and agreed on by all. Prioritization of recommendations and overall messaging was discussed and decided on within the entire TWG. The full TWG report was presented to the CHHS-AP Steering Committee and was used to inform the recommendations of the CHHS-AP.
RESULTS:
Specific actionable recommendations for CR are made in accordance with the key principles of the CCM.
CONCLUSIONS:
The present CR blueprint, as part of the CHHS-AP, will be a first step toward reducing the health care burden of CVD in Canada.
Keywords: Canadian Heart Health Strategy and Action Plan, Cardiac rehabilitation, Chronic care model
Abstract
HISTORIQUE :
En octobre 2006, le gouvernement fédéral a annoncé un financement pour élaborer une stratégie nationale afin de lutter contre les maladies cardiovasculaires (MCV) au Canada. La Stratégie canadienne de santé cardiovasculaire et plan d’action (SCSC-PA) complète, indépendante et élaborée par les parties prenantes, a été dévoilée au ministre de la Santé le 24 février 2009.
OBJECTIFS :
Les six groupes de travail thématiques (GTT) de la SCSC-PA avaient comme mandat de déterminer le modèle optimal de prise en charge des maladies chroniques qui intégrerait un accès rapide à des services de réadaptation ainsi q’à la planification et aux soins de fin de vie. Le présent article visait à fournir un aperçu des démarches mondiales à l’égard des MCV ainsi que des stratégies de réadaptation cardiaque (RC) et des recommandations en matière de soins en RC au Canada, dans le contexte du modèle de soins chroniques (MSC) bien connu. Un article distinct portera sur les enjeux de fin de vie en MCV.
MÉTHODOLOGIE :
Le GTT se composait de représentants du contenu, de représentants des soins primaires et de patients. On a obtenu l’apport du secteur de la santé cardiovasculaire des autochtones et des indigènes grâce à des consultations individuelles auprès d’experts. L’information propre au présent article provenait de publications internationales et de lignes directrices de pratiques exemplaires. Tous ont discuté des principes du MSC et les ont acceptés. Le GTT a discuté de la priorisation des recommandations et du message global et l’a établi ensemble. Le rapport complet du GTT a été présenté au comité directeur de la SCSC-PA, qui l’a utilisé pour étayer ses recommandations.
RÉSULTATS :
Des recommandations précises en RC, donnant matière à des mesures, sont proposées conformément aux grands principes du MSC.
CONCLUSIONS :
Le présent plan directeur en RC, intégré à la SCSC-PA, constitue une première étape vers la réduction du fardeau des soins de santé en MCV au Canada.
On October 23, 2006, the Honourable Tony Clement, then federal Minister of Health, announced funding for the development of a new heart health strategy to fight cardiovascular disease (CVD) in Canada. A 29-member expert Steering Committee was established to develop the comprehensive, independent, stakeholder-driven Canadian Heart Health Strategy and Action Plan (CHHS-AP), which was delivered to the Minister of Health on February 24, 2009 (www.chhs-scsc.ca).
Among the working groups of the CHHS-AP was Theme Working Group 6, whose mandate was to identify the optimal chronic disease management (CDM) model to incorporate timely access to rehabilitation services, and end-of-life planning and care.
The present paper places recommendations related to cardiac rehabilitation (CR) services in the context of a CDM philosophy and framework. The full Theme Working Group report was presented to the CHHS-AP Steering Committee and was used to inform the overall recommendations of the CHHS-AP. A separate publication will address end-of-life planning and care. The purpose of the present paper is to provide an overview of worldwide approaches to CVD and CR strategies as a basis for recommendations of CR care in Canada, within the context of the well-known Chronic Care Model (CCM) (1).
