Abstract
In 1999, the Texas Tech University Health Sciences Center School of Pharmacy expanded its Dallas/Fort Worth presence by creating a regional campus for pharmacy students in their third and fourth years (P3 and P4 years) of the program. This expansion was driven by the need for additional practice sites. The VANTHCS was an obvious choice for the school due to the similarity of missions for clinical practice, education, and research. The VANTHCS and pharmacy school renovated a 4,000 square foot building, which includes classrooms, conference rooms, a student lounge, and faculty offices (expanded to 8,000 square feet in 2003). To date, the school has invested $1 million in the building. From a practice perspective, VANTHCS purchases faculty professional services from the school to augment its clinical specialist staff. These professional practice contracts provide VANTHCS with 12 additional clinical pharmacy specialists serving 50% of their time in multiple specialty areas. The collaboration has also allowed for expansion of clinical teaching, benefitting both institutions. In addition to the pharmacy student interns on P3 and P4 practice experiences, the collaboration allows for 8 to 10 postgraduate pharmacy residents to train with VANTHCS clinical specialists and school faculty members each year. The VANTHCS/pharmacy school collaboration has clearly enhanced the ability of both institutions to exceed their teaching, research, and practice goals in a cost-effective manner.
Keywords: veterans affairs health system, partnership, practice experiences
INTRODUCTION
The Department of Veterans Affairs (VA) has been an important partner to many pharmacy schools because of its progressive clinical pharmacy practice model and its similar tri-part mission of practice, teaching, and research. Many schools utilize the VA as a site to precept students and for a few faculty members to practice. Most schools of pharmacy have failed to take full advantage of the opportunities offered by the VA. The major, intentional intertwining of the Veterans Affairs North Texas Health Care System (VANTHCS) and the Texas Tech school of pharmacy has resulted in the Dallas school of pharmacy campus being located on VANTHCS campus, 12 faculty members fulfilling practice contracts with VANTHCS, 8-10 residents at the VANTHCS in postgraduate year (PGY) 1 and PGY 2 programs, and 90 pharmacy students training at the VANTHCS campus.
The purpose of this paper is to describe the implementation of the unique collaboration between the pharmacy school and VANTHCS in order to address the varied challenges of both institutions with an integrative practice collaboration model. This type of collaboration may serve as a framework for other pharmacy schools, VA medical centers, or health systems to manage these same challenges.
Issues Facing the VA and Academia
The VA continues to experience a demand for its medical services due to ongoing military conflicts with increasingly complex combat injuries, coupled with the aging of the existing veteran population. In addition, VA has had a shortage of pharmacists. In FY 2006, VA pharmacists had an attrition rate of 7% from resignations, retirements, and other separations.1 Based on anticipated vacancies and the VA's future mission needs, pharmacy has been identified as one of the top 10 priority occupations for recruitment and retention efforts.1 Because VA pharmacy residents are excellent candidates for VA employment, VA plans to expand its existing pharmacy residency programs to assist with recruitment of these young health care professionals.
The VA uses several development models for pharmacy residency programs: (1) directly sponsoring the accredited pharmacy residency; (2) participating in integrated pharmacy residency programs sponsored through educational institutions; and (3) the educational consortium sponsoring the pharmacy residency. Every year, the VA allocates approximately $19 million to provide training stipends for 400 pharmacy residents.
Colleges and schools of pharmacy are also challenged to meet the increased need for pharmacists. Some of the challenges facing schools in addressing this problem include the faculty shortage as well as the capacity of practice sites to accommodate healthcare professionals in training.2,3 The VA represents an excellent practice setting to train both doctor of pharmacy (PharmD) candidates and postgraduate pharmacy residents and represents an important partner in alleviating both pharmacist and faculty shortages.
