Abstract
OBJECTIVE
To evaluate cardiovascular disease (CVD) and total mortality associated with thoracoabdominal calcifications.
RESEARCH DESIGN AND METHODS
Thoracoabdominal calcifications of native radiograms were evaluated in 833 subjects with type 2 diabetes and 1,292 subjects without diabetes, aged 45–64 years, without prior evidence of CVD. The type 2 diabetic and nondiabetic study cohorts were followed up for 18 years.
RESULTS
After adjustment for conventional risk factors, marked thoracoabdominal calcifications predicted CVD/total mortality with hazard ratio (HR) (95% CI) of 1.5 (0.8–3.0)/1.8 (1.1–2.9) in type 2 diabetic men, 3.0 (1.6–5.7)/3.1 (1.9–5.0) in type 2 diabetic women, 5.0 (2.2–12)/4.0 (2.2–7.4) in nondiabetic men, and 7.8 (1.8–34)/3.0 (1.3–7.0) in nondiabetic women and in the presence of C-reactive protein below/over 3 mg/l with HR of 2.4 (1.3–4.4)/3.0 (1.4–6.1) in type 2 diabetic subjects and 4.0 (1.5–10.8)/6.6 (2.7–16.0) in nondiabetic subjects.
CONCLUSIONS
Thoracoabdominal calcifications in native radiograms are significant predictors of CVD and total mortality, especially in type 2 diabetic and nondiabetic women with elevated high-sensitivity C-reactive protein level.
Vascular calcification is initiated by metabolic, mechanical, infectious, or inflammatory injury to vasculature. Its progression is mainly determined by inflammatory response to vascular injury (1). It may precede cardiovascular disease (CVD) morbidity and mortality by years or decades in subjects with type 2 diabetes (2) and in the general population (3–6). Medial calcification has been associated with CVD morbidity and mortality in diabetic subjects (7) and in subjects with end-stage renal disease (8). Calcifications can be divided into intimal type, medial type of arterial calcification, cardiac valve calcification, and vascular calciphylaxis (9). These four entities of calcifications are consequences of distinct but overlapping pathophysiological mechanisms, which can occur simultaneously. Calcifications may function as a limiting factor for intimal plaque growth and represent a biological response to this process (10). A new perspective to the question of clinical significance of calcification has evolved from the practical need to evaluate CVD effects of medications targeted to bone formation and the bone density effects of medications targeted to vascular welfare (11,12).
Although inflammation is involved in the initiation and progression of vascular calcification, inflammation and calcification may reflect partly independent processes. A combination of markers of calcification and inflammation might therefore be a good predictor CVD mortality. This study evaluates thoracoabdominal calcifications, and their combination with elevated high-sensitivity C-reactive protein (hs-CRP), in prediction of CVD mortality in a cohort of two diabetic and nondiabetic subjects without prior evidence of CVD during an 18-year follow-up.
RESEARCH DESIGN AND METHODS
A detailed description of the original study population including 1,059 type 2 diabetic and 1,373 nondiabetic subjects aged 45–64 years has been published previously (13). Subjects with prior CVD (n = 301) or missing information on calcification (n = 6) were excluded. Of 2,125 participants, 1,862 subjects (317 men and 370 women with type 2 diabetes, 511 nondiabetic men, and 610 nondiabetic women) were available for the analyses of hs-CRP. End points were total and CVD mortality by the International Classification of Diseases, Ninth Revision (ICD-9) codes 390–459. The 18-year follow-up lasted until 1 January 2001.
hs-CRP was analyzed with latex turbidimetric immunoassay (Wako Chemicals, Neuss, Germany), with detection limit of 0.06 mg/l. The interassay coefficient of variation was 3.3 and 2.7% at mean hs-CRP levels of 1.52 (n = 116) and 2.51 (n = 168) mg/l, respectively. From lateral lumbar radiograms, taken with the patient in a standing position, thoracoabdominal calcification was graded by a radiologist (M.S.) from no calcification (grade 0) to marked calcification (grade 3) blinded to clinical data. The κ coefficient (SE) for intraobserver variation was 0.87 (0.24).
Data analyses were conducted with the SPSS 14.0.1 program (SPSS, Chicago, IL). Cox models for CVD and total mortality were adjusted for age, sex, status of diabetes, area of residence, current smoking, systolic blood pressure, total cholesterol, HDL cholesterol, BMI, glomerular filtration rate, urinary protein (log), fasting glucose (in nondiabetic subjects) or glycated hemoglobin A1 (in type 2 diabetic subjects), and duration of diabetes (in type 2 diabetic subjects). A P value <0.05 was considered statistically significant. The ethics committees of the Kuopio University Hospital and the Turku University Central Hospital approved the study. All study participants gave informed consent.
