Abstract
A broad spectrum of colonic complications can occur in patients with colon cancer. Clinically, some of these complications can obscure the presence of underlying malignancies in the colon and these complications may require emergency surgical management. The complications of the colon that can be associated with colon cancer include obstruction, perforation, abscess formation, acute appendicitis, ischemic colitis and intussusception. Although the majority of these complications only rarely occur, familiarity with the various manifestations of colon cancer complications will facilitate making an accurate diagnosis and administering prompt management in these situations. The purpose of this pictorial essay is to review the CT appearance of the colonic complications associated with colon cancer.
Keywords: Colon, Colon neoplasms, Complications, Computed tomography (CT), Introduction
Computed tomography (CT) has played an important role in the preoperative staging and postoperative surveillance of colon cancer (1). The recent advances in CT technology provide greater accuracy for the preoperative staging of colorectal cancer (2). The findings associated with adenocarcinoma of the colorectum generally include asymmetric bowel wall thickening with contrast enhancement or the presence of a soft-tissue mass that frequently leads to luminal narrowing or obstruction. Colorectal cancer may occasionally be associated with a wide spectrum of colonic complications that commonly cause acute abdominal symptoms. Various complications such as obstruction, perforation, abscess formation, acute appendicitis, ischemic colitis and intussusception can occur in patients with colon cancer. Moreover, colon cancer can be clinically and/or radiologically obscured by these complicated conditions, and this may result in a delayed diagnosis and treatment. Thus, radiologists should be familiar with the uncommon presentations of colon cancer. In this article, we present the CT findings of the colonic complications that are associated with colon cancer.
Colon Cancer with Bowel Obstruction
Bowel obstruction is the most commonly observed complication of colon cancer. The reported frequency of patients with obstructive colon cancer has ranged from 8% to 29% (3). Left-sided colon malignancies are more prone to obstruct the colon lumen than are the right-sided malignancies. This is because the diameter of the left colon is smaller than that of the right colon. CT is a sensitive imaging modality for detecting bowel obstruction, and the multiplanar reconstruction images can provide additional information on the transition point in problematic cases (1). Identifying the transitional zones and an obstructing lesion on CT, and these usually appear as irregular circumferential thickening of the colon, is important to differentiate this entity from other benign conditions such as adynamic ileus, colonic pseudoobstruction and stercoral colitis, and all these maladies can present with colonic dilatation.
Because of the relatively larger diameter of the cecal lumen, cecal adenocarcinomas have a tendency to grow without displaying clinical manifestations for a long time (4). Therefore, cecal cancer only infrequently presents as bowel obstruction; as the initial manifestation, distal small bowel obstruction has been reported to occur in 1.5-8.1% of the patients with cecal cancer (5). Additionally, adenocarcinoma developing near the ileocecal valve area can cause distal small bowel obstruction even though the tumor is small (Fig. 1). CT is also useful for examining cecal cancer patients who present with small bowel obstruction. Careful inspection of the cecum on the CT, and especially the ileocecal valve area, is needed to diagnose this rare condition.
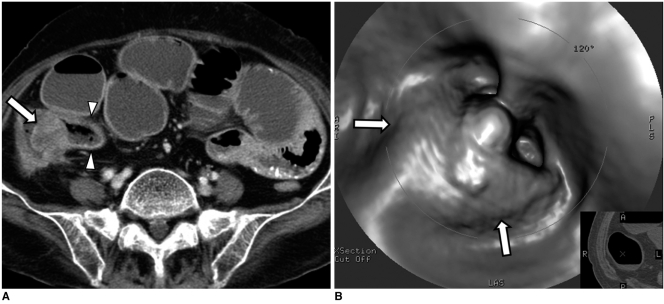
Fig. 1.
80-year-old woman with adenocarcinoma near ileocecal valve and she presented with small bowel obstruction.
A. Contrast-enhanced axial CT scan shows polypoid mass obstructing ileocecal valve area (arrow). Note dilated small bowel loops, including terminal ileum (arrowheads).
