Abstract
OBJECTIVE
Prior research has shown that less social support is associated with increased mortality in individuals with chronic illnesses. We set out to determine whether lower propensity to seek support as indicated by relationship style, based on attachment theory, is associated with mortality in patients with diabetes.
RESEARCH DESIGN AND METHODS
A total of 3,535 nondepressed adult patients with type 1 and type 2 diabetes enrolled in a health maintenance organization in Washington State were surveyed at baseline and followed for 5 years. Relationship style was assessed at baseline. Patients with a greater propensity to seek support were classified as having an interactive relationship style and those less inclined to seek support as having an independent relationship style. We collected Washington State mortality data and used Cox proportional hazards models to estimate relative risk (RR) of death for relationship style groups.
RESULTS
The rate of death in the independent and interactive relationship style groups was 39 and 29 per 1,000 individuals, respectively. Unadjusted RR of death was 1.33 (95% CI 1.12–1.58), indicating an increased risk of death among individuals with an independent relationship style. After adjustment for demographic and clinical covariates, those with an independent relationship style still had a greater risk of death compared with those with an interactive relationship style (hazard ratio 1.20 [95% CI 1.01–1.43]).
CONCLUSIONS
In a large sample of adult patients with diabetes, a lower propensity to reach out to others is associated with higher mortality over 5 years. Further research is needed to examine possible mechanisms for this relationship and to develop appropriate interventions.
The presence of a supportive social network positively affects health by increasing access to instrumental, informational, and emotional support (1). In patients with diabetes, a higher level of social support is associated with improved treatment adherence, better glycemic control, and greater diabetes knowledge (2). Conversely, lower social support has been associated with higher mortality in patients with various chronic conditions (3,4), including patients with diabetes (5).
Clinicians treating patients with chronic conditions generally understand these associations and attempt to encourage patients to seek and receive greater support from patients' family, friends, peers, and social agencies. Clinicians may also encourage greater collaboration in the patient-provider relationship. Although many patients are receptive to such suggestions and efforts, a significant proportion is less receptive or not receptive at all. For example, regardless of the ready availability of a social network, many patients do not benefit from their support at times of need. Among patients who do not collaborate well with others, many have long-term patterns of not doing so, suggesting the influence of stable characteristics. If there are measurable patient characteristics that predict an individual's capacity to use supports over time, such information may be useful for shaping approaches and recommendations that providers make in clinical settings.
Attachment theory provides a theoretical, evidence-based model for understanding the propensity and ability of individuals to reach out to others for support. This theory posits that all individuals develop a cognitive map based on prior experiences that determines one's comfort and ability to interact with or reach out to others, particularly at times of distress (6). On the basis of empirical research in infants, children, and adults over the past 30 years, distinct relationship styles arising from these cognitive maps have been identified (7) and demonstrate high levels of stability and continuity between early childhood and adulthood (8). Two of the styles, “dismissing” and “fearful” attachment style, are characterized by difficulty reaching out for support or trusting others, and patients with these styles and characteristics have been described as having an independent relationship style (9). Among clinical populations with diabetes, 48% of patients are typically found to have an independent relationship style (10). The remainder have an interactive relationship style, comprising those with “secure” and “preoccupied” attachment styles. Patients with an interactive relationship style have greater comfort reaching out to others, although individuals with a preoccupied style are often characterized as being highly dependent on others (11).
In a large sample of primary care patients with diabetes (9,12), an independent relationship style has been associated with more missed primary care visits, lower satisfaction with care, higher A1C levels, and decreased adherence to exercise, quitting smoking, foot care, diet, and oral hypoglycemic medications. Another study showed that having a relationship style characterized by difficulty trusting or reaching out to others is associated with decreased adherence to glucose monitoring and insulin injections among patients with diabetes (13).
In a recent article, we demonstrated that patients with major depression in this epidemiological sample were more likely to die over a 5-year period (hazard ratio [HR] 1.53) (14). In the current study, we set out to determine whether relationship styles are associated with mortality in patients with diabetes. Because depression status is associated with poorer collaboration as measured by relationship style (15), we conducted our analyses in nondepressed patients. In the current study, we hypothesized that among nondepressed patients with diabetes, those with an independent relationship style would have higher mortality over a 5-year period than patients with an interactive relationship style.
