Abstract
Background and objectives: Venous blood gas (VBG) analysis is a safer procedure than arterial blood gas (ABG) analysis and may be an alternative for determining acid-base status. The objective of this study was to examine the agreement between ABG and central VBG samples for all commonly used parameters in a medical intensive care unit (ICU) population.
Design, setting, participants, & measurements: We performed a single-center, prospective trial to assess the agreement between arterial and central VBG measurements in a medical ICU. Adult patients who were admitted to the ICU and required both a central venous line and an arterial line were enrolled. When an ABG was performed, a central venous sample was obtained to examine the agreement among the pH, Pco2, and bicarbonate. Data comparing central and peripheral VBG values were also obtained.
Results: The mean arterial minus venous difference for pH, Pco2, and bicarbonate was 0.027, −3.8, and −0.80, respectively. Bland-Altman plots for agreement of pH, Pco2, and bicarbonate showed 95% limits of agreement of −0.028 to 0.081, −12.3 to 4.8, and −4.0 to 2.4, respectively. Regression equations were derived to predict arterial values from venous values as follows: Arterial pH = −0.307 + 1.05 × venous pH, arterial Pco2 = 0.805 + 0.936 × venous Pco2, and arterial bicarbonate = 0.513 + 0.945 × venous bicarbonate. The mean central minus peripheral differences for pH, Pco2, and bicarbonate were not clinically important.
Conclusions: Peripheral or central venous pH, Pco2, and bicarbonate can replace their arterial equivalents in many clinical contexts encountered in the ICU.
Arterial blood gas (ABG) analysis is a commonly performed procedure that is often used to determine the acid-base and respiratory status of critical patients; however, this test can result in patient discomfort as well as complications such as arterial injury, thrombosis or embolization, hematoma, aneurysm formation, and reflex sympathetic dystrophy (1–3). In addition, the procedure has a small but appreciable risk for needlestick injury to health care workers. Venous blood gas (VBG) analysis requires fewer punctures, is a relatively safer procedure for both the patient and the health care provider, and may be an alternative to ABG analysis for acid-base status. Although a few studies have expressed reservations regarding the accuracy of VBG values (4–6), there is emerging evidence to suggest that there is agreement between ABG and VBG values (7–15). To our knowledge, no previous study has examined the agreement among all of the commonly used parameters in arterial and central VBG samples in a diverse population of medical intensive care unit (ICU) patients. Also, no previous study has specifically obtained multiple paired ABG and VBG samples from each patient throughout their ICU course to evaluate whether the agreement between ABG and VBG values is acceptable throughout the dynamic acid-base and respiratory conditions encountered in the ICU. The main objective of this study was to examine the agreement between ABG and central VBG samples for all commonly used parameters (pH, Pco2, and bicarbonate) in a pathologically diverse ICU patient population, specifically analyzing multiple paired arterial and venous samples from each patient. In addition, a secondary objective was to compare central and peripheral VBG values with respect to pH, Pco2, and bicarbonate.
Materials and Methods
We performed a single-center, prospective trial to assess the agreement between arterial and central VBG measurements. This study was conducted in the medical ICU at Olive View-UCLA Medical Center, a 377-bed county hospital that serves primarily low-income and indigent patients. All adult patients who were admitted to the ICU and had been determined by their treating clinicians to require both a central venous line and an arterial line were enrolled in the study. Given that only minimal blood was required to perform this study, a waiver of consent was granted from our review board. When an ABG was deemed to be necessary as part of ICU management, a central venous sample was also obtained within 2 minutes. All of the samples were analyzed using the same Bayer Rapid Point 405 blood gas analyzer as quickly as possible. A maximum of 10 paired ABG-VBG samples were obtained per patient to prevent a single patient from dominating the data set. Additional data collected on a standardized data collection form included primary diagnosis, intubation status, use of inotropic agents, and hypotension (defined as a systolic BP <90 mmHg). Data comparing central and peripheral VBG values were also obtained. Paired central and peripheral venous samples were drawn within 2 minutes of one another in ICU patients with both central venous lines and peripheral intravenous lines already in place.