B. Endoluminal 3D view from CT colonography shows polypoid mass at ileocecal valve area (arrows).
Closed-loop obstruction is a unique form of mechanical obstruction in which two points of a bowel segment are occluded, and this most frequently occurs in the small bowel (6). On rare occasion an obstructing colon cancer with a competent ileocecal valve can lead to the condition in which the intraluminal pressure of the colon proximal to the obstructing mass increases due to failure of decompression through the ileocecal valve; this produces effects that are similar to those of a closed-loop obstruction in the small bowel (7). On CT, this condition can be identified as an obstructive colon mass that causes severe dilatation of the proximal colon (Fig. 2). The affected colon is usually filled with fecal material, and the small bowel is not dilated due to a competent ileocecal valve. Radiologists and surgeons should be aware of a closed-loop obstruction associated with colon cancer because this is an urgent surgical situation that can lead to a perforated colon.
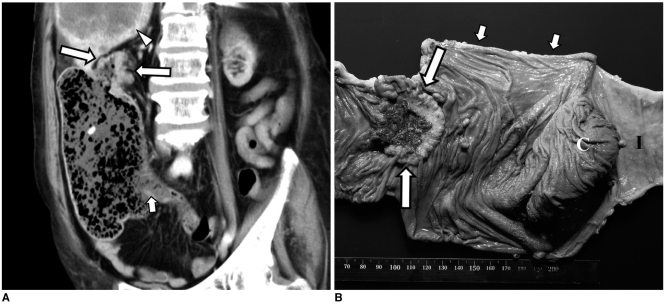
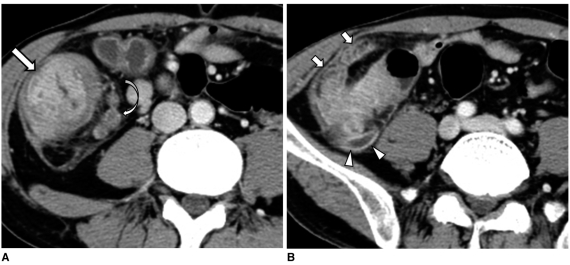
Fig. 2.
75-year-old woman with closed-loop obstruction secondary to adenocarcinoma of ascending colon and she had competent ileocecal valve.
A. Oblique coronal reformatted CT image shows obstructive mass in distal ascending colon (arrows) and marked dilatation of proximal colon that was filled with fecal material. Small bowel is not dilated and ileocecal valve area is indicated by short arrow. Also noted is hepatic metastasis (arrowhead).
B. Two days after CT scan, patient underwent emergency right hemicolectomy for her colon perforation. Photograph of resected specimen shows obstructive mass in ascending colon (arrows) and segmental dilatation of colon proximal to mass (short arrows). Perforation occurred just below colon cancer (not shown). C = cecum, I = terminal ileum.
Perforated Colon Cancer
Perforation occurs in 2.5-10% of the patients with colon cancer (8, 9). Perforated colon cancer can present as a free perforation with peritoneal spillage or as a localized perforation with an abscess or fistula formation (9) (Figs. 3, 4). In addition, perforation can occur at the site of the colon cancer secondary to tumor necrosis or the adjacent inflammation, or it can occur at the proximal portion of the colon cancer due to the increased pressure proximal to the tumor (3) (Figs. 3, 4). Perforated colon cancer can occasionally cause fistula formation between the colon and the adjacent organs such as the urinary bladder, the female genital tract or the bowel.
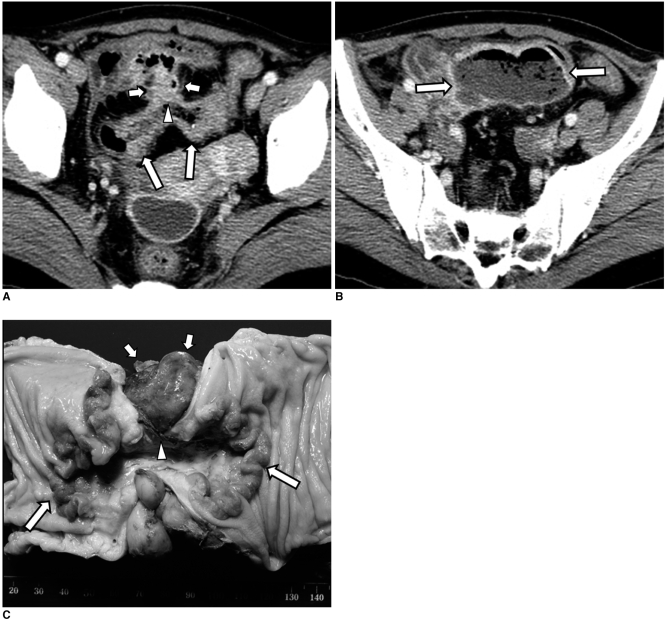
Fig. 3.
