Abstract
OBJECTIVE
Type 2 diabetes is associated with insulin resistance and skeletal muscle mitochondrial dysfunction. We have found that subjects with early-onset type 2 diabetes show incapacity to increase Vo2max in response to chronic exercise. This suggests a defect in muscle mitochondrial response to exercise. Here, we have explored the nature of the mechanisms involved.
RESEARCH DESIGN AND METHODS
Muscle biopsies were collected from young type 2 diabetic subjects and obese control subjects before and after acute or chronic exercise protocols, and the expression of genes and/or proteins relevant to mitochondrial function was measured. In particular, the regulatory pathway peroxisome proliferator–activated receptor γ coactivator (PGC)-1α/mitofusin-2 (Mfn2) was analyzed.
RESULTS
At baseline, subjects with diabetes showed reduced expression (by 26%) of the mitochondrial fusion protein Mfn2 and a 39% reduction of the α-subunit of ATP synthase. Porin expression was unchanged, consistent with normal mitochondrial mass. Chronic exercise led to a 2.8-fold increase in Mfn2, as well as increases in porin, and the α-subunit of ATP synthase in muscle from control subjects. However, Mfn2 was unchanged after chronic exercise in individuals with diabetes, whereas porin and α-subunit of ATP synthase were increased. Acute exercise caused a fourfold increase in PGC-1α expression in muscle from control subjects but not in subjects with diabetes.
CONCLUSIONS
Our results demonstrate alterations in the regulatory pathway that controls PGC-1α expression and induction of Mfn2 in muscle from patients with early-onset type 2 diabetes. Patients with early-onset type 2 diabetes display abnormalities in the exercise-dependent pathway that regulates the expression of PGC-1α and Mfn2.
Early-onset type 2 diabetes is increasing in prevalence, in parallel with the worldwide obesity epidemic (1), and is typically characterized by early-onset obesity and severe insulin resistance in young people with a strong family history of type 2 diabetes (1,2). Weight reduction and increased physical exercise are effective treatments to improve insulin sensitivity. We have been studying the effects of a variety of exercise and dietary regimens in these very insulin-resistant patients. We recently demonstrated that a 3-month, four times weekly, aerobic exercise intervention in subjects with early-onset type 2 diabetes failed to improve Vo2max and had no significant effect on whole-body or hepatic insulin sensitivity (3). Equally obese nondiabetic control subjects had a 20% increase in Vo2max following the same regime. This suggested the possibility that, in these diabetic patients, chronic exercise training failed to activate a mitochondrial oxidative response.
Defective mitochondrial function in skeletal muscle has been reported in a variety of insulin-resistant states, including type 2 diabetes (4,5). Muscle mitochondria from type 2 diabetic subjects show reduced size and reduced activity of the electron transport chain (4,6). In parallel, type 2 diabetes is associated with reduced expression of genes of oxidative metabolism as well as repression of the mitofusin-2 (Mfn2) gene, which encodes the mitochondrial fusion protein mitofusin-2 (7–9). Decreased expression of nuclear genes encoding proteins of oxidative phosphorylation has been reported in skeletal muscle of nondiabetic individuals with a family history of type 2 diabetes (8,9), along with reduced in vivo oxidative phosphorylation (5). These findings suggest that mitochondrial abnormalities in type 2 diabetes may have a heritable component.
Chronic exercise induces mitochondrial biogenesis in skeletal muscle and enhances mitochondrial function (10). Exercise is known to induce PGC-1α (11), which in turn induces the transcription of different nuclear genes encoding mitochondrial proteins (12,13). One example is Mfn2, which is induced by PGC-1α through interaction with the transcription factor ERRα (14). This may be particularly relevant, since it has been reported that Mfn2 regulates not just mitochondrial fusion but also mitochondrial function through changes in mitochondrial membrane potential and the expression of OXPHOS subunits (15). The stimulatory effect of exercise on mitochondrial biogenesis and function has also been reported in muscle in insulin-resistant conditions such as obesity (6) and aging (16) and in type 2 diabetes (17).
Subjects who took part in the chronic exercise protocol (3) underwent skeletal muscle biopsies at baseline and after 3 months of exercise training. To address mechanistic questions, we measured the expression of mitochondrial proteins from this initial study. We then conducted an acute (short-term) exercise intervention protocol in a similar cohort of patients with early-onset type 2 diabetes and examined the expression in muscle biopsies of a range of specific mitochondrial genes and proteins. We hypothesized that the lack of a whole-body response to exercise training in the early-onset type 2 diabetic subjects may be a consequence of alterations in the abundance or activity of relevant mitochondrial proteins in skeletal muscle.