Statistical Analysis
The Bland-Altman method was used to assess agreement between arterial (A) and central venous (V) measurements of pH, Pco2, and bicarbonate. The A-V difference versus the average value ([A+V]/2) was plotted. Means, SDs, and 95% prediction intervals (limits of agreement) of the A-V differences are reported as well as the Pearson correlation between A-V and (A+V)/2. If there is no trend in the A-V differences, then this correlation should be 0. In addition, Pearson correlations between the arterial and central venous values are reported and linear regression was used to establish equations for estimation of arterial values from central venous values. Because there were multiple A and V measurements for a single patient, components of variance computations were carried out to determine whether there was between-patient SD heterogeneity, and a random slope and intercept model was used to determine whether there was between-patient heterogeneity in the regression analyses. A sample size of 40 patients was based on estimating the central venous minus arterial differences (lack of agreement) and their SD (SDe) to within ±23% with 95% confidence for Pco2, bicarbonate, or pH differences.
Results
The study involved 40 patients with a total of 221 paired ABG-VBG samples. Thirty-one paired samples were excluded (13 samples because of clerical errors, 16 samples because of being run on different blood gas analyzers, and two samples because the arterial and venous samples were drawn >2 minutes apart); therefore, 190 paired samples were included in the analysis. Table 1 shows the patient characteristics. The patient population consisted of roughly equal numbers of men and women, with a mean ± SD age of 57 ± 16 years. The most common presenting diagnosis was sepsis (72.5%), although a number of other conditions that frequently are encountered in the ICU were present. The vast majority of enrolled patients were intubated, hypotensive, and on inotropic agents. None of the patients in the study were receiving bicarbonate.
Table 1.
Patient characteristics
| Characteristic | Value |
|---|---|
| Age (years; mean ± SD) | 57 ± 16 |
| Gender (male/female; n [%]) | 22 (55)/18 (45) |
| Intubated (n/N [%]) | 36/40 (90) |
| Hypotensive (n/N [%]) | 36/40 (90) |
| Inotropic agent use (n/N [%]) | 35/40 (87.5) |
| Primary diagnosis (%) | |
| sepsis | 72.5 |
| interstitial lung disease | 2.5 |
| altered mental status | 2.5 |
| upper gastrointestinal bleed | 2.5 |
| renal failure | 2.5 |
| congestive heart failure | 2.5 |
| pulmonary tuberculosis | 2.5 |
| pneumocystis pneumonia | 2.5 |
| pancreatitis | 2.5 |
| diabetic ketoacidosis | 2.5 |
| cor pulmonale | 2.5 |
| respiratory failure of unclear cause | 2.5 |
Arterial versus central venous intercept and slope homogeneity tests for pH, Pco2, and bicarbonate had P values of 0.995, 0.122, and 0.497, respectively (data not shown). Thus, all 190 observations could be combined (see the Discussion section).
The arterial pH values ranged from 6.73 to 7.63, the arterial Pco2 values ranged from 16 to 79 mmHg, and arterial bicarbonate values ranged from 2 to 45 mEq/L. Table 2 shows the mean values and SDs for arterial and central venous pH, Pco2, and bicarbonate, as well as for the arterial minus central venous difference of these parameters.
Table 2.
Arterial and central venous blood gas values (n = 190)
| Parameter | ABG (Mean ± SD) | VBG (Mean ± SD) | A-V Difference (Mean ± SD)a |
|---|---|---|---|
| pH | 7.370 ± 0.138 | 7.340 ± 0.134 | 0.027 ± 0.027 |
| Pco2 (mmHg) | 38.4 ± 12.4 | 42.3 ± 12.6 | −3.8 ± 4.3 |
| Bicarbonate (mEq/L) | 22.40 ± 7.60 | 23.20 ± 7.80 | −0.80 ± 1.58 |
Total between- + within-person SD. There was no significant between person heterogeneity in the A-V SD.