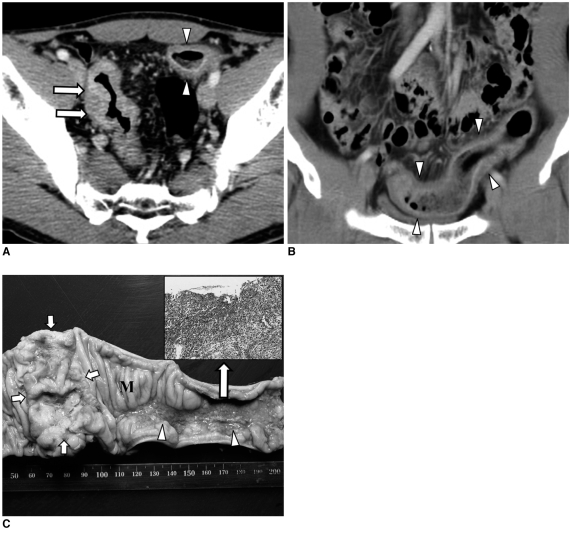
53-year-old woman with adenocarcinoma of sigmoid colon.
A, B. Contrast-enhanced axial CT scans show segmental wall thickening with contrast enhancement involving sigmoid colon (arrows in A). Anterior colon wall defect (arrowhead) with pericolic enhancing mass (short arrows) is identified. There is large abscess (arrows in B) in cranial direction to enhancing mass.
C. Photograph of specimen reveals ulcerofungating mass (arrows) with focal perforation (arrowhead). Pericolic inflammatory mass is also seen (short arrows).
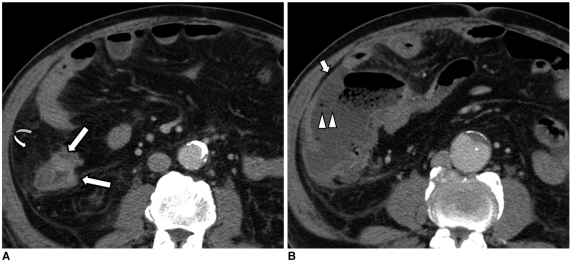
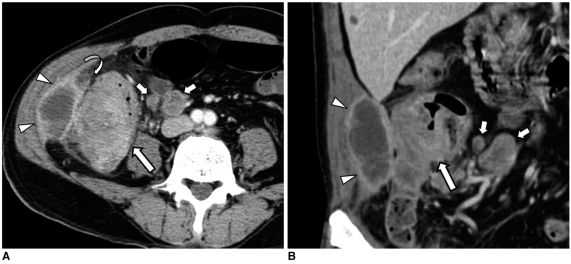
Fig. 4.
72-year-old man with adenocarcinoma of ascending colon.
A. Contrast-enhanced axial CT scan shows irregular thickening of ascending colon (arrows) and pericolic fat stranding (curved arrow).
B. Caudal to colon wall thickening, there are colon wall defect (arrowheads) at level of ileocecal valve and adjacent peritoneal fluid (short arrow). Free perforation was surgically confirmed at proximal portion of colon cancer.
The various potential causes of colonic perforation include malignant neoplasm, diverticulitis, trauma, ischemia, inflammatory bowel disease and stercoral colitis (10). Perforation of the colon that is induced by these causes can be diagnosed by CT with the demonstration of a focal defect in the colon wall that may be accompanied by a fluid-density abscess, free air or stranding of the pericolic fat. In order to differentiate colonic perforation that is caused by cancer from that caused by various benign conditions, identifying the irregular wall thickening of the adjacent colon is critical for making the diagnosis of an underlying colon cancer. CT has been reported to be an effective modality for detecting perforated colorectal cancer because it reveals pericolic inflammatory changes and abscess formation, as well as a colorectal mass (8). However, in some cases, identification of severe pericolic inflammation with a large abscess or peritoneal spillage may make it difficult to make an accurate diagnosis because these situations can mimic various conditions that cause perforation of the colon. Although it is still a matter of debate whether perforation can cause peritoneal seeding, making an early, accurate diagnosis and administering aggressive treatment might improve patient survival (3).
