Abstract
Although socioeconomic status is a major contributing factor to health disparities, the mechanisms through which socioeconomic status influences health remain unclear. The purpose of the present study was to evaluate an a priori conceptual model of the pathways between socioeconomic status and modifiable health risk factors in a sample of 399 African Americans seeking smoking cessation treatment. A latent variable modeling approach was utilized to characterize the interrelationships among socioeconomic status, neighborhood disadvantage, social support, negative affect/perceived stress, and three specific modifiable risk factors (i.e., overweight/obesity, insufficient physical activity, at-risk drinking). Findings indicated that neighborhood disadvantage, social support, and negative affect/perceived stress function as pathways linking socioeconomic status and modifiable risk factors among African American smokers, and negative affect/perceived stress appears to play a key mediating role. Policy, community, and individual-level interventions may attenuate the impact of socioeconomic status on health by targeting intermediate psychosocial, environmental, and behavioral pathways.
Keywords: Socioeconomic Status, African American, Smoking, Obesity, Physical Activity, Alcohol
African Americans (AAs) experience profound health disparities related to numerous conditions including cardiovascular disease, cancer, and diabetes (Fagan et al., 2007; Mensah et al., 2005; Miller et al., 2004), and they suffer disproportionately from the adverse consequences of certain modifiable risk factors. For example, AAs have the highest rates of tobacco-related morbidity and mortality, despite smoking fewer cigarettes per day and having a later onset of smoking than Caucasians (e.g., the lung cancer mortality rate is nearly 40 percent higher among AA than Caucasian males; for a review see Fagan, et al., 2007). Unfortunately, the prevalence of many modifiable risk factors is greater among AAs relative to other racial/ethnic groups (Hutchinson et al., 1997; Kendzor, Costello, et al., 2008; Sharma et al., 2004). Risk factors including obesity, insufficient physical activity, and alcohol consumption have each been independently linked with increased mortality (Di Castelnuovo et al., 2006; Katzmarzyk et al., 2003), and confer additional health risks when combined with smoking (Blot et al., 1988; Freedman et al., 2006; Marrero et al., 2005). Plausibly, the presence of modifiable risk factors in addition to smoking may contribute to tobacco-related health disparities (Fernander et al., 2007). Thus, AA smokers who also manifest other health risk factors represent a population at extraordinarily high risk for adverse health consequences and health disparities.
A key contributing factor to the health disparities experienced by AAs is socioeconomic status (SES). Although some research suggests that AAs suffer poorer health than Caucasians within similar socioeconomic classes, the class differentials in health appear to be substantially larger than the race differentials (Navarro, 1990). Overall, AAs have a much lower socioeconomic status than Caucasians in the United States (Ostrove & Feldman, 1999; U.S. Census Bureau, 2007), and numerous studies suggest that smoking, heavy drinking, overweight/obesity, and low levels of physical activity are more prevalent among individuals of lower SES (Lantz et al., 1998; Lynch et al., 1997). Prospective research has indicated that low SES in childhood predicts an increased likelihood of modifiable risk factors in adulthood (Melchior et al., 2007). Thus, it is not surprising that low SES is also associated with greater risk for cardiovascular disease, lung cancer, and all-cause mortality (Adler & Rehkopf, 2008; Fagan et al., 2007; Lantz et al., 1998). Although low SES clearly contributes to the disparities in health and modifiable risk factors experienced by AAs relative to other racial/ethnic groups, there are few studies that have examined the influence of SES on modifiable health risk factors or on the mechanisms underlying these relationships in AA samples.
SES is a multi-dimensional construct that has been measured in a variety of ways across studies. Education, income, and occupational status are perhaps the most commonly used indicators of SES, and each of these measures has specific strengths and limitations (for a discussion see Braveman et al., 2005; Shavers, 2007). For example, education is relatively stable in adulthood and is predictive of having a more favorable occupation, income, or neighborhood. On the other hand, educational levels may not be equivalent across cultures or countries of origin. Thus, researchers have recommended the inclusion of multiple measures of SES in research studies, and have suggested that SES measures be chosen based upon their conceptual links with the outcomes of interest (Braveman et al., 2005; Shavers, 2007). Notably, the potential usefulness of other less commonly used measures of SES, such as economic hardship and subjective perceptions of social position, has also been acknowledged (Braveman et al., 2005).
Several conceptual models have described plausible pathways between SES and modifiable risk factors in the general population (Adler & Ostrove, 1999; Gallo & Matthews, 2003). Adler and Ostrove (1999) described a model in which SES is hypothesized to have a direct influence on environmental resources/constraints (e.g., physical and social environments, access to resources) as well as on affect/cognition (e.g., negative affect), that in turn, are hypothesized to influence modifiable risk factors. Gallo and Matthews (2003) proposed a model in which SES is hypothesized to directly influence the probability of exposure to harm/threat (e.g., residence in a disadvantaged neighborhood), as well as reserve capacity, an individual's reservoir of tangible, interpersonal, and intrapersonal resources (e.g., social support). Exposure to threat/harm and an individual's reserve capacity are each hypothesized to have a direct influence on negative emotion/cognition and modifiable risk factors. Overall, the models are similar with the notable exception that SES is hypothesized to have a direct influence on negative affect in one model (Adler & Ostrove, 1999), and only an indirect influence on negative affect in the other model (Gallo & Matthews, 2003).
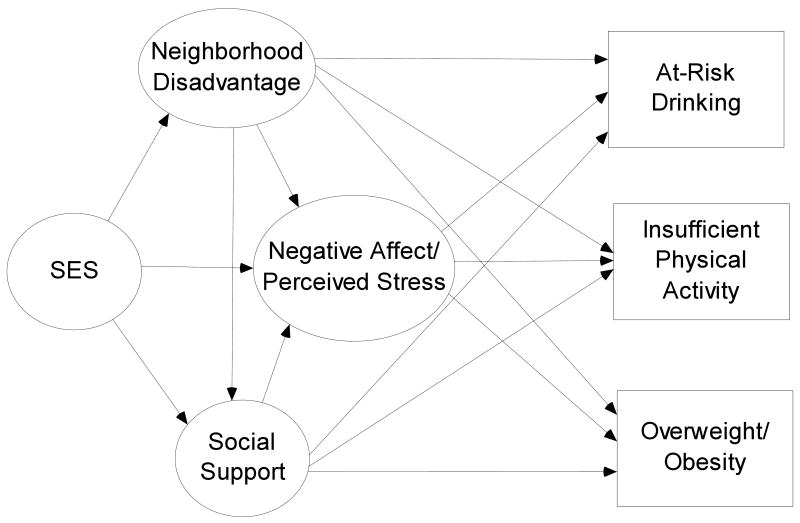
Figure 1 shows one potential operationalization of these models, and includes measures of SES, neighborhood disadvantage, social support, negative affect/perceived stress, and specific risk factors. SES is hypothesized to influence neighborhood disadvantage (i.e., environmental resources and exposure to threat/harm), social support (i.e., reserve capacity), and negative affect/perceived stress. In turn, greater neighborhood disadvantage, lower social support, and greater negative affect/perceived stress are hypothesized to influence the likelihood of insufficient physical activity, at-risk drinking, and overweight/obesity. Thus, SES is posited to influence health risk factors, in part, through its impact on neighborhood disadvantage, social support, and negative affect/perceived stress. Each of the individual links among constructs in the model is supported by previous research, although little is known about these relationships in AA smokers and other high risk populations.
