Abstract
OBJECTIVES
To examine the relationship between urinary incontinence (UI) and psychological distress in older adults. We hypothesized that persons with UI associated with condition-specific functional loss would be most likely to report psychological distress.
DESIGN
A population-based longitudinal survey.
SETTING
Continuing participants in a study of community-dwelling adults who were initially living in East Baltimore in 1981.
PARTICIPANTS
Persons aged 50 and older (n = 781) at follow-up interviews conducted between 1993 and 1996 for whom complete data were available.
MEASUREMENTS
Participants were classified as incontinent if they reported any uncontrolled urine loss within the 12 months preceding the 13-year follow-up interview. Condition-specific functional loss secondary to UI was further assessed based on a series of questions relating directly to participants’ inability to engage in certain activities due to their UI. Psychological distress was assessed using the General Health Questionnaire (GHQ) at interviews in 1981 and at the 13-year follow-up.
RESULTS
Persons with UI were more likely to experience psychological distress as measured by the GHQ than were persons without UI (unadjusted odds ratio (OR) = 1.74, 95% confidence interval (CI) = 1.13–2.68). Persons with condition-specific functional loss secondary to UI were substantially more likely to have psychological distress as measured by the GHQ than were persons without UI (unadjusted OR = 4.02, 95% CI = 1.86–8.70). In multivariate models that controlled for potentially influential characteristics such as age, gender, ethnicity, and chronic medical conditions the association between condition-specific functional loss secondary to UI and psychological distress remained statistically significant. Among people with UI, persons with persistently elevated GHQ scores were much more likely to report condition-specific functional impairment from UI (adjusted OR = 6.55, 95% CI = 1.94–22.12).
CONCLUSION
Individuals with UI, especially when incontinence was associated with condition-specific functional loss, were more likely to have psychological distress than were other older adults. Our findings support a general conceptual model that condition-specific functional impairment mediates the relationship between a chronic medical condition and psychological distress.
Keywords: urinary incontinence, older adults, psychological distress, depression, functional status
Urinary incontinence (UI) is a commonly encountered problem, especially in older adults. Although sampling and methodological differences account for variability in estimates from surveys, 1 the prevalence of UI in community-dwelling older adults has been reported as at least 10% for men and 20% for women. 2,3 As many as half of nursing home patients may be affected by UI. 4 However, despite the high prevalence of UI and although most incontinence can be improved or cured by medical treatment, 5–7 one study on UI in older adults found that only 38% of adults with UI spoke to their doctor about incontinence symptoms. 8 Psychological consequences associated with UI may reduce the likelihood that patients will actively seek treatment. 9
The detection and treatment of UI is important not only to avoid medical consequences but also to mitigate the psychological and social consequences of the condition. UI may cause shame, loss of self-confidence, and withdrawal from social activities. Older outpatients have described their experience with UI as embarrassing and producing significant interference with daily lives. 10 Persons with UI may be anxious about not having ready access to a toilet and fearful of a urinary accident in public. For these reasons, depression and anxiety symptoms may be associated with UI.
Previous studies have suggested an association between UI and depression. However, previous investigations have been limited in several ways: small sample size (n = 100; 11 n = 117; 12 n = 110 13 ), selection bias due to recruitment from specialized health service settings, 12,14–16 nonstandard measures of psychological status, 17 use of a predominantly Caucasian sample, 9 and inadequate comparison groups. 15 Furthermore, the evidence for an association between UI and emotional distress has been conflicting. Herzog et al. found that UI was only weakly related to psychological well-being. 17 Chiara et al. found no signs of depression in female patients with urge incontinence, stress incontinence, or mixed incontinence. 14 Dugan et al. found depressive symptoms were more likely to be reported by adults with UI, and the degree of depression was linked to the severity of incontinence. 9 Our investigation differs in several ways from prior work on the relationship between UI and psychological distress. Our sample is from a large ethnically diverse sample of community-dwelling adults. In addition, we have 13-year prospective data on psychological distress and information on change in activities or routines specifically related to UI.