Colon Cancer with an Abscess
Abscess formation associated with colon cancer is a rare complication that occurs in 0.3-4% of the patients with colon cancer (11). Perforation of the colon, fistula formation between the colon and adjacent structures, or direct tumor invasion can result in the formation of an abscess. The most common location for abscess formation is the peritoneal cavity, including the paracolic space and the pelvic cavity (Figs. 3, 5); however, fistula formation or inflammation that spreads along the tissue planes may lead to abscesses in unusual locations such as the retroperitoneum, the abdominal wall, the perirectal space, the psoas muscle and the thigh (11-13) (Figs. 6, 7). In the cases that present with these unusual clinical findings, making the accurate diagnosis of an underlying colon cancer may be more difficult. Further, abscess-forming colon cancers that occur in the right lower quadrant or the pelvic cavity can be mistaken for inflammatory conditions, including diverticulitis, appendicitis with perforation and pelvic inflammatory disease. Relatively severe pericolic fat stranding adjacent to a thickened colon wall is generally the most significant CT finding for differentiating inflammatory diseases from colon cancer that is without perforation or abscess (4, 14). However, if perforation or abscess is present in patients with colon cancer, then physicians can be faced with diagnostic uncertainty with a CT finding of severe pericolic fat stranding. Evaluation and characterization of a thickened bowel wall is needed in this situation; marked asymmetric wall thickening with loss of stratified enhancement that involves a short segment of the colon favors the diagnosis of an underlying malignancy, while preserved layering of a thickened bowel wall is an important feature favoring the diagnosis of benign inflammatory conditions (4, 14). Moreover, an abrupt transition from a normal to an abnormal bowel wall is characteristic of malignancy, whereas a smooth, gradual, long transition is usually present in benign conditions (4). The presence of pericolic lymphadenopathy is more commonly found in colon cancer than it is in benign conditions (4, 14). Therefore, in cases that display the confusing manifestations of severe pericolic fat stranding, the physician must perform a morphologic analysis of the abnormal bowel, including determining the enhancement pattern, the length of the abnormal bowel, the wall thickness at the site of interest and the transition from a normal wall to an abnormal wall.
Fig. 5.
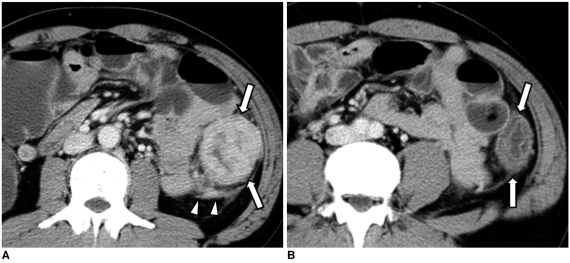
65-year-old man with adenocarcinoma of ascending colon.
A, B. Contrast-enhanced axial CT scan and coronal reformations show colon wall thickening with contrast enhancement (arrows), low-attenuated lesion of right paracolic gutter attached to abdominal wall (arrowheads) and adjacent fat stranding (curved arrow). Note pericolic enlarged lymph nodes (short arrows). Pericolic low-density lesion was surgically confirmed and it was pathologically diagnosed as inflammatory mass with abscess. There was no tumor involvement in peritoneal wall.
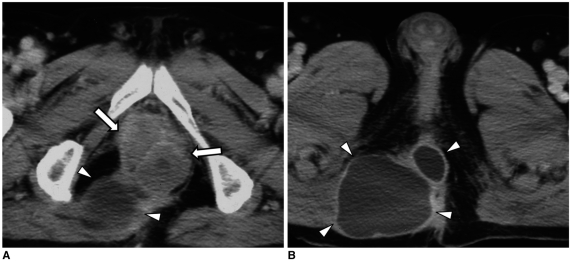
Fig. 6.
71-year-old woman with adenocarcinoma of ascending colon.
A, B. Contrast-enhanced axial CT scans show polypoid enhancing mass with colon wall thickening (arrows). Colon perforation occurred at posterior wall of ascending colon (arrowheads), resulting in abscess formation in iliacus muscle (short arrows).
Fig. 7.
74-year-old man with adenocarcinoma of rectum.
A, B. Contrast-enhanced axial CT scans show irregular, enhancing mass in rectum (arrows) with abscesses in perianal area (arrowheads).
