Abstract
Objective
Maternal obesity is associated with adverse pregnancy outcomes. To improve outcomes, obstetric providers must effectively evaluate and manage their obese pregnant patients. We sought to determine the knowledge, attitudes, and practice patterns of obstetric providers regarding obesity in pregnancy.
Methods
In 2007–2008, we surveyed 58 practicing obstetricians, nurse practitioners, and certified nurse-midwives at a multispecialty practice in Massachusetts. We administered a 26-item questionnaire that included provider self-reported weight, sociodemographic characteristics, knowledge, attitudes, and management practices. We created an 8-point score for adherence to 8 practices recommended by the American College of Obstetricians and Gynecologists (ACOG) for the management of obese pregnant women.
Results
Among the respondents, 37% did not correctly report the minimum body mass index (BMI) for diagnosing obesity, and most reported advising gestational weight gains that were discordant with 1990 Institute of Medicine (IOM) guidelines, especially for obese women (71%). The majority of respondents almost always recommended a range of weight gain (74%), advised regular physical activity (74%), or discussed diet (64%) with obese mothers, but few routinely ordered glucose tolerance testing during the first trimester (26%), planned anesthesia referrals (3%), or referred patients to a nutritionist (14%). Mean guideline adherence score was 3.4 (SD 1.9, range 0–8). Provider confidence (β = 1.0, p = 0.05) and body satisfaction (β = 1.5, p = 0.02) were independent predictors of higher guideline adherence scores.
Conclusions
Few obstetric providers were fully compliant with clinical practice recommendations, defined obesity correctly, or recommended weight gains concordant with IOM guidelines. Provider personal factors were the strongest correlates of self-reported management practices. Our findings suggest a need for more education around BMI definitions and weight gain guidelines, along with strategies to address provider personal factors, such as confidence and body satisfaction, that may be important predictors of adherence to recommendations for managing obese pregnant women.
Introduction
In women of childbearing age, the prevalence of obesity is high (28.9%) and shows no signs of abating.1 Maternal obesity is associated with a number of adverse outcomes during and after pregnancy, such as gestational hypertension and diabetes in mothers, and macrosomia and later overweight in their children.2 Obese women are more likely to gain in excess of current gestational weight gain guidelines,3 which itself increases the risk for maternal and offspring morbidity.4,5
Data suggest that improvements in glucose metabolism and delivery outcomes are achievable for obese women who control their weight gain and remain physically active in pregnancy.6–8 Because pregnant women have frequent interactions with the healthcare system, obstetric providers are uniquely positioned to address the issues of weight gain and exercise with their obese pregnant patients. In a national survey, however, only 58% of obstetrician/gynecologists reported counseling their pregnant patients about weight gain during pregnancy “most of the time,” and even fewer (35.7%) modified their recommendations based on their patients' prepregnancy body mass index (BMI).9 This lack of counseling is a concern, as women who receive advice from their providers regarding appropriate gestational weight gain are more likely to gain within recommended ranges.10,11
To address the role of the obstetric provider in the assessment and management of obesity in pregnancy, the American College of Obstetricians and Gynecologists (ACOG) released Committee Opinion No. 315, Obesity in Pregnancy, in late 2005.12 Included in this report was a series of recommendations designed to aid providers in assessing, counseling, and referring their obese pregnant patients. No data yet exist about whether obstetric providers are following these recommendations or what clinician factors are associated with adherence to them.
In the current study, we surveyed obstetric providers at a large, multispecialty group practice to determine knowledge, attitudes, and practice patterns regarding obesity in pregnancy. Additionally, we identified provider characteristics associated with greater adherence to ACOG clinical practice recommendations for the obese pregnant patient.
Materials and Methods
Between late fall 2007 and spring 2008, we administered surveys to 101 practicing obstetricians, nurse practitioners (NP), and certified nurse-midwives (CNM) at Harvard Vanguard Medical Associates, a multispecialty group practice in eastern Massachusetts. At the time of the survey, Harvard Vanguard comprised 16 practice sites with an estimated 3000 deliveries per year. We surveyed 64 providers in attendance at their quarterly department meeting and obtained 43 responses. We mailed surveys to the 37 nonattendees and received an additional 15 responses, for a total of 58 of 101 (58%) completed questionnaires. Participants provided written informed consent, and the institutional review board of Harvard Pilgrim Health Care approved the study.
