Abstract
Objectives
Women diagnosed with gestational diabetes mellitus (GDM) are at high risk for future diabetes, with rates of GDM consistently higher in Hispanic than non-Hispanic white women. Currently recognized risk factors for GDM are absent in up to half of affected women, and studies addressing modifiable risk factors for GDM in Hispanic women are sparse.
Methods
Proyecto Buena Salud is an ongoing prospective cohort study of Hispanic women in Massachusetts designed to assess physical activity, psychosocial stress, and GDM risk. Bilingual interviewers recruit prenatal care patients early in pregnancy and assess activity, trait anxiety, perceived stress, and depressive symptoms using validated questionnaires.
Results
Baseline characteristics of the first 632 participants are presented. Women were predominantly young (69% <24 years), were unmarried (87%), and had low levels of education (48% had less than high school). Women with high acculturation were less likely to live with a partner (OR: 0.6, 95% CI 0.4-0.8) than women with low acculturation. Few participants met physical activity guidelines during pregnancy (5.2%). Levels of perceived stress (mean 26.9 ± 7.1), trait anxiety (mean 41.6 ± 10.4), and depressive symptoms (33.2%) were high.
Conclusions
Proyecto Buena Salud represents a high-risk population of pregnant Hispanic women who are predominantly inactive, with higher levels of perceived stress, trait anxiety, and depressive symptoms compared to predominantly non-Hispanic white cohorts studied earlier. Therefore, Proyecto Buena Salud provides a unique opportunity to prospectively evaluate modifiable risk factors for GDM. Findings will inform prenatal behavioral intervention programs designed to address modifiable GDM risk factors.
Introduction
Diabetes and obesity have reached epidemic proportions in the United States, with rates consistently higher in Hispanic than non-Hispanic white women.1,2 As the prevalence of diabetes continues to rise worldwide, it becomes increasingly important to identify high-risk populations and to implement strategies to delay or prevent diabetes onset.3,4 Women diagnosed with gestational diabetes mellitus (GDM) are at high risk for future diabetes, with 17%–63% developing type 2 diabetes within 5–16 years in different ethnic groups.5 Their children, in the long term, are at increased risk of obesity and glucose intolerance.6–8
Hispanic women have two to four times the risk of developing GDM compared with non-Hispanic white women.9 This is critical, as Hispanics are projected to have the highest birth rates for any minority group in the United States by the year 200910 and will be the largest minority group in the United States by the year 2030.11 Studies addressing modifiable risk factors for GDM in Hispanic women are sparse. Physical activity and psychosocial stress during pregnancy have been proposed as potential modifiable risk factors for GDM.
Prior studies of pregnancy recreational activity and GDM have suggested a protective role for recreational physical activity, with one case-control study observing a protective effect12 and others supporting this trend, although not significantly.13–16 The one prior study among Hispanic women was limited by a small number of cases but suggested that women with high household activity and sports/exercise in midpregnancy had a reduced risk of GDM compared with women with low levels.17 Although epidemiological studies have not examined the association between self-reported psychosocial stress and GDM risk, prior research has examined the association between stress and other maternal and fetal outcomes. Findings have been conflicting, predominantly restricted to non-Hispanic white or black women and limited by variations in measurement and analysis.18–20
Proyecto Buena Salud is an ongoing prospective study of physical activity, psychosocial stress, and mediators between these variables and risk of GDM in a cohort of prenatal care patients of Puerto Rican and Dominican descent. We present the study design and methods of Proyecto Buena Salud as well as the baseline characteristics of the first 632 participants.
Materials and Methods
Setting
Proyecto Buena Salud is based in the ambulatory obstetrical practices of Baystate Health, an integrated health system in Western Massachusetts. The study sites serve an ethnically and socioeconomically diverse population; approximately 57% are Hispanic (predominantly from Puerto Rico), 17% are African American, 23% are non-Hispanic white, and 3% are of other ethnicity.
Study overview
Recruitment began in January 2006. Bilingual interviewers recruited patients at a prenatal care visit early in pregnancy (up to 20 weeks gestation), informed them of the aims and procedures of the study, and obtained written informed consent as approved by the Institutional Review Boards of the University of Massachusetts-Amherst and Baystate Health. Interviews were conducted in Spanish or English (based on patient preference) in order to eliminate potential language or literacy barriers. Two subsequent interviews, conducted at the time of routine ultrasound (18–20 weeks gestation) and GDM screen (24–28 weeks gestation), will update information on these variables and collect information on dietary intake using the Hispanic Food Frequency Questionnaire.21 After delivery, medical records will be abstracted for medical and obstetrical history, including prepregnancy body mass index (BMI), previous history of GDM and family history of diabetes, clinical characteristics of the current pregnancy, incident GDM, and birth outcomes.
Eligibility
Eligibility was restricted to women of Puerto Rican or Dominican Republic heritage (Caribbean Islanders). Women who (1) were themselves born in the Caribbean Islands or (2) had a parent born in the Caribbean Islands or (3) had at least two grandparents born in the Caribbean Islands were included. Exclusion criteria included (1) current medications thought to adversely influence glucose tolerance, (2) multiple gestation, (3) history of diagnosis of diabetes, hypertension, heart disease, or chronic renal disease, and (4) <16 years of age or >40 years of age, as the association among physical activity, stress, and GDM may differ at the extremes of childbearing age.