In patients with mucinous carcinoma of the colon or appendix, the hypoattenuated areas caused by extracellular mucin components can sometimes mimic the appearance of an abscess. It has also been reported that for colon cancer patients who present with an abdominal wall abscess, many cases were a mucinous carcinoma, and this is thought to be due to the tumor characteristics; mucinous carcinomas have a tendency to grow slowly and to spread by direct extension (12). The presence of intratumoral calcification and the relative absence of pericolic fat stranding can be useful for differentiating a mucinous carcinoma from an abscess (Fig. 8). Yet the overlap in the imaging appearances often complicates differentiating an abdominal wall abscess from abdominal wall invasion by a mucinous carcinoma (Fig. 9).
Fig. 8.
48-year-old woman with perforated mucinous carcinoma of appendix.
A. Contrast-enhanced axial CT scans show irregular, peripheral enhancing low-density lesion (arrows) connected to cecum (arrowhead). This air-containing lesion extends laterally to abdominal wall through retroperitoneum, and it mimics appearance of perforated appendicitis with periappendiceal abscess.
B. Nonenhanced axial CT image shows intratumoral calcifications (short arrows). Perforated mucinous carcinoma of appendix with direct invasion into abdominal wall was pathologically confirmed.
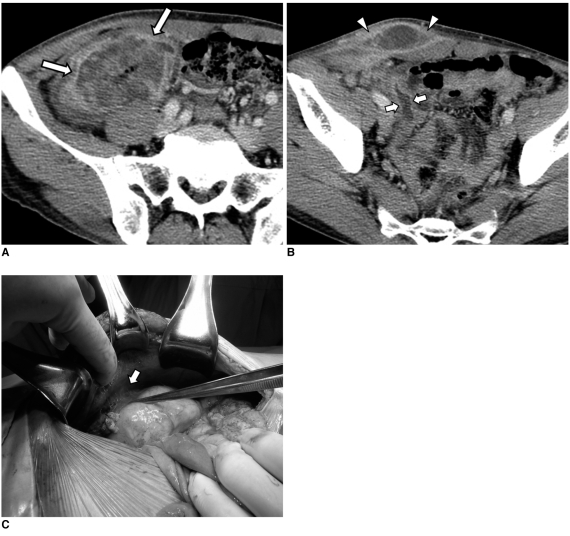
Fig. 9.
47-year-old man with mucinous adenocarcinoma involving cecum and proximal ascending colon.
A, B. Contrast-enhanced axial CT scans show marked circumferential wall thickening with large areas of low attenuation in cecum (arrows). Two lesions with low attenuation are identified in anterior abdominal wall (arrowheads) and pelvic cavity (short arrows), respectively.
C. At surgery, thickened colon wall was seen to be adhered to anterior abdominal wall (arrow). Mucinous material was drained from anterior abdominal wall during surgery, indicating that mucinous material spread by direct extension. There was also mucinous material in pelvic cavity. Perforated mucinous adenocarcinoma was pathologically confirmed.
Colon Cancer Presenting as Acute Appendicitis
Cecal cancer infrequently presents as an acute appendicitis with or without abscess formation (11, 15). Obstruction of the appendiceal lumen by cecal cancer can cause acute appendicitis. Cecal cancer has been found to be a cause of acute appendicitis in 10-25% of elderly patients and in only 3% of the patients between the ages of 20 and 40 years (11, 15). Making an accurate preoperative diagnosis can be difficult because the affected patients clinically present with acute abdominal symptoms that are compatible with an acute appendicitis. An inaccurate diagnosis without recognizing an underlying malignancy may lead to incomplete treatment. Therefore, identifying the cecal wall thickening with a loss of the layered enhancement patterns in patients with the clinical and imaging findings of an acute appendicitis should raise a suspicion for an underlying cecal cancer as the cause of the appendicitis (Fig. 10). In patients with acute appendicitis and who do not have cecal cancer, the appendiceal wall inflammation can occasionally extend directly to the cecum, resulting in cecal wall thickening. Cecal wall thickening that appears as focal wall thickening at the cecal apex contiguous with the appendix has been reported to be present in 80% of the patients with acute appendicitis (16).
Fig. 10.
40-year-old man with cecal adenocarcinoma and he presented with acute pain in right lower quadrant and leukocytosis.
