Abstract
Background and objectives: There have been no recent analyses of the adequacy of training in U.S. nephrology training programs or the importance of specific aspects of fellowship training in the careers and practices of nephrologists who recently completed training.
Design, setting, participants, & measurements: An internet-based survey was sent to members of the American Society of Nephrology who completed nephrology training in 2004 to 2008. Respondents were asked to rate their fellowship training (little or no training, some training but not enough to feel competent, well trained and competent) in specific areas and the importance of each area to their current careers and practices.
Results: Among 133 recent adult nephrology trainees, most felt well trained and competent in many areas of patient care and core content. A significant percentage of respondents reported receiving little or no training, or some training but not enough to feel competent in other specific areas, such as genetic renal disease, care of adults with childhood kidney disease, pregnancy complications, poisoning, nutrition, end-of-life care, clinical pharmacology, home and self-care hemodialysis, peritoneal dialysis, plasmapheresis, interpretation and performance of renal ultrasound and other renal imaging, renal biopsy pathology interpretation, business and administrative aspects of nephrology, research, and research funding. Many of these areas were also identified as somewhat or very important to the careers and practices of respondents.
Conclusions: Nephrology training programs are perceived as doing an excellent job training fellows in many areas. Gaps in training should be addressed in fellowship training and post-training education.
There have been no recent systematic analyses of the quality and comprehensiveness of training received in United States nephrology training programs. The Accreditation Council for Graduate Medical Education (ACGME) requires that education and training in certain core content areas and procedural skills are included during fellowship and that each program assess its trainees' competence in these areas, but it does not itself directly assess competence. The core subject knowledge of nephrologists who have completed training is assessed by the American Board of Internal Medicine (ABIM) nephrology and American Board of Pediatrics subspecialty examinations. There are, however, no current assessments available of actual or perceived clinical competence of nephrologists who have recently completed their fellowship training. The most recent previous assessment of perceived training adequacy was published more than 15 years ago and addressed training that occurred more than two decades ago (1). A more recent survey-based analysis evaluated training and clinical experience during training in various procedures (2) and found great variability among programs in the scope and extent of procedural training and in expectations for clinical competency.
To assess the adequacy of training during fellowship in a wide variety of core knowledge, patient care, procedural, research, and business/administrative aspects of nephrology as perceived by nephrologists who recently completed their fellowship training, a web-based survey was developed and administered in conjunction with the American Society of Nephrology (ASN). The survey also queried respondents as to the importance of each area to their current practice or career situation.
Materials and Methods
An internet-based survey was sent to all active members of the ASN assessing multiple aspects of career choice, training, and post-training careers. This paper reports responses to a subset of survey questions which address training received during fellowship in specific content areas; these questions were asked only of ASN members who completed adult (Internal Medicine) or pediatric nephrology training programs in 2004 to 2008 to limit responses to those most likely to be reflective of current training programs and practices. Because only 11 responses were received from individuals trained in pediatric nephrology, only responses from adult nephrology-trained respondents are considered here. For each content area, respondents were asked to: “rate your fellowship training” (1 = little or no training, 2 = some training but not enough to feel competent, 3 = well trained, competent), and “how important is it in your current practice” (1 = not at all important, 2 = somewhat important, 3 = very important). The initial survey was sent via e-mail in June 2009 by the ASN to all of its members; two follow-up reminders were sent approximately 2 and 3 weeks later, and the survey was closed in July 2009. The survey was written by the author, then reviewed and modified in response to comments by the ASN Council; other members of the ASN, including the chair of the Training Program Director Executive Committee; and an expert in psychometrics and instrument development. Responses to the survey were entered by the respondents directly into an internet-based database and were anonymous. The survey and this study were approved by the University of Pennsylvania Office of Regulatory Affairs, which determined that informed consent was not required. Between-group comparisons were performed with Pearson χ2 test with P < 0.05 (two-tailed) considered to be statistically significant.
Results
Responses to the entire survey were provided by 933 ASN members; responses in this report are limited to those from the 133 respondents who indicated that they completed adult nephrology fellowship training in 2004 to 2008. The demographic characteristics of respondents are shown in Table 1.
Table 1.