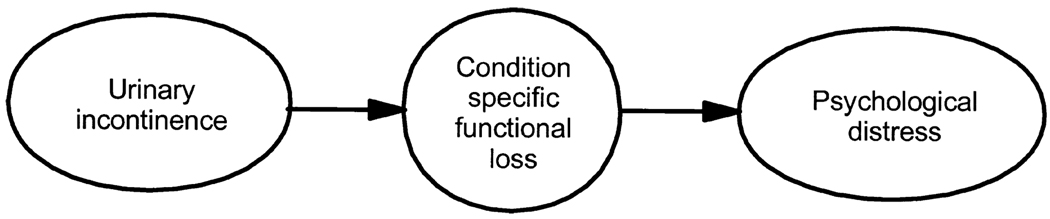
We hypothesized that condition-specific functional status may be a mediator in the relationship between UI and psychological distress (see Figure 1). UI can lead to a loss in functioning, which may limit social and physical activities. 18 Some of this condition-specific functional loss may be self-imposed by older persons to help manage their condition, such as going out only for short trips. 19 Withdrawal from activities, even if self-imposed, may lead to feelings of loss of control and diminished life satisfaction. Previous research has suggested that condition-specific functional loss accompanying low vision, 20 arthritis, 21 or other chronic medical conditions 22 was associated with depression. However, no previous research has examined whether persons with UI associated with condition-specific functional loss are more likely to have depressive symptoms than persons who do not report condition-specific functional loss due to UI.
Figure 1.
Conceptual model for the hypothesis that functional loss mediates the relationship between urinary incontinence and psychological distress.
The purpose of this paper was to examine the association between UI and psychological distress among community-dwelling older adults. In particular, our specific aims were: to determine whether there is an association between UI and psychological distress, to examine how loss of condition-specific functioning associated with UI modifies the relationship between UI and psychological distress, and, in the persons with UI, to assess whether persistent psychological distress increases vulnerability to condition-specific functional loss from UI.
METHODS
The Epidemiologic Catchment Area Program
The Epidemiologic Catchment Area (ECA) Program was a survey of psychiatric disorders in the general population between 1980 and 1984 at five university-based sites in the United States. The target population for the Baltimore site of the ECA was the household residents of East Baltimore, a population of 175,000 adult residents. Blocks were selected at random based on the expected number of households. Next, a random sample of households was selected and one individual was randomly selected from each household to respond to the survey. In addition, to oversample older people at the Baltimore site, all persons in a household aged 65 and older were interviewed. ECA data consists of highly structured interviews of community-dwelling adults. Each interview was conducted in a private place, usually the respondent’s home. All interviewers were lay professionals who received specific training in all assessments. Details of the study design of the ECA have been published elsewhere. 23
The Baltimore ECA Follow-Up
In Baltimore and the other ECA sites, the initial cohort aged 18 and older at their first interview was reinterviewed 1 year later. At the Baltimore site, an initial cohort of 3,481 respondents was interviewed in 1981, and then an attempt to retrace and reinterview the entire cohort was made from 1993 to 1996 (most interviews were conducted in 1994). The target population at baseline was 175,211 adult household residents of east Baltimore. In 1981, 4,238 residents aged 18 and older were probabilistically designated; 3,481 (82%) completed interviews and were the target sample for follow-up interviews in 1994. During the follow-up, 848 respondents died, the addresses of 415 could not be established, 2,218 persons were located, and 1,920 (87%) participated in the interviews. 24,25 The participants gave permission for future follow-up at the baseline interview, and the Committee on Human Research of the Johns Hopkins University School of Hygiene and Public Health reviewed and approved the protocol. Our analysis was also reviewed and approved by the Institutional Review Board at the University of Pennsylvania. For this investigation, we selected adults who were aged 50 and older during the 1993 to 1996 interviews. Information on UI was available for the 1993 to 1996 interviews only.
Urinary Incontinence
Participants were asked “Have you ever had any difficulty in controlling your water, that is, losing your urine or having trouble getting to the bathroom on time?” Persons were classified as having UI if they reported any uncontrolled urine loss in the 12 months before the interview and as continent if they denied uncontrolled urine loss within the 12 months before the interview.
UI and Condition-Specific Functional Loss
Condition-specific functional loss associated with UI was assessed by four questions in the interview. Participants were asked if, because of their UI, any of the following applied to them: “avoiding social gatherings, visiting friends, or going to church,” “avoiding travel,” “not going shopping,” and “avoiding physical activities.” UI was the only condition assessed in the ECA in which condition-specific functional loss was assessed. We considered persons with a positive response to any of these questions as having condition-specific functional loss due to UI.