Outcome variables
Women will be classified as having a pregnancy complicated by GDM if (1) two or more of the following plasma glucose concentrations obtained during the 100 g, 3-hour oral glucose tolerance test are abnormal according to American Diabetes Association criteria: fasting, 95 mg/dL; 1-hour, 180 mg/dL; 2-hour, 155 mg/dL; 3-hour, 140 mg/dL,22 (2) a 1-hour oral glucose tolerance test >180 mg/dL,23 or (3) elevated fasting (>105 mg/dL) or elevated 2-hour postprandial blood sugar (>120 mg/dL) in patients unwilling or unable to tolerate the oral glucose tolerance test.24 Baystate Obstetrical Practices routinely screen all prenatal care patients for GDM between 24 and 28 weeks of gestation using the 50 g, 1-hour glucose tolerance test. Those whose 1-hour plasma glucose levels from this test are >135 mg/dL are considered at increased risk for GDM and undergo the diagnostic 3-hour oral glucose tolerance test. Diagnosis of GDM is confirmed by an obstetrician, who reviews the medical records of each suspected case.
Primary exposure variables
Physical activity
Physical activity during early and prepregnancy (1 year before the pregnancy) was assessed at the baseline interview using a modified version of the Pregnancy Physical Activity Questionnaire (PPAQ), a semiquantitative questionnaire that assesses the duration, frequency, and intensity of total physical activity.25 Respondents select the category that best estimates the amount of time spent in 35 activities, including household and caregiving activities, occupational activities, sports and exercise, and transportation. The PPAQ was modified for the current study to be interviewer administered as opposed to self-administered by listing each activity item and response option in a concise grid format, as opposed to repeating response options vertically under each activity item.
The duration of time spent on each activity was multiplied by its intensity defined by the Compendium of Physical Activities26 to arrive at a measure of average weekly energy expenditure (MET-hrs/week) attributable to each activity. For those activities determined to have different intensities during pregnancy, a modified compendium value was used.27 The average number of MET-hrs/week was calculated according to intensity: light (<3 METs), moderate (3.0-5.9 METs), or vigorous (≥6.0 METs) and type: household/caregiving activities, occupational activities, sports/exercise, and transportation.
American College of Obstetricians and Gynecologists (ACOG) guidelines for physical activity in pregnancy recommend 30 minutes of moderate physical activity on most days for pregnant women, with no contraindications to physical activity in pregnancy.28 Therefore, women with ≥10 MET hrs/week in sports/exercise activities of moderate intensity or greater (i.e., 2.5 hrs/week multiplied by the minimum MET for moderate physical activity, 4 METs) were considered to have met the physical activity guidelines.
The PPAQ was validated using ActiGraph accelerometers (ActiGraph LLC, Fort Walton Beach, FL) at the study setting.25 Intraclass correlation coefficients used to measure reproducibility of the PPAQ were 0.78 for total activity, 0.82 for moderate activity, and 0.81 for vigorous activity and ranged from 0.83 for sports/exercise to 0.93 for occupational activity. Spearman correlations between the PPAQ and three published cutoff points used to classify Actigraph data ranged from 0.08 to 0.43 for total activity, 0.25 to 0.34 for vigorous activity, 0.20 to 0.49 for moderate activity, and −0.08 to 0.22 for light-intensity activity.
Psychosocial stress
Perceived stress, trait anxiety, and depressive symptoms were assessed during the baseline interview. Perceived stress was measured using Cohen's Perceived Stress Scale (PSS-14), which includes 14 items designed to address a person's sense of control over daily life demands.29 Each item is rated on a 5-point scale ranging from never (0) to almost always (4). Positively worded items are reverse scored, and the ratings are summed. Scores range from 0 to 56, with higher scores indicating more perceived stress. Internal consistency of the PSS as assessed by Cronbach's alpha was 0.85 in three samples tested by Cohen et al.29 and 0.78 in a general population study.30,31 Correlations were also observed with indices of depressive symptomatology (0.65 and 0.76). The European Spanish version of the PSS-14 demonstrated adequate reliability (internal consistency, alpha = 0.81, and test-retest, r = 0.73), validity (concurrent), and sensitivity.31
Trait anxiety was assessed using the Spielberger State-Trait Anxiety Inventory (STAI).32 The STAI trait anxiety scale measures relatively stable individual differences in anxiety proneness and contains 20 statements about how the respondent generally feels. Questions are based on a 4-point response scale ranging from almost never (1) to almost always (4), and a composite score is generated after reverse scoring appropriate items. Scores range from 20 to 80, with higher scores indicating higher levels of anxiety. Internal consistency ranges from 0.89 to 0.91.32 The instrument has been used previously in studies during the antenatal period.33 The Spanish version of the STAI was validated and adapted by TEA Editions.34
Depressive symptoms were assessed using the 10-item Edinburgh Postnatal Depression Scale (EPDS) available in English35 and Spanish.36 Each item asks how the woman has felt during the previous week and includes four categorical response options, ranging from; yes, most of the time to: no, not at all. Items are rated on a 4-point scale (0, 1, 2, 3) with a range of 0–30. Women with a score of ≥10 or who indicated any response other than never to the question describing thoughts of harming oneself were considered at risk for a depressive illness.35 As an alternative measure, we also considered an EPDS score >12 to indicate probable depression, as have others.37–40 The EPDS has been validated as a depression screening tool in pregnant and postpartum Hispanic women41 and has a sensitivity of 90%–100% and a specificity of 78%–88% for identification of major and minor depression.35
Potential confounding and mediating factors
At the baseline interview, interviewers collected sociodemographic factors, including age, education, annual household income, health insurance, marital status, living situation (i.e., with a partner), number of children and adults in the household including the index woman, language preference for speaking/reading, birthplace, and generation in the United States. Pregnancy behaviors included prepregnancy and early pregnancy alcohol consumption and cigarette smoking.