Demographic characteristics of survey respondents who completed adult nephrology fellowship training in 2004 to 2008 (n = 133)
| Characteristic | Value, % |
|---|---|
| Gender | |
| male | 68.5 |
| female | 31.5 |
| Ethnicity/race | |
| Caucasian | 47.7 |
| South Asian | 21.5 |
| East Asian | 11.5 |
| African-American | 6.9 |
| Hispanic | 5.4 |
| Board certified in Internal Medicine | 98.5 |
| Board certified in Nephrology | 93.2 |
| U.S. nephrology training program | 92.4 |
| Trained at academic hospital-based program | 80.3 |
| Trained at academic-affiliated or community hospital-based program | 9.8 |
| 2-yr clinical training program | 62.1 |
| Clinical plus research training program >2 yr in duration | 34.8 |
| U.S. medical school | 63.4 |
| U.S. residency training program | 95.4 |
| Practice type | |
| private practice | 42.9 |
| academic medical center | 40.6 |
| industry | 2.3 |
| research | 3.0 |
| Involved in patient care | |
| yes | 97.7 |
| no | 2.3 |
Patient Care
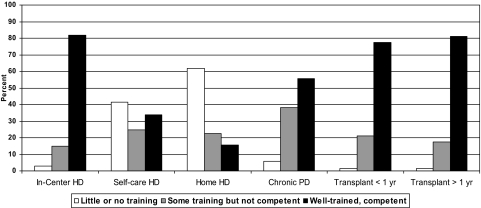
Approximately 80% of respondents reported that they were well trained and felt competent leaving fellowship in the care of chronic in-center hemodialysis (HD) patients and transplant patients (Figure 1). Only 55.6% felt well trained and competent in the care of chronic peritoneal dialysis (PD) patients, and even fewer felt well trained and competent in the care of self-care HD patients (33.8%) and home HD patients (15.8%). For these last two areas, 41.4% and 61.7% of respondents, respectively, indicated that they received little or no training. Each of these areas of patient care was reported to be very or somewhat important in the current career or practice of 64.2% to 92.5% of respondents.
Figure 1.
Reported training level and competence in care of dialysis and transplant patients.
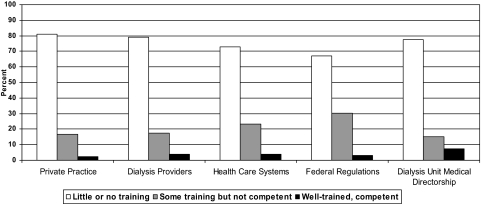
Business and Administrative Aspects of Medical Practice
Few respondents reported being well trained and competent in any of the surveyed areas of business, administrative, and regulatory aspects of medical practice (Figure 2), with most indicating that they received little or no training in these areas. A majority of respondents (68.4% to 90.2%) indicated that each of these areas was either somewhat important or very important in their current career or practice. Respondents who were in private practice were more likely (P < 0.05) to report all business and administrative-related areas as somewhat or very important compared with respondents at academic medical centers; there were no statistically significant differences between these groups in the percentage of respondents who reported themselves well-trained and competent in these areas.
Figure 2.
Reported training level and competence in business and administrative aspects of nephrology.
Disease Diagnosis and Management
The majority of respondents felt well trained and competent in many areas of disease diagnosis and management (Table 2). Topic areas for which fewer than 75% of respondents reported being well trained and competent were kidney stones, genetic renal disorders, children with kidney disease, adults with childhood kidney disease, renal complications of pregnancy, poisoning, nutrition, end-of-life care, and clinical pharmacology. More than 80% of respondents indicated that each of these topics was very important or somewhat important in their current career or practice, with the exception of children with kidney diseases (27.8%).
Table 2.
