Abstract
Objective
To evaluate the performance of a near patient test for Helicobacter pylori infection in primary care.
Design
Validation study performed within a randomised trial of four management strategies for dyspepsia.
Setting
43 general practices around Nottingham.
Subjects
394 patients aged 18-70 years presenting with recent onset dyspepsia.
Main outcome measures
Results of the FlexSure test compared with an enzyme linked immunosorbent assay (ELISA; HM-CAP) with an identical antigen profile and with results of an earlier validation study in secondary care. Diagnostic yield of patients undergoing endoscopy on the basis of their FlexSure result compared with those of patients referred directly for endoscopy.
Results
When used in primary care FlexSure test had a sensitivity and specificity of 67% (95% confidence interval 59% to 75%) and 98% (95% to 99%) compared with a sensitivity and specificity of 92% (87% to 97%) and 90% (83% to 97%) when used previously in secondary care. Of the H pylori test and refer group 14% (28/199) were found to have conditions for which H pylori eradication was appropriate compared with 23% (39/170) of the group referred directly for endoscopy.
Conclusions
When used in primary care the sensitivity of the FlexSure test was significantly poorer than in secondary care. About a third of patients who would have benefited from H pylori eradication were not detected. Near patient tests need to be validated in primary care before they are incorporated into management policies for dyspepsia.
Key messages
Near patient tests for H pylori infection have been recommended in the management of dyspepsia in primary care without proper evaluation
Such tests should have a high sensitivity to avoid missing treatable illness related to infection
The FlexSure near patient test had a lower sensitivity than previously reported in validation studies performed in secondary care
Fewer than expected numbers of patients with H pylori related pathology were identified with the FlexSure in primary care
Introduction
Prescription of “ulcer healing drugs” for dyspepsia accounts for 10% of prescribing costs in general practice, over £500 million in England and Wales in 1996.1Eradication of Helicobacter pylori in patients with peptic ulcers offers the prospect of reducing the enormous costs of these drugs, and some guidelines for dyspepsia management recommend testing patients in primary care for H pylori.2,3
Of the tests for H pylori that might be used in primary care, near patient tests have obvious attractions in being independent of a laboratory and giving a result quickly enough to guide initial management. Initial reports conflict as to the sensitivity and specificity of such tests,4–8 and there has been little assessment of their accuracy and performance in primary care.9,10 As part of a trial of the management of dyspepsia in primary care we have used a near patient test in two of the four management strategies being compared. This paper reports our experience with one near patient test and compares the diagnostic yield resulting with that from early endoscopy.
Methods
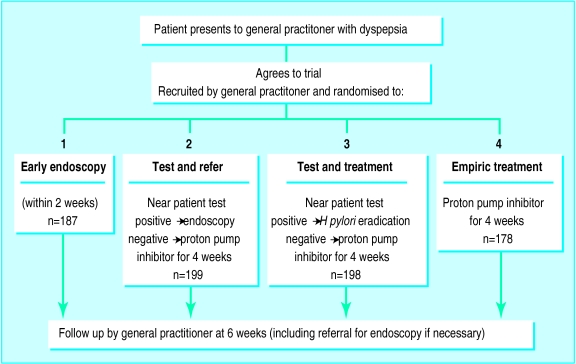
Between May 1995 and June 1998, 43 general practices in Nottinghamshire took part in a randomised trial of four strategies for the management of dyspepsia (fig 1). Two strategies involved testing for H pylori with the FlexSure test (SmithKline Diagnostics, San Jose, California). In one, patients withpositive results on the FlexSure test were referred for endoscopy and in the other, patients withpositive results received eradication treatment without further investigation. In the remaining two strategies, patients were not tested for H pylori but were randomised to early endoscopy or received empiric treatment with a proton pump inhibitor.
Figure 1.