Psychological Status
Psychological status was assessed using the General Health Questionnaire (GHQ). 26,27 The GHQ is a widely used method of assessing psychological distress in clinical and community settings. The GHQ consists of four categories measuring somatic symptoms, anxiety and insomnia, social dysfunction, and severe depression. The conventional method for scoring the GHQ was used, in which a score of 4 or more indicated psychological “caseness,” consistent with previous studies from the ECA. 28,29 The GHQ does not render a specific psychiatric diagnosis but helps identify persons who may have a psychiatric disorder. When compared with a standardized psychiatric examination in the Baltimore ECA, the GHQ was about 80% specific and 75% sensitive for depression. 28 The GHQ as employed in the ECA consists of 20 items; use in the ECA has been described in detail elsewhere. 28 In addition, we wished to examine how the pattern of psychological distress assessed at baseline (1981) and at follow-up (1994) related to a report of condition-specific functional loss due to UI in 1994 (a strategy consistent with another analysis from the ECA 21). Participants were sorted into one of four groups based on their pattern of GHQ scores assessed in 1981 and 1994. Grouped in this way, participants were considered to have no psychological distress if their GHQ scores were less than 4 at both interviews, remitted psychological distress if their GHQ scores were 4 or more in 1981 but less than 4 in 1994, new psychological distress if their GHQ scores were less than 4 in 1981 and 4 or more in 1994, and persistent psychological distress if their GHQ scores were 4 or more at both interviews. Given the timing of assessments, we recognized that we were limited in our ability to make strong temporal statements about the relationship of condition-specific functional loss associated with UI and psychological distress, and we will address the implications of the study design in our discussion of limitations. Nevertheless, we reasoned that, if condition-specific functional loss associated with UI was more highly associated with new or persistent psychological distress over the course of the 13-year follow-up when compared with persons with remitted or no significant psychological distress, this would be evidence that the conditions were closely related in time.
Medical Conditions
The participants were asked whether they had ever had any of the following conditions: diabetes mellitus, heart trouble, arthritis, stroke, or cancer. Based on follow-up interviews, a positive response to any of these conditions was considered a medical comorbidity.
Other Covariates
Activities of daily living (ADLs) were assessed in relation to standard survey items on getting to bed by oneself, dressing and undressing, taking a bath or shower, using the toilet, and using a knife or fork to cut up food. Instrumental activities of daily living (IADLs) were assessed in terms of preparing meals, cleaning house, using the telephone, keeping track of money and bills, and being able to get together with friends. Individuals were characterized as having ADL or IADL impairment at follow-up if they were unable to perform at least one activity without help, consistent with previous ECA reports. 29 Cognitive status was assessed with the Mini-Mental State Examination (MMSE). 30 MMSE scores were analyzed as a continuous variable.
Study Sample
Three thousand four hundred eighty-one persons were interviewed in the household survey in Baltimore in 1981; of these, 1,920 were contacted and interviewed during 1993 to 1996. 25 Our study sample included 820 persons aged 50 and over who had complete information on UI. Thirty-five people were excluded because they did not know whether they had been incontinent in the past year, and six were excluded because of missing GHQ scores, leaving a sample size of 781 for this analysis.
Analytic Strategy
Data analysis was performed using STATA 6.0 for Windows (STATA Corporation, College Station, TX). The analytic plan proceeded in three phases. The first phase consisted of calculating descriptive statistics for the subjects with and without UI and the appropriate means and frequencies for each variable. Comparisons between groups of participants were made using chi-square or t tests as appropriate for categorical data or differences in means. We then examined bivariate associations between GHQ scores and other important variables. The second phase consisted of carrying out multivariate analyses using the 1993 interview data. All multivariate models were adjusted for age, gender, ethnicity, chronic health conditions, and education level by including them in the final models. Based on bivariate associations with our dependent variable, GHQ score, we included risk factors in multivariate models that we found were associated at the P < .20 level. Our measure of association was the odds ratio. We used a back-wards stepwise regression approach to obtain a parsimonious model, withdrawing the least significant variables first. Covariates were removed from further models if the value of the likelihood ratio test had a P -value > .05. We examined only biologically relevant interaction terms such as gender, IADL impairment, and chronic medical conditions. We employed separate multivariate logistic regression models to assess the relationship of psychological distress to UI and UI with and without condition-specific functional loss. The third and last phase consisted of using multivariate logistic regression models to examine the relationship of the pattern of GHQ scores in the 1981 and the 1993 to 1996 interviews to UI with condition-specific functional loss. Goodness-of-fit was assessed for all multivariate models using the Hosmer-Lemeshow test. 31
RESULTS
Baseline Characteristics
The mean age ± standard deviation of our study sample was 67.2 ± 10.8 (range 50–96). Five hundred two (64%) of the participants were women. The self-identified ethnic groups of the participants consisted of 540 whites (69%); 207 African Americans (27%), and 26 American Indians, Hispanics, or Asians (4%). Of all the 781 participants, 158 (20%) reported having UI during the previous year. Of persons with UI, 127 (81%) were women and 30 (19%) were men. Twenty-nine adults with UI (18%) reported condition-specific functional loss specifically related to their UI. In terms of the responses to the four questions on condition-specific functional loss secondary to UI, we found that 14 people reported one limitation, seven reported two limitations, five reported three limitations, and three reported four limitations. Sociodemographic characteristics, continence status, functional status, and presence of chronic medical conditions were compared between persons with and without psychological distress (Table 1). Respondents with psychological distress were similar in age, ethnicity, and education level to persons without psychological distress. Proportionally more women experienced psychological distress, and persons with psychological distress were more likely to have functional and cognitive impairment. Persons with psychological distress were also more likely to report the presence of heart trouble, arthritis, and stroke.