Responses to questions regarding training experience in disease diagnosis and management
| Little or No Training | Some Training but Not Enough to Feel Competent | Well Trained | |
|---|---|---|---|
| Kidney stones | 9.0 | 27.1 | 63.9 |
| Complex hypertension | 1.5 | 14.3 | 84.2 |
| Acute GN | 1.5 | 12.8 | 85.7 |
| Nephrotic syndrome | 0.8 | 9.8 | 89.5 |
| Diabetic nephropathy | 0 | 1.5 | 98.5 |
| Other glomerular diseases | 1.5 | 19.5 | 78.9 |
| Renovascular disease | 1.5 | 15.8 | 82.7 |
| Chronic kidney disease and its complications | 0 | 1.5 | 98.5 |
| Electrolyte disorders | 1.5 | 13.5 | 85.0 |
| Acid-base disorders | 1.5 | 12.0 | 86.5 |
| Genetic renal diseases | 15.0 | 49.6 | 35.3 |
| Children with kidney disease | 76.7 | 20.3 | 3.0 |
| Adults with childhood kidney disease | 27.8 | 46.6 | 25.6 |
| Acute renal failure/acute kidney injury | 0 | 1.5 | 98.5 |
| Patients with acute critical illness, sepsis, etc. | 0.8 | 5.3 | 94.0 |
| Renal complications of pregnancy | 7.5 | 46.6 | 45.9 |
| Poisonings | 9.0 | 36.8 | 54.1 |
| Primary care related to chronic kidney disease/ESRD patients | 4.5 | 14.3 | 81.2 |
| Nutrition | 12.8 | 51.9 | 35.3 |
| End-of-life care | 19.5 | 29.3 | 51.1 |
| Clinical pharmacology | 11.9 | 43.6 | 45.1 |
| Nephrotoxicity of drugs | 2.3 | 15.8 | 82.0 |
| Renal physiology | 0.8 | 18.8 | 80.5 |
All values are given in percentages.
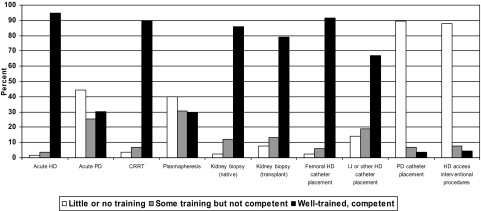
Procedures
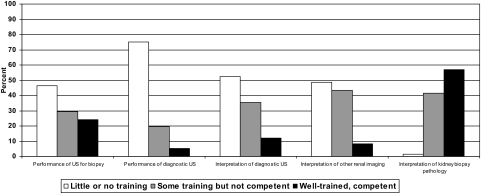
As shown in Figure 3, most respondents indicated that they were well trained and competent in performing acute HD, continuous renal replacement therapy (CRRT), native and transplant kidney biopsy, and placement of temporary HD catheters, but fewer reported feeling well trained and competent in performing acute PD (30.1%), plasmapheresis (29.3%), placement of PD catheters (3.8%), and HD access interventions (4.5%). Few respondents reported feeling well trained and competent in performing ultrasound (US) for renal biopsy (24.1%) or diagnostic purposes (5.3%) and interpreting diagnostic renal US (12.0%) or other renal imaging studies (8.2%) (Figure 4). A larger proportion of respondents (57.1%) indicated that they felt well trained and competent in interpreting kidney biopsy pathology. Each of the procedures was reported to be very or somewhat important to the current career or practice of 60.2% to 96.3% of respondents, except placement of PD catheters (20.3%), interventional procedures (30.0%), and performance of renal US for biopsy (48.9%) or diagnostic (41.4%) purposes.
Figure 3.
Reported training level and competence in acute dialysis, plasmapheresis, kidney biopsy, and dialysis access placement. IJ, internal jugular.
Figure 4.
Reported training level and competence in US and other imaging performance and interpretation and kidney biopsy pathology interpretation.
Research and Other Topics
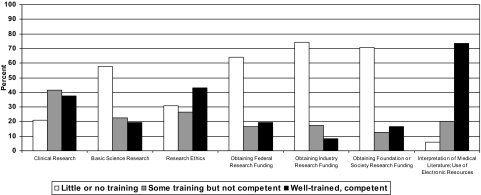
In areas related to research, most respondents indicated that they had not received sufficient training to feel competent, other than in skills necessary for interpreting medical literature and using electronic resources (Figure 5); each of these areas was reported to be somewhat or very important in the career or practice of 50% or more of respondents, except performance of bench/basic science research (36.1%). Respondents who were in academic medical center positions compared with those in private practice were more likely to report themselves as well trained and competent for each research-related area (P < 0.05) except clinical research and interpretation of medical literature/use of electronic resources. Even among respondents in academic positions, only 29.6% reported feeling well trained and competent in bench/basic science research, and only 11.1% to 35.2% reported feeling well trained and competent in obtaining federal, industry, or foundation/society research funding. All research-related areas were more likely (P < 0.05) to be reported as somewhat or very important by these respondents.
Figure 5.
Reported training level and competence in research and related topics.
Discussion
This survey provides a view of the successes and failures of renal fellowship experiences across a wide spectrum of patient care, core knowledge, procedures, research experience, and exposure to business and administrative aspects of nephrology. The survey also assesses the perceived importance of each specific area to the careers and practices of respondents.