Degree of acculturation was assessed using the Psychological Acculturation Scale (PAS).42 The PAS consists of 10 items measuring an individual's sense of psychological attachment to and belonging within Anglo-American and Latino/Hispanic cultures. Item responses are scored on a 5-point Likert scale ranging from 1 (only Latino/Hispanic) to 5 (only Anglo-American) with a bicultural orientation defining its midpoint. We defined scores <3 as low acculturation and scores ≥3 as high acculturation. PAS scores have been correlated with migration history and patterns of Spanish and English language use in a sample of Puerto Rican females; correlations between PAS scores from the Spanish and English versions (r = 0.94) suggest a high degree of cross-language measurement equivalence.42
Data analysis
We examined frequency distributions of participant characteristics and evaluated the distributions by level of acculturation using chi-square tests or Fisher's exact test, in cases of small cell size. Descriptive statistics for stress and physical activity measures were calculated. Means and standard errors (SE) for sports/exercise activities for the study sample were corrected for measurement error based on a validation study in which we readministered the PPAQ to 44 women with implausible values. All physical activity variables were highly skewed, and we, therefore, present median as well as mean ± SE values. Statistical analysis was conducted using SAS 9.1.3 software by SAS Institute Inc. (SAS, Cary, NC).
Results
Demographics
Recruitment into the study began in January 2006, and we present the results from the first 632 women. Overall, 5% of Hispanic women approached refused to participate. The participants in this study were young, with low levels of education and income (Table 1). Almost 84% of participants were enrolled in public health insurance, 5% had no health insurance, and 87% were not married.
Table 1.
Baseline Participant Characteristics by Acculturation Level: Proyecto Buena Salud, Western Massachusetts, 2004–2008
| |
Total sample |
Acculturationa |
|
||
|---|---|---|---|---|---|
| n | % | Low (%) | High (%) | p value | |
| Total sample | 632 | 100.0 | 81.1 | 18.9 | |
| Age | 0.25 | ||||
| 16–24 | 425 | 69.1 | 80.2 | 19.8 | |
| 25–29 | 123 | 20.0 | 87.1 | 12.9 | |
| 30–34 | 45 | 7.3 | 78.6 | 21.4 | |
| 35–40 | 22 | 3.6 | 72.7 | 27.3 | |
| Educational status | 0.93 | ||||
| <High school | 284 | 47.8 | 80.1 | 19.9 | |
| High school graduate | 201 | 33.8 | 80.9 | 19.1 | |
| Some college/graduate | 109 | 18.4 | 84.5 | 15.5 | |
| Annual household income | 0.50 | ||||
| ≤$15,000 | 193 | 32.8 | 79.4 | 20.6 | |
| >$15,000–$30,000 | 92 | 15.6 | 77.8 | 22.2 | |
| >$30,000 | 47 | 8.0 | 80.9 | 19.1 | |
| Don't know/refused | 257 | 43.6 | 83.9 | 16.1 | |
| Health insurance | 0.53 | ||||
| No insurance | 27 | 4.8 | 74.0 | 26.0 | |
| Private insurance | 7 | 1.2 | 100.0 | 0.0 | |
| Public insurance | 453 | 79.8 | 81.1 | 18.9 | |
| Other | 78 | 13.7 | 84.2 | 15.8 | |
| Don't know/refused | 3 | 0.5 | 66.7 | 33.3 | |
| Marital status | 0.18 | ||||
| Single/divorced/separated/widowed | 509 | 86.6 | 80.1 | 19.9 | |
| Married | 73 | 12.4 | 88.9 | 11.1 | |
| Refused | 6 | 1.0 | 83.3 | 16.7 | |
| Live with spouse/partner | 0.005 | ||||
| No | 275 | 46.8 | 76.5 | 23.5 | |
| Yes | 313 | 53.2 | 85.6 | 14.4 | |
| Children (<18 years) in householdb | 0.46 | ||||
| 0 | 116 | 19.8 | 79.3 | 20.7 | |
| 1 | 205 | 35.0 | 81.8 | 18.2 | |
| 2 | 146 | 25.0 | 84.6 | 15.4 | |
| 3+ | 118 | 20.2 | 77.2 | 22.8 | |
| Adults (≥18 years) in householdb | 0.04 | ||||
| 1 | 140 | 23.7 | 74.3 | 25.7 | |
| 2 | 292 | 49.5 | 84.2 | 15.8 | |
| 3+ | 154 | 26.8 | 83.4 | 16.6 | |
| Language preference for speaking/reading | <0.001 | ||||
| English | 438 | 73.5 | 75.6 | 24.4 | |
| Spanish | 153 | 25.7 | 97.2 | 2.8 | |
| Other | 5 | 0.8 | 100.0 | 0.0 | |
| Birthplace | <0.001 | ||||
| Puerto Rico/Dominican Republic | 288 | 47.8 | 72.2 | 27.8 | |
| United States | 315 | 52.2 | 89.7 | 10.3 | |
| Generation in the U.S.c | <0.001 | ||||
| First generation | 288 | 47.9 | 89.7 | 10.3 | |
| Second generation | 277 | 46.1 | 72.2 | 27.8 | |
| Third generation | 36 | 6.0 | 71.0 | 29.0 | |
| Prepregnancy alcohol consumption | 0.82 | ||||
| None | 341 | 59.8 | 81.9 | 18.1 | |
| 1–5 drinks per month | 71 | 12.5 | 77.1 | 22.9 | |
| 5–12 drinks per month | 71 | 12.5 | 81.4 | 18.6 | |
| >12 drinks per month | 87 | 15.3 | 80.0 | 20.0 | |
| Early pregnancy alcohol consumption | 0.17 | ||||
| None | 537 | 97.1 | 81.5 | 18.5 | |
| Yes | 16 | 2.9 | 73.3 | 26.7 | |
| Prepregnancy cigarette smoking | 0.68 | ||||
| None | 190 | 49.6 | 80.5 | 19.5 | |
| ≤10 cigarettes per day | 103 | 26.9 | 76.5 | 23.5 | |
| >10 cigarettes per day | 90 | 23.5 | 80.7 | 19.3 | |
| Early pregnancy cigarette smoking | 0.47 | ||||
| None | 472 | 85.5 | 81.8 | 18.2 | |
| ≤10 cigarettes per day | 65 | 11.8 | 79.4 | 20.6 | |
| >10 cigarettes per day | 15 | 2.7 | 71.4 | 28.6 | |
Acculturation is measured by the Psychological Acculturation Scale and ranges from 1 to 5; score <3 = low acculturation.