RESULTS
During the 18-year follow-up, 817 all-cause deaths and 465 CVD deaths occurred. Baseline characteristics are given in online appendix Table A1 (available at http://care.diabetesjournals.org/cgi/content/full/dc09-1813/DC1). Thoracoabdominal calcifications were more frequent in men than women (66.1 vs. 55.7%) and in type 2 diabetic than nondiabetic subjects (71.5 vs. 53.6%). The presence of thoracoabdominal calcifications was associated with the presence of hs-CRP ≥3 mg/l in type 2 diabetic women (P = 0.006), not quite in nondiabetic women (P = 0.069), and not in nondiabetic men (P = 0.739) or in type 2 diabetic men (P = 0.550).
In multivariate analysis, thoracoabdominal calcifications predicted CVD mortality independently of other risk factors in type 2 diabetic women, nondiabetic men, and nondiabetic women but not in type 2 diabetic men (online appendix Table A2). CVD survival was markedly dependent on the presence of calcifications and the status of diabetes at baseline, as presented by sex in online appendix Fig. A1. There was no interaction between sex and thoracoabdominal calcifications (P = 0.678) in prediction of CVD mortality. However, an interaction was observed between sex and hs-CRP in association with thoracoabdominal calcifications (P = 0.037 for the interaction term of hs-CRP by sex).
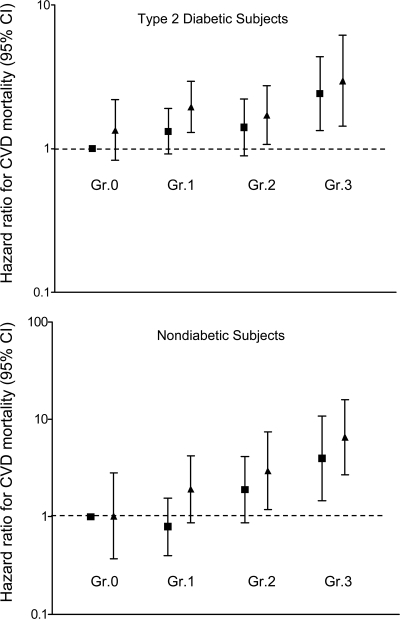
The association of thoracoabdominal calcification grade with CVD and total mortality was consistent in subgroups with hs-CRP <3 and ≥3 mg/l (online appendix Fig. A2). Multivariate Cox analysis, including both hs-CRP and thoracoabdominal calcifications, suggested that they are independent predictors of CVD and total mortality. Hazard ratio (HR) of CVD death for calcification tended to be higher in the presence of elevated hs-CRP through calcification categories from 0 to 3 (Fig. 1).
Figure 1.
HR (95% CI) in Cox multivariate model of CVD mortality during 18-year follow-up for grade 1 (slight), grade 2 (moderate), and grade 3 (marked) calcification of thoracoabdominal aorta. The reference with HR 1 are the subjects with no thoracoabdominal calcifications (grade 0) and hs-CRP <3 mg/l. Squares mark subjects with hs-CRP <3 mg/l and triangles mark subjects with hs-CRP ≥3 mg/l. In multivariate analysis, marked thoracoabdominal calcifications predicted CVD in the presence of hs-CRP below/over 3 mg/l with HR (95% CI) of 2.4 (1.3–4.4)/3.0 (1.4–6.1) in type 2 diabetic subjects and 4.0 (1.5–10.8)/6.6 (2.7–16.0) in nondiabetic subjects.
CONCLUSIONS
In this 18-year follow-up study, marked thoracoabdominal calcifications predicted CVD and total mortality, especially in nondiabetic and type 2 diabetic women with elevated hs-CRP level.
The relative risk associated with calcifications was higher in nondiabetic subjects compared with diabetic subjects and in women compared with men. Predominance of aortic calcification was observed in women in the Reykjavik study, but sex differences in the risk associated to calcifications have not been observed (14). In our study, marked calcifications tended to signify a higher relative risk for CVD mortality in women than in men, but a statistically significant interaction with sex was not observed.
The risk increase of CVD death associated with the presence of calcifications was lower in the presence of low hs-CRP and higher in the presence of elevated hs-CRP. Calcium deposits may alter or stimulate the process of CVD (1), as they accumulate in dying cells and lipoprotein deposits, and activate endochondral and intramembranous types of ossification by secretion of inflammatory cytokines, tumor necrosis factor-α, and interleukin-1 and interleukin-8 (15). In this study, an interaction with sex between inflammatory activity and grade of calcifications was observed.