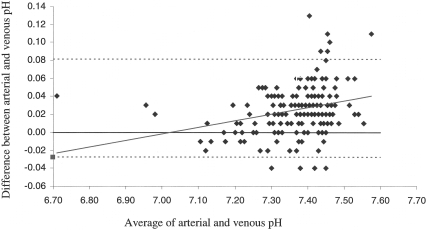
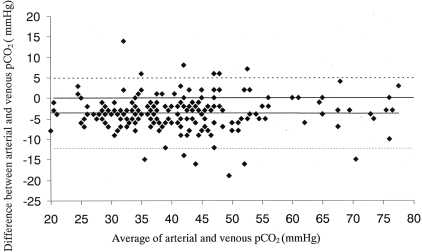
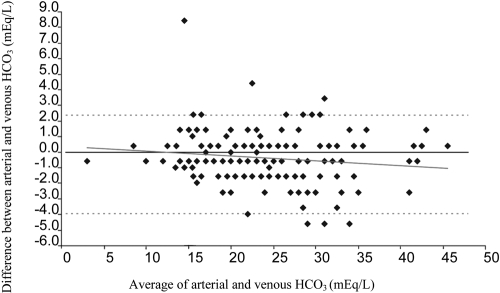
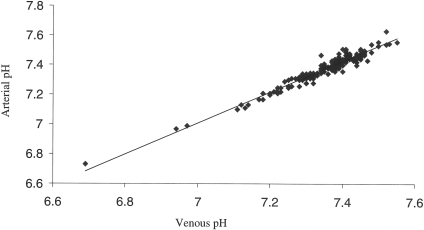
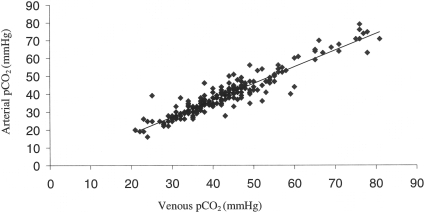
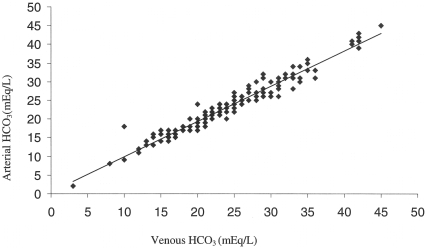
Figures 1, 2, and 3 show the Bland-Altman plots for pH, Pco2, and bicarbonate with their 95% limits of agreement (95% prediction intervals), respectively. Figures 4, 5, and 6 show the correlation between central venous and arterial blood gas values for pH, Pco2, and bicarbonate, respectively. Regression equations were derived to predict arterial values from central venous values as follows:
Arterial pH = −0.307 + 1.05 × venous pH (R2 = 0.945)
Arterial Pco2 = 0.805 + 0.936 × venous Pco2 (R2 = 0.883)
Arterial bicarbonate = 0.513 + 0.945 × venous bicarbonate (R2 = 0.950)
Figure 1.
Bland-Altman plot of arterial and central venous blood pH showing the regression line (solid line) and the 95% limits of agreement of −0.028 to 0.081 (dotted lines) for the A-V difference. r = 0.296, R2 = 0.088.
Figure 2.
Bland-Altman plot of arterial and central venous blood Pco2 showing the regression line (solid line) and the 95% limits of agreement of −12.3 to 4.8 mmHg (dotted lines) for the A-V difference. r = −0.01, R2 = 0.0001.
Figure 3.
Bland-Altman plot of arterial and central venous blood HCO3 showing the regression line (solid line) and the 95% limits of agreement of −4.0 to 2.4 mEq/L (dotted lines) for the A-V difference. r = −0.136, R2 = 0.018.
Figure 4.
Correlation between central venous and arterial blood gas values for pH. R2 = 0.95.
Figure 5.
Correlation between central venous and arterial blood gas values for Pco2. R2 = 0.88.
Figure 6.
Correlation between central venous and arterial blood gas values for HCO3. R2 = 0.95.