CDM
CDM refers to a system of health care that supports individuals with chronic illness to adopt behaviours to remain as healthy and independent as possible. For many years, the health care system has been more of an ‘illness care’ system, wherein there is reaction to illness rather than a proactive approach to maintaining or improving health status. CDM models change this paradigm by placing the patient at the centre, supported by health care providers, the health care system, and the community at large to facilitate optimum health and long-term well-being. Implicit in CDM is the concept that patients should be well-informed about their illness(es), and should be active participants and decision makers in their own care. The focus of CDM on moving care and prevention ‘upstream’ in the health care continuum has been shown to be cost-effective, and to improve the health status of individuals and populations (2–4).
THE CCM
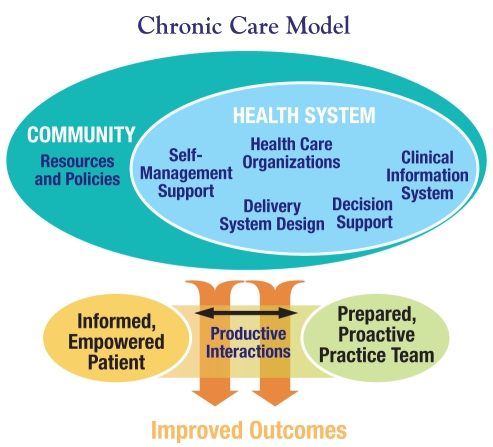
There are a number of CDM models that embody a core set of principles. The model that has received the most widespread acceptance and has been widely adopted is the CCM (1) (Figure 1). Since its introduction, this model has evolved and a number of modified versions exist. However, the core elements remain:
The health system – The organization, senior leadership and culture of the health care system must promote safe, high-quality coordinated chronic disease care.
Delivery system design – The delivery of effective and efficient clinical care is ensured through the implementation of well-defined roles of team members, proactive interventions and systematic follow-up, as the mainstay of care. This aspect, when implemented using both physician and nonphysician interdisciplinary team members, has been particularly associated with improved health care outcomes.
Decision support – Clinical care is delivered according to best evidence and patient preferences. Evidence-based guidelines are embedded in clinical practice at the point of patient contact. Members of the health care team have access to, and are educated in, the most up-to-date clinical care information. Specialist services are organized to support primary care and are available for presentations that are more complicated.
Clinical information systems – Individual and aggregate patient data are available and organized to facilitate efficient CDM and aid in system-wide decision making. Information is efficiently transferred between providers and is shared with the patient. Alerts and reminders, as well as outcome measures, are used to facilitate optimum care.
Self-management support – The organization and community empower patients to manage their health and health care. To do so, patients are provided with access to the necessary information as well as to support in goal-setting, action-planning, problem-solving and other techniques that allow them to play a major role in the maintenance of their health.
The community – The larger community supports the care of patients. Community organizations, resources and policies are organized to contribute to the self-management and care of patients with chronic disease.
Figure 1).
The Chronic Care Model. Reprinted with permission from reference 26
CR
CR is an important specialized component of chronic vascular disease care that also uses a multifaceted approach. This approach includes comprehensive targeted cardiovascular risk factor therapies, behaviour modification strategies to sustain healthy lifestyles and promote pharmacological adherence, and therapeutic exercise and physical activity programs. The breadth and depth of services required to achieve these goals successfully are usually beyond the current resources of family physician teams or practitioners and most cardiovascular specialists (5). However, when situated in the CCM, CR is viewed as a partnered responsibility that includes the family physician, specialist, CR team, the patient and family.
CR decreases total and cardiac mortality (6) by 20% to 25%, and may also reduce rehospitalizations for cardiac disease and the need for subsequent revascularization procedures (7–9) in patients with coronary artery disease. CR is cost-effective and may in fact reduce the cost to the health care system for high-risk patients (10). There is emerging evidence that the beneficial effects of CR (compared with usual care) remain significant regardless of whether the key elements of CR care are delivered as traditional hospital-based programs, delivered as home-based programs or integrated within community family health centres (11–14).
OVERVIEW OF RECENT CR STRATEGIES
There have been a number of Canadian and international CR strategies. The successful elements of each are reviewed below to provide support for the concluding recommendations.