Including the participant as appropriate: if <18 years, included as a child; if >18 years, included as an adult.
First generation: born in PR/DR or parent born in PR/DR; second generation: born in U.S. but parents born in PR/DR; third generation: born in U.S., parents born in U.S., grandparents born in PR/DR.
Note: numbers may not total to 632 due to missing data.
The mean acculturation score was 2.3 ± 0.7 on a possible scale of 1–5. Living situation, language preference, birthplace, generation in the United States, and number of adults living in the household all differed significantly by level of acculturation. Women with high levels of acculturation were 45% less likely to live with a partner (OR: 0.6, 95% CI 0.4-0.8) and 90% less likely to prefer Spanish (OR: 0.1, 95% CI 0.4-0.8) than women with low acculturation. As expected, women born in the continental United States or who were second- or third-generation residents of the continental United States were more likely to be highly acculturated compared to first-generation residents. Women with two or more adults in the household were less likely to be highly acculturated compared with those with one adult. A total of 40% of women reported prepregnancy alcohol consumption, which decreased to 3% with the onset of pregnancy. Similarly, whereas 50% of women reported smoking cigarettes prior to pregnancy, a total of 15% reported smoking in early pregnancy, with 3% smoking ≥10 cigarettes per day. Age, education, annual household income, health insurance, marital status, the number of children <18 years in the household, alcohol consumption, and cigarette smoking did not differ by acculturation status.
Physical activity
A total of 18.7% of participants met the ACOG guidelines for physical activity prior to pregnancy, and 5.2% of participants met these guidelines in early pregnancy (Table 2). In the prepregnancy period, mean total energy expenditure was 64.4 ± 37.2 MET-hrs/week, with the highest mean values reported in the domains of household/caregiving activities (29.3 ± 21.5 MET-hrs/week), followed by occupational activity, transportation, and sports/exercise.
Table 2.
Distribution of Physical Activity in Prepregnancy and Early Pregnancy: Proyecto Buena Salud, Western Massachusetts, 2004–2008
| |
Prepregnancy MET-hrs/week |
Early pregnancy MET-hrs/week |
Pre to Early ChangeaMET-hrs/week |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SE | Median | 25th–75th percentile | Mean | SE | Median | 25th–75th percentile | Mean | SE | Median | 25th–75th percentile | |
| Summary scores | ||||||||||||
| Total energy expenditure | 64.4 | 1.6 | 56.8 | 39.2, 80.0 | 42.4 | 1.1 | 37.0 | 23.6, 54.0 | −21.2 | 1.2 | −16.1 | −33.8, −3.8 |
| Total activity (light and above) | 52.6 | 1.4 | 44.9 | 29.4, 67.0 | 33.3 | 1.1 | 27.9 | 15.6, 44.0 | −19.2 | 1.1 | −13.3 | −30.8, −3.0 |
| Meeting PA guidelines (n, %)b | 112 | 18.7% | 30 | 5.2% | ||||||||
| By type | ||||||||||||
| Household/caregiving | 29.3 | 0.9 | 24.0 | 13.7, 39.6 | 20.8 | 0.7 | 16.6 | 8.8, 27.3 | −8.2 | 0.7 | −5.0 | −14.5, 0.8 |
| Occupational | 13.9 | 0.7 | 11.1 | 0, 18.6 | 7.5 | 0.4 | 2.1 | 0, 12.1 | −6.3 | 0.6 | −1.5 | −12.1, 0 |
| Sports/exercise | 6.5 | 0.3 | 3.8 | 2.0, 7.6 | 2.9 | 0.2 | 1.7 | 1.4, 2.9 | −3.6 | 0.3 | −1.3 | −3.9, 0 |
| Transportation | 7.0 | 0.3 | 4.7 | 2.2, 8.6 | 4.9 | 0.2 | 3.7 | 1.5, 7.1 | −2.2 | 0.3 | −0.5 | −4.0, 0.8 |
Within-woman change in physical activity based on women with data available for both measures.
≥10 METs per week of sports and exercise of moderate intensity or greater.
Women reported decreases in each domain of activity (household/caregiving, occupational, sports/exercise, and transportation) with the onset of pregnancy, with an overall within-woman change in total energy expenditure of −21.2 ± 27.7 MET-hrs/week. The largest within-woman change was for sports/exercise activity (−8.2 ± 16.6 MET-hrs/week), and the smallest within-woman change was for transportation (−2.2 ± 7.1 MET-hrs/week).
Psychosocial stress
The mean level of psychosocial stress, as measured by the PSS was 26.9 ± 7.1 (range 5–48) (Table 3). A mean score of 41.6 ± 10.4 (range 20–76) was observed on the STAI. The mean score on the EPDS was 9.7 ± 5.9 (range 0–26). A total of 48.8% of participants were classified as at risk for depressive illness (EPDS scores ≥10), and 33.2% were classified as having probable depression (EPDS scores >12).
Table 3.