RESEARCH DESIGN AND METHODS
Group Health Cooperative (GHC) is a mixed model prepaid health plan serving about 500,000 members in Washington State. Most GHC patients receive medical services within the integrated group practice, which includes 30 primary care clinics in Western Washington. The GHC enrollment is demographically similar to the area population. Nine GHC primary care clinics were selected for the study based on 1) having the largest number of patients with diabetes, 2) geographic proximity to Seattle, and 3) racial and ethnic diversity. All study procedures were approved by institutional review boards at GHC and the University of Washington.
The original cohort for this longitudinal study, the Pathways Epidemiology Study, was sampled from adults aged ≥18 years from the GHC diabetes registry who received care at any one of the nine study clinics between 2000 and 2002. The diabetes registry database includes all GHC members meeting any of the following eligibility criteria in the prior 12 months: filled prescription for insulin or an oral hypoglycemic agent, two fasting glucose levels ≥126 mg/dl in a 12-month period, two random plasma glucose levels ≥200 mg/dl in a 12-month period, two outpatient diagnoses of diabetes, or any inpatient diagnosis of diabetes. Beginning in March 2001, surveys were mailed to 9,064 potentially eligible patients, but 1,222 patients were later found to be ineligible because of death, disenrollment, and erroneous diagnosis of diabetes or cognitive impairment. Among 7,841 eligible patients, 4,839 subjects (61.7% of eligible patients) returned the baseline questionnaire.
Measures
Relationship style.
Participants completed the four-item Relationship Questionnaire (7) and were categorized as being characterized by one of four attachment styles. This instrument demonstrates convergent and discriminant validity with other self-report and interview ratings (7). The dismissing and fearful attachment styles, which are associated with difficulty trusting others and reaching out for support, were combined to form the independent relationship style group (10). The other two attachment styles, secure and preoccupied, were grouped together because they are associated with a greater propensity to reach out to others and formed the interactive relationship style group.
Clinical and demographic data.
The baseline questionnaire included demographic characteristics: age, sex, years of education, employment, race/ethnicity, and marital status. Questions about clinical status included age of onset and duration of diabetes, treatment at onset of disease, smoking, height, and weight. Type 1 diabetes was diagnosed in patients if age of onset was ≤30 years, insulin was the first treatment prescribed, and they were currently taking insulin.
Mortality.
GHC conducts an annual automated search of enrollee deaths using death registry files of Washington State. We determined the vital status of our participants using this information, and several additional deaths were ascertained at the time of the follow-up telephone survey. The date of death was obtained from Washington State death records.
Other measures.
Computerized pharmacy records were used to calculate a chronic disease score known as RxRisk, which was a measure of medical comorbidity based on prescription drug use in the previous 12 months (16). The RxRisk score has been shown to predict subsequent hospitalization and mortality rates over the next 1-year period. A higher score indicates more medical comorbidity (16). For this study, insulin, antidepressants, and oral hypoglycemic medications were not included in the RxRisk calculation, and we consider this score to be an index of overall medical comorbidity excluding diabetes and depression.
We searched the computerized medical record for baseline diagnoses in seven categories of diabetes complications (retinopathy, neuropathy, nephropathy, cerebrovascular, cardiovascular, peripheral vascular, and metabolic) to calculate a diabetes complications severity index, which has been shown to predict mortality and hospitalization rates over the next 1-year period in our system (17). We searched GHC automated data for the nearest A1C in the 18 months before the return date of the screening questionnaire.
Evidence of prior macrovascular and microvascular complications and coronary (stent placement, coronary artery bypass surgery, or angioplasty), cerebrovascular (carotid endarterectomy), and peripheral vascular procedures were developed from automated data using ICD-9 and CPT codes and verified by chart review. The specific codes and definitions of events were developed using methods developed in the Women's Health Initiative study (18).