Figure 1.
Initial conceptual model of the pathways between socioeconomic status and modifiable risk factors.
Low SES is associated with elevated negative affect (Lincoln et al., 2007; Mirowsky & Ross, 2001), which is linked with behavioral factors that increase the risk of disease (e.g., Goodwin, 2003; Hasin et al., 2005; Simon et al., 2006). In addition, recent evidence suggests that SES indirectly influences the total number of modifiable risk factors among AA smokers, in part through increased negative affect (Kendzor, Cofta-Woerpel et al., 2008). Although the specific mechanisms linking negative affect and modifiable risk factors remains unclear, possible explanations might include excessive consumption of alcohol to attenuate negative affect, affect-related increases in appetite that contribute to obesity, and affect-related decreases in energy that discourage physical activity.
Disadvantaged environments may influence modifiable health risk factors directly via specific neighborhood characteristics that facilitate or discourage healthful behaviors (e.g., limited access to parks/trails, limited availability of nutritious foods, high density of alcohol/tobacco advertising), and indirectly through increased exposure to threatening or stressful situations that increase negative affect (e.g., crime, lack of social cohesion; Adler & Ostrove, 1999; Gallo & Matthews, 2003). Consistent with these hypotheses, studies have linked various measures of neighborhood disadvantage (e.g., neighborhood problems, neighborhood social cohesion) with modifiable risk factors (Echeverria et al., 2008; Mujahid et al., 2008). Not surprisingly, neighborhood disadvantage is associated with negative affect (Cutrona et al., 2005; Echeverria et al., 2008; Galea et al., 2007), and there is evidence that negative affect may mediate the relationship between neighborhood disadvantage and modifiable risk factors (Gallo & Matthews, 2003; Hill & Angel, 2005). For example, Hill and Angel (2005) reported that the relationship between residing in a disadvantaged neighborhood and heavy drinking was mediated by negative affect. Overall, the evidence suggests that neighborhood characteristics have both direct and indirect effects on modifiable risk factors.
Social support has been conceptualized as one component of reserve capacity (Gallo & Matthews, 2003) and as an environmental resource (Adler & Ostrove, 1999). Inadequate reserve capacity and/or environmental resources are hypothesized to increase the negative impact of stressors and challenges faced by individuals with low SES (Adler & Ostrove, 1999; Gallo & Mathews, 2003; Vilhjalmsson, 1993). Supporting this hypothesis, low social support is associated with greater negative affect (Peirce et al., 2000; Ross & Mirowsky, 1989; Turner & Lloyd, 1999; Vilhjalmsson, 1993), and a variety of modifiable health risk factors (Delva et al., 2006; Strine et al., 2008; Wendel-Vos et al., 2007). Further, the evidence indicates that social support functions as a mediator of the relationship between SES and modifiable risk factors (Cerin & Leslie, 2008; Lincoln et al., 2005), and also of the relationship between SES and negative affect (Turner & Lloyd, 1999).
Although a model of the relationships between SES, negative affect, and the likelihood of engaging in multiple modifiable risk factors has been evaluated in previous research (Kendzor, Cofta-Woerpel, et al., 2008), the purpose of the present study was to evaluate a conceptual model of multiple mediating pathways between SES and single modifiable risk factors (i.e., insufficient physical activity, overweight/obesity, at risk drinking) in a population that experiences profound health disparities (i.e., AA smokers). The model characterizes the roles of neighborhood disadvantage, social support, and negative affect/perceived stress among AA smokers as illustrated in two previously hypothesized theoretical models (i.e., Adler & Ostrove, 1999; Gallo & Matthews, 2003). Specifically, 1) SES was hypothesized to directly influence neighborhood disadvantage, social support, and negative affect/perceived stress, 2) neighborhood disadvantage was hypothesized to directly influence social support, negative affect/perceived stress, and each of three modifiable risk factors (i.e., overweight/obesity, insufficient physical activity, at-risk drinking, 3) social support was hypothesized to directly influence negative affect/perceived stress and each modifiable risk factor, and finally, 4) negative affect/perceived stress was expected to have a direct influence on each modifiable risk factor (see Figure 1).
Method
Participants
Data for the current study were collected as part of a randomized clinical trial designed to determine the efficacy of a smoking cessation treatment that utilized palmtop computers and was targeted specifically at AA smokers. Individuals were eligible to participate if they were AA, smoked five or more cigarettes per day for at least 12 months, produced expired carbon monoxide levels of ≥ eight parts per million, were willing to quit smoking within the next two weeks, possessed a functioning home telephone number, had a permanent home address, and were able to understand English at a sixth grade literacy level. Individuals were excluded from the study if they reported regular use of tobacco products other than cigarettes, were using pharmacological smoking cessation treatments other than the nicotine patches supplied by the study, reported that the nicotine patch was medically contraindicated, or were pregnant or lactating. Participant recruitment and flow through the study protocol are reported elsewhere (Kendzor, Cofta-Woerpel et al., 2008).
Procedure
Participants enrolled in the parent study were randomly assigned to either a standard smoking cessation treatment that included the nicotine patch, culturally sensitive self-help materials, and individual counseling, or the standard treatment supplemented with treatment delivered via palmtop computer (Hewlett Packard iPAQ 1935 Pocket PC). All study procedures were approved by the Institutional Review Board of the University of Texas M. D. Anderson Cancer Center. Informed consent was obtained from all participants. All data used in the present study were collected prior to smoking cessation and treatment initiation within the larger smoking cessation study.
Measures
Tobacco Use
The Tobacco History Questionnaire is a self-report measure of years smoking and daily smoking rate. Participants who smoked < 20 cigarettes per day were considered light/moderate smokers and those who smoked ≥ 20 cigarettes per day were considered heavy smokers.
Socioeconomic Status/Demographic Information
The Demographic Information Questionnaire is a self-report measure of demographic (i.e., age, gender, and marital status) and socioeconomic characteristics. Education included two categories: 1) those that completed ≤ high school and 2) those that completed ≥ some college. Annual Household Income included three categories: 1) < $10,000, 2) $10,000-$19,999, and 3) ≥ $20,000. Employment categories included: 1) not employed (unemployed, retired, disabled), and 2) employed (full-time or part-time). The Financial Strain questionnaire was adapted from the Economic Strain Model (Pearlin et al., 1981) to assess the degree to which it was financially difficult for participants to afford the necessities (e.g., food, clothing, housing) and items or activities that might be considered optional (e.g., furniture, leisure activities). Items were rated on a scale from one to three (i.e., no difficulty, some difficulty, great difficulty). Total scores may range from 8 to 24, with higher scores indicating greater financial strain.