Distribution of Psychosocial Stress in Early Pregnancy: Proyecto Buena Salud, Western Massachusetts, 2004–2008
| |
Early pregnancy |
|
|---|---|---|
| Mean | SD | |
| Perceived Psychosocial Stressa | 26.9 | 7.1 |
| Quartile 1 | 17.4 | 3.3 |
| Quartile 2 | 24.0 | 1.5 |
| Quartile 3 | 29.0 | 1.4 |
| Quartile 4 | 35.8 | 3.5 |
| Spielberger Trait Anxietyb | 41.6 | 10.4 |
| Quartile 1 | 28.8 | 3.3 |
| Quartile 2 | 36.8 | 2.0 |
| Quartile 3 | 44.6 | 2.3 |
| Quartile 4 | 55.1 | 1.3 |
| Edinburgh Depression Scalec | 9.7 | 5.9 |
| At risk for depressive illnessd (n, %) | 269 | 48.8 |
| Probable depressione (n, %) | 183 | 33.2 |
Perceived Stress Scale ranges from 0 to 56.
Speilberger Trait Anxiety ranges from 20 to 80.
Edinburgh Depression Scale ranges from 0 to 30.
Defined as ≥10 or indicate any response other than never to the question describing thoughts of harming oneself.
Defined as >12.
Discussion
Proyecto Buena Salud has identified and enrolled a large number of women of Puerto Rican and Dominican Republic heritage who represent a wide range of sociodemographic, behavioral, and acculturation levels. Overall, the population is at high risk, with the majority being young, unmarried, and with low levels of income and education. Women who were highly acculturated were less likely to live with a partner or to prefer Spanish than women with low acculturation. Sociodemographic factors and alcohol consumption and cigarette smoking did not differ by acculturation status.
Participants reported a variety of behaviors that are potential risk factors for GDM. For example, few participants met physical activity guidelines. Leiferman and Evenson43 used data collected from the year 2000 Behavioral Risk Factor Surveillance System to evaluate the prevalence of meeting physical activity guidelines (defined consistently with ACOG guidelines) among 1979 pregnant women (12% Hispanic). The authors found that 10.6% ± 3.0% of Hispanic pregnant women met guidelines compared with 16.7% ± 1.5% of non-Hispanic white pregnant women. Pereira et al.44 assessed participation in total physical activity among 1442 participants of Project Viva (4.9% Hispanic). A total of 21.6% of pregnant women were found to be insufficiently active during pregnancy, defined as <150 minutes/week of total leisure time physical activity, including walking, light to moderate, and vigorous physical activity; findings were not reported separately for Hispanic women. In the current study, we observed that 5.2% of women met ACOG guidelines. Differences in study findings are due to racial/ethnic and sociodemographic differences between study samples as well as variation in the definition of meeting activity guidelines.
Participants reported higher levels of perceived stress, trait anxiety, and depressive symptoms than those reported by prior studies among predominantly non-Hispanic white populations. Laraia et al.45 used the PSS-14 to evaluate stress before 20 weeks gestation among 606 participants (7.9% other racial/ethnic groups) who had incomes ≤400% of the poverty line. Mean PSS-14 scores were 22.3 ± 8.14. We observed a mean of 26.9 ± 7.1 (range 5–48) in our sample of Hispanic women. Dayan et al.46 used a self-administered STAI among a sample of 634 pregnant women in France between the 20th and 28th week of gestation and observed a mean value for trait anxiety of 38.8 ± 9.2 (range 20–73). Daniells et al.47 evaluated trait anxiety in a sample of 50 pregnant women with normal glucose tolerance in Australia at 30 weeks gestation and found a mean value of 38.3 ± 10.2 in this group. Faisal-Cury and Rossi Menezes found mean values of 40.8 ± 9.7 in a sample of 432 pregnant women in Sao Paolo, Brazil. In their cohort of low-income women, Laraia et al.45 observed mean values of 39.0 ± 11.4 (range 20–77) for trait anxiety. We observed a somewhat higher mean value in the current study of 41.6 ± 10.4, with a range of 20–76.
In terms of prenatal depressive symptoms, Rich-Edwards et al.40 found that 9% of 1662 participants in Project Viva had EPDS scores >12 at midpregnancy. Hispanic women (5% of the sample) had a higher prevalence of depressive symptoms (16%) compared with non-Hispanic white mothers (7%). Evans et al.38 assessed depressive symptoms in a prospective longitudinal study of women in England (n = 8323); a total of 11.8% of women scored >12 on the EPDS at 18 weeks gestation (7.0 ± 4.9). In their cohort of French women, Dayan et al.49 observed a mean score of 7.2 ± 5.6 on the EPDS, with 14.5% of participants scoring >14. Our finding that 48.8% of participants scored ≥10 on the EPDS and 33.2% scored >12 is substantially higher than in these prior studies; however, these studies included few Hispanic women and were conducted in women of predominantly high socioeconomic status. Studies using other depression assessment tools have reported prevalence rates ranging from 25% to 50% among low-income prenatal populations,50–52 supporting prior findings that differences in rates may reflect demographic differences that are, in turn, related to depressive symptoms (e.g., age, marital status, social support, and other cultural differences, including acculturation).40
Strengths of Proyecto Buena Salud include prospective information on the duration, frequency, and intensity of total physical activity (household, occupational, and recreational) and psychosocial stress (perceived stress, anxiety, and depressive symptoms) during pregnancy. Other innovations of the study include the use of a physical activity questionnaire designed for pregnancy and validated in the study population that can characterize threshold and dose-response effects, as well as the use of psychosocial stress scales validated in Hispanic populations. Finally, the high participation rates are also study strengths.
This study is subject to several limitations. Physical activity and psychosocial stress were based on self-report and, therefore, were subject to misclassification. Because of the prospective nature of the study, however, reporting of these variables should not be influenced by GDM diagnosis. We did not collect information on cultural attitudes to exercise and dieting, which may also be important factors in this population. Our use of a self-reported measure of probable depression, as opposed to a clinical diagnosis, is also a limitation. Although the EPDS has been validated among Hispanic pregnant women, it is possible that cultural or economic factors may lead to an underreporting or overreporting of depressive symptoms. Social desirability bias may particularly affect minority53 and lower socioeconomic54 participants. However, a score ≥12 on the EPDS is widely used to indicate probable depressive disorder.