History and Organization
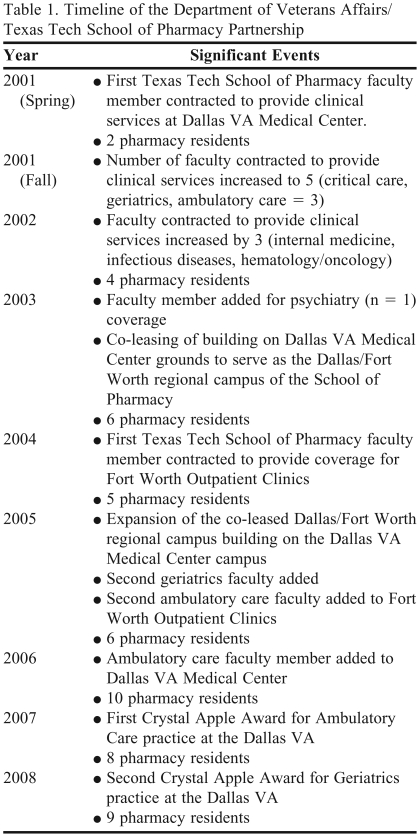
In 1998, the VANTHCS administrative director recognized the opportunities afforded by a collaborative relationship with a school of pharmacy. As a result, the school and VANTHCS entered into an agreement to renovate physical facilities on the VANTHCS campus and to use the hospital and clinics as its primary teaching sites. In 1999, the school expanded its Dallas/Fort Worth presence by creating a regional campus for P3 and P4 students. This expansion decision was driven by the need for additional practice sites in anticipation of expanding class size. The VANTHCS was an obvious choice for the school's regional campus due to the similarity of missions. A timeline of the significant events in the partnership between the VANTHCS and school is outlined in Table 1.
Table 1.
Timeline of the Department of Veterans Affairs/Texas Tech School of Pharmacy Partnership
School of Pharmacy Campus.
The Dallas VANTHCS and school renovated a 4,000 square foot building that included classrooms, small group conference rooms, a student lounge, and faculty offices. While the school campus could have been located anywhere in the Dallas/Fort Worth metroplex, there were distinct advantages to both the school and VANTHCS having the campus located on VANTHCS grounds. Locating the Dallas campus on VANTHCS grounds has resulted in the free flow of students, residents, and faculty members across both institutions and has increased opportunities for collaboration. Being able to walk from VANTHCS clinical buildings to the school provides faculty members, residents, and candidates increased work time by eliminating the drive to the school campus. Any other suitable campus location in the Dallas/Fort Worth metroplex would have required a 30-minute or longer drive to and from VANTHCS. Faculty members’ offices are equipped with VANTHCS computers, allowing faculty access to VANTHCS's electronic medical records, providing multiple advantages to both the school and VANTHCS. The school is able to maximize faculty members’ work time by allowing them to work on clinical care activities at the school and easily transition between clinical consults and other faculty duties. The VANTHCS is also able to maximize use of its clinical buildings to see patients with school faculty having VANTHCS computers in their offices. This also helps to minimize any negative effect of education on clinical care because in-depth academic discussions of patient issues can occur in school faculty offices outside of rounds and typical patient care.
Again as a collaborative effort between VANTHCS and the school, the building was expanded to 8,000 square feet in 2003. This expansion was in response to the increased class size of the school as well as the increased number of faculty members that were also fulfilling professional service contracts at VANTHCS. The financial arrangements require the school to lease the building from VANTHCS. To date, the school has invested $1 million in the building through lease improvements and payments.
Professional Service Contracts.