Neighborhood Disadvantage
The Neighborhood Vigilance scale is a self-report measure of vigilance for threat within an individual's neighborhood (John D. and Catherine T. MacArthur Research Network on Socioeconomic Status and Health, 1999). Items are rated on a five-point Likert scale, and scores range from 5 to 30. Higher scores indicate greater vigilance for threat. The Neighborhood Problems scale is a self-report measure of problems such as vandalism, litter, and traffic within a neighborhood (Steptoe & Feldman, 2001). Scores range from 10 to 30, with higher scores indicating greater neighborhood problems. The Social Cohesion and Trust scale is a self-report measure of beliefs about an individual's neighbors (e.g., neighbors' willingness to help, trustworthiness, values; Sampson et al., 1997). All items were measured on a five-point Likert scale, and scores ranged from 5 to 25. Higher scores suggest greater neighborhood social cohesion and trust.
Social Support
The Interpersonal Support Evaluation List (ISEL-12; Cohen & Hoberman, 1983) is a 12-item self-report measure of perceived availability of social support that contains three subscales. The Tangible Support subscale measures the perceived availability of material aid (e.g., able to borrow money if needed), the Belonging subscale measures the perceived availability of others' with whom one may engage in activities, and the Appraisal subscale measures the perceived availability of others with whom one can talk about problems. Items are rated on a four-point scale, and scores range from 4 to 16 on each subscale. Higher scores indicate greater social support.
Negative Affect/Perceived Stress
The Center for Epidemiological Studies Depression (CES-D) questionnaire was administered to measure depressive symptoms (Radloff, 1977). Items are rated on a four-point scale, and total scores range from 0 to 60. Scores of ≥ 16 indicate clinically significant distress. The Positive and Negative Affect Schedule (PANAS) is a self-report measure on which participants rate the degree to which each of 20 adjectives reflect their mood during the past seven days (Watson et al., 1988). The measure is comprised of separate positive affect and negative affect subscales. Items are rated on a five-point Likert scale, and scores range from 10 to 50 on each subscale. Higher scores indicate greater positive or negative affect. The Perceived Stress Scale – Short Version (PSS) is a self-rating scale of perceived stress level during the past week (Cohen et al., 1983). Items are rated on a five-point Likert scale, and total scores range from 0 to 16. Higher scores indicate greater perceived stress.
Overweight/Obesity
Weight status was determined based on height and weight measurements, which were converted to body mass index (BMI; kg/m2). Participants with a BMI ≥ 25 were considered overweight/obese.
Insufficient Physical Activity
The International Physical Activity Questionnaire – Short Format (IPAQ) is a self-report questionnaire that measures the amount of time spent in moderate activity, vigorous activity, and walking during the past seven days (Craig et al., 2003). Weekly minutes spent engaging in each type of activity were multiplied by the corresponding metabolic equivalent (MET) value, and MET minutes were summed to arrive at the total weekly MET minutes spent in physical activity. Physical activity categories (low, moderate, high) were assigned based on total weekly MET minutes, the number of days per week engaged in physical activity, and the amount of time spent in each type of physical activity (see Guidelines for data processing and analysis of the IPAQ). Individuals were considered insufficiently active if they were categorized as having low activity during the previous week.
At-Risk Drinking
The Patient Health Questionnaire (PHQ) – Alcohol Abuse/Dependence Scale is a self-report questionnaire used to indicate probable abuse or dependence on alcohol (Spitzer et al., 1999). The first item assesses current alcohol consumption, and any positive response on the subsequent items suggests probable alcohol abuse or dependence. The Alcohol Quantity and Frequency Questionnaire is a self-report measure of average alcohol consumption on each day of the week over the last 30 days (Sobell & Sobell, 2003). Average daily alcohol consumption was summed to determine average weekly consumption of alcohol. In addition, the measure assesses the number of binge drinking episodes (i.e., five or more drinks on one occasion) during the past three months. At-risk drinking (USDHHS, 2007) was confirmed if any of the following criteria were met: 1) participant was male and consumed an average of > 14 drinks per week, 2) participant was female and consumed an average of > seven drinks per week, 3) participant consumed ≥ five drinks on at least one occasion during the previous three months, or 4) participant had probable alcohol abuse or dependence as indicated by the PHQ Alcohol Abuse/Dependence Scale.
Analytic Plan
A model of specific pathways between SES and modifiable health risk factors was evaluated with Mplus software (version 5.1) using a latent variable modeling approach. Four latent variables (i.e., SES, neighborhood disadvantage, social support, negative affect/perceived stress) were included in the model as predictors of three modifiable risk factors (i.e., insufficient physical activity, at-risk drinking, and overweight/obesity). The SES latent variable was comprised of the standard measures of SES including education, income, and employment status. In addition, financial strain was included as a measure of economic hardship, which was not necessarily captured by the other SES measures. The Neighborhood Disadvantage latent variable included measures of Neighborhood Problems, Social Cohesion and Trust, and Neighborhood Vigilance. The social support latent variable included the three subscales of the ISEL-12 (i.e., Tangible Support, Belonging, Appraisal). Finally, the negative affect/perceived stress latent variable was comprised of the CES-D, PANAS negative affect, and PSS. Each health risk variable was dichotomized in order to reflect the point at which a the risk factor may warrant intervention (e.g., normal weight vs. overweight/obesity).
Most of the variables in the model were treated as continuous, although employment status, education level, income level, and each of the three modifiable risk factors were specified as categorical variables. Given the inclusion of some categorical variables, mean and variance adjusted weighted least squares (WLSMV) estimation was utilized to evaluate the model. Although weighted least squares estimation typically requires very large sample sizes, there is evidence that the WLSMV estimator offered in the Mplus software package produces accurate test statistics and parameter estimates with more moderate sample sizes (e.g., 150-200 participants in a model that includes 10-15 indicators; see Brown, 2006). After the initial model was tested, pathways between variables were successively deleted based on the strength of their association with other variables (i.e., weakest paths were deleted first) until a final model was generated that was both a good fit for the data and included only statistically significant pathways. The pathways in the final model were tested within each gender group and compared to identify gender differences in the relationships among variables, and to determine whether the model was a good fit among both AA males and females.
Results
Participant Characteristics
A total of 399 AA smokers (50.9% female) participated in the study. The mean age of the participants was 42.42 (±9.75) years, and 21.6% were married or living with a significant other. A total of 51.8% of participants had ≤ a high school education, and 60.4% were not employed (i.e., unemployed, retired, disabled). A total of 48.3% reported an annual household income of < $10,000, 17.4% reported an annual income of $10,000-$19,999, and 34.4% reported an annual income of ≥ $20,000. A total of 48.3% of participants scored ≥ 16 on the CES-D suggesting clinically significant distress. Participants smoked an average of 20.56 (±12.17) cigarettes per day for 21.49 (±10.76) years, and 58.8% of participants were heavy smokers.