RESEARCH DESIGN AND METHODS
Subjects with early-onset type 2 diabetes (i.e., diagnosed before age 25 years and negative for GAD antibodies) were recruited from our clinic, along with obese and otherwise healthy subjects who were as far as possible matched for age and BMI, but with normal glucose tolerance and without family history of diabetes. All subjects were sedentary. All gave written informed consent for the study, which had been approved by the local research ethics committee.
Clinical and metabolic characteristics of both groups of subjects, in each study, are summarized in Tables 1 and 2.
Table 1.
Baseline characteristics of subjects in the chronic exercise study
| Control subjects | Youth with type 2 diabetes | |
|---|---|---|
| n | 6 | 7 |
| Male:female ratio | 0:6 | 5:2 |
| Age (years) | 22 ± 1 | 27 ± 1* |
| Duration of diabetes (years) | NA | 3.2 ± 1.5 |
| Treatment for diabetes | NA | Met 7; Met/SU 1 |
| Weight (kg) | 108.7 ± 10.6 | 108.1 ± 6.7 |
| BMI (kg/m2) | 37.78 ± 3.43 | 33.23 ± 1.81 |
| Systolic blood pressure (mmHg) | 104 ± 3 | 122 ± 5* |
| Diastolic blood pressure (mmHg) | 71 ± 3 | 72 ± 3 |
| Waist circumference (cm) | 113.2 ± 4.6 | 117.4 ± 3.2 |
| Waist-to-hip ratio | 0.91 ± 0.03 | 1.00 ± 0.09 |
| A1C (%) | 5.5 ± 0.2 | 8.2 ± 0.6† |
| Fasting glucose (mmol/) | 5.2 ± 0.2 | 9.1 ± 0.8† |
| Fasting insulin (pmol/l) | 91.1 ± 9.4 | 77.1 ± 12.3 |
| Fasting C-peptide (μg/l) | 3.4 ± 0.3 | 3.1 ± 0.4 |
| Total cholesterol (mmol/l) | 4.33 ± 0.21 | 4.50 ± 0.42 |
| HDL (mmol/) | 1.11 ± 0.08 | 0.88 ± 0.03* |
| LDL (mmol/l) | 2.57 ± 0.23 | 2.34 ± 0.35 |
| Triglycerides (mmol/l) | 1.41 ± 0.27 | 3.05 ± 0.64* |
| Free fatty acids (mmol/l) | 0.635 ± 0.053 | 0.820 ± 0.104 |
| Glucose disposal (μmol/min/kg/mU/l) | 26.25 ± 4.66 | 16.13 ± 4.16 |
| Vo2max (ml · kg−1 · min−1) | 28.61 ± 1.94 | 22.67 ± 1.57* |
Data are means ± SE, unless specified otherwise.
*Significantly different from control group (P < 0.05).
†Significantly different from control group (P < 0.01). Met, metformin; SU, sulfonylurea.
Table 2.
Baseline characteristics of subjects in the acute exercise study
| Control subjects | Youth with type 2 diabetes | |
|---|---|---|
| n | 7 | 12 |
| Male:female ratio | 2:5 | 10:2 |
| Age (years) | 26 ± 2 | 27 ± 1 |
| Duration of diabetes (years) | NA | 2.5 ± 0.7 |
| Treatment for diabetes | NA | Met 9; Met/Ins 2; Diet 3 |
| Weight (kg) | 113.9 ± 11.2 | 114.5 ± 7.3 |
| BMI (kg/m2) | 39.13 ± 2.54 | 36.13 ± 1.78 |
| Systolic blood pressure (mmHg) | 117 ± 3 | 127 ± 4 |
| Diastolic blood pressure (mmHg) | 75 ± 4 | 81 ± 3 |
| Waist circumference (cm) | 120.2 ± 6.1 | 111.4 ± 4.8 |
| Waist-to-hip ratio | 0.98 ± 0.03 | 0.99 ± 0.02 |
| A1C (%) | 5.6 ± 0.1 | 7.5 ± 0.5† |
| Fasting glucose (mmol/l) | 5.2 ± 0.1 | 8.0 ± 0.7† |
| Fasting insulin (pmol/l) | 163.0 ± 65.3 | 169.6 ± 61.7 |
| Fasting C-peptide (μg/l) | 5.3 ± 1.2 | 3.4 ± 0.4* |
| Total cholesterol (mmol/l) | 4.13 ± 0.32 | 4.29 ± 0.26 |
| HDL (mmol/l) | 1.30 ± 0.17 | 0.95 ± 0.05* |
| LDL (mmol/l) | 2.21 ± 0.29 | 2.63 ± 0.28 |
| Triglycerides (mmol/l) | 1.35 ± 0.20 | 1.76 ± 0.26 |
| Free fatty acids (mmol/l) | 0.67 ± 0.16 | 0.77 ± 0.22 |
| Vo2max (ml · kg−1 · min−1) | 22.85 ± 2.71 | 23.79 ± 1.79 |
Data are means ± SE, unless specified otherwise.