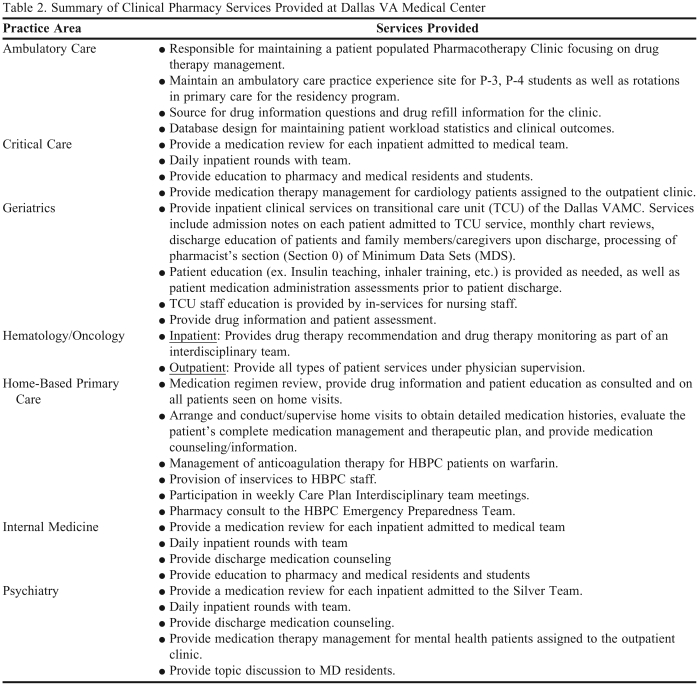
VANTHCS contracts faculty professional services from the school to augment its clinical specialist staff. While this augmentation began with 1 faculty member, it has grown to 12 faculty members and currently represents a 50% increase in the number of clinical specialist staff available to VANTHCS. School faculty members are 100% funded by the school and are responsible for fulfilling VANTHCS's school contracts as determined by VANTHCS and school administration. These professional practice contracts provide VANTHCS with 12 additional clinical pharmacy specialists serving 50% of their time in multiple specialty areas including ambulatory care, cardiology/critical care, geriatrics, hematology/oncology, internal medicine, and psychiatry (Table 2). School faculty members fulfilling practice contracts at VANTHCS undergo the same credentialing processes as VANTHCS clinical pharmacy specialists, including submitting a record of education/employment history and professional qualifications, undergoing a criminal background check, providing 3 character references, and submitting fingerprints. School faculty members have level 3 pharmacist privileges, which include the opportunity to submit a scope of practice that includes the ability to independently prescribe medications and order laboratory tests. All school faculty members in the outpatient setting have a scope of practice and independently see patients in anticoagulation, cardiology, hematology/oncology, infectious diseases, or pharmacotherapy clinics. School faculty members in the inpatient setting have scopes of practice if needed to conduct their practice activities.
Table 2.
Summary of Clinical Pharmacy Services Provided at Dallas VA Medical Center
The professional service contracts provide a significant source of income to enhance educational programs and build infrastructure for the school through the Pharmacy Income Plan. The Pharmacy Income Plan, approved by the University's Board of Regents, allocates portions of income from pharmacy practice contracts to the Health Sciences Center as well as school program and development funds. Professional service contracts also supplement faculty members’ salaries in order to be competitive with the private sector.
School faculty members are required by the VANTHCS contract to submit online every 2 weeks the number of hours worked. The hours must be electronically approved by the school faculty members, VANTHCS pharmacy administration, and school administration to count toward the contract requirements.
The regional dean is charged with minimizing conflicts between VANTHCS and the school of pharmacy. Conflicts do occur from time to time and are managed on a case-by-case basis. Any issues that cannot be resolved between the regional dean and VANTHCS pharmacy administration are elevated to the pharmacy practice department chair for faculty matters and to the dean of the school for administrative issues. The clinical education coordinator for VANTHCS pharmacy services collaborates with the regional dean and school administration to resolve any issues that arise. Issues that cannot be resolved by the clinical education coordinator are elevated first to the VANTHCS director of pharmacy services, and then to VANTHCS hospital administration only if necessary.
The clinical specialist collaboration between school faculty members and VANTHCS staff members allows for the development of practice teams in specialty areas that help ensure continuity of patient care. All clinical pharmacy specialists (VANTHCS staff and school faculty members) attend pharmacy meetings to ensure consistency in complying with VA clinical care directives, policies, and procedures. These meetings also provide time for faculty members and VANTHCS staff members to discuss practice strategies that have worked well and discuss other areas needing improvement. School faculty members must also inform VANTHCS of upcoming leave, professional events, and other school commitments in order to ensure that continuity of care will be maintained. VANTHCS reserves the right to refuse leave requests by school faculty members with conflicts being handled through the aforementioned methods.
Teaching.
The VANTHCS collaboration has allowed for expansion of clinical teaching, benefitting both the school and VANTHCS. In addition to the pharmacy students on P3 and P4 practical experiences, the VANTHCS collaboration allows postgraduate pharmacy residents to train with VANTHCS clinical specialists and school faculty members each year. The number of postgraduate residents has grown from 1 initially to 8 to 10 in recent years. This number of residencies at VANTHCS is more than either institution would be willing to support financially or have the manpower to train alone.