Statistical analyses
Baseline demographic and clinical characteristics were compared between those with independent and interactive relationship styles using χ2 analyses or independent group t tests. Incident death rates per 1,000 individuals were calculated for the entire sample and separately for those with independent and interactive relationship style groups. We used a Cox proportional hazards model without covariates to compute the unadjusted HR that estimates the relative risk (RR) of death for the relationship style groups. A multivariable Cox model was also fit, examining the RR of death for the relationship groups including covariates that were chosen a priori because they are risk factors for mortality in our previous research or were found to have significant univariate relationships to the relationship style groups. Adjusted HRs and their 95% CIs were determined for relationship style and for each covariate.
All subjects were used in the analysis; those who died during the 5-year interval had a dependent variable of the time to death calculated by the difference between their study screening date and date of death obtained from Washington State death records. Patients were censored at their follow-up assessment data at the end of the study or when lost to follow-up, as determined by disenrollment from GHC. The average length of follow-up was 4.5 ± 0.9 years (mean ± SD) for the sample and 4.5 ± 0.9 years for each of the relationship style groups.
RESULTS
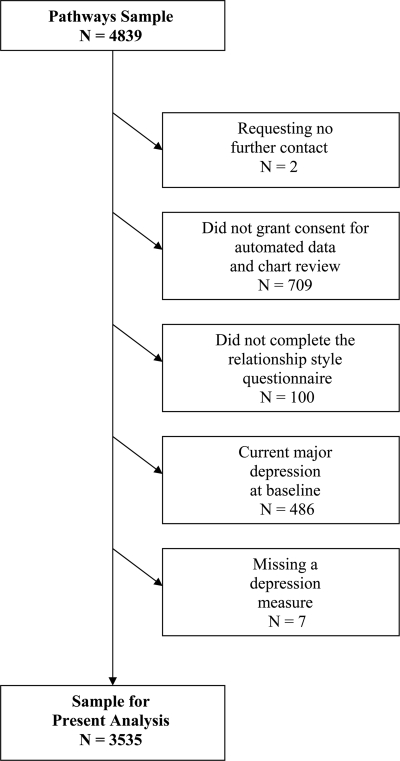
The analysis sample consisted of 3,535 participants with type 1 and type 2 diabetes who completed the 5-year assessment, who gave permission for their medical records to be abstracted, who completed the relationship style questionnaire at baseline, and who did not have current major depression at baseline (73.1% of the total respondent baseline sample) (Fig. 1).
Figure 1.
Pathways flow diagram for follow-up survey.
Baseline demographic and clinical characteristics were compared between the two relationship style groups and are described in Table 1. Compared with patients with independent relationship styles, patients with interactive relationship styles were significantly more likely to be male, white, more educated, and unmarried and have significantly higher BMI.
Table 1.
Baseline or prebaseline characteristics of participants by relationship style
| Relationship style groups |
Statistical test: χ2 df = 1 or t(df) = 3,533 | ||
|---|---|---|---|
| Interactive relationship style | Independent relationship style | ||
| n (%) | 1,902 (53.8) | 1,633 (46.2) | |
| Demographics | |||
| Male sex | 49.5 (941) | 43.4 (709) | 12.71* |
| Nonwhite | 16.3 (310) | 22.7 (371) | 22.88* |
| High school graduate or less | 21.2 (403) | 25.2 (412) | 7.86† |
| Unmarried | 28.9 (549) | 36.5 (596) | 23.03* |
| Age | 63.1 ± 13.0 | 63.5 ± 13.8 | 0.86 |
| Clinical characteristics | |||
| Type 1 diabetes | 5.2 (99) | 3.9 (63) | 3.34 |
| Treatment intensity | 2.10 | ||
| Nothing or diet | 25.3 (482) | 27.4 (448) | |
| Pills only | 45.5 (866) | 43.8 (715) | |
| Any insulin | 29.1 (554) | 28.8 (470) | |
| Years with diabetes | 9.7 ± 9.5 | 9.6 ± 9.6 | 0.25 |
| A1C (%) | 7.7 ± 1.5 | 7.7 ± 1.5 | 0.36 |
| Smoking | 7.2 (136) | 8.5 (138) | 1.90 |
| Hypertension diagnosis (ICD-9) | 43.5 (828) | 43.7 (714) | 0.01 |
| BMI | 31.5 ± 7.0 | 30.7 ± 6.6 | 3.36† |
| RxRisk | 3,062.4 ± 2,451.7 | 3,108.3 ± 2,308.3 | 0.57 |
| At least 1 microvascular event/procedure | 52.8 (1,004) | 52.5 (858) | 0.02 |
| Retinopathy | 38.4 (730) | 37.61 (614) | 0.22 |
| Nephropathy | 50.1 (952) | 51.98 (847) | 1.16 |
| Foot ulcer | 5.3 (101) | 4.8 (79) | 0.39 |
| Amputation | 1.3 (25) | 1.0 (17) | 0.56 |
| At least 1 macrovascular event/procedure | 20.6 (391) | 21.7 (355) | 0.74 |
| Myocardial infarction | 10.6 (201) | 11.7 (190) | 1.06 |
| Peripheral vascular disease procedure | 1.1 (20) | 1.0 (16) | 0.04 |
| Cerebrovascular procedure | 0.5 (10) | 0.7 (12) | 0.62 |
| Cardiovascular procedure | 9.1 (174) | 9.9 (162) | 0.61 |
| History of stroke | 6.0 (114) | 5.8 (94) | 0.09 |
Data are (%) n or means ± SD.