*Significantly different from control group (P < 0.05).
†Significantly different from control group (P < 0.01). Ins, insulin; Met, metformin.
Concurrent medications
None of the obese control subjects was receiving medications during the course of these studies.
Chronic exercise study.
All subjects were receiving metformin. One subject was also receiving gliclazide. Doses of oral hypoglycemic agents were unchanged during the course of the study.
Acute exercise study.
Three subjects were on dietary management alone. Seven of the 12 subjects were receiving oral hypoglycemic agents alone. Two subjects were on oral and insulin combination therapy (metformin plus basal bolus insulin treatment). All subjects on oral hypoglycemic agents were on stable doses throughout the duration of the study. Subjects on the combination therapy had their insulin doses reduced by ∼20% during the course of the study.
Baseline studies
Baseline studies were identical for both the chronic and acute exercise studies (3) and included the following.
Screening.
Each subject was screened with a medical history and physical examination and routine blood and urine biochemistries. Waist-to-hip ratio, weight, height, and BMI were measured. Blood pressure was measured using the left arm after the subject had been sitting comfortably for 5 min, using an oscillometric device (Omron 705 CP). Three readings were taken and the lowest one recorded. Body composition was assessed using an electrical impedance device (Tanita Body Composition Analyzer). An exercise stress test with electrocardiogram and oxygen uptake was performed. Subjects with any abnormal stress response were excluded, as were those with clinically significant abnormalities on routine lab testing.
Aerobic capacity (Vo2peak).
Maximal oxygen consumption was measured by treadmill, as previously described (3).
Muscle biopsy.
Muscle biopsies were taken either after an overnight fast or immediately after the most recent session of exercise, as described below.
Biopsies were obtained under local anesthesia from the vastus lateralis muscle. The muscle samples were immediately frozen in liquid nitrogen and stored for protein extraction for samples from pre- and 12 weeks post-exercise program (chronic exercise study) and subsequently for both RNA and protein extraction (acute exercise study: for samples pre- and 1-h and 7 days post-exercise).
Hyperinsulinemic-euglycemic clamp.
A clamp study (with insulin infusion 40 mU · m−2 · min−1) was performed at baseline and after exercise training in the chronic exercise study (3). Subjects taking insulin omitted the basal dose on the night before the clamp as well as the dose on the morning of the clamp study. The glucose disposal rate (between 80 and 120 min after commencement of the insulin infusion) was calculated after correction for residual hepatic glucose production using the [6,6-2H2] glucose tracer.
Exercise training
For more information on exercise training, see supplementary Figs. 1 and 2 in the online appendix at http://care.diabetesjournals.org/cgi/content/full/dc09-1305/DC1. The subjects maintained a stable diet and treatment for diabetes during both exercise programs. Subjects exercised either on a treadmill or a stationary bicycle ergometer. Each session lasted for a total of 70 min (5-min warm-up, 60-min exercise, 5-min cool down) and was fully supervised by an exercise physiologist or physician. Each exercise session was conducted at the same intensity, i.e., at 70% of the subject's Vo2max. This intensity of exercise has previously been shown by us and others to improve insulin sensitivity in obese middle-aged subjects with type 2 diabetes. Blood glucose was checked before exercise, and heart rate and blood pressure were monitored throughout exercise. Compliance with the exercise regimens was greater than 90%.
Chronic exercise.
After completion of all baseline measurements and a baseline muscle biopsy, subjects exercised for 4 1-h sessions each week. Each exercise session was conducted at 70% of the subject's Vo2max. The study continued for a total of 12 weeks. Baseline measurements were repeated and a final muscle biopsy was taken immediately after the last exercise session at the end of the study (3) (supplementary Fig. 1).
Acute exercise.
After completion of all baseline measurements and a baseline muscle biopsy, subjects exercised for a single 1-h session at 70% of Vo2max. A second muscle biopsy was taken immediately after the first session of exercise. The subjects then exercised for 1 h daily for 7 days, followed by a final muscle biopsy immediately after the final exercise session at the end of this study (supplementary Fig. 2).
RNA extraction and real-time quantitative PCR (acute exercise study).
For more information on the RNA extraction and real-time quantitative PCR, see the online appendix.
Homogenate extracts from muscle biopsies and Western blot assays (acute and chronic exercise studies).