The number of advanced pharmacy practice experience (APPE) sites available to schools of pharmacy to train pharmacy students and residents is only 1 aspect of maximizing clinical training. Others have discussed the importance of evaluating the duration of the APPE, documenting workload during the APPE using an algorithm, longitudinal vs. block APPEs, student to preceptor ratios, and limited partnerships for directed programs in community and hospital settings.4-7 While these aspects are not the focus of this review, they should be considered in a global assessment of APPE resources.
Service.
VANTHCS utilizes professional services from the school to augment the number of clinical specialists on its staff. This collaboration helps ensure continuity of care with a VANTHCS clinical specialist and faculty member available to provide coverage for each clinical area staffed with clinical specialists. Services (also known as departments) in VANTHCS can be recognized by Courtesy in Action (CIA) stars or “speak to the director” comment cards submitted by patients and visitors. CIA stars are indicative of positive customer service provided by pharmacy. During fiscal year 2007, pharmacy services at VANTHCS received 36 CIA stars or “speak to the director” comments (September 2006 to September 2007).
Postgraduate Pharmacy Residency Programs.
The VA's Office of Academic Affiliations oversees all clinical health professions training programs in the VA, including the pharmacy residency programs. There are typically 8-10 pharmacy residents at VANTHCS in the areas of pharmacy practice, ambulatory care, critical care, and hematology/oncology. Future expansion of residency programs at VANTHCS is expected to include programs in pharmacy management as well as pharmacoeconomics. Of the previously noted 8 to 10 resident positions, the VANTHCS system funds 4 to 5 of the pharmacy practice positions as well as 2 to 3 of the specialty residency positions. The other specialty residencies are funded by the school. Regardless of the funding source, the residencies are managed as a collaborative effort between VANTHCS pharmacy staff and faculty members. VANTHCS clinical specialists and faculty specialty residency program directors are members of VANTHCS's Residency Advisory Council. They review resident progress and identify opportunities to improve the residency programs through resident and preceptor feedback. The School Residency Advisory Committee (RAC) addresses broad residency issues and policy for all school funded and affiliated programs including VANTHCS.
VANTHCS pharmacy leadership directs the pharmacy practice residency program, providing a broad array of experiences for residents through VANTHCS and school preceptors. Faculty members serve as program directors for the currently offered specialty residency programs.
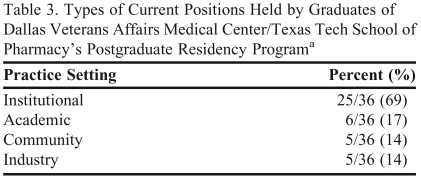
Both institutions have been able to benefit from the academic-practice partnership to recruit pharmacists for their respective institutions. Table 3 shows the current positions held by graduates of the shared VANTHCS/school postgraduate pharmacy residencies. VANTHCS currently employs 9 clinical pharmacy specialists on its staff who graduated from VA pharmacy residencies (5 from VANTHCS residencies). The Dallas School regional campus of Texas Tech employs 7 faculty members who have graduated from VA pharmacy residencies (2 from VANTHCS residencies).
Table 3.
Types of Current Positions Held by Graduates of Dallas Veterans Affairs Medical Center/Texas Tech School of Pharmacy's Postgraduate Residency Programa
Residents who entered academia with a clinical practice site are counted in all applicable rows.
Research.
Increased research activity has been a significant advantage to both VANTHCS and the school. Faculty members are expected to publish at least 1 peer-reviewed manuscript every year. Pharmacy residents must present a research poster for residency certification and are encouraged to submit their work for publication. Thus, the partnership has created an environment for productive research collaborations, resulting in the receipt of National Lipid Association Young Investigator's Award in 2007 and 2008 for work conducted at VANTHCS.