*P < 0.001;
†P < 0.01.
Overall the incident death rate was 34 per 1,000 individuals. The rate of death in the interactive relationship style group was 29 per 1,000 individuals (n = 251), whereas in the independent style group, the death rate was 39 per 1,000 individuals (n = 282). The unadjusted RR of death for relationship style was 1.33 (95% CI 1.12–1.58), indicating that those in the independent relationship style group had a 33% increased risk of death. Table 2 presents the Cox proportional hazards model used to derive the adjusted RR for relationship style. In the presence of salient sociodemographic, clinical, and disease severity covariates, those with an independent relationship style had a 20% increased risk of death compared with those with an interactive relationship style, the model demonstrating modest significance (HR 1.20 [95% CI 1.01–1.43]). In addition, risk of death within the 5-year period was significantly related to older age, being unmarried, more years with diabetes, using insulin, current smoking, increased medical comorbidity, having at least one macrovascular event or procedure, and having at least one microvascular event or procedure.
Table 2.
Cox proportional hazards model for death within 5 years
| HR (95% CI) | |
|---|---|
| Relationship style (independent style = 1) | 1.20 (1.01–1.43)* |
| Sociodemographic covariates | |
| Age (per year) | 1.06 (1.05–1.07)† |
| Sex (1 = female) | 0.95 (0.78–1.15) |
| Racial ethnicity (1 = nonwhite) | 0.84 (0.65–1.09) |
| Marital status (1 = unmarried) | 1.35 (1.11–1.63)‡ |
| Education (1 = high school graduate or less) | 1.01 (0.84–1.22) |
| Clinical and disease severity covariates | |
| Years with diabetes | 1.01 (1.01–1.02)‡ |
| Type of diabetes (1 = type 1) | 0.50 (0.22–1.11) |
| Treatment intensity (diet/exercise = reference group) | |
| 1 = Oral medication only | 1.06 (0.84–1.35) |
| 2 = Insulin (with or without oral medication) | 1.41 (1.08–1.85)‡ |
| A1C level | 1.01 (0.94–1.08) |
| Current smoker (1 = yes) | 1.59 (1.12–2.25)‡ |
| Hypertension (1 = presence) | 1.01 (0.84–1.21) |
| RxRisk score (medical comorbidity score) | 1.01 (1.01–1.02)† |
| At least 1 macrovascular event or procedure | 1.54 (1.29–1.85)† |
| At least 1 microvascular event or procedure | 1.72 (1.40–2.11)† |
| BMI | 0.99 (0.97–1.01) |
Data are HR (95% CI). n = 3,535.
*P < 0.05;
†P < 0.001;
‡P < 0.01.