Because subjects were recruited at their prenatal care visits (up to 20 weeks gestation), we excluded, by definition, high-risk women who do not attend prenatal care. However, our study population included a sizable proportion of women who were at high risk based on socioeconomic factors and ethnicity. In addition, 2006 vital statistics data for births in Springfield, Massachusetts, indicate that 93.3% of Hispanics begin prenatal care by the second trimester.55
Prior and ongoing pregnancy cohort studies of physical activity and GDM have been conducted among predominantly higher income, non-Hispanic white populations.13,14 More importantly, to our knowledge, prior studies have not evaluated the association between psychosocial stress and GDM.
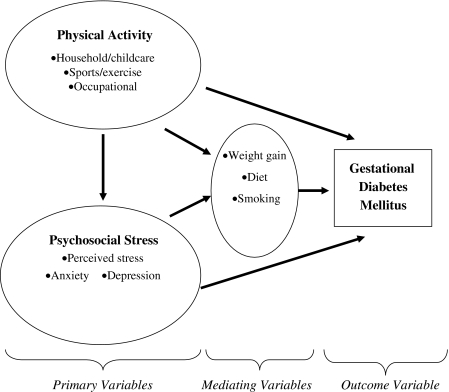
Future directions for Proyecto Buena Salud are 2-fold. The first is to determine if physical activity in early to midpregnancy is prospectively associated with risk of GDM. We hypothesize that an increasing dose of physical activity (the product of frequency, intensity, and duration) will be associated with a decreased risk of GDM (Fig. 1). We also hypothesize that physical activity will indirectly affect GDM risk through decreasing maternal weight gain and reducing psychosocial stress and cigarette smoking. The second direction is to determine if psychosocial stress in early to midpregnancy is prospectively associated with risk of GDM. We hypothesize that higher levels of self-reported psychosocial stress will be associated with increased risk of GDM. We also hypothesize that psychosocial stress will indirectly affect GDM risk through negatively impacting diet and increasing cigarette smoking.
FIG. 1.
Conceptual model, Proyecto Buena Salud, Western Massachusetts, 2006–2008.
Conclusions
In summary, Proyecto Buena Salud represents a group of Hispanic women who are predominantly inactive, with higher levels of perceived stress, trait anxiety, and depressive symptoms compared with prior predominantly non-Hispanic white cohorts. Therefore, Proyecto Buena Salud provides the unique opportunity to prospectively evaluate modifiable risk factors for GDM. Early maternal lifestyle modifications in pregnancies at risk for GDM might offer the opportunity not only for reduction in risk of type 2 diabetes in the mother but also for risk of diabetes and obesity in children. The impact of these maternal lifestyle modifications is likely to be greatest in ethnic groups, such as Hispanics, with consistently high incidence rates of GDM.
Acknowledgments
This work was supported by NIH grant NIDDK064902.
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.King H. Aubert RE. Herman WH. Global burden of diabetes, 1995–2025: Prevalence, numerical estimates, and projections. Diabetes Care. 1998;21:1414–1431. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 2.Spiegel AM. Executive summary of the Strategic Plan for National Institutes of Health Obesity Research. Am J Clin Nutr. 2005;82(Suppl 1):211–214. doi: 10.1093/ajcn/82.1.221S. [DOI] [PubMed] [Google Scholar]
- 3.Reichard P. Nilsson BY. Rosenqvist U. The effect of long-term intensified insulin treatment on the development of microvascular complications of diabetes mellitus. N Engl J Med. 1993;329:304–309. doi: 10.1056/NEJM199307293290502. [DOI] [PubMed] [Google Scholar]
- 4.U.K. Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–853. [PubMed] [Google Scholar]
- 5.Kjos SL. Postpartum care of the woman with diabetes. Clin Obstet Gynecol. 2000;43:75–86. doi: 10.1097/00003081-200003000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Pettitt DJ. Knowler WC. Long-term effects of the intrauterine environment, birth weight, and breast-feeding in Pima Indians. Diabetes Care. 1998;21(Suppl 2):B138–141. [PubMed] [Google Scholar]
- 7.Silverman BL. Rizzo TA. Cho NH. Metzger BE. Long-term effects of the intrauterine environment. The Northwestern University Diabetes in Pregnancy Center. Diabetes Care. 1998;21(Suppl 2):B142–149. [PubMed] [Google Scholar]
- 8.Vohr BR. McGarvey ST. Tucker R. Effects of maternal gestational diabetes on offspring adiposity at 4–7 years of age. Diabetes Care. 1999;22:1284–1291. doi: 10.2337/diacare.22.8.1284. [DOI] [PubMed] [Google Scholar]
- 9.Sepe SJ. Connell FA. Geiss LS. Teutsch SM. Gestational diabetes. Incidence, maternal characteristics, and perinatal outcome. Diabetes. 1985;34(Suppl 2):13–16. doi: 10.2337/diab.34.2.s13. [DOI] [PubMed] [Google Scholar]
- 10.Simpson CE. Closing the gap. Vol. 3. Washington, DC: Office of Minority Health, U.S. Department of Health and Human Services; 1998. Reaffirming our commitment to improving health services for Hispanics. [Google Scholar]
- 11.Ramirez AG. Villarreal R. Suarez L. Flores ET. The emerging Hispanic population: A foundation for cancer prevention and control. J Natl Cancer Inst Monogr. 1995;18:1–9. [PubMed] [Google Scholar]