Canada
The Cardiac Rehabilitation Pilot Project (CRPP) (15) was funded by the Ontario provincial government from 2001 to 2002 to evaluate the effectiveness of a regional model of CR service delivery (16). Twenty-four existing and new CR sites participated, representing 45% of the province’s identifiable CR programs. Participating sites implemented a consensus-based, coordinated model of service delivery, expanded existing programs or established new programs, and provided CR services (six-month duration) for their communities. By the end of the project, 60% more patients received CR services than the previous year. Overall, the cardiac risk profiles of patients improved substantially by the time they exited the CR program. The CRPP successfully demonstrated that a standardized model of CR services, consistent with international guidelines, could be rapidly implemented across different regions and practice settings at a cost of approximately $1,500 per patient (15).
The key findings of the Ontario CRRP:
Planning and delivery of CR services must be integrated with that of overall cardiac care services.
Regional CR networks should be developed to support regional referral processes, communication and sharing of regional resources, and integration and standardization of patient care.
Access should be promoted through automatic inpatient referral processes and the development of a priority rating system for referral to CR services.
Wait times for access to CR should, in general, not exceed 30 days (preferred) or 60 days (acceptable) from the referring event, and should be shorter for high-risk patients.
The location of CR programs should take into account local demand.
A centralized patient data registry should be developed, using a comprehensive set of standardized CR patient and service outcome measures.
Ongoing research of CR services should be conducted to explore optimal CR delivery cost-effectiveness.
United Kingdom
The United Kingdom National Service Framework (17) established 12 standards for the management of coronary artery disease that include CR and emphasize secondary prevention more strongly than the other national strategies. The United Kingdom government is committed to reducing the death rate from coronary artery disease, stroke and related diseases in people younger than 75 years of age by at least 40% by 2010.
The key elements of this strategy:
Emphasis on reducing health inequities caused by socioeconomic status, necessity and geographic variations.
CR services should be integrated closely with other services provided in primary and secondary care.
Development of a range of CR services and service models in each locality to support individualized patient care.
Development of CR system surveillance and performance indicators.
Performance management to set CR targets.
National milestones against which every CR service and region is assessed to set realistic and achievable targets.
Finland
The Finnish Heart Plan (18) was conceived based on the North Karelia project (19), which is one of the best-known and successful (greater than 50% reduction in mortality and morbidity) population-level chronic disease prevention programs in the world. The strategy was community-based, with adherence to well-established principles of general program planning, implementation and evaluation.
The key elements of this strategy:
Improve continuity of care by developing cooperation between special and primary health care clinics.
Develop CR for primary care.
Combination of well-planned media messages with a broad range of community activities involving primary health care, voluntary organizations, the food industry, worksites, schools and local media.
Focus on psychosocial recovery of patients.
Collaboration and support from both formal decision makers and informal opinion leaders.
Address the differences in health care use, independent of the severity of the disease, between highly and undereducated patients, and higher and lower socioeconomic status patients.
Change social and physical environments in the community to be more conducive to health and healthy lifestyles.
Australia
The goal of the Australia National Chronic Disease Strategy (20) is to achieve significant and sustainable change using a population health approach with health promotion and prevention across the continuum.
The Australian CR strategy includes:
Broad eligibility to include cardiovascular patients following an acute heart, stroke or peripheral vascular event.
Reduction of disparity by addressing CR needs of disadvantaged groups, including Aboriginal peoples.
Better recognition and treatment of mental health conditions and the importance of psychosocial health in the context of CR programs.
SUMMARY OF CURRENT STRATEGIES
While CR strategies have been developed in several countries, and there is general agreement among them regarding both the content and the process of CR delivery, there is very little evidence about progress related to implementation of these strategies or outcomes that are a direct result of the strategic plan. There is a clear need for focus on the implementation and evaluation of any CR or heart health strategy if real and measurable change is to occur. In addition, CR strategies for at-risk patients without overt vascular disease were not generally addressed.