Protein homogenate was extracted from ∼25 mg skeletal muscle. The muscle was immersed in ice-cold medium buffer A (0.1 mM KCL, 5 mm MgCl2, 5 mm EGTA, 5 mm sodium pyrophosphate, pH adjusted to 7.4, 2 μm leupeptin, 2 μm pepstatin, 0.5 mm phenylmethylsulphonylfluoride for 2 × 10 min). After this, the muscle was finely minced in 1/10 (wt/vol) buffer B (0.25 mM sacharose, 50 mm KCl, 5 mm EDTA, 1 mm sodium pyrophosphate, 5 mm MgCl2, pH adjusted to 6.8, 2 μm leupeptin, 2 μm pepstatin, 0.5 mm phenylmethylsulphonylfluoride) and then disrupted with a motor-driven Teflon/glass homogenizer. The entire procedure was performed at 0–4°C. The protein concentration was determined using a Micro BCA protein assay (Pierce, Rockford, IL). Western blot assays were performed as reported (15) (see online appendix).
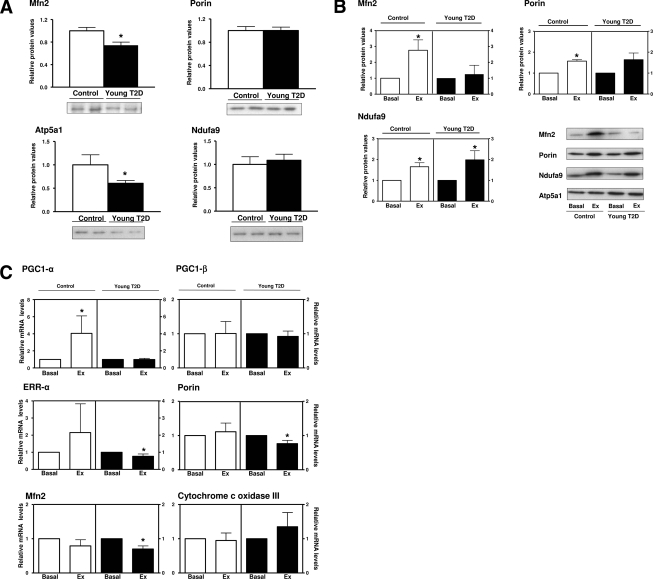
Statistical analysis
Unpaired t tests were performed to compare muscle protein expression between control subjects and subjects with diabetes at baseline (Fig. 1A). Paired t tests were performed to compare the effects of chronic exercise (Fig. 1B) and acute exercise (Fig. 1C) on the expression of a range of proteins and RNAs. In all cases, significance level for the t tests was set at P < 0.05.
Figure 1.
A: Baseline: Young type 2 diabetic subjects show an impaired expression of mitochondrial proteins in skeletal muscle. Western blot assays were performed in extracts obtained from skeletal muscle biopsies from 11 normal glucose tolerant (control) and 16 young type 2 diabetic patients (young T2D). Data are means ± SE. *Statistically significant difference compared with the control group at P < 0.05. Representative autoradiograms are also shown. B: Chronic exercise. Chronic exercise causes a deficient induction of muscle mitochondrial proteins in young type 2 diabetic subjects. Western blot assays were performed in extracts obtained from skeletal muscle biopsies from normal glucose tolerant and young type 2 diabetic patients before and after a protocol of chronic exercise. Representative autoradiograms are shown in the lower right corner. Data are means ± SE. *Statistical significant difference compared with basal values at P < 0.05. C: Acute exercise. Acute exercise induces skeletal muscle PGC-1α gene expression in control but not in young type 2 diabetic subjects. Real-time PCR was performed in skeletal muscle biopsies from nine normal glucose tolerant and six young type 2 diabetic patients before and after an acute session of exercise. Data are means ± SE. *Statistical significant difference compared with basal values at P < 0.05.
RESULTS
Clinical and metabolic measurements
Chronic exercise study.
Baseline characteristics (Table 1) of the chronic exercise participants have been described previously (3). The nondiabetic control subjects were matched for BMI with the diabetic group, but the diabetic subjects were slightly older. The 3-month exercise training program led to no significant change in whole-body or hepatic insulin sensitivity in either the control subjects or the subjects with diabetes (3). Vo2max increased by 20% in the control group (from 28.61 ± 1.94 to 35.15 ± 2.95 ml · kg−1 · min−1, P < 0.01), but was unchanged in the group with diabetes (22.67 ± 1.57 vs. 24.40 ± 1.50 ml · kg−1 · min−1, P = NS) after exercise. Fasting plasma free fatty acid concentrations tended to be lower at baseline, although not reaching significance, in the control group (0.635 vs. 0.820 mmol/l, P = NS) and were significantly lower (0.561 vs. 0.826 mmol/l, P = 0.003) in the control subjects after the 3-month exercise intervention (3). No correlation was found between either age or sex and Vo2max (data not shown).
Acute exercise study.