Recruitment and randomisation process (of 187 patients randomised to early endoscopy, 17 failed to attend)
Patients randomised were between 18 and 70 years old. Dyspepsia was defined as symptoms thought to be arising from the upper gastrointestinal tract and of sufficient severity to justify empiric treatment with an H2 antagonist or proton pump inhibitor. Patients were not eligible for inclusion if they had symptoms suggestive of malignancy, a history of peptic ulcer or reflux oesophagitis diagnosed by endoscopy or barium meal, or previous investigation for dyspepsia within the past five years. Onset of symptoms with treatment with non-steroidal anti-inflammatory drugs or with either eradication treatment for H pylori or more than three prescriptions for acid suppression treatment in the past six months were also criteria for exclusion. After randomisation a 7 ml blood sample was taken. For the two strategies requiring H pylori testing the doctor or practice nurse tested serum from the clotted sample. In practices without centrifuges, operators allowed the sample to stand for at least three hours before completing testing according to the manufacturer's instructions. Our previous hospital study showed that this method enabled sufficient serum to form and had a sensitivity of 92% (95% confidence interval 87% to 97%) and specificity of 90% (83% to 97%).11
After recruitment the completed near patient test card and blood sample were sent to University Hospital. The serum remaining was stored at −400 C and later tested with an immunoassay based H pylori test with identical antigen profile ((enzyme linked immunosorbent assay (ELISA); HM-CAP, Enteric Products, Westbury, NY, US). Testing was performed by a single operator blinded to the FlexSure results.
All general practitioners and practice nurses from the highest recruiting practices were sent a questionnaire with a five point Likert scale, asking about the test's ease of performance and interpretation of results.
Results were analysed with spss (spss, Chicago, IL, US). Differences in the prevalence of disease between groups was assessed with a χ2test. Antibody titres of patients with true positive and false negative FlexSure test results were compared by using Mann-Whitney U test and the Wilcoxon rank sum test for non-parametric data. Linear regression and log linear regression were used to assess the relation between tests performed and the proportion of false negative results for each operator. The trial was approved by the University Hospital ethics committee and the local medical committee for Nottinghamshire.
Results
Patients and FlexSure test results
Between May 1995 and June 1998, 762 patients were recruited to the trial. The mean (range) age of patients was 42 (18-73) years. In 27% (204/762) of patients dyspepsia was of recent onset while in 28% (208) symptoms had first occurred five or more years earlier. In 422 (56%) symptoms of dyspepsia were reported to be of sufficient severity to interfere with the patient's normal daily activities. FlexSure testing was performed on 394 patients in 39 general practices. Three patients refused testing. In the four remaining practices no patients were randomised to the two strategies involving H pylori testing. On the basis of the near patient test 98 (25%) patients were positive for H pylori, 291 (73%) were negative for H pylori, and for five patients (1%) the results were invalid (the control line failed to appear).
Validation against ELISA
Five patients did not have serum available for ELISA testing. Of the 389 remaining, 139 (36%) patients had positive results for H pylori by the ELISA test, 241 (62%) had negative results, and nine (2%) had indeterminate ELISA results, lying between the positive and negative cut off. The FlexSure results relative to the ELISA results are shown in table 1. FlexSure had a sensitivity of 67% (59% to 75%) and a specificity of 98% (95% to 99%) against ELISA. Eight of the nine indeterminate results on ELISA were negative on FlexSure testing. The correlation between ELISA titre and FlexSure result is shown in figure 2. ELISA titres in the false negative FlexSure group were significantly lower than in the true positive group (P<0.0001).
Table 1.
Accuracy of FlexSure near patient test compared with Helicobacter pylori status as determined by enzyme linked immunosorbent assay (ELISA)
| Result of FlexSure test* |
H pylori status by ELISA
|
||
|---|---|---|---|
| Positive | Negative | Total | |
| Positive | 90 | 5 | 95 |
| Negative | 44 | 236 | 280 |
| Total | 134 | 241 | 375† |
Sensitivity 67% (95% CI 59% to 75%), (90/134); specificity 98% (95% to 99%), (236/241).
Excludes indeterminate results on ELISA (n=9) and invalid results on FlexSure (n=5) and patients who had no serum available (n=8).
Figure 2.