We developed the questionnaire based on our review of the medical literature and our previous experience surveying women during pregnancy.5,7 We then field tested the questionnaire with eight local experts in medicine, obstetric care, and obesity research, who reviewed the draft and provided feedback. The final survey consisted of 26 questions about provider demographics, BMI, body satisfaction, clinical site characteristics, knowledge about obesity and weight gain recommendations in pregnancy, along with attitudes and perceived barriers to managing obese pregnant patients (scored on a 4-point Likert scale, from strongly agree to strongly disagree, which we subsequently dichotomized as strongly agree/agree vs. disagree/strongly disagree). We also assessed obstetric provider adherence to 2005 ACOG practice recommendations for the obese pregnant patient by querying how frequently providers (1) told obese women they were overweight or obese, (2) discussed the risks associated with being obese during pregnancy, (3) recommended a specific range of weight gain during pregnancy, (4) recommended regular physical activity, (5) discussed diet, (6) ordered glucose tolerance testing during the first trimester, (7) planned to obtain an anesthesia referral prior to delivery, and (8) referred obese women to a nutritionist/dietitian.12 Responses ranged from almost always to almost never, using a 4-point Likert scale, which we then dichotomized as almost always vs. less frequently.
We conducted simple descriptive statistics, such as means and frequency tables, for all responses. For the few questions with missing responses, we excluded participants who did not answer. Differences between physicians and nurses (NP or CNM) in their answers to knowledge, attitude, and practice recommendations were evaluated using chi-square tests. We also created an 8-point adherence score by summing the number of almost always responses to the 8 ACOG practice recommendations and then used multivariable linear regression to identify provider characteristics associated with a higher score. We used SAS version 9.1 (SAS Institute, Cary, NC) to carry out all analyses.
Results
Characteristics of the 58 respondents are reported in Table 1. The majority of respondents were physicians; 88% were women (48% M.D.s, 52% nurses), and the remaining 12% were men, all of whom were physicians. Mean self-reported BMI was 24.3 (standard deviation [SD] 3.3) kg/m2, and 38% of providers were overweight or obese (BMI ≥ 25.0 kg/m2). Approximately 30% of providers reported they were either extremely or somewhat satisfied with their own weight. Overweight or obese respondents were less likely than their normal weight colleagues to be satisfied with their weight (p = 0.002); however, even among normal weight providers, less than half (46%) reported body weight satisfaction.
Table 1.
Characteristics of Surveyed Obstetric Providers
| Provider characteristics | n (%) |
|---|---|
| Female | 50 (88) |
| White race | 48 (83) |
| Provider type | |
| Obstetrician | 32 (55) |
| Nurse practitioner | 8 (14) |
| Certified nurse-midwife | 18 (31) |
| Clinical training completed > 10 years ago | 37 (64) |
| Self-reported weight status | |
| Underweight | 1 (2) |
| Normal weight | 34 (61) |
| Overweight or obese | 21 (38) |
| Satisfied with body weight | 17 (30) |
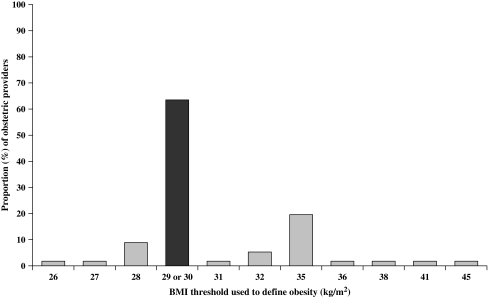
Providers estimated that, on average, 36% of their pregnant patients were overweight and 19% were obese. However, when we asked providers to report the BMI values that delimit each weight category, only 63% correctly identified the BMI that is the threshold for obesity, even though we allowed correct responses to range between 29 kg/m2 (according to 1990 Institute of Medicine [IOM] guidelines13) and 30 kg/m2 (according to National Heart, Lung, and Blood Institute guidelines14) (Fig. 1). Most (90%) who provided incorrect answers thought that the threshold was higher than 30 kg/m2 (range 31–45 kg/m2).
FIG. 1.