IMPLEMENTATION CHALLENGES
Underuse of CR
Despite the overwhelming evidence in favour of CR, it is underused, with only 20% utilization reported in North American jurisdictions, and approximately 30% in European and Australasian jurisdictions (15,21,22). The cause and variance between jurisdictions of CR underuse relate to patient and health system factors (23). Factors that have been associated with increased CR referral and attendance are discharge diagnosis of acute myocardial infarction or coronary artery bypass surgery, age less than 65 years, previous participation in CR (24) and male sex (25). Thus, a systematic approach to universal referral to CR has the potential to improve CR uptake, as demonstrated in the Ontario CRPP, in which a systematic CR referral process increased CR participation among eligible patients from approximately 15% to 25% in just six months (15).
The following additional gaps related to CR were identified:
Access is limited for a number of potentially marginalized groups such as women, seniors (particularly those with mobility limitations), residents of rural settings, aboriginal and indigenous peoples, and ethnocultural groups who are recent immigrants and do not speak English.
Congenital heart disease patients do not receive systematic care delivery.
Heart failure patients are eligible for CR programs but are not referred readily.
RECOMMENDATIONS TO THE CHHS-AP
The following principles were endorsed as potential important solutions to the gaps in delivery of optimal CR in Canada:
CR is a comprehensive program designed to facilitate all of the various healthy behaviours undertaken to promote cardiovascular health (eg, optimizing exercise, nutritional habits and adherence to evidence-based pharmaceuticals).
Chronic care management in CR is a continuum and patients should receive care based on their risk of a future cardiovascular event.
A paradigm shift is necessary such that acute interventions are viewed as adjuncts to chronic cardiovascular care, available as needed. A successful paradigm shift will require a concerted widespread education effort of patients, media, the public at large, health care professionals, health care administrators and policy makers.
Adequate resource reallocation is essential. CR and chronic care management need to receive sufficient funding support because chronic care management is the platform on which appropriate cardiac care is built.
When situated in the context of the CCM, the recommendations for CR are as follows:
Health system
CR must be recognized as an integral part of overall cardiovascular care. Patients should be identified and engaged as early as possible during their disease. The CCM dictates that CR care should be accessed in a timely manner. To address access to or disparity in the delivery of health care as a result of age, sex, income, and rural and urban locations, it is suggested that if strategies were designed around the individuals who have the most challenges in receiving care, they should work for everyone else as well.
Provinces and territories should resource CR services appropriately. CR should be a funded insured service and funding should be linked to performance.
Delivery system design
Care should be delivered in the context in which patients generally reside (ie, within their family or group). The primary care team-patient interaction should be maintained or enhanced, thus enabling this team to take the lead for a cardiovascular CCM at the patient level.
CDM in CR should be delivered by adhering to the notion of ‘shared care’ between the primary care team and the regional or local CR program, to a greater or lesser degree, depending on the patient’s risk for future events. Communication between the CR team and the primary care team is very important. CR delivery must be truly patient-centred and primary care-based for the majority of patients.
Case management is important; however, its focus should be on the higher-risk, more complex patients. Caution should be exercised so that another layer of health professionals (case managers) is not added to an already complex system. A resource person or patient navigator on the primary care team may facilitate access to services for patients.
The delivery system must be flexible with respect to service delivery and service location, to allow care as close to home as possible. Use of novel telecommunications technology to deliver care would also allow the creation of cost-effective programs for rural programs.
Decision support
Clinical care should be delivered according to best evidence and patient preferences. Evidence-based guidelines are embedded in clinical practice at the point of patient contact. Members of the health care team have access to, and are educated in, the most up-to-date clinical care information. Specialist services are organized to support primary care.
Potential roles for the regional CR centres would be to provide regional training for health care professionals, links to related chronic care programs, oversight of health system and health outcome surveillance, access to care coordination, and actual care delivery to more complex CR cases.
Clinical information systems
System support would likely comprise many different elements such as point-of-care electronic decision support (requires electronic health record), care algorithms and regional resource CR centres. A surveillance system should be established to monitor system- and patient-level outcomes including resource use.