Combining hs-CRP, a surrogate of activity of atherosclerosis with the presence of calcifications, a surrogate of stage of atherosclerosis, the prognostic value improves. Based on the findings of the present study, detection of thoracoabdominal radiological calcification should lead to a detailed evaluation and treatment of CVD risk.
Supplementary Material
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Demer LL, Tintut Y: Vascular calcification: pathobiology of a multifaceted disease. Circulation 2008; 117: 2938– 2948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Reaven PD, Sacks J: Coronary artery and abdominal aortic calcification are associated with cardiovascular disease in type 2 diabetes. Diabetologia 2005; 48: 379– 385 [DOI] [PubMed] [Google Scholar]
- 3. Levitzky YS, Cupples LA, Murabito JM, Kannel WB, Kiel DP, Wilson PW, Wolf PA, O'Donnell CJ: Prediction of intermittent claudication, ischemic stroke, and other cardiovascular disease by detection of abdominal aortic calcific deposits by plain lumbar radiographs. Am J Cardiol 2008; 101: 326– 331 [DOI] [PubMed] [Google Scholar]
- 4. Niskanen L, Siitonen O, Suhonen M, Uusitupa MI: Medial artery calcification predicts cardiovascular mortality in patients with NIDDM. Diabetes Care 1994; 17: 1252– 1256 [DOI] [PubMed] [Google Scholar]
- 5. London GM, Guerin AP, Marchais SJ, Metivier F, Pannier B, Adda H: Arterial media calcification in end-stage renal disease: impact on all-cause and cardiovascular mortality. Nephrol Dial Transplant 2003; 18: 1731– 1740 [DOI] [PubMed] [Google Scholar]
- 6. Johnson RC, Leopold JA, Loscalzo J: Vascular calcification: pathobiological mechanisms and clinical implications. Circ Res 2006; 99: 1044– 1059 [DOI] [PubMed] [Google Scholar]
- 7. Iribarren C, Sidney S, Sternfeld B, Browner WS: Calcification of the aortic arch: risk factors and association with coronary heart disease, stroke, and peripheral vascular disease. JAMA 2000; 283: 2810– 2815 [DOI] [PubMed] [Google Scholar]
- 8. Hollander M, Hak AE, Koudstaal PJ, Bots ML, Grobbee DE, Hofman A, Witteman JC, Breteler MM: Comparison between measures of atherosclerosis and risk of stroke: the Rotterdam Study. Stroke 2003; 34: 2367– 2372 [DOI] [PubMed] [Google Scholar]
- 9. Wilson PW, Kauppila LI, O'Donnell CJ, Kiel DP, Hannan M, Polak JM, Cupples LA: Abdominal aortic calcific deposits are an important predictor of vascular morbidity and mortality. Circulation 2001; 103: 1529– 1534 [DOI] [PubMed] [Google Scholar]
- 10. Shao JS, Cai J, Towler DA: Molecular mechanisms of vascular calcification: lessons learned from the aorta. Arterioscler Thromb Vasc Biol 2006; 26: 1423– 1430 [DOI] [PubMed] [Google Scholar]
- 11. Hamerman D: Osteoporosis and atherosclerosis: biological linkages and the emergence of dual-purpose therapies. Q J Med 2005; 98: 467– 484 [DOI] [PubMed] [Google Scholar]
- 12. Naves M, Rodriguez-Garcia M, Diaz-Lopez JB, Gomez-Alonso C, Cannata-Andia JB: Progression of vascular calcifications is associated with greater bone loss and increased bone fractures. Osteoporos Int 2008; 19: 1161– 1166 [DOI] [PubMed] [Google Scholar]
- 13. Laakso M, Rönnemaa T, Pyörälä K, Kallio V, Puukka P, Penttilä I: Atherosclerotic vascular disease and its risk factors in non-insulin-dependent diabetic and nondiabetic subjects in Finland. Diabetes Care 1988; 11: 449– 463 [DOI] [PubMed] [Google Scholar]
- 14. Danielsen R, Sigvaldason H, Thorgeirsson G, Sigfusson N: Predominance of aortic calcification as an atherosclerotic manifestation in women: the Reykjavik study. J Clin Epidemiol 1996; 49: 383– 387 [DOI] [PubMed] [Google Scholar]
- 15. Nadra I, Mason JC, Philippidis P, Florey O, Smythe CD, McCarthy GM, Landis RC, Haskard DO: Proinflammatory activation of macrophages by basic calcium phosphate crystals via protein kinase C and MAP kinase pathways: a vicious cycle of inflammation and arterial calcification? Circ Res 2005; 96: 1248– 1256 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.