CONCLUSIONS
Prior studies have demonstrated that lower support-seeking behavior is associated with poorer treatment adherence and poorer diabetes outcomes. For example, an independent relationship style in patients with diabetes is associated with missed primary care visits, higher A1C levels, lower satisfaction with health care, and decreased adherence to foot care, exercise, diet, oral hypoglycemic medication use, insulin injections, glucose monitoring, and smoking cessation (9,12,13). This study adds to these findings by showing that patients with diabetes who are less likely to seek support based on their relationship style have a significantly higher risk of death (HR 1.20) compared with those who are more likely to seek support, even after controlling for potential risk factors of mortality known to also be associated with relationship styles such as age, marital status, medical comorbidity, diabetes complications, and BMI (9).
This is the first known study to demonstrate that relationship styles, or attachment styles, show an association with mortality. It is possible that there are immunological differences between relationship style groups (19) or that the buffering effects of social support on the stress response may have beneficial effects on immune function or neuroendocrine and cardiovascular reactivity (20). However, poorer adherence to diabetes self-care and related lifestyle behaviors in patients with an independent relationship style may be the main mediator of this association. Many self-management behaviors related to diabetes are optimally undertaken in collaboration with support of others—family, peers, and health care providers. For example, smoking cessation is best carried out with the emotional, motivational, and tangible support of others. Changing or maintaining behaviors related to a healthy diet and exercise are best undertaken with supportive others, i.e., those who are actually doing the cooking, or others with whom to exercise also provide motivational support. In addition, as a chronic condition gets more severe or as the number of complications or other medical comorbidities accumulates, a self-reliant approach (i.e., “being a self-starter”) that worked initially may no longer be effective or may become a liability. In other words, the proportion of tasks that require support of others for completion begins to outweigh tasks that can be carried out without the support of others. Longitudinal studies using repeated measures of self-management are needed to definitively determine whether decreased levels of self-care and adherence are primary mediators of the association between relationship style and mortality.
Clinicians in medical settings are uniquely poised to help change the trajectory of outcomes in patients with an independent relationship style. However, rather than focusing on changing an individual's relationship style, a clinical team can offer a patient alternative ways of engaging with the health care system in pursuing desired outcomes. For example, in a study that examined depression management in 324 patients with diabetes (10), a collaborative care approach that involved a focus on patient preferences, tailoring of patients' care through outreach or extra telephone calls with a nurse case manager, and facilitation of communication between the patient and the primary care provider was compared with usual primary care. Among patients with an independent relationship style, collaborative care resulted in significantly reduced depression over 12 months and significantly greater satisfaction with care compared with usual care control subjects. Among patients receiving the intervention, those with an independent relationship style also received significantly more case management sessions than patients with an interactive relationship style even though relationship style was not actively used to determine session frequency. Among patients with an interactive relationship style, there was no difference in depression outcomes between the two treatment arms. This somewhat paradoxical outcome points out that patients with an interactive relationship style probably already have an advantage in interacting with providers and health teams to navigate through a relatively fragmented prevailing health care system (i.e., usual care) compared with individuals with an independent relationship style, and the intervention components did not confer any added advantage.
Current initiatives to reduce health care fragmentation are slow in taking shape because of the expense and need for significant system redesign. A focus on relationship style–focused care in the patient-provider relationship may be attractive from the perspective of resource-limited health care systems. Clinical education about the theoretical basis and evidence regarding relationship styles may be followed by clinical use of one of the many validated attachment style measurement instruments (21). Such steps may encourage greater provider empathy and understanding with less collaborative patients who might otherwise be labeled as “difficult” (22) because of missed appointments and lack of adherence to physician recommendations and provoke nihilism or power struggles from busy providers.
In addition to collaborative care interventions (10,23), other existing strategies may be used to address patients' need for autonomy while respecting their potential fear of intimacy. The result may be increases in collaboration, treatment adherence, and outcomes. For example, clinical methods that increase patient empowerment, techniques based on motivational interviewing, relationship-focused problem-solving therapy, assisted navigators (24), patient coaching, or use of prompt sheets (25) in which interpersonal preferences can be stated and addressed all hold promise as potential interventions in this regard.