ELISA titre by FlexSure result
Performance of the test
Only one practice had a centrifuge. In all other practices blood specimens were allowed to stand before testing. The mean number of tests performed in each practice was 21 (range 1-43) with a mean of 8 (range 1-31) being performed by each operator. Practice nurses performed 74% (292) of tests and general practitioners 17% (66); in 10% (39) of cases the operator was unknown. The invalid results occurred in five different practices. The mean number of false negative results per individual operator was 0.8 (range 0-5), and the mean number of false negatives per practice was 1 (range 0-8). There was no correlation between the number of tests performed by an operator and the percentage of false negative results (P=0.8). Nineteen (79%) of the 24 general practitioners and practice nurses surveyed about the test replied. Eighteen (95%) respondents reported that the test was easy to perform and the results easy to interpret. Four (21%) respondents found it a problem to wait for serum to form, and only two (11%) believed the patients found it a problem to wait for results. Patients were usually contacted by phone with the result.
Endoscopic findings in the test and refer versus endoscopy group
Of the 394 patients who underwent the FlexSure test, 199 had been randomised to the H pylori test and refer strategy. In this group 52 (26%) patients had a positive result on the FlexSure test; 49 attended for endoscopy and three refused endoscopy. Endoscopic diagnoses in this group are shown in table 2. Eleven of the 12 patients with duodenal ulcers and the seven patients with erosive duodenitis were also positive for H pylori on urease testing (CLO test, Delta West Ply, Bentley, Australia). One patient had a malignant gastric ulcer. Of the 147 patients with a negative result on the FlexSure test, 39 were later referred for endoscopy; one had erosive duodenitis and one had a gastic ulcer, both were positive for H pylori on urease testing.
Table 2.
Endoscopic findings* in patients selected by FlexSure result compared with early endoscopy strategies according to patient group
| Endoscopic findings | Test and refer (n=199)
|
No (%) unselected (n=170) | ||
|---|---|---|---|---|
| Early (FlexSure positive n=49) | Later (FlexSure negative n=39) | Total | ||
| Normal | 19 | 30 | 49 | 85 (50) |
| Oesophagitis | 12 | 11 | 23 | 58 (34) |
| Gastro-oesophageal cancer | 1 | 1 | 1 | 0 (0) |
| Conditions where H pylori eradication indicated: | ||||
| Duodenal ulcer | 12† | 0 | 12† | 20† (12) |
| Erosive duodenitis | 7 | 1 | 8 | 14 (8) |
| Gastric ulcer | 7 | 1 | 8 | 5‡ (3) |
Dual pathology recorded separately.
One patient in each group was negative for H pylori on urease testing
Two patients were negative for H pylori on urease testing.
Thus of the 199 randomised to the test and refer strategy, 28 (14%) were found to have conditions for which H pylori eradication is indicated, although only 26 (13%) were detected as a result of positive results on FlexSure testing. By comparison, 39 (23%) of 170 patients randomised to early endoscopy had conditions warranting eradication treatment—an absolute difference of 9% (1% to 17%).
Discussion
Near patient tests for H pylori have provided general practitioners with a quick and easy method of testing. Apart from two small studies, however, the performance of these tests has not been assessed in primary care.9,10 We have found that the performance of one near patient test, which we had previously found to be satisfactory in secondary care was notably poorer with a much lower sensitivity when used in primary care. The explanation for this change is not entirely clear. None of the operators reported difficulty in interpreting the test results. No association was found between the total number of tests performed by an operator and the proportion of false negative results, although most operators performed fewer than 20 tests. We did find that the H pylori antibody titre in the group with false negative FlexSure test results was significantly lower than in true positive group. This might indicate that antibody titres in our original series of patients in secondary care were higher overall than in primary care, with fewer patients with ELISA titres close to borderline.
The immediate question that arises is whether our findings apply to other near patient tests for H pylori. Only one other test, the Helisal rapid blood test, has been validated in primary care. In secondary care this test was reported to have a sensitivity of 88% and specificity of 91%.6 In contrast, Jones et al obtained a sensitivity of 83% and specificity of 78% in primary care in England,9 while Talley et al found the sensitivity was only 59% and specificity 90%, when used by general practitioners in Australia.10
The impact of the lower sensitivity in our randomised trial seems to have been considerable as the diagnostic yield of ulcer disease in patients positive for H pylori in the test and refer group was only two thirds that of the immediate endoscopy group—a figure exactly in line with that expected from the reduced sensitivity of the test.