Participants had an average BMI of 29.40 (±7.32), and 69.2% were within the overweight/obese range of BMI. A total of 31.6% of participants reported insufficient physical activity during the previous week as measured by the IPAQ. Participants consumed an average of 9.75 (±20.01) alcoholic beverages per week during the previous month, and 26.4% were considered heavy drinkers (i.e., > 14 drinks per week for males; > 7 drinks per week for females). Participants engaged in an average of 2.38 (±5.69) binge drinking episodes during the previous three months, with 44.7% of participants reporting ≥ one episode of binge drinking. A total of 26.8% of participants met criteria for probable Alcohol Abuse/Dependence as assessed by the PHQ, and 51.8% met the study criteria for at-risk drinking. Consistent with previous research in AA samples (Seale, Davis-Smith, & Okosun, 2006; Wang & Beydoun, 2007; Whitt-Glover, Taylor, Heath, & Macera, 2007), males were less likely to be overweight/obese or insufficiently active and more likely to engage in at-risk drinking than females. No gender differences were noted in age, education, employment status, marital status, cigarettes smoked per day, or years of smoking. Detailed participant characteristics by gender are presented elsewhere (see Kendzor, Cofta-Woerpel, et al., 2008). Means and standard deviations for each of the study questionnaires are presented in Table I.
Table I.
Descriptive statistics for study questionnaires.
| Mean (±SD) | Possible Range | |
|---|---|---|
| Financial Strain | 17.35 (±4.30) | 8-24 |
| Neighborhood Problems | 16.42 (±4.51) | 10-30 |
| Social Cohesion and Trust | 15.76 (±3.68) | 5-25 |
| Neighborhood Vigilance | 17.65 (±4.25) | 5-30 |
| Tangible Supporta | 12.05 (±2.83) | 4-16 |
| Belonging a | 12.10 (±2.61) | 4-16 |
| Appraisal a | 12.09 (±3.00) | 4-16 |
| Depression b | 16.77 (±11.72) | 0-60 |
| Negative Affect c | 20.31 (±8.78) | 10-50 |
| Perceived Stress | 6.31 (±3.14) | 0-16 |
Note: No differences were found between gender groups on any of the study questionnaires
Measured with the Interpersonal Support Evaluation List (ISEL)
Measured with the Center for Epidemiologic Studies Depression (CES-D)
Measured with the Positive and Negative Affect Schedule (PANAS)
Latent Variable Model
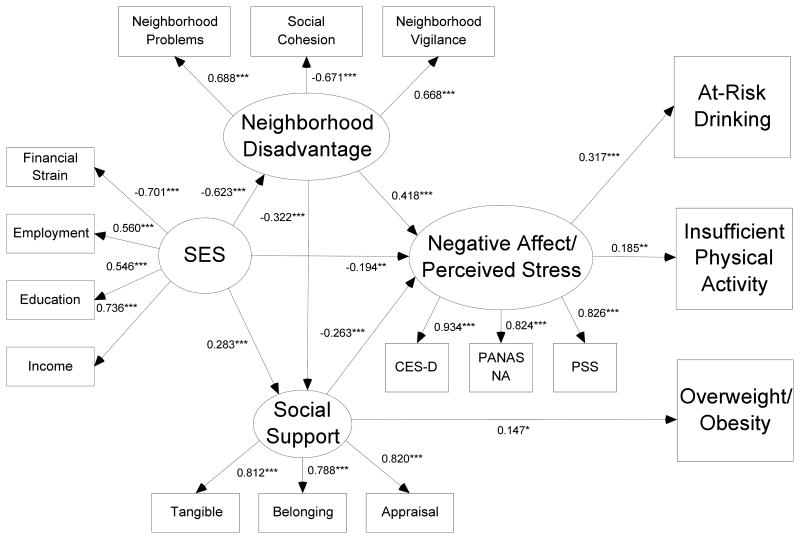
WLSMV estimation for the initial model (see Figure 1) yielded the following model fit values: χ2(47) = 115.918, p < .001; Root Mean Square Error of Approximation (RMSEA) = .061, Tucker-Lewis index (TLI) = .944, Comparative Fit Index (CFI) = .868, and Weighted Root Mean Square Residual (WRMR) = .793. WLSMV estimation for the final model (after deletion of the non-significant paths) yielded the following improved model fit values: χ2(47) = 98.15, p < .001; RMSEA = .052, TLI = .958, CFI = .902, and WRMR = .801. Overall, the model is a good fit for the data based on currently accepted model fit guidelines (Hu & Bentler, 1999; Muthen, 2004). Although the indicator variables of each latent variable are correlated, the magnitudes of the relationships do not suggest collinearity (see Table II). The final model including standardized path estimates is presented in Figure 2. R-squared values, reflecting the amount of variance accounted for by the latent variables upon which each of the mediating and outcome variables are regressed, are as follows: Neighborhood disadvantage, r2 = .388, social support, r2 = .297, negative affect/perceived stress, r2 = .541, at-risk drinking, r2 = .101, insufficient physical activity, r² = .034, and overweight/obesity, r² = .022. Path coefficients indicating the total effects of SES on the outcome variables are as follows: at-risk drinking, -.329, p < .001, insufficient physical activity, -.192, p = .013, and overweight/obesity, .127, p = .068. Most of the specific indirect effects in the final model are statistically significant at p < .05, with the following exceptions: SES → Neighborhood Disadvantage → Social Support → Overweight/Obesity, p = .08; Neighborhood Disadvantage → Social Support → Overweight/Obesity, p =.08; SES → Social Support → Negative Affect/Perceived Stress → Insufficient physical activity, p = .06; SES → Social Support → Overweight/Obesity, p = .10.
Table II.
Correlations among variables in the final model.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Financial Strain | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 2. Employment a | -.29*** | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 3. Education b | -.13** | .23*** | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 4. Income | -.39*** | .45*** | .35*** | - | - | - | - | - | - | - | - | - | - | - | - |
| 5. Neighborhood Problems | .32*** | -.16** | -.22*** | -.28*** | - | - | - | - | - | - | - | - | - | - | - |
| 6. Social Cohesion and Trust | -.38*** | .13** | .16*** | .29*** | -.46*** | - | - | - | - | - | - | - | - | - | - |
| 7. Neighborhood Vigilance | .28*** | -.11* | -.19*** | -.26*** | .45*** | -.45*** | - | - | - | - | - | - | - | - | - |
| 8. Tangible Support (ISEL) | -.33*** | .16** | .16*** | .27*** | -.28*** | .26*** | -.25*** | - | - | - | - | - | - | - | - |
| 9. Belonging (ISEL) | -.34*** | .14** | .16** | .26*** | -.29*** | .24*** | -.26*** | .65*** | - | - | - | - | - | - | - |
| 10. Appraisal (ISEL) | -.30*** | .08 | .16** | .22*** | -.28*** | .33*** | -.28*** | .67*** | .64*** | - | - | - | - | - | - |
| 11. Depression (CES-D) | .38*** | -.25*** | -.31*** | -.31*** | .43*** | -.40*** | .46*** | -.41*** | -.39*** | -.46*** | - | - | - | - | - |
| 12. Negative Affect (PANAS) | .37*** | -.19*** | -.16** | -.23*** | .38*** | -.36*** | .42*** | -.33*** | -.36*** | -.38*** | .83*** | - | - | - | - |
| 13. Perceived Stress | .46*** | -.16** | -.25*** | -.24*** | .35*** | -.38*** | .37*** | -.42*** | -.38*** | -.38*** | .71*** | .69*** | - | - | - |
| 14. At-Risk Drinking c | .08 | .02 | -.18*** | -.06 | .13** | -.09 | .10 | -.17*** | -.09 | -.13** | .22*** | .20*** | .24*** | - | - |
| 15. Insufficient Physical Activity d | .09 | -.17*** | -.05 | -.12* | -.01 | -.03 | .07 | -.04 | -.07 | -.06 | .12* | .12* | .12* | -.10 | - |
| 16. Overweight/Obesity e | -.03 | -.05 | .10* | .04 | -.06 | -.05 | -.05 | .07 | .09 | .08 | -.09 | -.07 | -.08 | -.17*** | -.02 |
Note: ISEL = Interpersonal Support Evaluation List; CES-D = Center for Epidemiologic Studies Depression; PANAS = Positive and Negative Affect Schedule
Unemployed = 1, Employed = 2
≤ High School = 1, > High School = 2
Low-Risk drinking = 1, At-Risk Drinking = 2
Moderate/High Activity = 1, Insufficient Physical Activity = 2
Normal BMI = 1, Overweight/Obese = 2
p ≤ .05
p ≤ .01
p ≤ .001
Figure 2.