There have been very few published assessments of the scope and success of training provided by nephrology fellowship programs. The effectiveness of renal fellowship training for clinical practice was assessed in a survey of nephrologists who trained in the 1970s and 1980s and successfully passed the ABIM nephrology subspecialty exam in 1974, 1980, and 1986; this report was published in 1991 and is thus not reflective of current training experiences (1). Training was reported to be effective in the areas of fluid and electrolyte disorders, acid-base metabolism, glomerular diseases, systemic disorders affecting the kidneys, and many aspects of patient care, but ineffective in many areas related to the theoretical and practical aspects of dialysis for end-stage renal disease, renal US and other renal imaging studies, management of renal transplant patients, pediatric nephrology, transplant immunology, the kidney in pregnancy, kidney stone disease, and nutrition. Respondents to this early survey indicated a high degree of training effectiveness for acute PD access but less effectiveness for CRRT (in that survey, continuous arteriovenous therapies), plasmapheresis, chronic PD, and access for chronic PD. It is interesting to note that some of the areas noted for training ineffectiveness more than 20 years ago were also similarly identified in the survey presented here by more recent trainees.
Specific areas of curriculum content and training, including technical and other skills that are expected to be addressed by clinical experience, formal instruction, and other components of training programs such as conferences, are delineated in the ACGME Program Requirements for Fellowship Education in Nephrology and Pediatric Nephrology. A nephrology core curriculum was also developed by the ASN and its Training Program Director's Committee more than 10 years ago (3), but it is not clear to what extent this influences current fellowship training. Although ACGME Program Requirements for Fellowship Education specify specific topics and procedure for which training is required, there are no defined criteria for determining competence, which is left largely to the discretion of each individual training program director.
Position papers recommending minimal training necessary for competence in percutaneous renal biopsy, acute hemodialysis, continuous arteriovenous hemodialysis, and acute peritoneal dialysis were published by the American College of Physicians 20 years ago (4–7), noting specific cognitive and technical skills needed but not how technical competence should be determined or a specific number of procedures that should be performed during training. Others have suggested the minimum number of procedures needed to achieve and maintain competence (8). A survey of nephrology program training program directors that was published many years ago assessed training provided in their programs (9) but did not address the competence of trainees, the need for which was addressed more than 20 years ago (10) and is now an expectation of all training programs. The exposure of nephrology trainees to various procedures was recently detailed on the basis of a survey of training program directors (2). Although that survey revealed a wide variation in the training experiences and required number of procedures needed to assess competency, it did not assess success of training programs in achieving procedural competence. There has never been an assessment of the success of nephrology fellowship programs in procedural training, nor is this as part of the ABIM nephrology certifying examination.
In each of the last 5 years, similar to most other Internal Medicine subspecialty exams, 91% to 93% of first-time takers for initial certification passed the ABIM subspecialty exam in nephrology, suggesting that by this benchmark, the basic core knowledge of nephrology was effectively conveyed during fellowship training. This is supported by the findings reported here. The only other broad assessment of training comes from the nephrology in-training exam, which was administered for the first time in April 2009. This exam tests core knowledge in the same areas that are tested with the ABIM nephrology certifying exam (11). Fellows taking this exam were also required to complete a survey asking “Do you consider your training in the following subject area to be adequate?” for many of the same topic or subject areas that were addressed in the survey reported here. Areas in which more than 25% of fellows during their second or later year of training answered “No” included cystic kidney diseases (50.1%), plasmapheresis (60.1%), renal US (51.8%), PD (36.5%), home HD (65.0%), arteriovenous access management (34.4%), nephrolithiasis (34.7%), geriatrics (25.2%), and palliative care (37.4.%) (M. Rosner, personal communication). Thus, several of the areas cited by respondents to the survey reported here as not providing adequate training were similarly cited by fellows still in training, emphasizing the need to address these areas of training.