If we assume that the impact of independent relationship styles on poor outcomes could be significantly reduced using clinical strategies, it is worth considering the public health benefits of such strategies. One way to explore these is to get a better understanding of the adverse impact that an independent relationship style can have on a population of individuals with diabetes by comparing it to the impact of depression on health outcomes and mortality in patients with diabetes. For example, we have previously found in this same epidemiological sample that the adjusted odds of all-cause mortality in patients with major depression compared with that in nondepressed patients was 1.53 (95% CI 1.19–1.96) (14). With a prevalence of major depression of 12%, the population-attributable risk percent effect is estimated to be 4.94%, i.e., the percentage of the population in whom a given outcome (e.g., death) could be theoretically eliminated by addressing the factor causing the outcome (e.g., depression). In the current analysis, in nondepressed patients with diabetes, 46%, or approximately four times as many individuals, have an independent relationship style, albeit with a lower associated risk of mortality (HR 1.20). From a population attributable risk percent perspective, however, assuming that the adverse impact of an independent relationship style on health outcomes could be significantly reduced, the theoretical percentage of deaths that could be similarly eliminated by addressing the impact of an independent relationship style is 12.48%. In reality, the association between major depression and death or relationship style and death is highly complex. This comparison, however is useful in that it suggests that if there are actions that can reduce the influence of an independent relationship style on outcomes in patients with diabetes, there is a strong possibility of improving outcomes and reducing mortality over time.
Strengths of this study include the following characteristics: clinical diagnosis of diabetes from chart data, automated data-derived indexes of medical comorbidity and complications, automated laboratory data, and automated collection of death data based on state records. In addition to demographic characteristics, our baseline data included a number of clinical characteristics including diabetes duration, specific diabetes treatment type, and treatment adherence. Further strengths include the fact that this is a large representative primary care population sample of patients with diabetes. In addition, the longitudinal nature of this study, with measures of relationship style at baseline with subsequent death data, improves the validity of the results as compared with cross-sectional data.
Limitations of the study include the fact that these data may not generalize to other populations, e.g., rural populations, or populations with lower socioeconomic status or with limitations in insurance coverage. Also, a limitation of these data is that even with a moderately high response rate at baseline, there was some attrition of the sample over the 5-year follow-up period.
In summary, in a large primary care sample of adult patients with diabetes, having a lower propensity to reach out to others is associated with higher mortality over 5 years. Further research is needed to examine possible mechanisms for this relationship and to develop effective interventions.
Acknowledgments
This study was supported by grants from the National Institute of Mental Health (K24-MH-067587 to W.J.K. and MH-073686 to M.V.K.).
P.C. is CEO of Samepage, which is in the business of consulting and creating interventions to improve patient-provider relationships. No other potential conflicts of interest relevant to this article were reported.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Berkman LF: The role of social relations in health promotion. Psychosom Med 1995;57:245–254 [DOI] [PubMed] [Google Scholar]
- 2. Fukunishi I, Horikawa N, Yamazaki T, Shirasaka K, Kanno K, Akimoto M: Perception and utilization of social support in diabetic control. Diabetes Res Clin Pract 1998;41:207–211 [DOI] [PubMed] [Google Scholar]
- 3. Berkman LF, Syme SL: Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol 1979;109:186–204 [DOI] [PubMed] [Google Scholar]