Reported body mass index (BMI) thresholds for obesity among surveyed obstetric providers. Dark column represents the correct threshold for obesity, according to 1990 Institute of Medicine guidelines13 and the National Heart, Lung, and Blood Institute guidelines.14 Data were missing on two providers (total n = 56).
We also asked providers to report how much weight gain they recommend for women according to prepregnancy BMI category. Provider gestational weight gain recommendations were generally discordant with current IOM guidelines (Table 2). Although the 1990 IOM guidelines advise obese women to gain at least 15 lbs, with no upper limit,13 more respondents in our survey reported that they recommended gain up to 15 lbs (45%) rather than gain of at least 15 lbs (29%) for these heaviest women. We did not find substantial differences between physicians and nurses who reported advising weight gains discordant with 1990 IOM recommendations (data not shown).
Table 2.
Gestational Weight Gain Ranges Recommended by 58 Surveyed Obstetric Providers
| |
Lower and upper limits of gestational weight gain |
||
|---|---|---|---|
| Maternal weight status | Mean (range) reported (lbs) | 1990 Institute of Medicine recommendation (lbs)13 | % Concordant with Institute of Medicine guidelines |
| Underweight | |||
| Lower limit | 28 (10–35) | ≥ 28a | 31 |
| Upper limit | 37 (20–45) | ≤ 40 | 45 |
| Normal weight | |||
| Lower limit | 23 (10–30) | ≥ 25 | 62 |
| Upper limit | 33 (25–40) | ≤ 35 | 55 |
| Overweight | |||
| Lower limit | 15 (0–25) | ≥ 15 | 39 |
| Upper limit | 22 (15–35) | ≤ 25 | 35 |
| Obeseb | |||
| Lower limit | 10 (0–25) | ≥ 15 | 29 |
Credit was also given for respondents who answered 25 lbs.
The 1990 Institute of Medicine guidelines did not specify an upper limit of weight gain for obese women.
The majority of respondents (83%) agreed with the statement that “obesity is an important health problem during pregnancy,” and a similar proportion (84%) indicated that once an obese woman is pregnant, she still has the ability to change the risks of pregnancy complications from obesity. However, only 67% of providers believed their “advice influences how much weight obese patients gain during pregnancy,” and even fewer (40%) agreed that “obese patients are motivated to make changes to their health.” Approximately half of surveyed providers felt confident in their counseling knowledge (53%) or reported that they “have enough time to counsel patients properly about the risks of obesity during pregnancy (48%).” Although 86% of providers agreed that “nutrition referrals are helpful for my obese patients,” only 65% reported that nutrition appointments were available to these patients.
Provider adherence to ACOG recommendations about diet and physical activity counseling for obese pregnant women was more common than compliance with recommendations regarding obesity assessment or referrals (Table 3). More nurses than physicians reported that they almost always discussed diet and physical activity with their obese pregnant patients; however, the mean total guideline adherence score did not considerably differ between nurses (mean 3.7, SD 1.6) and physicians (mean 3.1, SD 2.0, p = 0.2). On bivariate analyses, many provider factors, such as years since training, time for counseling, or attitudes about obese patients' motivations to change their health, were not associated with the adherence score. Only female sex, body satisfaction, confidence in knowledge about counseling, and the belief that obese pregnant patients can make changes to avoid pregnancy complications were significant predictors (p < 0.10) of a higher adherence score. On multivariable linear regression analysis, adjusting for these four factors as well as provider BMI, respondents who were confident in their knowledge about counseling (vs. not confident in knowledge, β = 1.0, p = 0.05) or were satisfied with their body weight (vs. indifferent or dissatisfied, β = 1.5, p = 0.02) were more likely to achieve a higher guideline adherence score.
Table 3.