The acute exercise participants (Table 2) had a similar phenotype to individuals we have reported from previous studies (2,3). The control subjects were matched for age and BMI and had similar Vo2max at baseline to individuals with diabetes (22.85 ± 2.71 vs. 23.79 ± 1.79 ml · kg−1 · min−1, respectively; P = NS).
Neither Vo2max nor insulin sensitivity were re-measured at the end of this protocol, since neither of these parameters were expected to change after only 1 week of exercise training.
Expression of skeletal muscle mitochondrial proteins at baseline (combined baseline data from the chronic and acute studies)
Muscle biopsies were collected from young type 2 diabetes or control subjects, homogenates were obtained and the expression of mitochondrial proteins was studied. The yield of total proteins was similar in homogenates from control and young type 2 diabetic subjects (54.1 ± 2.6 and 54.8 ± 3.1 mg protein/g of tissue in control and young type 2 diabetic groups, respectively). The young type 2 diabetic group showed a reduced expression of the mitochondrial fusion protein, Mfn2 (26% reduction in those with diabetes) and the alpha subunit of ATP synthase (ATP5a1) (39% reduction in those with diabetes) (Fig. 1A). Under these conditions, the abundance of porin (a marker of mitochondrial mass) and of the p37 subunit of Complex I of the respiratory chain (Ndufa9) was unaltered indicating that the changes of Mfn2 and ATP synthase were not secondary to changes in mitochondrial mass (Fig. 1A).
Expression of skeletal muscle mitochondrial proteins after 3 months exercise: chronic exercise study
iChronic exercise was associated with the induction of Mfn2 (2.8-fold increase), porin (1.6-fold increase), and p37 subunit of Complex I (Ndufa9) (1.7-fold ncrease) in skeletal muscle from control subjects (Fig. 1B). In the young type 2 diabetic group, chronic exercise caused a different pattern of muscle changes. The expression of Mfn2 was unchanged, while there was induction in both Ndufa9 (2.0-fold increase) and porin (1.6-fold increase but not reaching statistical significance) (Fig. 1B).
Mitochondrial gene expression in skeletal muscle in response to acute exercise: acute exercise study
Muscle samples taken after 7 days of exercise showed no significant changes in gene expression (data not shown). However, acute exercise after 1 h caused a substantial induction in PGC-1α gene expression in skeletal muscle from control subjects (fourfold induction) (Fig. 1C). These changes in PGC-1α had reverted to baseline after 7 days of exercise (data not shown). Control subjects also showed an increased ERRα gene expression (2.2-fold increase), although this did not reach statistical significance and no changes in the gene expression of PGC-1β, porin, Mfn2, or the mitochondrial gene COXIII (Fig. 1C). In contrast, acute exercise led to no change in PGC-1α gene expression in skeletal muscle in the young type 2 group, and the expression of ERRα (23% reduction), Mfn2 (30% reduction), or porin (23% reduction) was significantly reduced (Fig. 1C). No changes in PGC-1β or COXIII gene expression were detected in young type 2 diabetic subjects (Fig. 1C). We analyzed whether AMPK was stimulated under these conditions; however, we detected no phosphorylation of AMPK in either the control or type 2 diabetic subjects (data not shown). No correlation was found between Vo2max and the expression of mitochondrial genes or proteins (data not shown).
CONCLUSIONS
We have previously reported that young subjects with type 2 diabetes are severely insulin resistant, achieving a maximal glucose disposal rate of only 2.15 ± 0.42 mg · kg−1 · min−1, compared with 4.09 ± 0.58 mg · kg−1 · min−1 in very obese control subjects (3). We undertook the current studies to directly analyze a range of parameters of muscle mitochondrial function in these subjects at baseline and after different durations of exercise training. The mitochondrial parameters reveal interesting new abnormalities in the subjects with diabetes both at baseline and after exercise. At baseline, subjects with diabetes display modestly (∼25%) reduced expression of Mfn2 and some OXPHOS subunits. Thus, in the baseline state, without any intervention, subjects with diabetes showed a defective pattern of mitochondrial protein expression in muscle compared with equally obese young people without diabetes. The patients with type 2 diabetes, in comparison with matched obese control subjects, were markedly dyslipidemic. Lipotoxicity in the patients with diabetes at baseline could either cause or result from the mitochondrial abnormalities that we have demonstrated in the current study.