Table 1.
General Health Questionnaire (GHQ) Status by Continence Status, Sociodemographic Variables, Functional Status, and Physical Disorders Among Persons Aged 50 and Older (n = 781)
| Variable | No Psychological Distress (n = 651) |
Psychological Distress (n = 130) |
P-value* |
|---|---|---|---|
| Sociodemographic | |||
| Age in years, mean ± standard deviation | 67.0 ± 10.6 | 68.1 ± 11.8 | .274 |
| Women, n (%) | 408 (62.5) | 96 (73.9) | .014 |
| Education less than high school, n (%) | 376 (57.7) | 82 (63.1) | .261 |
| White, n (%) | 447 (68.7) | 93 (71.5) | .517 |
| Functional Status | |||
| Activities of daily living status impaired, n (%) | 11 (1.7) | 9 (6.9) | .001 |
| Instrumental activities of daily living status impaired, n (%) | 34 (5.2) | 24 (18.5) | .001 |
| Mini-Mental State Examination score, mean ± standard deviation |
27.1 ± 3.0 | 26.5 ± 3.4 | .036 |
| Chronic health conditions | |||
| Diabetes mellitus, n (%) | 100 (15.4) | 19 (14.6) | .829 |
| Heart trouble, n (%) | 160 (24.6) | 52 (40.0) | < .001 |
| Arthritis, n (%) | 329 (50.5) | 83 (63.9) | .006 |
| Stroke, n (%) | 44 (6.8) | 19 (14.6) | .003 |
| Cancer, n (%) | 75 (11.5) | 18 (13.9) | .455 |
| Urinary incontinence status | |||
| No urinary incontinence, n (%) | 530 (81.4) | 93 (71.5) | .011 |
| Incontinent, n (%) | 121 (18.6) | 37 (28.5) | .011 |
| Incontinent with any secondary condition- specific functional loss, n (%) |
17 (2.6) | 12 (9.2) | <.011 |
Note: Data gathered from the Baltimore, Maryland Epidemiologic Catchment Area Program Follow-up, 1994.
P-values given for comparison of groups with chi-square or t test, as appropriate.
UI and Psychological Distress
The association of UI and psychological distress was evaluated using multiple logistic regression. A goodness-of-fit diagnostic and plots of the deviance residuals versus fitted values predicted by the model showed that the coefficient estimates were not influenced appreciably by any one observation. ADL impairment and MMSE scores were not statistically significant in multivariate models and were dropped from further consideration. Persons with UI were more likely to have psychological distress as measured by the GHQ than were persons without UI (unadjusted odds ratio (OR) = 1.74, 95% confidence interval (CI) = 1.13– 2.68). These findings remained significant after adjusting for age, gender, ethnicity, and education (OR = 1.56, 95% CI = 1.00–2.43) but no longer achieved conventional levels of significance in the final model after adjusting for IADL impairment and chronic medical conditions (OR = 1.42, 95% CI = 0.90–2.23). Similar results were obtained when men and women were considered separately.
UI Associated with Condition-Specific Functional Loss
Additional multivariate analyses were performed that incorporated UI with and without associated condition-specific functional loss in the models. Three categories were created: no UI, UI with condition-specific functional loss, and UI without condition-specific functional loss. An overall association of these three categories and the GHQ was found (P < .001). Results for these analyses are presented in Table 2. Persons who did not report condition-specific functional loss along with UI were similar in psychological distress as measured by the GHQ to persons without UI (unadjusted OR = 1.35, 95% CI = 0.83– 2.18). However, persons with condition-specific functional loss secondary to UI were more likely to have psychological distress as measured by the GHQ than were persons without UI (unadjusted OR = 4.02, 95% CI = 1.86–8.70). These findings remained significant in the final model even after adjusting for age, gender, ethnicity, education, IADL impairment, and chronic medical conditions (OR = 3.66, 95% CI = 1.61–8.33). We also considered several potential interaction terms: gender, IADL impairment, and chronic medical conditions, but none reached the level of significance of P = .05.