Multivariate regression was used to establish whether using all three of the central venous variables (pH, Pco2, and bicarbonate) in a single equation can be used to predict better the arterial values for pH, Pco2, and bicarbonate. The multivariate regression equations are as follows:
Arterial pH = 0.545 + 0.0288 × venous pH − 0.00139 × venous Pco2 + 0.00269 × venous HCO3 (R2 = 0.948)
Arterial Pco2 = −120.1 + 16.498 × venous pH + 1.193 × venous Pco2 −0.553 × venous HCO3 (R2 = 0.895)
Arterial HCO3 = −23.666 + 3.268 × venous pH + 0.053 × venous Pco2 + 0.855 × venous HCO3 (R2 = 0.951)
A total of 14 paired samples comparing central and peripheral VBG values were drawn from 14 patients (one paired sample per patient). For pH, the mean central venous value was 7.34 and the mean peripheral venous value was 7.34 with a mean central minus peripheral difference of −0.001 (−0.01%). For Pco2, the mean central venous value was 37.52 mmHg and the mean peripheral venous value was 36.80 mmHg with a mean central minus peripheral difference of 0.72 mmHg (1.94%). For bicarbonate, the mean central venous value was 21.18 mEq/L and the mean peripheral venous value was 20.87 mEq/L with a mean central minus peripheral difference of 0.31 mEq/L (1.46%).
Discussion
VBG analysis clearly does not replace ABG analysis in determining exact Po2 status, and arterial puncture may still be required for invasive arterial BP monitoring, but given the well-accepted accuracy of pulse oximetry, VBG analysis may be a safer alternative to ABG analysis for determining acid-base status, reducing the need for frequent invasive arterial sampling. A number of studies have suggested that there is agreement between ABG and VBG values, although most of the previous studies were limited by specific patient group samples (e.g., patients with diabetic ketoacidosis), analysis of only one or some parameters rather than all commonly used parameters (e.g., pH, Pco2, and bicarbonate), or examination of only one ABG and VBG sample per patient (7–15). A few authors even expressed doubts about the use of VBG values in lieu of arterial values (4–6). The aim of this study was to investigate the agreement between ABG and central VBG samples for all commonly used parameters (pH, Pco2, and bicarbonate) in a pathologically diverse ICU patient population.
Although the presenting diagnosis for patients in the study was predominantly sepsis, there was a range of other pathophysiology present. This patient population seems to be fairly representative of the disease processes encountered in many medical ICUs.
No previous study has assessed whether all patients share a common relationship between arterial and central venous pH, Pco2, and bicarbonate. Factors that are intrinsic to each individual patient, as well as their differing pathophysiologic states, could result in differential CO2 unloading at the tissue level; therefore, it cannot be assumed a priori that all patients have a common relationship between ABG and VBG values. Obtaining multiple paired arterial and central venous samples from each patient allowed us to perform homogeneity tests, which revealed that arterial versus venous intercept and slope for pH, Pco2, and bicarbonate had P values of 0.995, 0.122, and 0.497, respectively; therefore, there is a common relationship between arterial and central venous pH, Pco2, and bicarbonate for all patients, allowing all 190 observations to be pooled for the remainder of the analysis.
There is excellent agreement between arterial and central venous values for pH and bicarbonate, which is consistent with the results of other studies in the literature (4–11,13–15). In regard to pH, the mean arterial minus central venous difference was 0.027 (SD 0.027) with a 95% limits of agreement of −0.028 to 0.081 (Figure 1). Previous studies have shown a mean arterial minus venous difference for pH ranging from −0.04 to 0.05 (4–6,8–11,13–15). With respect to bicarbonate, the mean arterial minus central venous difference was −0.80 (SD 1.58) with a 95% limits of agreement of −4.0 to 2.4 (Figure 3). Previous studies have shown a mean arterial minus venous difference for bicarbonate ranging from −1.88 to −0.52 (5–7,10,11,13–15). There is acceptable agreement between arterial and central venous values for Pco2; the mean arterial minus central venous difference was −3.8 (SD 4.3) with a 95% limits of agreement of −12.3 to 4.8 (Figure 2). Previous literature showed a mean arterial minus venous difference for Pco2 ranging from −6.6 to −3.0 (4–6,14,15). Comparing the results of our study with other studies that also reported 95% limits of agreement, the arterial and central venous values for Pco2 in our study showed better agreement than the study by Kelly et al. (5), which demonstrated a mean arterial minus venous difference of −5.8 with a 95% limits of agreement of −8.8 to 20.5; however, there was less agreement in our study compared with studies by Malinoski et al. (4), which showed a mean arterial minus venous difference of −4.36 with a 95% limits of agreement of −2.20 to 10.90 and Malatesha et al. (15), which revealed a mean arterial minus venous difference of −3.0 with a 95% limits of agreement of −7.6 to 6.8. Overall, the results of our study in regard to Pco2 are consistent with the existing literature. Given that blood gas values should be interpreted in the context of the individual patient's clinical status and that frequently serial blood gases are obtained to help assess a patient's course, central venous Pco2 largely should be able to replace arterial Pco2 in most clinical circumstances.