Self-management support
Information needs to be patient and family centred. Tools need to be developed to support and assist with personal responsibility. Patients want to be engaged and active participants in their health care, but they, and their informal caregivers, require tools and resources for self-management.
The community
Buy-in from the public is essential; a social marketing plan emphasizing that the current system is not sustainable is needed. Engagement with public media could assist with promoting this shift to the population at large. Evidence-based marketing should be added to public relations. Public and private environments should be developed to promote healthy behaviours such as walking or cycling to work.
Industry engagement is very important. Workplace promotion of cardiovascular health and workplace involvement in rehabilitation following an acute event are potential solutions to some of the access issues. Third-party insurers should be actively involved in facilitating a cardiac patient’s return to work.
SUMMARY
CVD is a chronic and common condition with a huge health care burden. Our current understanding supports a change in model of care for patients with CVD; a multidisciplinary CCM, which includes CR, is the appropriate next step in CVD care delivery. At present, appropriate use of CR for Canadians is suboptimal and should be enhanced by using health system design, decision support, clinical information systems, patient self-management support, community support and innovative funding to make this goal a reality. In addition, strategies are still needed to deal with the patient who is at high risk for CVD but has not yet developed the overt condition. It is our hope that this blueprint will be a first step toward helping reduce the health care burden of CVD in Canada.
REFERENCES
- 1.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: Translating evidence into action. Health Aff (Millwood) 2001;20:64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 2.Goetzel RZ, Ozminkowski RJ, Villagra VG, Duffy J. Return on investment in disease management: A review. Health Care Finance Rev. 2005;26:1–19. [PMC free article] [PubMed] [Google Scholar]
- 3.Battersby MW. Health reform through coordinated care: SA HealthPlus. BMJ. 2005;330:662–5. doi: 10.1136/bmj.330.7492.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Piatt GA, Orchard TJ, Emerson S, et al. Translating the chronic care model into the community: Results from a randomized controlled trial of multifaceted diabetes care intervention. Diabetes Care. 2006;29:811–7. doi: 10.2337/diacare.29.04.06.dc05-1785. [DOI] [PubMed] [Google Scholar]
- 5.Stone JA, Arthur HM. Canadian Guidelines for Cardiac Rehabilitation and Cardiovascular Disease Prevention, second edition, 2004: Executive summary. Can J Cardiol. 2005;21(Suppl D):3D–19D. [PubMed] [Google Scholar]
- 6.Taylor RS, Brown A, Ebrahim S, et al. Exercise-based rehabilitation for patients with coronary heart disease: Systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116:682–92. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- 7.Sdringola S, Nakagawa K, Nakagawa Y, et al. Combined intense lifestyle and pharmacologic lipid treatment further reduce coronary events and myocardial perfusion abnormalities compared with usual-care cholesterol-lowering drugs in coronary artery disease. J Am Coll Cardiol. 2003;41:263–72. doi: 10.1016/s0735-1097(02)02693-1. [DOI] [PubMed] [Google Scholar]
- 8.Belardinelli R, Paolini I, Cianci G, Piva R, Georgiou D, Purcaro A. Exercise training intervention after coronary angioplasty: The ETICA Trial. J Am Coll Cardiol. 2001;37:1891–900. doi: 10.1016/s0735-1097(01)01236-0. [DOI] [PubMed] [Google Scholar]
- 9.Hambrecht R, Walther C, Mobius-Winkler S, et al. Percutaneous coronary angioplasty compared with exercise training patients with stable coronary artery disease: A randomized trial. Circulation. 2004;109:1371–8. doi: 10.1161/01.CIR.0000121360.31954.1F. [DOI] [PubMed] [Google Scholar]