Final model of the pathways between socioeconomic status and modifiable risk factors, including standardized path estimates. Note: CES-D = Center for Epidemiologic Studies Depression; PANAS NA = Positive and Negative Affect Schedule Negative Affect; PSS = Perceived Stress Scale; * p ≤ .05; ** p ≤ .01; *** p ≤ .001
Gender Differences
Separate analyses were conducted by gender group to determine whether the final model was a good fit for both males and females. WLSMV estimation for the final model yielded acceptable model fit values for each gender group: Males, χ²(42) = 69.73, p = .005, RMSEA = .058, TLI = .952, CFI = .882, and WRMR = .717; Females, χ²(39) = 54.669, p = .049, RMSEA = .044, TLI = .967, CFI = .939, and WRMR = .659. A multiple group analysis was conducted, using the DIFFTEST option for WLSMV estimation (see Muthen & Muthen, 2007), to determine whether the individual paths in the final model differed significantly by gender group. No differences between gender groups were noted; with the exception of the path between social support and negative affect/perceived stress. Specifically, the inverse relationship between social support and negative affect/perceived stress was stronger for males than females. Table III displays the unstandardized, rather than the standardized, path estimates by gender to allow for direct comparisons across gender groups (i.e., standardized estimates may not be directly compared across groups; see Kline, 2005).
Table III.
Unstandardized path estimates by gender in the final model.
| Males | Females | ||||
|---|---|---|---|---|---|
| Pathway | Unstandardized Estimate | SE | Unstandardized Estimate | SE | Diff. χ²(1) |
| SES → Social Support | .809 | .453 | 1.241* | .613 | .348 |
| SES → Neighborhood Disadvantage | -3.118*** | .576 | -3.183*** | .911 | .006 |
| SES → Negative Affect/Perceived Stress | -2.546 | 2.102 | -4.683* | 2.077 | .614 |
| Neighborhood Disadvantage → Social Support | -.312** | .102 | -.229** | .087 | .404 |
| Neighborhood Disadvantage → Negative Affect/Perceived Stress | 1.124* | .489 | 1.594*** | .336 | .591 |
| Social Support → Negative Affect/Perceived Stress | -1.991*** | .428 | -.732* | .346 | 6.095* |
| Social Support → Overweight/Obesity | .043 | .047 | .090* | .041 | .581 |
| Negative Affect/Perceived Stress → Insufficient Physical Activity | .021* | .009 | .014 | .009 | .252 |
| Negative Affect/Perceived Stress → At-Risk Drinking | .036*** | .009 | .026** | .008 | .695 |
p ≤ .05
p ≤ .01
p ≤ .001
Discussion
The present study evaluated an a priori conceptual model of the pathways linking SES and modifiable health risk factors (i.e., at-risk drinking, insufficient physical activity, overweight/obesity) in a sample of AA smokers. The final model indicated that SES, neighborhood disadvantage, and social support influence the likelihood of at-risk drinking and insufficient physical activity through their impact on negative affect/perceived stress. SES and neighborhood disadvantage appeared to influence overweight/obesity through their impact on social support. Overall, findings indicated that SES had a significant indirect impact on at-risk drinking and insufficient physical activity, and only a marginal influence on overweight/obesity. Although the inverse relationship between social support and negative affect/perceived stress was stronger for males than females, the final model was a good fit overall for both AA male and female smokers. The findings elucidate the important roles that neighborhood disadvantage, social support, and negative affect/perceived stress play as mediators of the links between SES and modifiable health risk factors in a high risk population (i.e., AA smokers) that suffers from significant health disparities.
Several differences between our final model and previously hypothesized models (i.e., Adler & Ostrove, 1999; Gallo & Matthews, 2003) were observed. Neighborhood disadvantage was not directly linked with any of the modifiable risk factors. Rather its influence on at-risk drinking and insufficient physical activity was mediated through negative affect/perceived stress. However, it seems plausible that the specific dimensions of neighborhood disadvantage that were measured in the current study (i.e., neighborhood problems, social cohesion, neighborhood vigilance) might have a greater impact on affect than on the three specific modifiable risk factors that were investigated. Other measures of neighborhood disadvantage such as the density of alcohol/tobacco outlets and advertising, access to parks and greenspace, or the availability of grocery stores may have a more direct influence on these modifiable risk factors.
Similarly, social support was not directly associated with at-risk drinking and insufficient PA. Perhaps the influence of social support on physical activity and alcohol consumption varies based on the social norms of the individuals who comprise the social support network. That is, some networks may encourage alcohol consumption or sedentary activities even when social support for members is strong. As a result, social support may have a more consistent impact on health risk factors indirectly through negative affect/perceived stress. Further, the measure of social support utilized in the current study did not specifically assess social support for healthy lifestyles. Thus, measures that assessed positive social support as it relates to physical activity, weight management, or moderate alcohol consumption may have had a more direct influence on modifiable risk factors. Finally, findings in the current study suggested that low social support may be more strongly linked with negative affect among men than women. This finding differs from previous research indicating that social support may protect against depression among AA women but not men (Brown & Gary, 1987; Husaini et al., 1991). Additional studies will be needed to reconcile discrepant findings in AA samples.
Surprisingly, greater social support was positively associated with overweight/obesity in the final model. Perhaps this finding may be understood in the context of social integration theory, which suggests that social groups and society have an influence on an individual's perceptions and beliefs (see Vilhjalmsson, 1993). AAs often prefer a larger body size than individuals from other racial/ethnic groups (Gluck & Geliebter, 2002), and rates of overweight/obesity are elevated among AAs in general and among treatment-seeking AA smokers (Kendzor, Costello, et al., 2008; Ogden et al., 2006). Thus, AA individuals who are more socially integrated may view overweight/obesity as normative when their support group possesses these characteristics. Therefore, such individuals may be less concerned about overweight/obesity and less inclined to engage in behaviors that promote weight management.