Comparing the bivariate R2 values to the multivariate R2 values shows that the multivariate models do not account for significantly more variation than the corresponding simple linear regression equations. This demonstrates that there is no advantage in using the more complicated multivariate equations. For example, the R2 for arterial pH using only central venous pH is R2 = 0.945. Using central venous pH, central venous Pco2, and central venous bicarbonate simultaneously to predict arterial pH only increases this to R2 = 0.948. We obtained additional data comparing central and peripheral VBG values and found that the mean central minus peripheral differences for pH, Pco2, and bicarbonate were not clinically important; therefore, peripheral as well as central venous samples have acceptable agreement with ABG values.
To our knowledge, our study is the first study to examine the agreement among all of the commonly used parameters in arterial and central VBG samples in a diverse population of medical ICU patients; however, the study does have some limitations. The first 40 patients that met study inclusion criteria were enrolled. Although patient selection did not involve formal random sampling, this is unlikely to have resulted in systematic bias, because our demographics are similar to a typical study population in a medical ICU and the ranges of arterial and venous values span the clinically important range. Second, although the enrolled patients did seem to be fairly representative of the disease processes encountered in many ICUs, there was a prevalence of sepsis. As a result, other pathophysiologic states, such as pure hypovolemic shock and cardiogenic shock, were underrepresented. It is unlikely that any of these pathophysiologic states would have a different relationship between arterial and venous values in the absence of severe circulatory failure, which was shown by Adrogue et al. (16) in previous work to result in poorer agreement between arterial and venous values. Nonetheless, that the patient population in the study had a predominance of patients with sepsis does limit the generalizability of our results, especially in patients with very low cardiac output. Third, the study did use central venous samples obtained from a central line, not peripheral venous samples; however, given that our study found acceptable agreement between arterial and central venous values, it would be expected that similar agreement would be found if peripheral venous samples were used, which in fact has been confirmed by both our own results and those of other studies (7–10,12–15). Last, even though the study did include a wide range of acid-base status, including arterial pH values that ranged from 6.73 to 7.63, arterial Pco2 values that ranged from 16 to 79 mmHg, and arterial bicarbonate values that ranged from 2 to 45 mEq/L, there were fewer values at the extremes. For example, only three samples had a pH <7 and only 10 samples had a pH >7.5. On the basis of the middle 95% range of the Bland-Altman plots, the relationship between arterial and central venous values holds between the ranges of 7.12 to 7.52, 24.5 to 74.1 (mmHg), and 12 to 41 (mEq/L) for pH, Pco2, and bicarbonate, respectively. These ranges encompass most of the values commonly encountered in an ICU setting, although there clearly is less certainty about the relationship between arterial and venous values at the extremes of pH, Pco2, and bicarbonate beyond these ranges.
Conclusions
Peripheral or central venous pH, Pco2 and bicarbonate can replace their arterial equivalents in many clinical contexts that are encountered in the ICU. Further work needs to be done to define better the relationship between ABG and VBG values in low-cardiac-output states.
Disclosures
None.
Acknowledgments
This project was supported by a seed grant from the Olive-View-UCLA Education and Research Institute.
We acknowledge Dr. Jeffrey Gornbein's assistance with the statistical analysis, as well as Dr. Constance Chen and the entire ICU and respiratory therapy staff at Olive View-UCLA Medical Center.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This trial has been registered at www.clinicaltrials.gov (identifier NCT00569634).