- 10.Brown A, Taylor R, Noorani H, Stone J, Skidmore B. Exercise-Based Cardiac Rehabilitation Programs for Coronary Artery Disease: A Systematic Clinical and Economic Review. Ottawa: Canadian Coordinating Office for Health Technology Assessment; 2003. [Google Scholar]
- 11.Clark AM, Hartling L, Vandermeer B, Lissel SL, McAlister FA. Secondary prevention programmes for coronary heart disease: A meta-regression showing the merits of shorter, generalist, primary care-based interventions. Eur J Cardiovasc Prev Rehabil. 2007;14:538–46. doi: 10.1097/HJR.0b013e328013f11a. [DOI] [PubMed] [Google Scholar]
- 12.Giannuzzi P, Saner H, Bjornstad H, et al. Secondary prevention through cardiac rehabilitation: Position paper of the working group on cardiac rehabilitation and exercise physiology of the European Society of Cardiology. Eur Health J. 2003;24:1273–8. doi: 10.1016/s0195-668x(03)00198-2. [DOI] [PubMed] [Google Scholar]
- 13.Leon AS, Franklin BA, Costa F, et al. Cardiac rehabilitation and secondary prevention of coronary heart disease: An American Heart Association Scientific Statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity) in Collaboration with the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2005;111:369–76. doi: 10.1161/01.CIR.0000151788.08740.5C. [DOI] [PubMed] [Google Scholar]
- 14.Arthur HM, Smith KM, Kodis J, McKelvie R. A controlled trial of hospital versus home-based exercise in cardiac patients. Med Sci Sports Exerc. 2002;34:1544–50. doi: 10.1097/00005768-200210000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Suskin N, Arthur HM, Swabey T, Ross J. The Ontario Cardiac Rehabilitation Pilot Project – Report and Recommendations. North York: Cardiac Care Network of Ontario; 2002. [Google Scholar]
- 16.Suskin N, MacDonald S, Swabey T, Arthur H, Vimr MA, Tihaliani R. Cardiac rehabilitation and secondary prevention services in Ontario: Recommendations from a consensus panel. Can J Cardiol. 2003;19:833–8. [PubMed] [Google Scholar]
- 17.UK Department of Health National Service Framework – Coronary Heart Disease. 2000.
- 18.Finnish Heart Association and Ministry of Social Affairs and Health . Action Plan for Promoting Finnish Heart Health for the Years 2005–2011. Helsinki: Finnish Heart Association; 2005. Finnish Heart Plan. [Google Scholar]
- 19.Puska P. Successful prevention of non-communicable diseases: A 25 year experience with North Karelia Project in Finland. Public Health Medicine. 2002;4:5–7. [Google Scholar]
- 20.National Chronic Disease Strategy, 2005. Canberra: Australian Government Department of Health and Ageing; 2005. [Google Scholar]
- 21.Doolan-Noble F, Broad J, Riddell T, North D. Cardiac rehabilitation services in New Zealand: Access and utilization. N Z Med J. 2004;117:U955. [PubMed] [Google Scholar]
- 22.Kotsev K, Wood DA, De Bacquer D, Heidrich J, De Backer G, on behalf of the EUROASPIRE II Study Group Cardiac rehabilitation for coronary patients: Lifestyle, risk factor and therapeutic management. Results from the EUROASPIRE II survey. Eur Heart J. 2004;(Suppl 6):j17–j26. [Google Scholar]
- 23.Dafoe W, Arthur H, Stokes H, Morrin L, Beaton L. Universal access: But when? Treating the right patient at the right time: Access to cardiac rehabilitation. Can J Cardiol. 2006;22:905–11. doi: 10.1016/s0828-282x(06)70309-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson N, Fisher J, Nagle A, Inder K, Wiggers J. Factors associated with referral to outpatient cardiac rehabilitation services. J Cardiopulm Rehabil. 2004;24:165–70. doi: 10.1097/00008483-200405000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Norris CM, Jensen LA, Galbraith PD, et al. Referral rate and outcomes of cardiac rehabilitation after cardiac catheterization in a large Canadian city. J Cardiopulm Rehabil. 2004;24:392–400. doi: 10.1097/00008483-200411000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1:2–4. [PubMed] [Google Scholar]