After exercise, the mitochondrial changes we have observed are much more pronounced and are consistent with the whole-body findings in these subjects. Thus, in the obese nondiabetic subjects, acute exercise intervention was associated with increased muscle expression of genes encoding for PGC-1α and ERRα under conditions in which Mfn2 or porin was unchanged. These data are consistent with prior observations indicating that AMPK activity is stimulated by acute exercise in skeletal muscle in humans (18) and that PGC-1α gene expression and promoter activity are stimulated by AMPK (19). Moreover, and based on the observations that Mfn2 gene transcription is induced by ERRα, and coactivated by PGC-1α (14), we propose that enhanced PGC-1α activity will promote an increase in Mfn2 gene transcription. In contrast with this profile, acute exercise caused a reduction in the expression of genes encoding Mfn2 and porin in muscle from the subjects with diabetes under conditions in which PGC-1α remained unchanged. These data can be explained by the incapacity of acute exercise to stimulate AMPK activity in patients with diabetes, which cancels the induction of PGC-1α gene expression. We also propose that the reduced expression of the Mfn2 gene (and perhaps the porin gene, which also encodes for a mitochondrial protein) may be due to reduced transcriptional activities of either PGC-1α or PGC-1β, key regulators of Mfn2 transcription (14,20). In the obese nondiabetic subjects, chronic exercise training led to an increase in both Mfn2 (2.8-fold) and porin (1.6-fold), consistent with the increase in Vo2max observed after 3 months. In subjects with diabetes, however, we found no increase in Mfn2, consistent with the lack of stimulation of whole-body oxygen uptake. In spite of the lack of induction of PGC-1α or Mfn2, chronic exercise induced porin or Ndufa9 expression in the type 2 diabetic subjects. The induction of porin or Ndufa9 in the absence of PGC-1α suggests the existence of mechanisms of mitochondrial biogenesis, alternative to PGC-1α gene induction, that are triggered by physical exercise.
Several studies have analyzed the effect of dietary and/or exercise interventions aimed to promote weight loss in obese or type 2 diabetic subjects. These studies have detected that weight loss induced by diet/exercise stimulate mitochondrial activity in skeletal muscle both in obese subjects as well as in type 2 diabetic patients (17,21,22). In a recent study, a delayed and reduced response in PGC-1α expression was detected in muscle from obese subjects in response to exercise (22). Under these conditions, the expression of genes downstream of PGC-1α such as NRF-1 or cytochrome c oxidase subunit VIc also showed a reduced response in obese subjects after exercise (22).
Interestingly, we have also noted a markedly different response to bariatric surgery in morbidly obese diabetic subjects compared with a matched nondiabetic cohort (23). Despite similar weight loss (∼60 kg) and a marked improvement in insulin sensitivity in both groups, the patients with diabetes showed a blunted response in terms of glucose oxidation and no significant changes in the expression of Mfn2, porin, and citrate synthase (23). In all, these data together with data from our current study suggest a link between insulin resistance and a defective regulation of PGC-1α and downstream mitochondrial proteins in response to exercise, so that under conditions of severe insulin resistance, the induction of PGC-1α in response to exercise is abolished. Further studies should investigate whether the defective PGC-1α expression is a primary defect or whether it is secondary to insulin resistance or reversible lipotoxicity.
There are further possible explanations to link environmental effects such as diet and physical activity with abnormalities of mitochondrial oxidative proteins in patients with type 2 diabetes. In a recent muscle biopsy study in human subjects including control subjects, subjects with impaired glucose tolerance, and subjects with type 2 diabetes, it was shown that type 2 diabetes is associated with hypermethylation of PGC-1α, concomitant with reduced mitochondrial content (24). Epigenetic effects may also modulate the effect of diet and activity on the pathogenesis of diabetes and could explain at least some of the abnormalities observed in the current study.
We acknowledge some limitations in the current studies. The overall number of subjects included is small, and it was not possible with these numbers to match groups for sex. Early-onset type 2 diabetes remains uncommon, and it is challenging to recruit young subjects of working age for these relatively complex protocols. In the initial (chronic exercise) study, the skeletal muscle investigations were limited by the biopsy amount, and it was not possible to measure PGC-1α or other gene expression.
In summary, our results indicate that early-onset type 2 diabetes is associated, at baseline, with reduced expression of skeletal muscle Mfn2, which is associated with concomitant reduction in activity of certain oxidative phosphorylation subunits. In addition, subjects with early-onset type 2 diabetes are characterized by a deficient capacity to induce PGC-1α or Mfn2 in response to aerobic exercise training. These alterations in Mfn2 expression and the failure to stimulate PGC-1α may be relevant to the observed incapacity in these patients to enhance whole-body Vo2max in response to exercise training. Further mechanistic studies of these pathways in this patient group are clearly indicated. A more complete understanding of these mechanisms will be crucial to the design of lifestyle interventions to prevent and treat type 2 diabetes in adolescents and young adults.