A, B. Contrast-enhanced axial CT scans show wall thickening with contrast enhancement in cecum (arrow) and thickened appendix (arrowheads). Surrounding fat stranding is severe (short arrows). Note pericolic enlarged lymph nodes (curved arrow). Cecal adenocarcinoma with invasion of appendix that resulted in acute appendicitis was pathologically confirmed.
Ischemic Colitis Associated with Colon Cancer
Colonic wall thickening proximal to a colon mass is known as ischemic or obstructive colitis, and this had been reported to be present in 1-11% of the patients with obstructive colon cancer (17, 18). Although bowel ischemia induced by bowel distention is generally regarded as the mechanism that is involved in the development of colon wall thickening, this can occur in patients who are without obstruction of the colon. Moreover, one report showed that many of these changes in the colon were pathologically confirmed to be submucosal edema rather than frank bowel ischemia (18).
Colon ischemia or submucosal edema can manifest on CT as smooth, annular wall thickening with a homogeneous or layered enhancement pattern that is frequently contiguous with an irregularly thickened tumorous segment (17, 18). Some patients (10-30%) occasionally have intervening normal mucosa between the tumor and the ischemic segment; this can be explained by the Laplace law; the tension applied to the bowel wall increases proportionately to an increase in both the intraluminal pressure and the wall diameter (17, 18) (Fig. 11). A segmental distribution of colon wall thickening that is distal to a large fungating mass can also be present in approximately 10% of patients with colon cancer, and this pathologically corresponds to edema or colitis (19) (Fig. 12). Because bowel ischemia or edema commonly occurs in cases that have obstructing or large fungating masses, this secondary ischemic change can be easily distinguished from primary ischemic colitis.
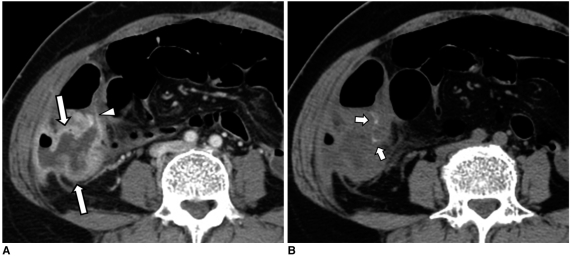
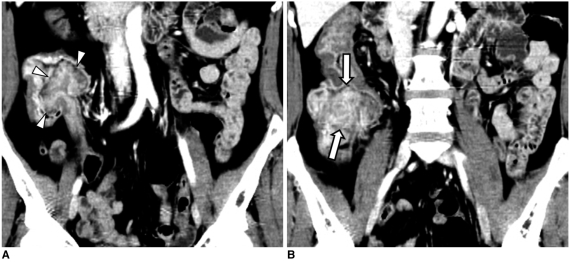
Fig. 11.
55-year-old man with ischemic colitis proximal to adenocarcinoma of sigmoid colon.
A, B. Contrast-enhanced axial CT scan and coronal reformations show irregular concentric wall thickening of sigmoid colon with contrast enhancement (arrows). Proximal to tumor segment, there is smooth, annular wall thickening with layered enhancement pattern involving long segment of sigmoid colon (arrowheads).
C. Photograph of resected specimen shows ulcerofungating mass in sigmoid colon (short arrows) and diffuse mucosal ulceration extending 10 cm proximal to tumor segment (arrowheads). This mucosal lesion was pathologically confirmed to be ischemic colitis (inset). Note intervening normal mucosa (M) between tumor and ischemic segment.
Fig. 12.
41-year-old man with adenocarcinoma of descending colon that was accompanied by distal segment of wall edema.
A. Contrast-enhanced axial CT scan shows large mass with contrast enhancement involving descending colon (arrows). Also note pericolic infiltration (arrowheads).
B. Axial CT scan obtained inferior to A shows mild annular wall thickening with preservation of wall layer in descending colon distal to tumor segment (arrows).