Contrary to our hypothesis, the indirect effect of SES and the direct effect of negative affect/perceived stress on overweight/obesity were not significant in the final model. Negative affect has been linked with both increases and decreases in appetite and weight. Thus, additional studies are needed to clarify the relationship between negative affect/perceived stress and overweight/obesity among AAs. The indirect effect of SES on overweight/obese only approached significance, suggesting that SES may have a subtle influence or that other relevant variables should be examined in future research (e.g., family history of obesity, availability of grocery stores, density of fast-food restaurants).
SES was found to have a significant direct influence on negative affect/perceived stress, providing support for this hypothesized pathway in the model described by Adler and Ostrove (1999). These results suggest that neighborhood disadvantage and social support do not fully explain the relationship between SES and negative affect/perceived stress. Additional variables related to SES may also contribute to negative affect/perceived stress such as exposure to traumatic experiences or reduced access to resources such as medical care or transportation.
The results of the current study highlight the roles of neighborhood disadvantage, social support, and negative affect/perceived stress in the relationship between SES and health risk factors in AA smokers. Findings suggest that multi-level and multiple risk behavior interventions might be useful in reducing the prevalence of health risk factors in AA smokers. Specifically, policy changes that positively impact distal factors such as employment, education, and income are likely to have a beneficial indirect influence on modifiable risk factors. Community and neighborhood-level interventions, such as reducing crime through neighborhood watch programs and increasing community advocacy and empowerment, may also influence the prevalence of health risk factors, at least in part, through their impact on collective efficacy and perceptions of neighborhood disadvantage. At the individual-level, it may be both beneficial and efficient to target multiple health risk behaviors within smoking cessation interventions. Treatments might include coping skills and stress management training for those who are experiencing chronic stress and negative affect related to low SES. Targeting negative affect may be particularly important, given that negative affect appears to function as a key mediator of the relationships between SES, neighborhood disadvantage, social support, and modifiable risk factors. In addition, interpersonal interventions that facilitate the development of new relationships with individuals who possess similar health goals (e.g., quitting smoking, becoming more active) and who may therefore have a positive influence on the individual's health behavior might be useful. Strategies that address many of the key influences on health and modifiable risk factors such as poverty, education, employment, the availability of public transportation and housing, and the affordability and accessibility of healthy foods have been described elsewhere (Tarlov, 1999).
Several strengths and limitations of the study should be noted. The entirely AA sample provided an opportunity to obtain valuable information about the impact of SES on the health risk factors of treatment-seeking AA smokers, a population at very high risk for experiencing adverse health outcomes and health disparities. In addition, the present study evaluated multiple pathways (i.e., neighborhood disadvantage, social support, negative affect/perceived stress) between SES and modifiable risk factors using latent variable modeling techniques. Unfortunately, causality cannot be inferred from the findings due to the cross-sectional design of the study. It is also important to note that overweight/obesity differs from the other two modifiable risk factors in that it is not a behavior itself, but is instead influenced by behavioral factors such as poor diet and insufficient physical activity. As such, overweight/obesity might also be considered a health outcome rather than a modifiable risk factor in the model. Modifiable risk factors were dichotomized to reflect the point at which a risk factor may warrant clinical intervention. Unfortunately, this may have limited the ability to detect a more subtle relationship between the variables in the model. Thus, it may be informative to include continuous outcomes in future studies (e.g., body mass index, weekly minutes of physical activity, number of drinks per week).
Another limitation of the findings is that the sample may not be representative of AA samples in general or AA smokers in particular, as participants tended to be heavy smokers of low SES, and all participants were seeking smoking cessation treatment and were willing to quit within the next two weeks. The estimated smoking prevalence among AAs in the U.S. was 18.9% in 2007 (CDC, 2008), indicating that AA smokers represent a minority of the general AA population. Smokers are also more likely to be of lower socioeconomic status that non-smokers (Lantz et al., 1998; Lynch et al., 1997), and smokers in the present study were more likely to be female, heavy smokers, unemployed, and of single marital status than in other nationally representative samples of AA smokers (Caraballo et al., 1998; Novotny et al., 1988). Although a convenience sample was utilized, AA smokers of low SES warrant further study because they represent a group of individuals who are at significantly greater risk of tobacco-related and other health disparities.
Future studies are needed to confirm the present model in additional populations using prospective designs, and to identify other key pathways between SES and health outcomes. It is possible that pathways in the model may differ by race/ethnicity, smoking status, and type of modifiable risk factor. Longitudinal research will be required to determine the time course of the relationships among SES, neighborhood disadvantage, social support, negative affect/perceived stress, and modifiable risk factors. Although SES is presumed to precede all other variables in the proposed model, this remains to be determined. Reciprocal relations among variables included in the model are also possible. Further, the extent to which SES and other variables in the model may influence changes in modifiable risk factors is unclear, as the present model focused on modifiable risk factors that were occurring at one point in time. Modifiable health risk factors may covary in specific patterns that facilitate or hinder behavior change, which may have implications for the sequence that behaviors are addressed within interventions. For example, physical activity tends to increase following successful smoking cessation (Nagaya et al., 2007) and interventions might attempt to capitalize on such phenomena. It will also be important to determine the contributions of other variables not included in the model to the relationship between SES and health (e.g., environmental exposure to carcinogens, built environment, neighborhood poverty), and to study additional modifiable health risk factors (e.g., diet, sun exposure). Efforts to understand gender differences in the prevalence of each modifiable risk factor are also needed. Plausibly, higher rates of overweight/obesity and insufficient physical activity among AA women may result from the acceptance of and/or preference for a larger body size, whereas greater alcohol consumption may be viewed as more socially acceptable for men than women. Finally, the influence of SES on disease risk via the interplay of environmental, psychosocial, and physiological pathways must be further explored (e.g., the effects of high neighborhood crime on perceived threat and the Hypothalamic-Pituitary-Adrenal axis). In sum, continued research aimed at gaining a better theoretical and empirical understanding of the socioeconomic, environmental, and psychosocial factors that influence modifiable risk factors may contribute to the elimination of tobacco-related and other health disparities among AAs.