Self-Reported Physician (M.D.) and Nurse (NP or CNM) Practice Patterns for Management of Obese Pregnant Patients
| |
|
% almost always |
|
|
|---|---|---|---|---|
| ACOG recommended practices12 | Entire sample n = 58% almost always | M.D. n = 32 | NP/CNM n = 26 | Chi-square p value |
| Tell the woman she is overweight or obese | 40 | 47 | 32 | 0.26 |
| Discuss the risks associated with being obese in pregnancy | 41 | 44 | 38 | 0.67 |
| Recommend a specific range of weight gain during pregnancy | 74 | 69 | 81 | 0.30 |
| Recommend regular physical activity | 74 | 59 | 92 | <0.01 |
| Discuss her diet | 64 | 44 | 88 | <0.01 |
| Order glucose tolerance testing during the first trimester | 26 | 26 | 27 | 0.92 |
| Plan to obtain an anesthesia referral prior to delivery | 3 | 3 | 4 | 0.88 |
| Refer her to a nutritionist/dietitian | 14 | 13 | 15 | 0.79 |
Discussion
In this survey of 58 obstetric providers, we found that most viewed obesity to be an important problem in pregnancy, yet few were fully compliant with ACOG clinical practice recommendations for the management of obese pregnant women. Provider personal factors, such as confidence and body satisfaction, may be important in the management of obesity in pregnancy. We identified deficiencies in knowledge about BMI categories and gestational weight gain guidelines, skepticism about obese patients' motivation to improve health, and a perceived need for greater availability of nutrition referrals and time for counseling.
An essential first step for appropriate assessment and management of obese patients requires basic provider knowledge of the BMI cutoff point at which obesity is diagnosed. The BMI categories are well established, accepted by all national bodies (including ACOG), and have been in place for over 10 years.14 However, over one third of surveyed obstetric providers defined obesity incorrectly, which may explain the lower estimation of obesity rates reported at Harvard Vanguard relative to actual population prevalence.1 Deficiencies in knowledge, however, are not isolated to obstetric providers; Block et al.15 in 2003 found that 60% of internal medicine residents did not know the minimum BMI to be considered obese. Education strategies are needed across specialties to achieve competency in this area.
Additionally, obstetric providers reported that they recommended gestational weight gain ranges to their patients that were largely discordant with IOM guidelines. A large proportion of providers differed from the guidelines for weight gain advice especially in obese patients, which may be due in part to the lack of consensus regarding an upper limit of weight gain in this group.13 The IOM guidelines were created at a time when inadequate gestational weight gain was of greatest clinical concern13; more recent data, however, have focused on the negative effects of gaining too much in pregnancy,16 including delivery complications,2 childhood overweight,5 and higher risk of postpartum weight retention and maternal obesity.17 This shift in clinical concern may underlie the current weight gain messages providers are recommending for their patients, particularly for obese mothers. As the IOM considers revising guidelines for weight gain in pregnancy, our results indicate a need for more clearly defined upper and lower limits of weight gain among obese women,18 as well as targeted dissemination of any revised recommendations to obstetric providers.
Provider personal factors, such as confidence and body satisfaction, proved important in determining the frequency with which obstetric providers followed practice recommendations for their obese pregnant patients. These findings are consistent with several prior studies linking provider personal characteristics, including confidence in counseling, healthy eating habits, and exercise, with self-reported counseling practices about exercise, nutrition, and weight loss.19–21 We are the first to describe, to our knowledge, associations between provider body satisfaction and obesity management, which was independent of actual provider BMI. This association may reflect a greater comfort level around issues of weight and nutrition among those with better body image. However, our findings should be interpreted cautiously, as we assessed body satisfaction with a single question; therefore, further evaluation with more detailed measures is required.
Similar to previous surveys of both obstetric and nonobstetric providers,9,22,23 the majority of respondents believed that obesity is an important health problem, and they attempted counseling about weight gain, diet, and physical activity. Interestingly, providers were least compliant with ACOG recommendations for referrals, including first trimester glucose tolerance testing and anesthesia consultation prior to delivery. As obese patients are at high risk for diabetes and for anesthetic complications at delivery, provider education seems appropriate to ensure that obese women receive adequate care. However, data do not yet exist about whether these practices in fact improve patient outcomes, therefore calling for more research to ensure these recommendations are in fact evidence based.