Colon Cancer Presenting as Intussusception
Although intussusception is rare in adults, the majority of adult intussusceptions are caused by lead points (20), and more than half of the patients with colon intussusceptions are related to malignant lesions such as adenocarcinoma, lymphoma or metastatic lesions (20). Adenocarcinoma of the colon is the most common lead mass for colon intussusceptions, and it can present as the ileocolic or colocolic forms (Figs. 13, 14). The CT demonstration of a bowel-within-bowel configuration with or without contained mesenteric fat or mesenteric vessels is considered pathognomonic for intussusceptions. A colon cancer can usually be identified as an enhancing mass within intussusceptions; however, identification of a lead mass is not always possible due to an edematous bowel wall (4, 20). In a previous study that used a multidetector-row CT scanner, the investigators reported that a lead mass could be distinguished from an edematous bowel in approximately 70% of the cases (21). In addition, they found that those intussusceptions with a lead point tended to be longer and larger in diameter as compared with the intussusceptions without a lead point; mechanical obstruction and pericolic infiltration were also valuable signs for determining the presence of a lead point (21).
Fig. 13.
52-year-old woman with ileocolic intussusception secondary to adenocarcinoma of ascending colon.
A. Coronal reformatted CT image shows invagination of ileal loop into colon (arrowheads).
B. Coronal reformatted CT image obtained posterior to A shows polypoid mass with contrast enhancement in ascending colon (arrows).
Fig. 14.
59-year-old woman with colocolic intussusception secondary to adenocarcinoma of sigmoid colon.
A, B. Contrast-enhanced axial CT scan and sagittal reformations show invagination of segment of colon (intussusceptum, arrowheads) through intussuscipiens (arrows). Note that lead point is seen as enhancing mass (M).
CONCLUSION
Colon cancer can present with a variety of complications. An accurate preoperative diagnosis of these conditions is critical to ensure that prompt, proper, treatment is administered. A variety of complicated situations can obscure making the diagnosis of underlying colon cancer, and the imaging features of colon cancer overlap with those imaging features of other pathological conditions. Being knowledgeable of the potential imaging findings of complicated colon cancers can help physicians arrive at an accurate diagnosis and then administer the appropriate treatment.
References
- 1.Horton KM, Abrams RA, Fishman EK. Spiral CT of colon cancer: imaging features and role in management. Radiographics. 2000;20:419–430. doi: 10.1148/radiographics.20.2.g00mc14419. [DOI] [PubMed] [Google Scholar]
- 2.Filippone A, Ambrosini R, Fuschi M, Marinelli T, Genovesi D, Bonomo L. Preoperative T and N staging of colorectal cancer: accuracy of contrast-enhanced multi-detector row CT colonography--initial experience. Radiology. 2004;231:83–90. doi: 10.1148/radiol.2311021152. [DOI] [PubMed] [Google Scholar]
- 3.Biondo S, Kreisler E, Millan M, Fraccalvieri D, Golda T, Marti Rague, J, et al. Differences in patient postoperative and long-term outcomes between obstructive and perforated colonic cancer. Am J Surg. 2008;195:427–432. doi: 10.1016/j.amjsurg.2007.02.027. [DOI] [PubMed] [Google Scholar]
- 4.Hoeffel C, Crema MD, Belkacem A, Azizi L, Lewin M, Arrive L, et al. Multi-detector row CT: spectrum of diseases involving the ileocecal area. Radiographics. 2006;26:1373–1390. doi: 10.1148/rg.265045191. [DOI] [PubMed] [Google Scholar]
- 5.Rovito PF, Verazin G, Prorok JJ. Obstructing carcinoma of the cecum. J Surg Oncol. 1990;45:177–179. doi: 10.1002/jso.2930450309. [DOI] [PubMed] [Google Scholar]
- 6.Balthazar EJ, Birnbaum BA, Megibow AJ, Gordon RB, Whelan CA, Hulnick DH. Closed-loop and strangulating intestinal obstruction: CT signs. Radiology. 1992;185:769–775. doi: 10.1148/radiology.185.3.1438761. [DOI] [PubMed] [Google Scholar]