- 12.Dempsey JC. Butler CL. Sorensen TK, et al. A case-control study of maternal recreational physical activity and risk of gestational diabetes mellitus. Diabetes Res Clin Pract. 2004;66:203–215. doi: 10.1016/j.diabres.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 13.Dempsey JC. Sorensen TK. Williams MA, et al. Prospective study of gestational diabetes mellitus risk in relation to maternal recreational physical activity before and during pregnancy. Am J Epidemiol. 2004;159:663–670. doi: 10.1093/aje/kwh091. [DOI] [PubMed] [Google Scholar]
- 14.Oken E. Ning Y. Rifas-Shiman SL. Radesky JS. Rich-Edwards JW. Gillman MW. Associations of physical activity and inactivity before and during pregnancy with glucose tolerance. Obstet Gynecol. 2006;108:1200–1207. doi: 10.1097/01.AOG.0000241088.60745.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dyck R. Klomp H. Tan LK. Turnell RW. Boctor MA. A comparison of rates, risk factors, and outcomes of gestational diabetes between aboriginal and non-aboriginal women in the Saskatoon health district. Diabetes Care. 2002;25:487–493. doi: 10.2337/diacare.25.3.487. [DOI] [PubMed] [Google Scholar]
- 16.Dye TD. Knox KL. Artal R. Aubry RH. Wojtowycz MA. Physical activity, obesity, and diabetes in pregnancy. Am J Epidemiol. 1997;146:961–965. doi: 10.1093/oxfordjournals.aje.a009223. [DOI] [PubMed] [Google Scholar]
- 17.Chasan-Taber L. Schmidt MD. Pekow P, et al. Physical activity and gestational diabetes mellitus among Hispanic women. J Womens Health. 2008;17:999–1008. doi: 10.1089/jwh.2007.0560. [DOI] [PubMed] [Google Scholar]
- 18.Dole N. Savitz DA. Hertz-Picciotto I. Siega-Riz AM. McMahon MJ. Buekens P. Maternal stress and preterm birth. Am J Epidemiol. 2003;157:14–24. doi: 10.1093/aje/kwf176. [DOI] [PubMed] [Google Scholar]
- 19.Hoffman S. Hatch MC. Stress, social support and pregnancy outcome: A reassessment based on recent research. Paediatr Perinat Epidemiol. 1996;10:380–405. doi: 10.1111/j.1365-3016.1996.tb00063.x. [DOI] [PubMed] [Google Scholar]
- 20.Lobel M. Conceptualizations, measurement, and effects of prenatal maternal stress on birth outcomes. J Behav Med. 1994;17:225–272. doi: 10.1007/BF01857952. [DOI] [PubMed] [Google Scholar]
- 21.Tucker KL. Bianchi LA. Maras J. Bermudez OI. Adaptation of a food frequency questionnaire to assess diets of Puerto Rican and non-Hispanic adults. Am J Epidemiol. 1998;148:507–518. doi: 10.1093/oxfordjournals.aje.a009676. [DOI] [PubMed] [Google Scholar]
- 22.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2004;27(Suppl 1):S5–S10. doi: 10.2337/diacare.27.2007.s5. [DOI] [PubMed] [Google Scholar]
- 23.Landy HJ. Gomez-Marin O. O'Sullivan MJ. Diagnosing gestational diabetes mellitus: Use of a glucose screen without administering the glucose tolerance test. Obstet Gynecol. 1996;87:395–400. doi: 10.1016/0029-7844(95)00460-2. [DOI] [PubMed] [Google Scholar]
- 24.Atilano LC. Lee-Parritz A. Lieberman E. Cohen AP. Barbieri RL. Alternative methods of diagnosing gestational diabetes mellitus. Am J Obstet Gynecol. 1999;181:1158–1161. doi: 10.1016/s0002-9378(99)70100-6. [DOI] [PubMed] [Google Scholar]
- 25.Chasan-Taber L. Schmidt MD. Roberts DE. Hosmer D. Markenson G. Freedson PS. Development and validation of a Pregnancy Physical Activity Questionnaire. Med Sci Sports Exerc. 2004;36:1750–1760. doi: 10.1249/01.mss.0000142303.49306.0d. [DOI] [PubMed] [Google Scholar]
- 26.Ainsworth BE. Haskell WL. Whitt MC, et al. Compendium of physical activities: An update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(Suppl 9):S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 27.Chasan-Taber L. Freedson PS. Roberts DE. Schmidt MD. Fragala MS. Energy expenditure of selected household activities during pregnancy. Res Q Exerc Sport. 2007;78:133–137. doi: 10.1080/02701367.2007.10599410. [DOI] [PubMed] [Google Scholar]
- 28.ACOG Committee Obstetric Practice. ACOG committee opinion. Number 267, January 2002: Exercise during pregnancy and the postpartum period. Obstet Gynecol. 2002;99:171–173. doi: 10.1016/s0029-7844(01)01749-5. [DOI] [PubMed] [Google Scholar]
- 29.Cohen S. Kamarck T. Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 30.Cohen LH. McGowan J. Fooskas S. Rose S. Positive life events and social support and the relationship between life stress and psychological disorder. Am J Community Psychol. 1984;12:567–587. doi: 10.1007/BF00897213. [DOI] [PubMed] [Google Scholar]
- 31.Remor E. Psychometric properties of a European Spanish version of the Perceived Stress Scale (PSS) Spanish J Psychol. 2006;9:86–93. doi: 10.1017/s1138741600006004. [DOI] [PubMed] [Google Scholar]
- 32.Spielberger CD. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 33.Hickey CA. Cliver SP. Goldenberg RL. McNeal SF. Hoffman HJ. Relationship of psychosocial status to low prenatal weight gain among nonobese black and white women delivering at term. Obstet Gynecol. 1995;86:177–183. doi: 10.1016/0029-7844(95)00161-j. [DOI] [PubMed] [Google Scholar]
- 34.Spielberger CD. Gorsuch RL. Lushene RE. Manual STAI. Cuestionario de Ansiedad Estado Rasgo. Técnicus Especialistas Asociados (TEA), Madrid, 1982.