Acknowledgments
This research was supported by grants R01-CA094826, R01-CA125413, and R25T-CA57730 awarded by the National Cancer Institute, and grants K01-DP001120 and K01-DP000086 awarded by the National Center for Chronic Disease Prevention and Health Promotion. The final version of this manuscript was published in the Journal of Behavioral Medicine. The original publication is available at springerlink.com: http://www.springerlink.com/content/l33674j338252044/
References
- Adler NE, Ostrove JM. Socioeconomic status and health: What we know and what we don't. Annals of the New York Academy of Sciences. 1999;896:3–15. doi: 10.1111/j.1749-6632.1999.tb08101.x. [DOI] [PubMed] [Google Scholar]
- Adler NE, Rehkopf DH. U.S. disparities in health: Descriptions, causes, and mechanisms. Annual Review of Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- Blot WJ, McLaughlin JK, Winn DM, Austin DF, Greenberg RS, Preston-Martin S, et al. Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Research. 1988;48:3282–3287. [PubMed] [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, et al. Socioeconomic status in health research: One size does not fit all. Journal of the American Medical Association. 2005;294:2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- Brown DR, Gary LE. Stressful life events, social support networks, and the physical and mental health of urban black adults. Journal of Human Stress. 1987;13:165–174. doi: 10.1080/0097840X.1987.9936810. [DOI] [PubMed] [Google Scholar]
- Brown TA. Data issues in CFA: Missing, non-normal, and categorical data. In: Brown T, editor. Confirmatory Factor Analysis for Applied Research. New York, NY: The Guilford Press; 2006. pp. 363–411. [Google Scholar]
- Caraballo RS, Giovino GA, Pechacek TF, Mowery PD, Richter PA, Strauss WJ, et al. Racial and ethnic differences in serum cotinine levels of cigarette smokers. Journal of the American Medical Association. 1998;280:135–139. doi: 10.1001/jama.280.2.135. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Cigarette smoking among adults – United States, 2007. Morbidity and Mortality Weekly Reports. 2008;57:1221–1226. [PubMed] [Google Scholar]
- Cerin E, Leslie E. How socio-economic status contributes to participation in leisure-time physical activity. Social Science & Medicine. 2008;66:2596–2609. doi: 10.1016/j.socscimed.2008.02.012. [DOI] [PubMed] [Google Scholar]
- Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology. 1983;13:99–125. [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health & Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International Physical Activity Questionnaire: 12-country reliability and validity. Medicine & Science in Sports & Exercise. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Cutrona CE, Russell DW, Brown PA, Clark LA, Hessling RM, Gardner KA. Neighborhood context, personality, and stressful life events as predictors of depression among African American women. Journal of Abnormal Psychology. 2005;114:3–15. doi: 10.1037/0021-843X.114.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delva J, Tellez M, Finlayson TL, Gretebeck KA, Siefert K, Williams DR, et al. Correlates of cigarette smoking among low-income African American women. Ethnicity & Disease. 2006;16:527–533. [PubMed] [Google Scholar]
- Di Castelnuovo A, Constanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G. Alcohol dosing and total mortality in men and women. Archives of Internal Medicine. 2006;166:2437–2445. doi: 10.1001/archinte.166.22.2437. [DOI] [PubMed] [Google Scholar]
- Echeverria S, Diez-Roux AV, Shea S, Borrell LN, Jackson S. Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: The multi-ethnic study of atherosclerosis. Health & Place. 2008;14:851–863. doi: 10.1016/j.healthplace.2008.01.004. [DOI] [PubMed] [Google Scholar]
- Fagan P, Moolchan ET, Lawrence D, Fernander A, Ponder PK. Identifying health disparities across the tobacco continuum. Addiction. 2007;102:S5–S29. doi: 10.1111/j.1360-0443.2007.01952.x. [DOI] [PubMed] [Google Scholar]
- Fernander AF, Shavers VL, Hammons GJ. A biopsychosocial approach to examining tobacco-related health disparities among racially classified social groups. Addiction. 2007;102:S43–S57. doi: 10.1111/j.1360-0443.2007.01954.x. [DOI] [PubMed] [Google Scholar]
- Freedman DM, Sigurdson AJ, Rajaraman P, Doody MM, Linet MS, Ron E. The mortality risk of smoking and obesity combined. American Journal of Preventive Medicine. 2006;31:355–362. doi: 10.1016/j.amepre.2006.07.022. [DOI] [PubMed] [Google Scholar]
- Galea S, Ahern J, Nandi A, Tracy M, Beard J, Vlahov D. Urban neighborhood poverty and the incidence of depression in a population-based cohort study. Annals of Epidemiology. 2007;17:171–179. doi: 10.1016/j.annepidem.2006.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role? Psychological Bulletin. 2003;129:10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- Gluck ME, Geliebter A. Racial/ethnic differences in body image and eating behaviors. Eating Behaviors. 2002;3:143–151. doi: 10.1016/s1471-0153(01)00052-6. [DOI] [PubMed] [Google Scholar]
- Goodwin RD. Association between physical activity and mental disorders among adults in the United States. Preventive Medicine. 2003;36:698–703. doi: 10.1016/s0091-7435(03)00042-2. [DOI] [PubMed] [Google Scholar]
- Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ) 2005 Retrieved June 5, 2008, from http://www.ipaq.ki.se/scoring.htm. [PubMed]
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of Major Depressive Disorder. Archives of General Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Hill TD, Angel RJ. Neighborhood disorder, psychological distress, and heavy drinking. Social Science & Medicine. 2005;61:965–975. doi: 10.1016/j.socscimed.2004.12.027. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Husaini BA, Moore ST, Castor RS, Neser W, Whitten-Stovall R, Linn JG, et al. Social density, stressors, and depression: Gender differences among the black elderly. Journal of Gerontology: Psychological Sciences. 1991;46:P236–242. doi: 10.1093/geronj/46.5.p236. [DOI] [PubMed] [Google Scholar]
- Hutchinson RG, Watson RL, Davis CE, Barnes R, Brown S, Romm F, et al. Racial differences in risk factors for atherosclerosis: The ARIC study. Angiology. 1997;48:279–290. doi: 10.1177/000331979704800401. [DOI] [PubMed] [Google Scholar]
- John D, Catherine T. MacArthur Research Network on Socioeconomic Status and Health. Reactive Responding – Long Form. 1999 Retrieved June 2, 2008, from http://www.macses.ucsf.edu/Research/Psychosocial/notebook/RR-42.html.