Of the various tests for H pylori available for use in primary care the main attraction of the near patient tests is that the results are available rapidly enough to guide initial management. Our results and those of others, however, show that the current tests are not sufficiently accurate to be used safely for a strategy of testing and referring patients positive for H pylori for endoscopy. Whether these tests are suitable to guide a strategy of testing and treating patients positive for H pylori is debatable. Symptoms of dyspepsia tend to recur and the uncertainty engendered by an insensitive test may lead to either increased empiric H pylori eradication or increased referral for endoscopy, or both. As a whole therefore the benefit of a rapid result is not sufficient to compensate for the inaccuracy of the current near patient tests. On the available evidence the best tests for H pylori in primary care remain either laboratory based serology or a carbon labelled urea breath test.12
Acknowledgments
We thank the Nottingham general practitioners and practice nurses whose considerable efforts in recruiting patients made the trial possible.
Footnotes
Funding: The Nottingham Dyspepsia Management Trial has been funded by the NHS Primary/Secondary Interface R&D Programme, Trent Region R&D, Wyeth-Lederle, and Abbott Laboratories. The near patient tests and ELISAs were provided by SmithKline Diagnostics.
Competing interests: None declared.
References
- 1.Office of Health Economics. Compendium of health statistics. 10th ed. London: Office of Health Economics; 1997. [Google Scholar]
- 2.British Society of Gastroenterology. Dyspepsia management guidelines [abstract]. London: British Society of Gastroenterology; 1996. [Google Scholar]
- 3.American Gastroenterological Association. American Gastroenterological Association medical position statement: evaluation of dyspepsia. Gastroenterology. 1998;114:579–581. doi: 10.1016/s0016-5085(98)70541-4. [DOI] [PubMed] [Google Scholar]
- 4.Stone M, Mayberry J, Wicks A, Livsey S, Stevens M. The Helisal test: an assessment of readability and performance [abstract] Gut. 1996;39:110. [Google Scholar]
- 5.Peitz U, Tillenburg B, Baumann M. Insufficient validity of a new rapid whole blood test for Helicobacter pylori(HP) infection [abstract] Gastroenterology. 1996;110:226. [Google Scholar]
- 6.Moayyedi P, Carter A, Catto A, Heppell R, Grant P, Axon A. Validation of a rapid whole blood test for diagnosing Helicobacter pylori. BMJ. 1997;314:119. doi: 10.1136/bmj.314.7074.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reilly T, Poxon V, Sanders D, Elliott T, Walt R. Comparison of serum, salivary, and rapid whole blood diagnostic test for Helicobacter pylori and their validation against endoscopy tests. Gut. 1997;40:454–458. doi: 10.1136/gut.40.4.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kroser J, Faigel D, Furth E, Metz D. Comparison of rapid office-based serology with formal laboratory-based ELISA testing for diagnosis of Helicobacter pylori gastritis. Dig Dis Sci. 1998;43:103–108. doi: 10.1023/a:1018832306135. [DOI] [PubMed] [Google Scholar]
- 9.Jones R, Phillips I, Felix G, Tait C. An evaluation of near-patient testing for Helicobacter pylori in general practice. Aliment Pharmacol Ther. 1997;11:01–05. doi: 10.1046/j.1365-2036.1997.125296000.x. [DOI] [PubMed] [Google Scholar]
- 10.Talley N, Lambert JR, Howell S, Lin HHX, Agreus L. An evaluation of whole blood testing for Helicobacter pylori in general practice. Aliment Pharmacol Ther. 1998;12:641–645. doi: 10.1046/j.1365-2036.1998.00363.x. [DOI] [PubMed] [Google Scholar]
- 11.Duggan A, Logan RPH, Knifton A, Logan RFA. Accuracy of near-patient blood tests for Helicobacter pylori. Lancet. 1996;348:617. doi: 10.1016/S0140-6736(05)64835-0. [DOI] [PubMed] [Google Scholar]
- 12.Churchill RD, Hill PG, Holmes GKT. Breath test is better than near patient blood tests. BMJ. 1998;316:1389. [PubMed] [Google Scholar]