Research collaborations have utilized both the VANTHCS electronic medical record for retrospective chart reviews and the Clinical Research Unit for prospective pharmacokinetic work. One of the focus areas has been the management of dyslipidemias in patients infected with human immunodeficiency virus (HIV).9-15 These studies have helped provide guidance for the best practices to utilize when caring for HIV-positive patients with dyslipidemias. The inclusion of VANTHCS in a multicenter evaluation of vancomycin that focused on dosing for obese patients led to the development of a vancomycin dosing and monitoring team at VANTHCS.16 Cardiology and oncology have been other focus areas for research collaboration.17-22 These collaborations have increased the numbers of grants, research posters, platform presentations, and publications for both institutions.
The VA has a rich history of collaborating with schools of pharmacy which can be attributed to a similar tri-part mission of clinical practice, education, and research. The VANTHCS/school of pharmacy collaboration is an example of how an intentional, global approach can maximize the benefit of the relationship for both parties. VANTHCS has been able to augment its clinical pharmacy specialist staff with 12 school of pharmacy faculty members to help ensure continuity of care for veterans. The professional service contracts have given the school a greater ability to enhance educational programs and build infrastructure. Both parties have benefitted from the school campus being located on VANTHCS grounds since this allows for increased faculty efficiency with both academic and clinical practice activities. In addition, more postgraduate residents have been able to train at VANTHCS than either institution could support alone. We hope our experiences encourage other hospitals and schools of pharmacy to work together to provide the best patient care possible while training the next generation of health care professionals.
SUMMARY
The VANTHCS/school of pharmacy collaboration has clearly enhanced the ability of both institutions to exceed their practice, teaching, and research goals in a cost-effective manner. As previously described, the outcomes from this collaboration have been exemplary. The VANTHCS/school collaboration fosters an integrated, interdisciplinary approach to caring for patients with health conditions that are unique to veterans and the general population. Comparable collaboration between other schools of pharmacy and Veterans Affairs Medical Centers should be seriously examined and pursued to enhance missions of the collaborating partners. We believe the VANTHCS/school of pharmacy collaboration has been beneficial to both parties and advanced pharmacy education toward fulfilling ACCP's vision of pharmacists who will provide direct patient care in all patient care settings by 2020.23
ACKNOWLEDGEMENTS
Dr. Hall's involvement in this manuscript was supported by Grant Number KL2RR024983, titled, “North and Central Texas Clinical and Translational Science Initiative” (Milton Packer, MD, PI) from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research, and its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Re-engineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overviewtranslational.asp.
REFERENCES
- 1. Department of Veterans Affairs. Workforce Succession Strategic Plan FY 2008-2012. Washington, DC: Veterans Health Administration.
- 2.Capacity of hospitals to partner with academia to meet experiential education requirements for pharmacy students. Am J Pharm Educ. 2008;72(5) doi: 10.5688/aj7205117. Article 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patry RA, Eiland LS. Addressing the shortage of pharmacy faculty and clinicians: the impact of demographic changes. Am J Health-Syst Pharm. 2007;64(7):773–775. doi: 10.2146/ajhp060591. [DOI] [PubMed] [Google Scholar]
- 4.Draugalis JR, Carter JT, Slack MK. Curricular and financial implications of PharmD clerkship placements. Am J Pharm Educ. 1996;60(2):146–151. [Google Scholar]
- 5.Carter JT, Draugalis JR, Slack MK, Cox ER. Algorithms for estimating learning opportunity and productivity impact at clerkship sites. Am J Pharm Educ. 1998;62(3):258–265. [Google Scholar]
- 6.Plaza CM, Draugalis JR. Implications of advanced pharmacy practice experience placements: a 5-year update. Am J Pharm Educ. 2005;69(3) Article 45. [Google Scholar]
- 7.Turner CJ, Ellis S, Giles J, et al. A strategy to develop advanced pharmacy practice experiences. Am J Pharm Educ. 2007;71(3) doi: 10.5688/aj710346. Article 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. American Council for Pharmacy Education, Professional degree programs, Chicago, IL, 2002, June 1, 2003.