- 4. Kaplan GA, Salonen JT, Cohen RD, Brand RJ, Syme SL, Puska P: Social connections and mortality from all causes and from cardiovascular disease: prospective evidence from eastern Finland. Am J Epidemiol 1988;128:370–380 [DOI] [PubMed] [Google Scholar]
- 5. Zhang X, Norris SL, Gregg EW, Beckles G: Social support and mortality among older persons with diabetes. Diabetes Educ 2007;33:273–281 [DOI] [PubMed] [Google Scholar]
- 6. Bowlby J: Attachment and Loss, Vol. II: Separation: Anxiety and Anger. New York, Basic Books, 1973. [Google Scholar]
- 7. Griffin DW, Bartholomew K: The metaphysics of measurement: the case of adult attachment. Adv Pers Relat 1994;5:17–52 [Google Scholar]
- 8. Waters E, Merrick S, Treboux D, Crowell J, Albersheim L: Attachment security in infancy and early adulthood: a twenty-year longitudinal study. Child Dev 2000;71:684–689 [DOI] [PubMed] [Google Scholar]
- 9. Ciechanowski P, Russo J, Katon W, Von Korff M, Ludman E, Lin E, Simon G, Bush T: Influence of patient attachment style on self-care and outcomes in diabetes. Psychosom Med 2004;66:720–728 [DOI] [PubMed] [Google Scholar]
- 10. Ciechanowski PS, Russo JE, Katon WJ, Korff MV, Simon GE, Lin EH, Ludman EJ, Young BA: The association of patient relationship style and outcomes in collaborative care treatment for depression in patients with diabetes. Med Care 2006;44:283–291 [DOI] [PubMed] [Google Scholar]
- 11. Bartholomew K: Avoidance of intimacy: an attachment perspective. J Soc Pers Relat 1990;7:147–178 [Google Scholar]
- 12. Ciechanowski P, Russo J, Katon W, Simon G, Ludman E, Von Korff M, Young B, Lin E: Where is the patient? The association of psychosocial factors and missed primary care appointments in patients with diabetes. Gen Hosp Psychiatry 2006;28:9–17 [DOI] [PubMed] [Google Scholar]
- 13. Turan B, Osar Z, Turan JM, Ilkova H, Damci T: Dismissing attachment and outcomes in diabetes: the mediating role of coping. J Soc Clin Psychol 2003;22:607–626 [Google Scholar]
- 14. Lin EH, Heckbert SR, Rutter CM, Katon WJ, Ciechanowski P, Ludman EJ, Oliver M, Young BA, McCulloch DK, Von Korff M: Depression and increased mortality in diabetes: unexpected causes of death. Ann Fam Med 2009;7:414–421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ciechanowski P, Katon W, Russo J: The association of depression and perceptions of interpersonal relationships in patients with diabetes. J Psychosom Med 2005;58:139–144 [DOI] [PubMed] [Google Scholar]
- 16. Fishman PA, Goodman MJ, Hornbrook MC, Meenan RT, Bachman DJ, O'Keeffe Rosetti MC: Risk adjustment using automated ambulatory pharmacy data: the RxRisk model. Med Care 2003;41:84–99 [DOI] [PubMed] [Google Scholar]
- 17. Young BA, Lin E, Von Korff M, Simon G, Ciechanowski P, Ludman EJ, Everson-Stewart S, Kinder L, Oliver M, Boyko EJ, Katon WJ: Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. Am J Manag Care 2008;14:15–23 [PMC free article] [PubMed] [Google Scholar]
- 18. Curb JD, McTiernan A, Heckbert SR, Kooperberg C, Stanford J, Nevitt M, Johnson KC, Proulx-Burns L, Pastore L, Criqui M, Daugherty S: Outcomes ascertainment and adjudication methods in the Women's Health Initiative. Ann Epidemiol 2003;13(Suppl. 9):S122–S128 [DOI] [PubMed] [Google Scholar]
- 19. Picardi A, Battisti F, Tarsitani L, Baldassari M, Copertaro A, Mocchegiani E, Biondi M: Attachment security and immunity in healthy women. Psychosom Med 2007;69:40–46 [DOI] [PubMed] [Google Scholar]
- 20. Uchino BN: Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med 2006;29:377–387 [DOI] [PubMed] [Google Scholar]
- 21. Stein H, Jacobs NJ, Ferguson KS, Allen JG, Fonagy P: What do adult attachment scales measure? Bull Menninger Clin 1998;62:33–82 [PubMed] [Google Scholar]
- 22. Macdonald M: Seeing the cage: stigma and its potential to inform the concept of the difficult patient. Clin Nurse Spec 2003;17:305–310; quiz 311–312 [DOI] [PubMed] [Google Scholar]
- 23. Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH: Collaborative management of chronic illness. Ann Intern Med 1997;127:1097–1102 [DOI] [PubMed] [Google Scholar]
- 24. Dohan D, Schrag D: Using navigators to improve care of underserved patients: current practices and approaches. Cancer 2005;104:848–855 [DOI] [PubMed] [Google Scholar]
- 25. Kaplan SH, Greenfield S, Ware JE, Jr: Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care 1989;27(Suppl. 3):S110–S127 [DOI] [PubMed] [Google Scholar]