Table 2.
Association Between Urinary Incontinence with and without Secondary Condition-Specific Functional Loss and Psychological Distress in Persons Aged 50 and Older (n = 781)
| Urinary Incontinence | Crude OR (95% CI) |
Adjusted*OR (95% CI) |
|---|---|---|
| With condition-specific functional loss |
4.02 (1.86–8.70) | 3.66 (1.61–8.33) |
| Without condition-specific functional loss |
1.35 (0.83–2.18) | 1.07 (0.65–1.79) |
| None | 1.00 | 1.00 |
Note: Data gathered from the Baltimore, Maryland Epidemiologic Catchment Area Program Follow-up, 1994.
Adjusted for age, education level, ethnicity, sex, instrumental activity of daily living impairment, and chronic health conditions.
OR = odds ratio; CI = confidence interval.
Pattern of Psychological Distress over the 13-Year Follow-Up
Additional multivariate analyses were performed using pattern of psychological distress as the independent variable. For these analyses, we restricted our attention to the persons who reported any UI at follow-up interviews in 1994 (n = 158). The results for these analyses are presented in Table 3. Persons with remitted psychological distress (GHQ scores ≥4 1981 and ≤4 in 1994) were not more likely to report condition-specific functional loss associated with UI than persons with no psychological distress (GHQ scores <4 at both interviews); (unadjusted OR = 1.75, 95% CI = 0.39–7.97). However, persons with new psychological distress (GHQ scores <4 in 1981 and >4 in 1994) were more likely to report condition-specific functional loss associated with UI than persons with no psychological distress (unadjusted OR = 3.20, 95% CI = 1.26–8.12). These findings remained significant in the final model after adjusting for age, gender, ethnicity, education, IADL impairment, and chronic medical conditions (OR = 2.85, 95% CI = 1.01, 7.98). In addition, an even stronger association was found for persons with persistent psychological distress (GHQ scores ≥4 at both interviews). Persons with persistent psychological distress were much more likely to report condition-specific functional loss associated with UI than persons with no psychological distress (unadjusted OR = 7.73, 95% CI = 2.57–23.28). These findings also remained significant in the final model after adjusting for age, gender, ethnicity, education, IADL impairment, and chronic medical conditions (OR = 6.55, 95% CI = 1.94–22.12).
Table 3.
Association Between Pattern of Psychological Distress and Urinary Incontinence with Secondary Condition-Specific Functional Loss in Persons Aged 50 and Older Who Reported Urinary Incontinence in 1994 (n = 158)
| Pattern of Psychological Distress | 1981 | 1994 | Crude OR (95% CI) | Adjusted* OR (95% CI) |
|---|---|---|---|---|
| Persistent | + | + | 7.73 (2.57–23.28) | 6.55 (1.94–22.12) |
| New | − | + | 3.20 (1.26–8.12) | 2.85 (1.01–7.98) |
| Remitted | + | − | 1.75 (0.39–7.97) | 1.55 (0.32–7.40) |
| None | − | − | 1.00 | 1.00 |
Note: Data gathered from the Baltimore, Maryland Epidemiologic Catchment Area Program Follow-up, 1994.
A “+” sign indicates that psychological distress was present at that interview, and a “−” sign indicates that psychological distress was not present, as assessed by the General Health Questionnaire.
Adjusted for age, education level, ethnicity, sex, instrumental activity of daily living impairment, and chronic health conditions.
OR = odds ratio; CI = confidence interval.
DISCUSSION
In this large community sample, persons with UI associated with condition-specific functional loss were found to have higher rates of psychological distress than persons with UI who did not report condition-specific functional impairment. This finding supports our original hypothesis, and the association persists even after controlling for potentially influential variables. The association between UI and psychological distress is consistent with other studies that have shown an association between UI and depressive symptoms.9,11–13,15,17 However, our study suggests that it is the condition-specific functional loss associated with the UI and not the UI itself that is most closely associated with psychological distress.