- 35.Cox JL. Holden JM. Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 36.Jadresic E. Araya R. Jara C. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Chilean postpartum women. J Psychosom Obstet Gynaecol. 1995;16:187–191. doi: 10.3109/01674829509024468. [DOI] [PubMed] [Google Scholar]
- 37.Righetti-Veltema M. Conne-Perréard E. Bousquet A. Manzano J. Risk factors and predictive signs of postpartum depression. J Affect Disord. 1998;49:167–180. doi: 10.1016/s0165-0327(97)00110-9. [DOI] [PubMed] [Google Scholar]
- 38.Evans J. Heron J. Francomb H. Oke S. Golding J. Cohort study of depressed mood during pregnancy and after childbirth. BMJ. 2001;323:257–260. doi: 10.1136/bmj.323.7307.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Warner R. Appleby L. Whitton A. Faragher B. Demographic and obstetric risk factors for postnatal psychiatric morbidity. Br J Psychiatry. 1996;168:607–611. doi: 10.1192/bjp.168.5.607. [DOI] [PubMed] [Google Scholar]
- 40.Rich-Edwards JW. Kleinman K. Abrams A, et al. Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. J Epidemiol Community Health. 2006;60:221–227. doi: 10.1136/jech.2005.039370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yonkers KA. Ramin SM. Rush AJ, et al. Onset and persistence of postpartum depression in an inner-city maternal health clinic system. Am J Psychiatry. 2001;158:1856–1863. doi: 10.1176/appi.ajp.158.11.1856. [DOI] [PubMed] [Google Scholar]
- 42.Tropp LR. Erkut S. Coll CG. Alarcon O. Vazquez Garcia HA. Psychological acculturation: Development of a new measure for Puerto Ricans on the U.S. mainland. Educ Psychol Measurement. 1999;59:351–367. doi: 10.1177/00131649921969794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Leiferman JA. Evenson KR. The effect of regular leisure physical activity on birth outcomes. Matern Child Health J. 2003;7:59–64. doi: 10.1023/a:1022545718786. [DOI] [PubMed] [Google Scholar]
- 44.Pereira MA. Rifas-Shiman SL. Kleinman KP. Rich-Edwards JW. Peterson KE. Gillman MW. Predictors of change in physical activity during and after pregnancy: Project Viva. Am J Prev Med. 2007;32:312–319. doi: 10.1016/j.amepre.2006.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Laraia BA. Siega-Riz AM. Gundersen C. Dole N. Psychosocial factors and socioeconomic indicators are associated with household food insecurity among pregnant women. J Nutr. 2006;136:177–182. doi: 10.1093/jn/136.1.177. [DOI] [PubMed] [Google Scholar]
- 46.Dayan J. Creveuil C. Herlicoviez M, et al. Role of anxiety and depression in the onset of spontaneous preterm labor. Am J Epidemiol. 2002;155:293–301. doi: 10.1093/aje/155.4.293. [DOI] [PubMed] [Google Scholar]
- 47.Daniells S. Grenyer BFS. Davis WS. Coleman KJ. Burgess JP. Moses RG. Gestational diabetes mellitus: Is a diagnosis associated with an increase in maternal anxiety and stress in the short and intermediate term? Diabetes Care. 2003;26:385–389. doi: 10.2337/diacare.26.2.385. [DOI] [PubMed] [Google Scholar]
- 48.Faisal-Cury A. Rossi Menezes P. Prevalence of anxiety and depression during pregnancy in a private setting sample. Arch Womens Mental Health. 2007;10:25–32. doi: 10.1007/s00737-006-0164-6. [DOI] [PubMed] [Google Scholar]
- 49.Dayan J. Creveuil C. Marks MN, et al. Prenatal depression, prenatal anxiety, and spontaneous preterm birth: A prospective cohort study among women with early and regular care. Psychosom Med. 2006;68:938–946. doi: 10.1097/01.psy.0000244025.20549.bd. [DOI] [PubMed] [Google Scholar]
- 50.Hobfoll SE. Ritter C. Lavin J. Hulsizer MR. Cameron RP. Depression prevalence and incidence among inner-city pregnant and postpartum women. J Consult Clin Psychol. 1995;63:445–453. doi: 10.1037//0022-006x.63.3.445. [DOI] [PubMed] [Google Scholar]
- 51.Séguin L. Potvin L. St-Denis M. Loiselle J. Chronic stressors, social support, and depression during pregnancy. Obstet Gynecol. 1995;85:583–589. doi: 10.1016/0029-7844(94)00449-N. [DOI] [PubMed] [Google Scholar]
- 52.Chung EK. McCollum KF. Elo IT. Lee HJ. Culhane JF. Maternal depressive symptoms and infant health practices among low-income women. Pediatrics. 2004;113:e523–e529. doi: 10.1542/peds.113.6.e523. [DOI] [PubMed] [Google Scholar]
- 53.Bardwell WA. Dimsdale JE. The impact of ethnicity and response bias on the self-report of negative affects. J Appl Biobehav Res. 2001;6:27–38. [Google Scholar]
- 54.Welte JW. Russell M. Influence of socially desirable responding in a study of stress and substance abuse. Alcoholism Clin Exp Res. 1993;17:758–761. doi: 10.1111/j.1530-0277.1993.tb00836.x. [DOI] [PubMed] [Google Scholar]
- 55.The Massachusetts Department of Public Health. Massachusetts Community Health Information Profile (MassCHIP) 1995–2008. October 29, 2008.