- 9.Busti AJ, Bain AM, Hall RG, 2nd, et al. Effects of atazanavir/ritonavir or fosamprenavir/ritonavir on the pharmacokinetics of rosuvastatin. J Cardiovasc Pharmacol. 2008;51(6):605–610. doi: 10.1097/FJC.0b013e31817b5b5a. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen ST, Eaton SA, Bain AM, et al. Lipid-lowering efficacy and safety after switching to atazanavir-ritonavir-based highly active antiretroviral therapy in patients with human immunodeficiency virus. Pharmacotherapy. 2008;28(3):323–330. doi: 10.1592/phco.28.3.323. [DOI] [PubMed] [Google Scholar]
- 11.Rahman AP, Eaton SA, Nguyen ST, et al. Safety and efficacy of simvastatin for the treatment of dyslipidemia in human immunodeficiency virus-infected patients receiving efavirenz-based highly active antiretroviral therapy. Pharmacotherapy. 2008;28(7):913–919. doi: 10.1592/phco.28.7.913. [DOI] [PubMed] [Google Scholar]
- 12.Busti AJ, Bedimo R, Margolis DM, Hardin DS. Improvement in insulin sensitivity and dyslipidemia in protease inhibitor-treated adult male patients after switch to atazanavir/ritonavir. J Investig Med. 2008;56(2):539–544. doi: 10.2310/JIM.0b013e3181641b26. [DOI] [PubMed] [Google Scholar]
- 13.Bain AM, Payne KD, Rahman AP, et al. A multicenter retrospective study of the lipid-lowering efficacy and safety of switching within the NNRTI class in HIV-infected patients. Am J Infect Dis. 2008;4:147–151. [Google Scholar]
- 14.Eaton SA, Rahman AP, Bain AM, et al. Efficacy of pravastatin in non-nucleoside reverse transcriptase inhibitor (NNRTI) and protease inhibitor (PI)-based HAART in HIV-infected patients. Am J Infect Dis. 2008;4:124–130. [Google Scholar]
- 15.Chastain L, Bain AM, Edwards K, Bedimo R, Busti AJ. A retrospective study of the lipid-lowering efficacy and safety of ezetemibe added to HMG-CoA reductase therapy in HIV-infected patients with hyperlipidemia. J Clin Lipidology. 2007;1:634–639. doi: 10.1016/j.jacl.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 16.Hall RG, 2nd, Payne KD, Bain AM, et al. Multicenter evaluation of vancomycin dosing: emphasis on obesity. Am J Med. 2008;121(6):515–518. doi: 10.1016/j.amjmed.2008.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mullin MA, Brouse SD. A comparison of event rates for patients receiving drug-eluting stents versus bare metal stents. J Pharm Technol. 2007;23:3–8. [Google Scholar]
- 18.Brouse SD, Wiesehan VG. Evaluation of Bleeding Complications Associated with Glycoprotein IIb/IIIa Inhibitors. Ann Pharmacother. 2004;38(11):1783–1788. doi: 10.1345/aph.1E048. [DOI] [PubMed] [Google Scholar]
- 19.Dobard M, Brouse SD, Shah MJ. Attainment of cholesterol guidelines in patients at high risk of coronary heart disease. Am J Health-Syst Pharm. 2006;63:212–214. doi: 10.2146/ajhp050382. [DOI] [PubMed] [Google Scholar]
- 20.Shah S, Dowell J, Greene S. An evaluation of clinical pharmacy services in a hematology/oncology outpatient setting. Ann Pharm. 2006;40:1527–1533. doi: 10.1345/aph.1H162. [DOI] [PubMed] [Google Scholar]
- 21.Stanford BL, Shah SR, Ballard EE, et al. A randomized trial assessing the utility of a test dose program with taxanes. Curr Med Res Opin. 2005;21:1611–1616. doi: 10.1185/030079905X65411. [DOI] [PubMed] [Google Scholar]
- 22.Shah SR, Vervan M. Use of i.v. immune globulin and occurrence of associated acute renal failure and thrombosis. Am J Health-Syst Pharm. 2005;62:720–725. doi: 10.1093/ajhp/62.7.720. [DOI] [PubMed] [Google Scholar]
- 23.American College of Clinical Pharmacy, ACCP position statement, postgraduate residency, direct patient care, future pharmacy profession, pharmacy practice. Pharmacotherapy. 2006;26(5):722–733. doi: 10.1592/phco.26.5.722. [DOI] [PubMed] [Google Scholar]