Before discussing our findings, the results must first be considered in the context of some potential study limitations. First, we did not have prospective data on the presence of UI, so we were unable to fully delineate temporal relationships between psychological distress and UI. However, we did attempt to assess whether preexisting or new psychological distress, determined using prospective data gathered 13 years earlier, was associated with increased reports of condition-specific functional loss due to UI in persons with the condition. Second, we only have a limited measure of UI. Only recently has consensus been reached on how to address UI in population-based surveys.32,33 Our measure of UI did not differentiate persons with UI from persons who were continent with symptoms of urgency or frequency that might make it difficult to get to the bathroom on time. For example, our measure did not separate incontinent persons from continent persons with symptoms of overactive bladder. Third, we did not have information on the type of incontinence (urge, stress, mixed, overflow, or functional) and were therefore unable to make any conclusions concerning different types of incontinence. For example, one study found that patients with detrusor instability and sensory urgency were more anxious than patients with other types of incontinence.34 However, we suspect that considering all types of UI together makes it more difficult to find any association with distress and may have biased our results toward the null. Fourth, there is the potential for all the sources of error associated with retrospective interview data including imperfect recall and response bias (e.g., socially desirable responding). Study data are based on self-reports, and depressed persons may overestimate disability. We attempted to mitigate these biases by limiting recall to the previous 12 months and by using available prospective data on psychological distress. Fifth, selection bias is a potential limitation because, although the initial study was based on a community sample, the follow-up data that we used consisted of all people that could be found and reinter-viewed. However, two studies based on the ECA follow-up data have shown little influence of depression at baseline on loss to follow-up.24,25
Nonetheless, despite limitations, our results deserve attention because we attempted to further characterize the relationship between UI and psychological distress, with a focus on condition-specific functional impairment specific to UI. In addition, because we examined a large ethnically diverse community-based population, the results are more generalizable to community-dwelling adults. It should also be noted that the rate of incontinence in older adults in our study was consistent with other published rates.1–3 The study provides additional evidence of the public health importance of UI and the role that psychological distress may play in associated condition-specific functional loss that occurs as a result.
The first aim of this study was to understand the extent of the association between UI and psychological distress. Our study demonstrated that although persons with UI were found to be more at risk for psychological distress, the association did not remain significant at conventional levels when functional impairment as measured by IADLs and chronic health conditions were included in the models. Our data were consistent with Herzog et al.,3 who reported that the magnitude of the relationship between UI and psychological well-being diminished when health status was taken into consideration. Therefore, the association between UI and psychological distress does not appear to be straightforward. In other words, part of the association of UI with distress might be explained by health and functional status.
The second aim was to examine how condition-specific loss of functioning associated with UI influences the relationship between UI and psychological distress. Consistent with our hypothesis, the persons with condition-specific functional loss secondary to UI were most likely to report psychological distress. In fact a positive response to any of the questions addressing how UI interferes with daily activities was the strongest predictor of psychological distress. In particular, in adults with UI, limitation of ability to enjoy daily activities and social interactions was the most important predictor of psychological distress. The implication of these findings is that inquiry regarding condition-specific functional loss secondary to UI should be conducted to identify persons most at risk for psychological distress.
The third aim was to focus on the pattern of psychological distress over the 13-year follow-up period and to determine whether persistent psychological distress based on prospective data was associated with condition-specific functional loss secondary to UI. Indeed, persistent or new psychological distress was found to be very strongly associated with the report of condition-specific functional loss secondary to UI. Specifically, persons who reported UI in 1994 with new psychological distress were about three times as likely to report condition-specific functional impairment secondary to UI than were persons who were below the threshold for psychological distress at both interviews, in 1981 and 1994. In itself, this result implies that the UI and psychological distress may be arising together. However, persons with a persistent pattern of psychological distress as assessed in 13-year prospective data were about six times as likely to report condition-specific functional impairment secondary to UI than was the comparison group without distress. Taken together, these results suggest that psychological distress plays a key role in the disablement process in older persons with UI. Persistent psychological distress may be a marker of vulnerability for lowered coping effort and increased condition-specific functional impairment. A more realistic mediation scenario posits a reciprocal relationship between depression and condition-specific functional impairment. Nevertheless, our findings support a general conceptual model, suggested for conditions other than UI such as low vision,20 arthritis,21 or other chronic medical conditions,22 that condition-specific functional impairment mediates the relationship between a chronic medical condition and psychological distress.
UI can affect many aspects of people’s lives. Our results suggest that persons with UI that interferes with their daily activities were most likely to have associated psychological distress. Regardless of the specific physical disorder, condition-specific functional loss may be the final common pathway in the development of depression by older adults with chronic illness. In addition, persistent depressive symptoms may identify those most at risk for condition-specific functional loss secondary to a chronic medical condition such as UI. According to the World Health Organization, major depression will be second only to cardiovascular disease as a worldwide cause of disability in 2020.35 An increased understanding of how depressive symptoms affect the diagnosis, treatment, and condition-specific functional impairment related to chronic medical conditions such as UI will be essential in the context of global aging if disability due to chronic illness is to be minimized.