It is clear from the survey results that recent trainees feel very well prepared (well trained and competent) in many areas, particularly in care of in-center HD patients and patients with kidney transplants, the diagnosis and management of many renal and fluid, electrolyte, and acid-base disorders, renal physiology, drug nephrotoxicity, acute HD, CRRT, renal biopsy, and placement of femoral HD catheters, but there are also many areas where recently trained nephrologists feel that their training did not result in competence. Table 3 lists the surveyed topic areas for which recent trainees in adult nephrology who are in the first several years of their careers indicated that they received little or no training or some training but not enough to feel competent and the associated perception of the importance of that area to their current careers or practice. These data should be informative in allowing training program directors to target those specific areas during the training of current and future fellows. As would be expected, there were significant differences among respondents in private practice and academic medical centers in level of perceived competence and importance of business/administrative aspects of nephrology and research-related areas.
Table 3.
Comparison of areas identified by >25% of respondents as having provided little or no training or some training but not enough to feel competent and perceived importance of those areas
| Little or No Training/Some Training but Not Enough to Feel Competent | Somewhat or Very Important | |
|---|---|---|
| Care of chronic self-care HD patients | 66.2 | 64.7 |
| Care of chronic home HD patients | 84.3 | 63.9 |
| Care of chronic PD patients | 44.3 | 91.7 |
| Business aspects of practice | 92.4 to 97.7 | 68.4 to 90.2 |
| Nephrolithiasis | 36.1 | 93.9 |
| Genetic renal disease | 64.6 | 83.4 |
| Children with kidney disease | 97.0 | 27.8 |
| Adults with childhood kidney disease | 74.4 | 82.0 |
| Renal complications of pregnancy | 54.1 | 88.7 |
| Poisoning | 45.8 | 89.4 |
| Nutrition | 64.7 | 97.0 |
| End-of-life care | 48.8 | 96.2 |
| Clinical pharmacology | 54.9 | 95.4 |
| Acute PD | 70.0 | 60.2 |
| Plasmapheresis | 70.6 | 77.4 |
| IJ catheter placement | 33.1 | 72.2 |
| PD catheter placement | 96.3 | 10.6 |
| Interventional procedures (HD access) | 95.5 | 30.0 |
| Performance of renal US for biopsy | 75.9 | 48.9 |
| Performance of diagnostic renal US | 94.7 | 41.4 |
| Interpretation of diagnostic renal US | 87.9 | 64.7 |
| Interpretation of other renal imaging studies | 91.8 | 70.7 |
| Interpretation of renal biopsy pathology | 52.9 | 87.2 |
| Performance of clinical research | 62.5 | 69.9 |
| Performance of bench/basic science research | 80.5 | 36.1 |
| Research ethics | 57.1 | 66.2 |
| Obtaining federal research funding | 80.4 | 50.3 |
| Obtaining industry research funding | 91.7 | 52.6 |
| Obtaining foundation or society research funding | 83.5 | 51.2 |
| Interpreting medical literature | 26.3 | 94.8 |
IJ, internal jugular. All values are given in percentages.
There are limitations to our findings. The survey was developed and written by the author with the involvement of experts in survey methodology, and its content was reviewed and revised in response to suggestions by other experts in nephrology and nephrology training, but it was not “field tested” before its general distribution to ASN members. Additionally, no attempt was made to verify the accuracy of the responses. The total number of responses to the survey was relatively small, and it is not possible to determine the response rate from among only those who trained in 2004 to 2008. It is known, however, that approximately 375 fellows complete training in the United States each year; thus, respondents to this survey represent approximately 8% to 10% of the number of graduating fellows each year. It is not possible to determine whether the respondents differed in any meaningful way in their fellowship training experiences or later career paths from others who did not respond. Although the small number of responses may limit the generalizability of the findings reported here, respondents do appear to represent the spectrum of training program experiences and subsequent career and practice types. Finally, the survey assessed self-perceived competence but not any objective assessment of knowledge or competence.
Despite the relatively small number of respondents, this survey provides the only current and detailed assessment of training of renal fellows in the United States across a wide spectrum of learning and content areas. Perceptions of the adequacy of training are not the same as an account of the actual training provided, nor are they necessarily accurate indicators of the actual skills of the respondent. Nevertheless, the results have potentially important implications for nephrology and nephrology education. The survey provides a large degree of reassurance that nephrology fellowships, for the most part, are doing an excellent job of training in many core knowledge areas and areas of clinical care, including some procedures. Gaps in training in areas that are also cited by survey respondents as being important in their post-training careers (Table 3) are most critical to address in fellowship training as well as in post-training continuing medical education programming, for which these survey results will hopefully serve as a useful needs assessment.