Supplementary Material
Acknowledgments
This study was funded in part by grant support from the European Foundation for the Study of Diabetes/Novo Nordisk (to J.J.N.) and by a grant from the EU Commission (LHSM-CT-2003-503041) (to J.J.N.). This study was also supported by research grants from the “Ministerio de Educación y Cultura” (SAF 2005-00445 and SAF 2008-03803) and grant 2005SGR00947 from the “Generalitat de Catalunya.” CIBER de Diabetes y Enfermedades Metabólicas Asociadas is an Instituto de Salud Carlos III project. M.H. is the recipient of a predoctoral fellowship from Consejo Nacional de Ciencia y Tecnologia, Mexico. M.L. was the recipient of a predoctoral fellowship from the Ministerio de Educación y Cultura, Spain. A.Z. was the recipient of a Science Intensification Award from the University of Barcelona.
No other potential conflicts of interest relevant to this article were reported.
The authors wish to thank the study patients and volunteers and their families, as well as the staff of the Metabolic Research Unit.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Fagot-Campagna A, Pettitt DJ, Engelgau MM, Burrows NR, Geiss LS, Valdez R, Beckles GL, Saaddine J, Gregg EW, Williamson DF, Narayan KM: Type 2 diabetes among North American children and adolescents: an epidemiologic review and a public health perspective. J Pediatr 2000;136:664–672 [DOI] [PubMed] [Google Scholar]
- 2. McQuaid S, O'Gorman DJ, Yousif O, Yeow TP, Rahman Y, Gasparro D, Pacini G, Nolan JJ: Early-onset insulin-resistant diabetes in obese Caucasians has features of typical type 2 diabetes, but 3 decades earlier. Diabetes Care 2005;28:1216–1218 [DOI] [PubMed] [Google Scholar]
- 3. Burns N, Finucane FM, Hatunic M, Gilman M, Murphy M, Gasparro D, Mari A, Gastaldelli A, Nolan JJ: Early-onset type 2 diabetes in obese white subjects is characterised by a marked defect in beta cell insulin secretion, severe insulin resistance and a lack of response to aerobic exercise training. Diabetologia 2007;50:1500–1508 [DOI] [PubMed] [Google Scholar]
- 4. Kelley DE, He J, Menshikova EV, Ritov VB: Dysfunction of mitochondria in human skeletal muscle in type 2 diabetes. Diabetes 2002;51:2944–2950 [DOI] [PubMed] [Google Scholar]
- 5. Petersen KF, Dufour S, Befroy D, Garcia R, Shulman GI: Impaired mitochondrial activity in the insulin-resistant offspring of patients with type 2 diabetes. N Engl J Med 2004;350:664–671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Toledo FG, Watkins S, Kelley DE: Changes induced by physical activity and weight loss in the morphology of intermyofibrillar mitochondria in obese men and women. J Clin Endocrinol Metab 2006;91:3224–3227 [DOI] [PubMed] [Google Scholar]
- 7. Bach D, Naon D, Pich S, Soriano FX, Vega N, Rieusset J, Laville M, Guillet C, Boirie Y, Wallberg-Henriksson H, Manco M, Calvani M, Castagneto M, Palacín M, Mingrone G, Zierath JR, Vidal H, Zorzano A: Expression of Mfn2, the Charcot-Marie-Tooth neuropathy type 2A gene, in human skeletal muscle: effects of type 2 diabetes, obesity, weight loss, and the regulatory role of tumor necrosis factor alpha and interleukin-6. Diabetes 2005;54:2685–2693 [DOI] [PubMed] [Google Scholar]
- 8. Mootha VK, Lindgren CM, Eriksson KF, Subramanian A, Sihag S, Lehar J, Puigserver P, Carlsson E, Ridderstråle M, Laurila E, Houstis N, Daly MJ, Patterson N, Mesirov JP, Golub TR, Tamayo P, Spiegelman B, Lander ES, Hirschhorn JN, Altshuler D, Groop LC: PGC-1alpha-responsive genes involved in oxidative phosphorylation are coordinately downregulated in human diabetes. Nat Genet 2003;34:267–273 [DOI] [PubMed] [Google Scholar]
- 9. Patti ME, Butte AJ, Crunkhorn S, Cusi K, Berria R, Kashyap S, Miyazaki Y, Kohane I, Costello M, Saccone R, Landaker EJ, Goldfine AB, Mun E, DeFronzo R, Finlayson J, Kahn CR, Mandarino LJ: Coordinated reduction of genes of oxidative metabolism in humans with insulin resistance and diabetes: potential role of PGC1 and NRF1. Proc Natl Acad Sci U S A 2003;100:8466–8471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gollnick PD, Armstrong RB, Saubert CW, 4th, Piehl K, Saltin B: Enzyme activity and fiber composition in skeletal muscle of untrained and trained men. J Appl Physiol 1972;33:312–319 [DOI] [PubMed] [Google Scholar]