Our findings may be limited in their generalizability to obstetric providers practicing in different geographical regions or clinical settings where a large number of women are uninsured. We were most interested in querying providers about compliance with potentially modifiable ACOG clinical practice guidelines for improving healthy behaviors and controlling weight gain in obese women. We did not ask participants about their compliance with recommendations for cardiac evaluations or the use of prophylactic antibiotics during cesarean deliveries, also addressed in Committee Opinion No. 315.12 Our 8-point adherence scale was unweighted and, therefore, assumes that all components have equal weight in the management of obese pregnant patients, which may not be true. Additionally, only 58% of practicing providers completed surveys, which may have introduced selection bias. Providers who were more concerned about obesity in pregnancy may have been more likely to return surveys, most likely leading to overestimation of obesity importance or counseling practices in our study. Further, our relatively small sample may explain the modest number of provider factors found to be significantly associated with a higher adherence score. All data were from self-report; social desirability bias may have influenced survey responses, but our use of an anonymous survey was intended to minimize this bias. It is possible that the overall population of obstetricians in this practice are even less compliant with recommended care guidelines for their obese patients.
It is well established that obese patients who receive healthcare provider advice about weight loss or strategies for improving diet and exercise are more likely to report they are working on these areas,24 even in pregnancy.10,11 To improve obstetric provider compliance with management of their obese pregnant patients, our findings suggest a need for more education around BMI definitions and weight gain guidelines, along with strategies to address provider personal factors, such as confidence and body satisfaction, that may be important predictors of adherence to management recommendations. Incorporating continuing education related to assessment and management of obese pregnant patients into obstetric practices may be one method to improve both obstetric provider knowledge and self-efficacy. More work will need to follow to determine if such provider-based interventions lead to changes in gestational weight gain and related behaviors, resulting in enhanced maternal and offspring health.
Acknowledgments
We thank Dr. Matthew W. Gillman, Department of Ambulatory Care and Prevention, Harvard Medical School and Harvard Pilgrim Health Care, for his helpful suggestions about study design and manuscript revisions.
This study was supported by a grant from the Harvard Pilgrim Health Care Foundation. S.J.H. was supported by an institutional Ruth L. Kirschstein National Research Service Award (5 T32 HP11001-19) from the Health Resources and Services Administration and the Department of Ambulatory Care and Prevention at Harvard Medical School and Harvard Pilgrim Health Care in Boston, Massachusetts.
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.Ogden CL. Carroll MD. Curtin LR. McDowell MA. Tabak CJ. Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Catalano PM. Management of obesity in pregnancy. Obstet Gynecol. 2007;109:419–433. doi: 10.1097/01.AOG.0000253311.44696.85. [DOI] [PubMed] [Google Scholar]
- 3.Schieve LA. Cogswell ME. Scnalon KS. Maternal weight gain and preterm delivery: Differential effects by body mass index. Epidemiology. 1999;10:141–147. doi: 10.1097/00001648-199903000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Jain NJ. Denk CE. Kruse LK. Dandolu V. Maternal obesity: Can pregnancy weight gain modify risk of selected adverse pregnancy outcomes? Am J Perinatol. 2007;24:291–298. doi: 10.1055/s-2007-981432. [DOI] [PubMed] [Google Scholar]
- 5.Oken E. Taveras EM. Kleinman KP. Rich-Edwards JW. Gillman MW. Gestational weight gain and child adiposity at age 3 years. Am J Obstet Gynecol. 2007;196(322):e1–8. doi: 10.1016/j.ajog.2006.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolff S. Legarth J. Vangsgaard K. Toubro S. Astrup A. A randomized trial of the effects of dietary counseling on gestational weight gain and glucose metabolism in obese pregnant women. Int J Obes. 2008;32:495–501. doi: 10.1038/sj.ijo.0803710. [DOI] [PubMed] [Google Scholar]