Acknowledgments
Data analysis was supported by a Health Resources and Services Administration Faculty Development Program in Primary Care training grant (Dr. Bogner). Data gathering in 1981 was supported by the Epidemiologic Catchment Area (ECA) Program of the National Institute of Mental Health Division of Biometry and Epidemiology (MH33870). Data gathering in the Baltimore ECA Follow-up (1993/94) was supported by the National Institute of Mental Health (MH47447).
Footnotes
Presented at the Annual Meeting of the American Geriatrics Society, Chicago, Illinois, May 2001.
REFERENCES
- 1.Thom D. Variation in estimates of urinary incontinence prevalence in the community: Effects of differences in definition, population characteristics, and study type. J Am Geriatr Soc. 1998;46:473–480. doi: 10.1111/j.1532-5415.1998.tb02469.x. [DOI] [PubMed] [Google Scholar]
- 2.Mohide EA. The prevalence and scope of urinary incontinence. Clin Geriatr Med. 1986;2:639–655. [PubMed] [Google Scholar]
- 3.Herzog AR, Diokno AC, Brown MB, et al. Two-year incidence, remission, and change patterns of urinary incontinence in noninstitutionalized older adults. J Gerontol. 1990;45:M67–M74. doi: 10.1093/geronj/45.2.m67. [DOI] [PubMed] [Google Scholar]
- 4.Ouslander JG, Kane RL, Abrass IB. Urinary incontinence in elderly nursing home patients. JAMA. 1982;248:1194–1198. [PubMed] [Google Scholar]
- 5.Bhatia NN, Bergman A, Karram MM. Effects of estrogen on urethral function in women with urinary incontinence. Am J Obstet Gynecol. 1989;160:176–181. doi: 10.1016/0002-9378(89)90114-2. [DOI] [PubMed] [Google Scholar]
- 6.Benvenuti F, Caputo GM, Bandinelli S, et al. Reeducative treatment of female genuine stress incontinence. Am J Phys Med. 1987;66:155–168. [PubMed] [Google Scholar]
- 7.Fantl JA, Wyman JF, McClish DK, et al. Efficacy of bladder training in older women with urinary incontinence. JAMA. 1991;265:609–613. [PubMed] [Google Scholar]
- 8.Burgio KL, Ives DG, Locher JL, et al. Treatment seeking for urinary incontinence in older adults. J Am Geriatr Soc. 1994;42:208–212. doi: 10.1111/j.1532-5415.1994.tb04954.x. [DOI] [PubMed] [Google Scholar]
- 9.Dugan E, Cohen SJ, Bland DR, et al. The association of depressive symptoms and urinary incontinence among older adults. J Am Geriatr Soc. 2000;48:413–416. doi: 10.1111/j.1532-5415.2000.tb04699.x. [DOI] [PubMed] [Google Scholar]
- 10.Ouslander JG, Abelson S. Perceptions of urinary incontinence among elderly outpatients. Gerontologist. 1990;30:369–372. doi: 10.1093/geront/30.3.369. [DOI] [PubMed] [Google Scholar]
- 11.Walters MD, Taylor S, Schoenfeld LS. Psychosexual study of women with detrusor instability. Obstet Gynecol. 1990;75:22–26. [PubMed] [Google Scholar]
- 12.Norton KR, Bhat AV, Stanton SL. Psychiatric aspects of urinary incontinence in women attending an outpatient urodynamic clinic. BMJ. 1990;301:271–272. doi: 10.1136/bmj.301.6746.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lagro-Janssen AL, Debruyne FM, Van Weel C. Psychological aspects of female urinary incontinence in general practice. Br J Urol. 1992;70:499–502. [PubMed] [Google Scholar]
- 14.Chaira G, Piccioni V, Perino M, et al. Psychological investigation in female patients suffering from urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1998;9:73–77. doi: 10.1007/BF01982211. [DOI] [PubMed] [Google Scholar]
- 15.Macaulay AJ, Stern RS, Holmes DM, et al. Micturition and the mind: Psychological factors in the aetiology and treatment of urinary symptoms in women. BMJ (Clin Res Ed) 1987;294:540–543. doi: 10.1136/bmj.294.6571.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Macaulay AJ, Stern RS, Stanton SL. Psychological aspects of 211 female patients attending a urodynamic unit. J Psychosom Res. 1991;35:1–10. doi: 10.1016/0022-3999(91)90002-6. [DOI] [PubMed] [Google Scholar]