Addressing these deficits may require development of new online and/or print curricula, as was recently done by the ASN for geriatric nephrology, and specific programming at meetings by the ASN and other national and regional nephrology organizations, perhaps especially in areas such as interpretation of renal biopsy pathology, core knowledge areas where expertise and experience at individual training programs may be limited (such as poisoning, clinical pharmacology, and care of adults with childhood kidney diseases), business and administrative aspects of nephrology, and areas related to research and research funding. Expanded use of simulation training centers and other types of programs for procedural training and competency assessment, and changes in the allocation of time devoted to didactic and clinical training away from some areas where training is broadly perceived to be excellent to those where training is perceived as being less than adequate (in this survey and the recent in-training exam) may be required to address perceived deficiencies in core knowledge and procedural areas. There may also be value to developing regional training programs at fellowship training sites with extensive resources, particular areas of expertise, and large patient populations in certain areas, such as PD, self-care and home HD, plasmapheresis, and performance and interpretation of renal US. Self-directed and lifelong learning are also essential and should be supported and encouraged during fellowship training experiences.
Disclosures
None.
Acknowledgments
The author wishes to gratefully acknowledge the assistance of Judy Shea, Susan Owens, Tod Ibrahim, Donald Kohan, members of the ASN Council, Liz O'Grady, Adam Berns, and Stan Goldfarb for assistance in the development of this survey, analysis of the results, and useful comments on the manuscript, and Mitchell Rosner for providing information from the ASN In-Training Examination.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Nephrology Fellowship Training in the 21st Century: Where Do We Stand?” on pages 387–389.
References
- 1.Kimmel PL, Bosch JP: Effectiveness of renal fellowship training for subsequent clinical practice. Am J Kidney Dis 18: 249–256, 1991 [DOI] [PubMed] [Google Scholar]
- 2.Berns JS, O'Neill WC: Performance of procedures by nephrologists and nephrology fellows at U.S. nephrology training programs. Clin J Am Soc Nephrol 3: 941–947, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumar R, Alpern R, Berl T, Blantz R, Chevalier R, Hostetter T, Madias N, Salant D, Wiggins R, Bennett W, Chapman A, Ekonyan G, Falk R, Gennari FJ, Helderman JH, Hruska K, Levey A, Lindheimer M, Miller R, Nissenson A, Schwab S, Schwab T, Schwartz R, Wilcox C: Nephrology core curriculum. The American Society of Nephrology and the American Society of Nephrology Training Program Directors Committee. J Am Soc Nephrol 8: 1018–1027, 1997 [DOI] [PubMed] [Google Scholar]
- 4.Clinical competence in acute peritoneal dialysis Health and Public Policy Committee, American College of Physicians. Ann Intern Med 108: 763–765, 1988 [PubMed] [Google Scholar]
- 5.Clinical competence in acute hemodialysis Health and Public Policy Committee, American College of Physicians. Ann Intern Med 108: 632–634, 1988 [PubMed] [Google Scholar]
- 6.Clinical competence in percutaneous renal biopsy Health and Public Policy Committee. American College of Physicians. Ann Intern Med 108: 301–303, 1988 [PubMed] [Google Scholar]
- 7.Clinical competence in continuous arteriovenous hemofiltration Health and Public Policy Committee, American College of Physicians. Ann Intern Med 108: 900–902, 1988 [PubMed] [Google Scholar]
- 8.Tape TG, Wigton RS, Blank LL, Nicolas JA: Procedural skills of practicing nephrologists. A national survey of 700 members of the American College of Physicians. Ann Intern Med 113: 392–397, 1990 [DOI] [PubMed] [Google Scholar]
- 9.Levin N, Cu G, McDonald F: The education of nephrology fellows–some recent observations. Semin Dial 5: 278–281, 1992 [Google Scholar]
- 10.Cohen JJ, Glassock RJ, Benson JA, Jr.: Evaluation of clinical competence in nephrologists. Kidney Int 33: 608–609, 1988 [DOI] [PubMed] [Google Scholar]
- 11.Rosner MH, Berns JS, Parker M, Tolwani A, Bailey J, DiGiovanni S, Lederer E, Norby S, Plumb TJ, Qian Q, Yeun J, Hawley JL, Owens SASN In-Training Examination Committee: Development, implementation and results of the ASN in-training examination for fellows. Clin J Am Soc Nephrol 5: 328–334, 2010 [DOI] [PubMed] [Google Scholar]