- 7.Oken E. Ning Y. Rifas-Shiman SL. Radesky JS. Rich-Edwards JW. Gillman MW. Associations of physical activity and inactivity before and during pregnancy with glucose tolerance. Obstet Gynecol. 2006;108:1200–1207. doi: 10.1097/01.AOG.0000241088.60745.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Artal R. Catanzaro RB. Gavard JA. Mostello DJ. Friganza JC. A lifestyle intervention of weight-gain restriction: Diet and exercise in obese women with gestational diabetes mellitus. Appl Physiol Nutr Metab. 2007;32:596–601. doi: 10.1139/H07-024. [DOI] [PubMed] [Google Scholar]
- 9.Power ML. Cogswell ME. Schulkin J. Obesity prevention and treatment practices of U.S. obstetrician-gynecologists. Obstet Gynecol. 2006;108:961–968. doi: 10.1097/01.AOG.0000233171.20484.db. [DOI] [PubMed] [Google Scholar]
- 10.Stotland NE. Haas JS. Brawarsky P. Jackson RA. Fuentes-Afflick E. Escobar GJ. Body mass index, provider advice, and target gestational weight gain. Obstet Gynecol. 2005;105:633–638. doi: 10.1097/01.AOG.0000152349.84025.35. [DOI] [PubMed] [Google Scholar]
- 11.Cogswell ME. Scanlon KS. Fein SB. Schieve LA. Medically advised, mother's personal target, and actual weight gain during pregnancy. Obstet Gynecol. 1999;94:616–622. doi: 10.1016/s0029-7844(99)00375-0. [DOI] [PubMed] [Google Scholar]
- 12.Obesity in pregnancy. ACOG Committee Opinion No. 315. American College of Obstetrician and Gynecologists. Obstet Gynecol. 2005;106:671–675. doi: 10.1097/00006250-200509000-00054. [DOI] [PubMed] [Google Scholar]
- 13.Institute of Medicine. Nutrition during pregnancy. Washington, DC: National Academy Press; 1990. Subcommittee on Nutritional Status and Weight Gain during Pregnancy and Subcommittee on Dietary Intake and Nutrient Supplements during Pregnancy. [Google Scholar]
- 14.National Institutes of Health, National Heart, Lung, and Blood Institute . Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity: The evidence report. Rockville, MD: U.S. Department of Health and Human Services; 1998. [Google Scholar]
- 15.Block JP. DeSalvo KB. Fisher WP. Are physicians equipped to address the obesity epidemic? Knowledge and attitudes of internal medicine residents. Prev Med. 2003;36:669–675. doi: 10.1016/s0091-7435(03)00055-0. [DOI] [PubMed] [Google Scholar]
- 16.Viswanathan M. Siega-Riz AM. Moos MK, et al. Outcomes of maternal weight gain. Evidence Report/Technology Assessment. 2008;168:1–223. [PMC free article] [PubMed] [Google Scholar]
- 17.Olson CM. Achieving a healthy weight gain during pregnancy. Annu Rev Nutr. 2008;28:411–423. doi: 10.1146/annurev.nutr.28.061807.155322. [DOI] [PubMed] [Google Scholar]
- 18.Oken E. Excess gestational weight gain amplifies risk among obese mothers. Epidemiology. 2009;20:82–83. doi: 10.1097/EDE.0b013e3181880ef5. [DOI] [PubMed] [Google Scholar]
- 19.Frank E. Wright EH. Serdula MK. Elon LK. Baldwin G. Personal and professional nutrition-related practices of U.S. female physicians. Am J Clin Nutr. 2002;75:326–332. doi: 10.1093/ajcn/75.2.326. [DOI] [PubMed] [Google Scholar]
- 20.Frank E. Rothenberg R. Lewis C. Belodoff BF. Correlates of physicians' prevention-related practices. Findings from the Women Physicians' Health Study. Arch Fam Med. 2000;9:359–367. doi: 10.1001/archfami.9.4.359. [DOI] [PubMed] [Google Scholar]
- 21.Abramson S. Stein J. Schaufele M. Frates E. Rogan S. Personal exercise habits and counseling practices of primary care physicians: A national survey. Clin J Sports Med. 2000;10:40–48. doi: 10.1097/00042752-200001000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Hoppe R. Ogden J. Practice nurses' beliefs about obesity and weight related interventions in primary care. Int J Obes. 1997;21:141–146. doi: 10.1038/sj.ijo.0800379. [DOI] [PubMed] [Google Scholar]
- 23.Befort CA. Greiner KA. Hall S, et al. Weight-related perceptions among patients and physicians. How well do physicians judge patients' motivation to lose weight? J Gen Intern Med. 2006;21:1086–1090. doi: 10.1111/j.1525-1497.2006.00567.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jackson JE. Doescher MP. Saver BG. Hart LG. Trends in professional advice to lose weight among obese adults, 1994 to 2000. J Gen Intern Med. 2005;20:814–818. doi: 10.1111/j.1525-1497.2005.0172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]