References
- 1.Milzma D, Janchar T: Arterial puncture and cannulation. In: Clinical Procedures in Emergency Medicine, 4th Ed., edited by Roberts JR, Hedges JR.Philadelphia, WB Saunders, 2004, pp 384–400 [Google Scholar]
- 2.Mortensen J: Clinical sequelae from arterial needle puncture, cannulation, and incision. Circulation 35: 1118–1123, 1967 [DOI] [PubMed] [Google Scholar]
- 3.Criscuolo C, Nepper G, Buchalter S: Reflex sympathetic dystrophy following arterial blood gas sampling in the intensive care setting. Chest 108: 578–580, 1995 [DOI] [PubMed] [Google Scholar]
- 4.Malinoski DJ, Todd SR, Slone S, Mullins RJ, Schreiber MA: Correlation of central venous and arterial blood gas measurements in mechanically ventilated trauma patients. Arch Surg 140: 1122–1125, 2005 [DOI] [PubMed] [Google Scholar]
- 5.Kelly AM, Kyle E, McAlpine R: Venous pCO2 and pH can be used to screen for significant hypercarbia in emergency patients with acute respiratory disease. J Emerg Med 22: 15–19, 2002 [DOI] [PubMed] [Google Scholar]
- 6.Rang LC, Murray HE, Wells GA, Macgougan CK: Can peripheral blood gases replace arterial blood gases in emergency department patients? CJEM 4: 7–15, 2002 [DOI] [PubMed] [Google Scholar]
- 7.Kelly AM, McAlpine R, Kyle E: Agreement between bicarbonate measured on arterial and venous blood gases. Emerg Med Australas 16: 407–409, 2004 [DOI] [PubMed] [Google Scholar]
- 8.Kelly AM, McAlpine R, Kyle E: Venous pH can safely replace arterial pH in the initial evaluation of patients in the emergency department. Emerg Med J 18: 340–342, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ma OJ, Rush MD, Godfrey MM, Gaddis G: Arterial blood gas results rarely influence emergency physician management of patients with suspected diabetic ketoacidosis. Acad Emerg Med 10: 836–841, 2003 [DOI] [PubMed] [Google Scholar]
- 10.Gokel Y, Paydas S, Koseoglu Z, Alparslan N, Seydaoglu G: Comparison of blood gas and acid-base measurements in arterial and venous blood samples in patients with uremic acidosis and diabetic ketoacidosis in the emergency room. Am J Nephrol 20: 319–323, 2000 [DOI] [PubMed] [Google Scholar]
- 11.Middleton P, Kelly AM, Brown J, Robertson M: Agreement between arterial and central venous values for pH, bicarbonate, base excess, and lactate. Emerg Med J 23: 622–624, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chu YC, Chen CZ, Lee CH, Chen CW, Chang HY, Hsiue TR: Prediction of arterial blood gas values from venous blood gas values in patients with acute respiratory failure receiving mechanical ventilation. J Formos Med Assoc 102: 539–543, 2003 [PubMed] [Google Scholar]
- 13.Brandenburg MA, Dire DJ: Comparison of arterial and venous blood gas values in the initial emergency department evaluation of patients with diabetic ketoacidosis. Ann Emerg Med 31: 459–465, 1998 [DOI] [PubMed] [Google Scholar]
- 14.Ak A, Ogun CO, Bayir A, Kayis SA, Koylu R: Prediction of arterial blood gas values from venous blood gas values in patients with acute exacerbation of chronic obstructive pulmonary disease. Tohoku J Exp Med 210: 285–290, 2006 [DOI] [PubMed] [Google Scholar]
- 15.Malatesha G, Singh NK, Bharija A, Rehani B, Goel A: Comparison of arterial and venous pH, bicarbonate, pCO2 and pO2 in initial emergency department assessment. Emerg Med J 24: 569–571, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adrogue HJ, Rashad MN, Gorin AB, Yacoub J, Madias NE: Assessing acid-base status in circulatory failure: Differences between arterial and central venous blood. N Engl J Med 320: 1312–1316, 1989 [DOI] [PubMed] [Google Scholar]