- Katzmarzyk PT, Janssen I, Adern CI. Physical inactivity, excess adiposity and premature mortality. Obesity Reviews. 2003;4:257–290. doi: 10.1046/j.1467-789x.2003.00120.x. [DOI] [PubMed] [Google Scholar]
- Kendzor DE, Cofta-Woerpel LM, Mazas CA, Li Y, Irvin Vidrine J, Reitzel LR, et al. Socioeconomic status, negative affect, and modifiable cancer risk factors in African American smokers. Cancer Epidemiology, Biomarkers, & Prevention. 2008;17:2546–2554. doi: 10.1158/1055-9965.EPI-08-0291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendzor DE, Costello TJ, Li Y, Irvin Vidrine J, Mazas CA, Reitzel LR, et al. Race/ethnicity and multiple cancer risk factors among individuals seeking smoking cessation treatment. Cancer Epidemiology, Biomarkers, & Prevention. 2008;17:2937–2945. doi: 10.1158/1055-9965.EPI-07-2795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. How to fool yourself with SEM. In: Kline R, editor. Principles and Practice of Structural Equation Modeling. New York: The Guilford Press; 2005. pp. 313–324. [Google Scholar]
- Lantz PM, House JS, Lepkowski JM, Williams DR, Mero RP, Chen JC. Socioeconomic factors, health behaviors, and mortality. Journal of the American Medical Association. 1998;279:1703–1708. doi: 10.1001/jama.279.21.1703. [DOI] [PubMed] [Google Scholar]
- Lincoln KD, Chatters LM, Taylor RJ. Social support, traumatic events, and depressive symptoms among African Americans. Journal of Marriage and Family. 2005;67:754–766. doi: 10.1111/j.1741-3737.2005.00167.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincoln KD, Chatters LM, Taylor RJ, Jackson JS. Profiles of depressive symptoms among African Americans and Carribbean Blacks. Social Science & Medicine. 2007;65:200–213. doi: 10.1016/j.socscimed.2007.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviors and psychosocial characteristics by stages of the socioeconomic life course. Social Science & Medicine. 1997;44:809–819. doi: 10.1016/s0277-9536(96)00191-8. [DOI] [PubMed] [Google Scholar]
- Marrero JA, Fontana RJ, Fu S, Conjeevaram HS, Su GL, Lok AS. Alcohol, tobacco, and obesity are synergistic risk factors for hepatocellular carcinoma. Journal of Hepatology. 2005;42:218–224. doi: 10.1016/j.jhep.2004.10.005. [DOI] [PubMed] [Google Scholar]
- Melchior M, Moffitt TE, Milne BJ, Poulton R, Caspi A. Why do children from socioeconomically disadvantaged families suffer from poor health when they reach adulthood? A life-course study. American Journal of Epidemiology. 2007;166:966–974. doi: 10.1093/aje/kwm155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- Miller ST, Schlundt DG, Larson C, Reid R, Pichert JW, Hargreaves M, et al. Exploring ethnic disparities in diabetes, diabetes care, and lifestyle behaviors: The Nashville REACH 2010 community baseline survey. Ethnicity & Disease. 2004;14:S38–45. [PubMed] [Google Scholar]
- Mirowsky J, Ross CE. Age and the effect of economic hardship on depression. Journal of Health & Social Behavior. 2001;42:132–150. [PubMed] [Google Scholar]
- Mujahid MS, Diez Roux AV, Shen M, Gowda D, Sanchez B, Shea S, et al. Relation between neighborhood environments and obesity in the multi-ethnic study of atherosclerosis. American Journal of Epidemiology. 2008;167:1349–1357. doi: 10.1093/aje/kwn047. [DOI] [PubMed] [Google Scholar]
- Muthen BO. Mplus Technical Appendices. Los Angeles, CA: Muthen & Muthen; 2004. p. 24. [Google Scholar]
- Muthen LK, Muthen BO. Mplus User's Guide. Los Angeles, CA: Muthen & Muthen; 2007. pp. 501–502. [Google Scholar]
- Nagaya T, Yoshida H, Takahashi H, Kawai M. Cigarette smoking weakens exercise habits in healthy men. Nicotine & Tobacco Research. 2007;9:1027–1032. doi: 10.1080/14622200701591575. [DOI] [PubMed] [Google Scholar]
- Navarro V. Race or class versus race and class: mortality differentials in the Unites States. The Lancet. 1990;336:1238–1240. doi: 10.1016/0140-6736(90)92846-a. [DOI] [PubMed] [Google Scholar]
- Novotny TE, Warner KE, Kendrick JS, Remington PL. Smoking by blacks and whites: Socioeconomic and demographic differences. American Journal of Public Health. 1988;78:1187–1189. doi: 10.2105/ajph.78.9.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. Journal of the American Medical Association. 2006;295:1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- Ostrove JM, Feldman P. Education, income, wealth, and health among Whites and African Americans. Annals of the New York Academy of Sciences. 1999;896:335–337. doi: 10.1111/j.1749-6632.1999.tb08133.x. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. Journal of Health and Social Behavior. 1981;22:337–356. [PubMed] [Google Scholar]
- Peirce RS, Frone MR, Russell M, Cooper ML, Mudar P. A longitudinal model of social contact, social support, depression, and alcohol use. Health Psychology. 2000;19:28–38. doi: 10.1037//0278-6133.19.1.28. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Ross CE, Mirowsky J. Explaining the social patterns of depression: Control and problem-solving – or support and talking? Journal of Health and Social Behavior. 1989;30:206–219. [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Seale JP, Davis-Smith M, Okosun I. Ethnic and gender differences in lifestyle risk factors in a bi-ethnic primary care sample: prevalence and clinical implications. Ethnicity & Disease. 2006;16:460–467. [PubMed] [Google Scholar]
- Sharma S, Malarcher AM, Giles WH, Myers G. Racial, ethnic and socioeconomic disparities in the clustering of cardiovascular disease risk factors. Ethnicity & Disease. 2004;14:43–48. [PubMed] [Google Scholar]
- Shavers VL. Measurement of socioeconomic status in health disparities research. Journal of the National Medical Association. 2007;99:1013–1023. [PMC free article] [PubMed] [Google Scholar]
- Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, et al. Association between obesity and psychiatric disorders in the US adult population. Archives of General Psychiatry. 2006;63:824–30. doi: 10.1001/archpsyc.63.7.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Alcohol consumption measures. In: Allen JP, Wilson VB, editors. Assessing alcohol problems: A guide for clinicians and researchers. Bethesda, MD: U.S. Department of Health and Human Services, National Institute on Alcohol Abuse and Alcoholism (NIH Publication No. 03-3745); 2003. pp. 75–99. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Journal of the American Medical Association. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress: Development of a measure of neighborhood problems, and associations with socioeconomic status and health. Annals of Behavioral Medicine. 2001;23:177–185. doi: 10.1207/S15324796ABM2303_5. [DOI] [PubMed] [Google Scholar]
- Strine TW, Chapman DP, Balluz L, Mokdad AH. Health-related quality of life and health behaviors by social and emotional support. Social Psychiatry and Psychiatric Epidemiology. 2008;43:151–159. doi: 10.1007/s00127-007-0277-x. [DOI] [PubMed] [Google Scholar]
- Tarlov AR. Public policy frameworks for improving population health. Annals of the New York Academy of Sciences. 1999;896:281–293. doi: 10.1111/j.1749-6632.1999.tb08123.x. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. The stress process and the social distribution of depression. Journal of Health and Social Behavior. 1999;40:374–404. [PubMed] [Google Scholar]
- U.S. Census Bureau. Income, Poverty, and Health Insurance Coverage in the United States: 2006. Washington, DC: U.S. Government Printing Office; 2007. pp. 60–233. [Google Scholar]
- U.S. Department of Health and Human Services (USDHHS) Helping patients who drink too much: A clinician's guide. 2007. NIH Publication No. 07-3769. [Google Scholar]
- Vilhjalmsson R. Life stress, social support and clinical depression: A reanalysis of the literature. Social Science & Medicine. 1993;37:331–342. doi: 10.1016/0277-9536(93)90264-5. [DOI] [PubMed] [Google Scholar]
- Wang Y, Beydoun MA. The obesity epidemic in the United States – gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegan A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality & Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wendel-Vos W, Droomers M, Kremers S, Brug J, van Lenthe F. Potential environmental determinants of physical activity in adults: A systematic review. Obesity Reviews. 2007;8:425–440. doi: 10.1111/j.1467-789X.2007.00370.x. [DOI] [PubMed] [Google Scholar]
- Whitt-Glover MC, Taylor WC, Heath GW, Macera CA. Self-reported physical activity among blacks: estimates from national surveys. Am J Prev Med. 2007 Nov;33(5):412–417. doi: 10.1016/j.amepre.2007.07.024. [DOI] [PubMed] [Google Scholar]