- 7.McKay A, Bathe OF. A novel technique to relieve a closed-loop obstruction secondary to a competent ileocecal valve and an unresectable mid-colon tumor. J Gastrointest Surg. 2007;11:1365–1367. doi: 10.1007/s11605-007-0230-z. [DOI] [PubMed] [Google Scholar]
- 8.Hulnick DH, Megibow AJ, Balthazar EJ, Gordon RB, Surapenini R, Bosniak MA. Perforated colorectal neoplasms: correlation of clinical, contrast enema, and CT examinations. Radiology. 1987;164:611–615. doi: 10.1148/radiology.164.3.3615859. [DOI] [PubMed] [Google Scholar]
- 9.Tsai HL, Hsieh JS, Yu FJ, Wu DC, Chen FM, Huang CJ, et al. Perforated colonic cancer presenting as intra-abdominal abscess. Int J Colorectal Dis. 2007;22:15–19. doi: 10.1007/s00384-006-0097-6. [DOI] [PubMed] [Google Scholar]
- 10.Kim SH, Shin SS, Jeong YY, Heo SH, Kim JW, Kang HK. Gastrointestinal tract perforation: MDCT findings according to the perforation sites. Korean J Radiol. 2009;10:63–70. doi: 10.3348/kjr.2009.10.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Okita A, Kubo Y, Tanada M, Kurita A, Takashima S. Unusual abscesses associated with colon cancer: report of three cases. Acta Med Okayama. 2007;61:107–113. doi: 10.18926/AMO/32885. [DOI] [PubMed] [Google Scholar]
- 12.Matsumoto G, Asano H, Kato E, Matsuno S. Transverse colonic cancer presenting as an anterior abdominal wall abscess: report of a case. Surg Today. 2001;31:166–169. doi: 10.1007/s005950170204. [DOI] [PubMed] [Google Scholar]
- 13.Tsukuda K, Ikeda E, Miyake T, Ishihara Y, Watatani H, Nogami T, et al. Abdominal wall and thigh abscess resulting from the penetration of ascending colon cancer. Acta Med Okayama. 2005;59:281–283. doi: 10.18926/AMO/31957. [DOI] [PubMed] [Google Scholar]
- 14.Pereira JM, Sirlin CB, Pinto PS, Jeffrey RB, Stella DL, Casola G. Disproportionate fat stranding: a helpful CT sign in patients with acute abdominal pain. Radiographics. 2004;24:703–715. doi: 10.1148/rg.243035084. [DOI] [PubMed] [Google Scholar]
- 15.Arjona Sanchez A, Tordera Torres EM, Cecilia Martinez D, Rufian Pena S. Colon cancer presenting as an appendiceal abscess in a young patient. Can J Surg. 2008;51:E15–E16. [PMC free article] [PubMed] [Google Scholar]
- 16.Rao PM, Rhea JT, Novelline RA, McCabe CJ, Lawrason JN, Berger DL, et al. Helical CT technique for the diagnosis of appendicitis: prospective evaluation of a focused appendix CT examination. Radiology. 1997;202:139–144. doi: 10.1148/radiology.202.1.8988203. [DOI] [PubMed] [Google Scholar]
- 17.Ko GY, Ha HK, Lee HJ, Jeong YK, Kim PN, Lee MG, et al. Usefulness of CT in patients with ischemic colitis proximal to colonic cancer. AJR Am J Roentgenol. 1997;168:951–956. doi: 10.2214/ajr.168.4.9124147. [DOI] [PubMed] [Google Scholar]
- 18.Xiong L, Chintapalli KN, Dodd GD, 3rd, Chopra S, Pastrano JA, Hill C, et al. Frequency and CT patterns of bowel wall thickening proximal to cancer of the colon. AJR Am J Roentgenol. 2004;182:905–909. doi: 10.2214/ajr.182.4.1820905. [DOI] [PubMed] [Google Scholar]
- 19.Jang HJ, Lim HK, Park CK, Kim SH, Park JM, Choi YL. Segmental wall thickening in the colonic loop distal to colonic carcinoma at CT: importance and histopathologic correlation. Radiology. 2000;216:712–717. doi: 10.1148/radiology.216.3.r00se10712. [DOI] [PubMed] [Google Scholar]
- 20.Kim YH, Blake MA, Harisinghani MG, Archer-Arroyo K, Hahn PF, Pitman MB, et al. Adult intestinal intussusception: CT appearances and identification of a causative lead point. Radiographics. 2006;26:733–744. doi: 10.1148/rg.263055100. [DOI] [PubMed] [Google Scholar]
- 21.Tresoldi S, Kim YH, Blake MA, Harisinghani MG, Hahn PF, Baker SP, et al. Adult intestinal intussusception: can abdominal MDCT distinguish an intussusception caused by a lead point? Abdom Imaging. 2008;33:582–588. doi: 10.1007/s00261-007-9328-8. [DOI] [PubMed] [Google Scholar]