- 17.Herzog AR, Fultz NH, Brock BM, et al. Urinary incontinence and psychologic distress among older adults. Psychol Aging. 1988;3:115–121. doi: 10.1037//0882-7974.3.2.115. [DOI] [PubMed] [Google Scholar]
- 18.Grimby A, Milsom I, Molander U, et al. The influence of urinary incontinence on the quality of life of elderly women. Age Ageing. 1993;22:82–89. doi: 10.1093/ageing/22.2.82. [DOI] [PubMed] [Google Scholar]
- 19.Johnson TM, II, Kincaid JE, Bernard SL, et al. Self-care practices used by older men and women to manage urinary incontinence: Results from the national follow-up survey on self-care and aging. J Am Geriatr Soc. 2000;48:894–902. doi: 10.1111/j.1532-5415.2000.tb06885.x. [DOI] [PubMed] [Google Scholar]
- 20.Rovner BW, Zisselman PM, Shmuely-Dulitzki Y. Depression and disability in older people with impaired vision: A follow-up study. J Am Geriatr Soc. 1996;44:181–184. doi: 10.1111/j.1532-5415.1996.tb02436.x. [DOI] [PubMed] [Google Scholar]
- 21.Armenian HK, Pratt LA, Gallo JJ, et al. Psychopathology as a predictor of disability: A population-based follow-up study in Baltimore, Maryland. Am J Epidemiol. 1998;148:269–275. doi: 10.1093/oxfordjournals.aje.a009635. [DOI] [PubMed] [Google Scholar]
- 22.Ormel J, Kempen GIJM, Penninx BWJH, et al. Chronic medical conditions and mental health in older people: Disability and psychosocial resources mediate specific mental health effects. Psychol Med. 1997;27:1065–1077. doi: 10.1017/s0033291797005321. [DOI] [PubMed] [Google Scholar]
- 23.Robins LN, Regier DA. Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. New York, NY: Free Press; 1991. [Google Scholar]
- 24.Eaton WW, Anthony JC, Tepper S, et al. Psychopathology and attrition in the Epidemiologic Catchment Area surveys. Am J Epidemiol. 1992;135:1051–1059. doi: 10.1093/oxfordjournals.aje.a116399. [DOI] [PubMed] [Google Scholar]
- 25.Badawi M, Eaton WW, Myllyluoma J, et al. Psychopathology and attrition in the Baltimore ECA 15-year follow-up 1981–1996. Soc Psychiatry Psychiatr Epidemiol. 1999;34:91–98. doi: 10.1007/s001270050117. [DOI] [PubMed] [Google Scholar]
- 26.Goldberg DP. The Detection of Psychiatric Illness by Questionnaire. London, England: Oxford University Press; 1972. [Google Scholar]
- 27.Goldberg DP, Rickels K, Downing R, et al. A comparison of two psychiatric screening tests. Br J Psychiatry. 1976;129:61–67. doi: 10.1192/bjp.129.1.61. [DOI] [PubMed] [Google Scholar]
- 28.Samuels JF, Nestadt G, Anthony JC, et al. The detection of mental disorders in the community setting using a 20-item interview version of the General Health Questionnaire. Acta Psychiatr Scand. 1994;891:14–20. doi: 10.1111/j.1600-0447.1994.tb01479.x. [DOI] [PubMed] [Google Scholar]
- 29.Gallo JJ, Rabins PV, Lyketsos CG, et al. Depression without sadness: Functional outcomes of nondysphoric depression in later life. J Am Geriatr Soc. 1997;45:570–578. doi: 10.1111/j.1532-5415.1997.tb03089.x. [DOI] [PubMed] [Google Scholar]
- 30.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 31.Hosmer DW, Lemeshow S. Applied Logistic Regression. New York, NY: John Wiley & Sons; 1989. [Google Scholar]
- 32.Khoury S, Cockett A, Aso Y, et al. International consultation on urological diseases: A decade of progress. Prostate. 2000;45:194–199. doi: 10.1002/1097-0045(20001001)45:2<194::aid-pros14>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 33.Temml C, Haidinger G, Schmidbauer J, et al. Urinary incontinence in both sexes: Prevalence rates and impact on quality of life and sexual life. Neurourol Urodynam. 2000;19:259–271. doi: 10.1002/(sici)1520-6777(2000)19:3<259::aid-nau7>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 34.Wyman JF, Harkins SW, Choi SC, et al. Psychosocial impact of urinary incontinence in women. Obstet Gynecol. 1987;70:378–381. [PubMed] [Google Scholar]
- 35.Murray CJL, Lopez AD. The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Cambridge, MA: Harvard University Press; 1996. [Google Scholar]