- 11. Baar K, Wende AR, Jones TE, Marison M, Nolte LA, Chen M, Kelly DP, Holloszy JO: Adaptations of skeletal muscle to exercise: rapid increase in the transcriptional coactivator PGC-1. FASEB J 2002;16:1879–1886 [DOI] [PubMed] [Google Scholar]
- 12. Mootha VK, Handschin C, Arlow D, Xie X, St Pierre J, Sihag S, Yang W, Altshuler D, Puigserver P, Patterson N, Willy PJ, Schulman IG, Heyman RA, Lander ES, Spiegelman BM: Erralpha and Gabpa/b specify PGC-1alpha-dependent oxidative phosphorylation gene expression that is altered in diabetic muscle. Proc Natl Acad Sci U S A 2004;101:6570–6575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wu Z, Puigserver P, Andersson U, Zhang C, Adelmant G, Mootha V, Troy A, Cinti S, Lowell B, Scarpulla RC, Spiegelman BM: Mechanisms controlling mitochondrial biogenesis and respiration through the thermogenic coactivator PGC-1. Cell 1999;98:115–124 [DOI] [PubMed] [Google Scholar]
- 14. Soriano FX, Liesa M, Bach D, Chan DC, Palacín M, Zorzano A: Evidence for a mitochondrial regulatory pathway defined by peroxisome proliferator-activated receptor-gamma coactivator-1 alpha, estrogen-related receptor-alpha, and mitofusin 2. Diabetes 2006;55:1783–1791 [DOI] [PubMed] [Google Scholar]
- 15. Pich S, Bach D, Briones P, Liesa M, Camps M, Testar X, Palacín M, Zorzano A: The Charcot-Marie-Tooth type 2A gene product, Mfn2, up-regulates fuel oxidation through expression of OXPHOS system. Hum Mol Genet 2005;14:1405–1415 [DOI] [PubMed] [Google Scholar]
- 16. Menshikova EV, Ritov VB, Fairfull L, Ferrell RE, Kelley DE, Goodpaster BH: Effects of exercise on mitochondrial content and function in aging human skeletal muscle. J Gerontol A Biol Sci Med Sci 2006;61:534–540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Toledo FG, Menshikova EV, Ritov VB, Azuma K, Radikova Z, DeLany J, Kelley DE: Effects of physical activity and weight loss on skeletal muscle mitochondria and relationship with glucose control in type 2 diabetes. Diabetes 2007;56:2142–2147 [DOI] [PubMed] [Google Scholar]
- 18. Musi N, Fujii N, Hirshman MF, Ekberg I, Fröberg S, Ljungqvist O, Thorell A, Goodyear LJ: AMP-activated protein kinase (AMPK) is activated in muscle of subjects with type 2 diabetes during exercise. Diabetes 2001;50:921–927 [DOI] [PubMed] [Google Scholar]
- 19. Irrcher I, Ljubicic V, Kirwan AF, Hood DA: AMP-activated protein kinase-regulated activation of the PGC-1alpha promoter in skeletal muscle cells. PLoS One 2008;3:e3614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Liesa M, Borda-d'Agua B, Medina-Gómez G, Lelliott CJ, Paz JC, Rojo M, Palacín M, Vidal-Puig A, Zorzano A: Mitochondrial fusion is increased by the nuclear coactivator PGC-1beta. PLoS One 2008;3:e3613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Menshikova EV, Ritov VB, Ferrell RE, Azuma K, Goodpaster BH, Kelley DE: Characteristics of skeletal muscle mitochondrial biogenesis induced by moderate-intensity exercise and weight loss in obesity. J Appl Physiol 2007;103:21–27 [DOI] [PubMed] [Google Scholar]
- 22. De Filippis E, Alvarez G, Berria R, Cusi K, Everman S, Meyer C, Mandarino LJ: Insulin-resistant muscle is exercise resistant: evidence for reduced response of nuclear-encoded mitochondrial genes to exercise. Am J Physiol Endocrinol Metab 2008;294:E607–E614 [DOI] [PubMed] [Google Scholar]
- 23. Hernández-Alvarez MI, Chiellini C, Manco M, Naon D, Liesa M, Palacín M, Mingrone G, Zorzano A: Genes involved in mitochondrial biogenesis/function are induced in response to bilio-pancreatic diversion in morbidly obese subjects with normal glucose tolerance but not in type 2 diabetics. Diabetologia 2009;52:1618–1627 [DOI] [PubMed] [Google Scholar]
- 24. Barres R, Osler M, Yan J, Rune A, Fritz T, Caidahl K, Krook A, Zierath J: Non-CpG methylation of the PGC-1α promoter through DNMT3B controls mitochondrial density. Cell Metab 2009;1:189–198 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.